Abstract
Background:
Knee replacement is one of the most frequently performed surgical procedures in the world. Local data on revision total knee arthroplasty (TKA) are limited. This study aims to assess the rates and causes of revision TKA in Kashani Hospital (Isfahan, Iran) from 2011 to 2013.
Materials and Methods:
We assessed all primary TKA and revision TKA procedures performed from 2011 to 2013 for the rate and causes of failures. Demographic data, duration from primary TKA to revision TKA and underlying diagnosis for primary TKA were also assessed.
Results:
Overall, 353 primary TKA procedures carried out in this period. The overall revisions following primary TKA in this period was 24 cases, indicating a revision burden of 6.8%. The most common cause of revision TKA was infection, which was in 16 cases (44.4%). Other causes included patellar complications, mechanical loosening of both tibia and femur, mechanical loosening of tibia, instability, and periprosthetic fracture. The main revision procedures were all component revision, tibial component revision, isolated tibial insert exchange and patellar tendon repair. The most common revision procedure was two stage all component revision, which was carried out in 13 subjects (36.1%).
Conclusion:
Local indications for revision TKA are mainly similar to those in other large centers. As compared with other centers, with considering the follow-up time, revision burden is relatively higher in this center.
Keywords: Revision causes, revision rate, total knee arthroplasty
INTRODUCTION
Arthritis is described by progressive degeneration of articular cartilage that manifests ultimately as stiffness, joint pain, and/or dysfunction.[1] Surgical choices for treatment of knee arthritis are arthroscopic joint debridement, distal femoral osteotomy, high tibial osteotomy, unicompartmental knee arthroplasty, and total knee arthroplasty (TKA).[2,3] TKA is one of the most common reconstructive procedures which is performing in adult, and its frequency continues to increase.[4,5] It is a common, safe and successful treatment for end-stage knee arthritis that achieves a high rate of satisfaction in patients.[6,7] Because of this success, its indications have broadened to include more active and younger patients, which has increased the demand for this procedure.[8,9]
In spite of the ability of TKA to improve function and reduce pain in patients with arthritis, it can incur significant cost and is a resource-intensive procedure, which is related to the cost of hospital stay, of the implant, and of rehabilitation needs postoperatively.[10,11] In the other hand, the prosthesis lifespan is ultimately limited, and a significant number of subjects face the prospect of knee arthroplasty revision eventually.[12,13] Regardless of the type of the initial surgery, revisions are typically to a TKA and often need stemmed components and additional augments, which must address bone stock and soft tissue integrity, which are often compromised.[3,9] The most common reasons for revision are infection, mechanical wear, aseptic loosening, pain, instability, arthrofibrosis, malalignment and periprosthetic fractures.[12,14] The revision procedure is not an enviable task because the surgeon often encounters diffculties in handling soft tissue insuffciency and bone loss. Thus, the overall outcome is not as good as primary arthroplasty.[9,15]
Considering the economic burden and technical complexity of the revision TKA procedure, it would be important to investigate predictors for TKA failure, by focusing efforts to address these failure mechanisms, and improve the final outcome of TKA. Hence knowing about rates and causes of revision has been focused by many literatures on TKA.[10,11,16,17] With improvements in surgical technique, prosthesis design and measures to prevent infection, revision rates have declined; based on the recent joint registers worldwide, the revision rate for the TKA is on average 6–12% over a period of 10-year.[18,19]
The survival National registries have been done in certain European countries, Canada, United States, New Zealand, and Australia to monitor the causes and rates of revision replacement surgery.[8,9] In Iran, Local data on revision knee arthroplasty are limited. This paper aims to present local registry data on the rate and causes of revision TKAs in Isfahan, Kashani Hospital, over 3 years.
MATERIALS AND METHODS
Study design and participants
This study was carried out between January 1, 2011 and December 30, 2013. The study followed the Declaration of Helsinki on Biomedical Research Involving Human Subjects and was approved by the Ethics Committee from the Isfahan University of Medical Sciences. All participants provided written informed consent.
Subjects were selected from patients who were admitted to the orthopedic ward of Kashani Hospital (Isfahan, Iran) and had a TKA. All subjects met the following inclusion criteria: (1) Patients who undergo a TKA between 2011 and 2013; (2) patients who had a revision of TKA between 2011 and 2013; and (3) willing and able to provide written informed consent. Subjects also had not any serious medical condition that may interfere with safe study participation.
Procedures and variables assessment
The hospitals database was used to identify primary, and revision knee arthroplasty procedures performed between 2011 and 2013. We used the registered data on documents and surgery reports after primary and revision TKAs. Eligible subjects also asked for an interview and physical examination.
Demographic data included age and sex; and clinical data included: (1) Date and cause of TKAs; (2) date and cause of revision TKAs; (3) type of revision TKAs; (4) mechanical lateral distal femoral angle (MLDFA) before and after TKA and (5) mechanical medial proximal tibial angle (MMPTA) before and after TKA.
Aseptic loosening may be obvious on radiograph as a complete radiolucent line of 2 mm or more around the prosthesis at the bone cement interface in cemented arthroplasty. If there was a suspicion for infection, erythrocyte sedimentation rate/C-reactive protein (ESR/CRP) were assessed and if either was positive, then joint aspiration was done for cell count/differential and culture to decide that whether or not there is an infection. Positive ESR/CRP plus positive cell count/differential or culture was considered as possible infection. If cell count and culture were both negative, frozen section and/or synovial fluid white blood cell count during surgery were determinant.[20] Instability can be defined as abnormal and excessive displacement of a knee prosthesis accompanied by clinical failure. The AP and lateral views are taken with the X-ray beam directed parallel to the base plate of the tibial component to identify any changes between bone cement and prosthesis.[21,22]
The MLDFA was measured between following drawn lines. The distal femoral joint orientation line and the line from the center of the hip to the center point of the knee on the femoral knee joint line (femoral mechanical axis). The normal range was considered as 85°–90°.[23]
The MMPTA was measured between following drawn lines. The proximal tibial joint orientation line and the line from the center point of the ankle to the center point of the knee on the tibial knee joint line (tibial mechanical axis). The normal range was considered as 85°–90°.[23]
After exclusion, we were left with 353 primary TKAs. There were 24 revision TKAs out of 353 primary TKAs and overall 36 revision TKAs, without considering time of primary TKA, during 3 years follow-up.
Statistical analysis
The data were analyzed by paired sample t-test and repeated measure of ANOVA. All analyzes were performed using Statistical Package for the Social Sciences version 20.0 (SPSS Inc., Chicago, Illinois, USA) and a P < 0.05 was considered as statistically significant for all analyses.
RESULTS
Overall, 353 primary TKA procedures carried out between January 1, 2011 and December 30, 2013 in Kashani Hospital (Isfahan, Iran). The mean (standard deviation [SD]) age of patients was 61.3 (6.7) years. The utilization rates for primary TKA was 252 (71.4%) for women, and 101 (28.6%) for men; which was higher in women significantly (P < 0.001).
In this 353 patients, the most common cause of primary TKA was osteoarthritis with 320 cases (90.6%).
The revisions following this 353 primary TKAs in this center and this period (3-year), were 24 cases which indicate a revision burden of 6.8% for this center. The mean (SD) of patient age was 68.5 (7.1) years ranging from 57 to 79 years. The mean follow-up time was 18.3 (2–35) months. Mean (SD) duration from primary TKA was 9.5 (9.6), ranging from 1 to 31 months. 5 (20.8%) of patients were male and 19 (79.2%) were female. The utilization rates for revision TKA were higher for women significantly (P < 0.004). Mean (SD) duration from primary TKA was not different significantly between men and women (P = 0.44).
On the other hand, the overall revision TKA procedures in this 3 years, without considering time of primary TKA, were 36 cases. For analyzing of overall causes of revision TKAs, we included all of this 36 revision. The mean (SD) age of patients was 68.2 (7.9) years, ranging from 47 to 83 years. Mean (SD) duration from primary TKA was 37.2 (58.6), ranging from 1 to 294 months. 9 (25%) of patients were male and 27 (75%) were female. The utilization rates for revision TKA was higher for women significantly (P < 0.003). Mean (SD) duration from primary TKA was not different significantly between men and women (P = 0.999).
In this 36 revisions, the most common cause of primary TKA was osteoarthritis with 31 cases (86.1%), [Table 1].
Table 1.
Causes of primary TKA in patients with revision (n=36)

The most common cause of revision TKA was infection, which was in 16 cases (44.4%). The predominant noninfectious causes were patellar complications (fracture or tendon tearing), with 9 cases (25%). Other causes included mechanical loosening of both tibia and femur, mechanical loosening of tibia, instability and fracture [Table 2].
Table 2.
Causes of revision in patients with revision TKA (n=36)
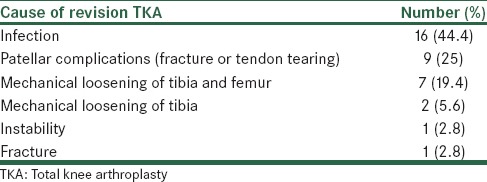
The mean (SD) age was 65.6 (7.9) years for patients with infection and 70.4 (7.6) years for patients with patellar complications.
Between 9 patients with patellar complications, after revision surgery, one had 20° lag of extension and others had full extension in physical examination. The mean degree of flexion was 104.4°.
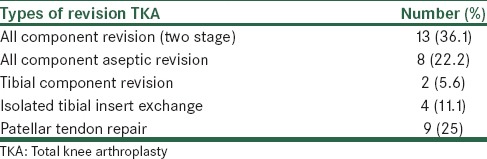
The main revision procedures were all component revision, tibial component revision, isolated tibial insert exchange and patellar tendon repair [Table 3]. The most common revision procedure was two stage all component revision, which was carried out in 13 subjects (36.1%); that is, antibiotic loaded cement spacers for an interval period, with intravenous antibiotics and also antibiotic loaded cement for prosthesis fixation at the time of re-implantation.
Table 3.
Types of revision in patients with revision TKA (n=36)
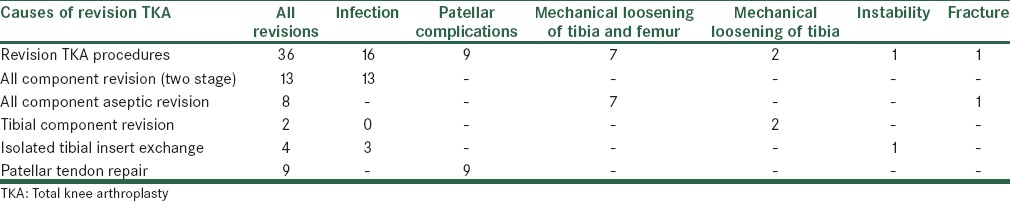
Causes of revision TKA associated with revision TKA procedures is presented in Table 4.
Table 4.
Causes of revision TKA associated with revision TKA procedures
In 36 patients with revision TKA, the mean (SD) of MLDFA before and after surgery were 96.2 (3.7) and 90.3 (2.1), respectively; which was reduced significantly (P < 0.001). And the mean (SD) of MMPTA before and after surgery were 80.25 (4.4) and 84.3 (2.03), respectively; which was increased significantly (P < 0.001).
DISCUSSION
In spite of the good functional outcomes that have been reported with primary TKA, revision TKA remain an important clinical challenge for surgeons and patients. In this study, with 3 years follow-up, revision burden was 6.8% which is more than some previous studies with 1.4%, 2.2%, 2.8% and 3.3% for 3, 10, 8 and 5 years follow-up, respectively.[15,24,25,26] In a recent systematic review, Pabinger et al. reported that overall 10 years worldwide revision rates of TKA was 6.2% (range: 4.9–7.8%),[19] which is near to revision rates in our 3-year follow-up study. This shows that considering the follow-up time, revision burden is higher in Kashani Hospital.
This matter could have different reasons and is affected by various items such as indications for primary TKA; age, gender and race of patients; and also length of hospital stay after TKA. In the other hand, in our study the most common reason for revision was infection. The infection is related to the increased operative time for surgery, poor wound healing, the increased age of our patient population and perioperative care methods. Understanding of these reasons are essential to improving implant performance and long-term patient outcomes, so should be assessed in future studies.
Several causes are well-defined for failure of TKA in previous studies, including mechanical wear, aseptic loosening, infection, instability, osteolysis, pain, stiffness, malalignment, patellar complications and periprosthetic fractures.[12,24,27,28,29] In our study, the causes of failure leading to revision are similar to recent series.[9,12,24]
In this study, the most common reason for revision was infection, which was similar to Julin et al. and Bozic et al. studies.[24,29] However in others, mechanical loosening had been the major cause of revision.[25,27] It is very important because the cost of surgery and treatment of infected TKA is much more than that of nonseptic revision TKA and that of primary TKA;[30] and also the patient outcomes is relatively poor with revision TKA for infection compared with revision TKA for aseptic causes of failure.[29] In our study, most of patients with infection (13 subjects) had two stage all component revision (the most expensive revision type), and also all of two stage all component procedures were done for patients with infection. Infection was the most common reason for isolated tibial insert revision (3 of 4 cases); this was the same as Bozic et al. study.[29]
Patellar complications were predominant noninfectious causes of revision TKA in our study which is similar to Julin et al. study.[24]
The most common type of revision TKA reported during the time period under study was all component revision (one or two stage); it is similar to Bozic et al. study.[29] This procedures were done mainly for infection and mechanical loosening of tibia and femur.
Advantages and limitations
These data provide an understanding of the risk and causes of revision after primary TKA in the local population. This study is particularly important from a local standpoint because according to our researches, the causes of revision knee arthroplasty in local setting have not been previously described. Therefore, it gives valuable data in this aspect. More understanding of current causes by which TKA fail may help surgeons to prevent these problems and improve outcomes for TKA. Our findings are also limited by a relatively small sample size and short-time period of data collection and hence this study can be improved by working on a larger sample size, which would allow for more accurate subgroup analysis.
CONCLUSION
In this study, local indications for revision TKA are mainly similar to those in other large centers. Also, in comparison with other centers, with considering the follow-up time, revision burden is relatively higher in this center. Increasing the follow-up time will enable us to clarify the survivorship of implants in the longer term.
ACKNOWLEDGMENT
We would like to express thanks for staffs of orthopedic ward of Kashani Hospital (Isfahan, Iran).
This paper is derived from a specialty thesis in Isfahan University of Medical Sciences.
Footnotes
Source of Support: This study is funded by Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Waller C, Hayes D, Block JE, London NJ. Unload it: The key to the treatment of knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19:1823–9. doi: 10.1007/s00167-011-1403-6. [DOI] [PubMed] [Google Scholar]
- 2.Palomo JM. Surgical options for middle-aged patients with osteoarthritis of the knee. J Bone Joint Surg Am. 2001;83-A:1429. doi: 10.2106/00004623-200109000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Bhandari M, Smith J, Miller LE, Block JE. Clinical and economic burden of revision knee arthroplasty. Clin Med Insights Arthritis Musculoskelet Disord. 2012;5:89–94. doi: 10.4137/CMAMD.S10859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: National projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–12. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–97. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 6.Tai CC, Cross MJ. Five- to 12-year follow-up of a hydroxyapatite-coated, cementless total knee replacement in young, active patients. J Bone Joint Surg Br. 2006;88:1158–63. doi: 10.1302/0301-620X.88B9.17789. [DOI] [PubMed] [Google Scholar]
- 7.Murphy M, Journeaux S, Russell T. High-flexion total knee arthroplasty: A systematic review. Int Orthop. 2009;33:887–93. doi: 10.1007/s00264-009-0774-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 9.Hossain F, Patel S, Haddad FS. Midterm assessment of causes and results of revision total knee arthroplasty. Clin Orthop Relat Res. 2010;468:1221–8. doi: 10.1007/s11999-009-1204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kreder HJ, Grosso P, Williams JI, Jaglal S, Axcell T, Wal EK, et al. Provider volume and other predictors of outcome after total knee arthroplasty: A population study in Ontario. Can J Surg. 2003;46:15–22. [PMC free article] [PubMed] [Google Scholar]
- 11.Kurtz SM, Ong KL, Lau E, Widmer M, Maravic M, Gómez-Barrena E, et al. International survey of primary and revision total knee replacement. Int Orthop. 2011;35:1783–9. doi: 10.1007/s00264-011-1235-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Mortazavi SM, Molligan J, Austin MS, Purtill JJ, Hozack WJ, Parvizi J. Failure following revision total knee arthroplasty: Infection is the major cause. Int Orthop. 2011;35:1157–64. doi: 10.1007/s00264-010-1134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paxton EW, Furnes O, Namba RS, Inacio MC, Fenstad AM, Havelin LI. Comparison of the Norwegian knee arthroplasty register and a United States arthroplasty registry. J Bone Joint Surg Am. 2011;93 Suppl 3:20–30. doi: 10.2106/JBJS.K.01045. [DOI] [PubMed] [Google Scholar]
- 15.Ong KL, Lau E, Suggs J, Kurtz SM, Manley MT. Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Relat Res. 2010;468:3070–6. doi: 10.1007/s11999-010-1399-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Serra-Sutton V, Allepuz A, Espallargues M, Labek G, Pons JM. Arthroplasty registers: a review of international experiences. Int J Technol Assess Health Care. 2009;25:63–72. doi: 10.1017/S0266462309090096. [DOI] [PubMed] [Google Scholar]
- 17.Saleh KJ, Rand JA, McQueen DA. Current status of revision total knee arthroplasty: How do we assess results? J Bone Joint Surg Am. 2003;85-A Suppl 1:S18–20. doi: 10.2106/00004623-200300001-00005. [DOI] [PubMed] [Google Scholar]
- 18.Labek G, Thaler M, Janda W, Agreiter M, Stöckl B. Revision rates after total joint replacement: Cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. 2011;93:293–7. doi: 10.1302/0301-620X.93B3.25467. [DOI] [PubMed] [Google Scholar]
- 19.Pabinger C, Berghold A, Boehler N, Labek G. Revision rates after knee replacement. Cumulative results from worldwide clinical studies versus joint registers. Osteoarthritis Cartilage. 2013;21:263–8. doi: 10.1016/j.joca.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 20.Frank RM, Cross MB, Della Valle CJ. Periprosthetic joint infection: Modern aspects of prevention, diagnosis, and treatment. J Knee Surg. doi: 10.1055/s-0034-1396015. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Rodriguez-Merchan EC. Instability following total knee arthroplasty. HSS J. 2011;7:273–8. doi: 10.1007/s11420-011-9217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gonzalez MH, Mekhail AO. The failed total knee arthroplasty: Evaluation and etiology. J Am Acad Orthop Surg. 2004;12:436–46. doi: 10.5435/00124635-200411000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Paley D. 3rd ed. New York: spriger-Verlag Berlin Heidelberg; 2005. Principles of Deformity Correction; pp. 19–30. [Google Scholar]
- 24.Julin J, Jämsen E, Puolakka T, Konttinen YT, Moilanen T. Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis. A follow-up study of 32,019 total knee replacements in the Finnish Arthroplasty Register. Acta Orthop. 2010;81:413–9. doi: 10.3109/17453674.2010.501747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kasahara Y, Majima T, Kimura S, Nishiike O, Uchida J. What are the causes of revision total knee arthroplasty in Japan? Clin Orthop Relat Res. 2013;471:1533–8. doi: 10.1007/s11999-013-2820-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sibanda N, Copley LP, Lewsey JD, Borroff M, Gregg P, MacGregor AJ, et al. Revision rates after primary hip and knee replacement in England between 2003 and 2006. PLoS Med. 2008;5:e179. doi: 10.1371/journal.pmed.0050179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tay KS, Lo NN, Yeo SJ, Chia SL, Tay DK, Chin PL. Revision total knee arthroplasty: Causes and outcomes. Ann Acad Med Singapore. 2013;42:178–83. [PubMed] [Google Scholar]
- 28.Mikulak SA, Mahoney OM, dela Rosa MA, Schmalzried TP. Loosening and osteolysis with the press-fit condylar posterior-cruciate-substituting total knee replacement. J Bone Joint Surg Am. 2001;83-A:398–403. doi: 10.2106/00004623-200103000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maradit Kremers H, Visscher SL, Moriarty JP, Reinalda MS, Kremers WK, Naessens JM, et al. Determinants of direct medical costs in primary and revision total knee arthroplasty. Clin Orthop Relat Res. 2013;471:206–14. doi: 10.1007/s11999-012-2508-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


