Abstract
Background:
Coma is one of the most important complications of brain injury. Comatose patients in the intensive care units are exposed to sensory deprivation. This study aims to survey the effect of family members’ voice on level of consciousness of comatose patients hospitalized in the intensive care units.
Materials and Methods:
In this single-blind randomized controlled trial, 40 comatose patients with brain injury with acute subdural hematoma in intensive care units were randomly assigned into two groups. The intervention group was stimulated twice a day each time 5-15 min with a recorded MP3 from family members’ voice for 10 days. The patients’ level of consciousness was measured with Glasgow Coma Scale before and after auditory stimulations. In the control group, GCS was measured without auditory stimulation with the same time duration like intervention group. Data analysis in software SPSS version 15 and using Chi-square test, independent t-test, paired t- test and analysis of variance with repeated measures was done.
Results:
On the first day before the intervention, there was no a statistically significant difference between the mean of GCS in both groups (P = 0.89), but on the tenth day after the intervention, there was a significant difference (P = 0.0001) between the mean GCS in both control and intervention groups. Also, there was a significant difference between the mean daily GCS scores in two groups (P = 0.003). The findings during ten days showed the changes in the level of consciousness in the intervention group from the 4rd day of the study were more in the mean daily GCS scores than control group.
Conclusion:
This study indicated that family members’ voice can increase level of consciousness of comatose patients with acute subdural hematoma.
Keywords: Auditory stimulation, brain injury, coma, family members’ voice, level of consciousness
INTRODUCTION
One of the main consequences of brain injury is coma. Coma is defined as a state of impaired consciousness that the patient is unresponsiveness so that cannot response to the environment stimulations and cannot be aroused.[1] Today, the amount of brain injury in the world has increased rapidly, so that each year about two million people are suffering from brain damage in the United States.[2] One of the most common complications resulting from impacts to the head is intracranial hematoma, which is depending on the position divided into epidural, subdural and intracerebral hematomas. In the study of traumatic coma data bank (TCDB), 58% of all of the patients who underwent hematoma discharge and 21% of all of the patients who had severe head trauma suffering subdural hematoma and the most common cause of acute subdural hematoma is accidents.[3] In this type of hematoma as blood accumulates in the subdural space, however, pressure on the brain increases and subsequently causing acute neurological disorders. Intracranial hematoma, including subdural hematoma, can be associated with life-threatening complications such as coma.[4] Comatose persons may stay in coma for long periods and when they come out of coma they will face with motor and cognitive impairments.[5] In addition to these dysfunctions, another threatening complication in comatose patients which is gained less attention is sensory deprivation.[6] Staying in environments with limited exposure to sensory stimuli, such as intensive care units (ICU), increases the risk of sensory deprivation in patients and have some effects like perceptual, cognitive and emotional impairments on patients.[7,8] One of the steps that can be done to prevent sensory deprivation in comatose patients is using the sensory stimulation through sensory stimulation programs. Sensory stimulation programs for comatose patients through stimulating the reticular activating system and increasing the level of cognitive functioning stimulate the brain and cause the patients come out of coma as soon as possible and achieve to optimal performance levels.[6] Onset of sensory stimulation on the first 72 hours after brain injury has a great importance in saving the patient's life, improving quality of life, and prognosis of the disease.[9] In this regard Hyunsoon and Whasook (2003) wrote: To facilitate the healing process and prevent the sensory deprivation in comatose patients with traumatic brain injury using the organized sensory stimulation programs in the early stages after brain injury is essential.[10] Hosseinzadeh et al., (2012) in their study concluded that patients receiving auditory stimulation back into consciousness by the nurse's voice earlier than other patients.[5] Among the various sensory stimulations, auditory stimulation more attention has taken into consideration because hearing is the last sense goes in coma patients, and unlike the other senses, there is no obstacle to stimulate this sense.[6] The current study was designed and done because of some reasons including: (a) The high rate of accidents which are the major cause of brain trauma in Iran, (b) the high incidence of subdural hematoma and occurrence the induced coma and therefore increasing the length of admission of the patients in the ICU and appearing various complications such as sensory deprivation because of inadequate sensory stimulation, (c) because the researcher gained some experiences about concentrations of nursing cares on the patients’ physical needs such as ventilation and feeding and other main needs like the need to sensory stimulation were ignored. Therefore, this study aims to evaluate the effect of family members’ voice on level of consciousness of comatose patients admitted to the intensive care unit.
MATERIALS AND METHODS
This study is a randomized controlled trial. The participants were 40 trauma patients admitted to intensive care units with acute subdural hematoma in Yazd, Shahid Rahnemoun hospital. Sampling lasted about 6 months and patients were assigned into control and intervention groups using simple randomization; 20 patients in each group. The inclusion criteria were: Age between 15 to 75 of both genders and Glasgow Coma Scale scores (GCS) were less than or equal to 8 at least 24 hours after fixing their hemodynamic symptoms. Exclusion criteria were: The history of brain injury, impaired hearing, blood excretion from ears and nose, skull base fractures, and the history of drug addiction. Comatose patients who met inclusion criteria went under study 24 h after recording their hemodynamic signs and obtained the written informed consent from their family members. In the intervention group, we used head phone to play voices for patients. For 10 days, patients received a voice of a loved person in their family twice a day in the morning and night shifts that recorded 5-15 min on MP3. The recorded voice included introducing speaker, place and time, what had happened to the patients, the name of patients that repeated at least 3 times during the recorded voice, sweet memories, and sentences about recovery and expressing hope. Glasgow Coma Scale (GCS) scores is recorded by the researcher assistants before and after auditory stimulation (four times daily). The patients should not be touched during the study. The sound of a loved one in the family was recorded by an MP3 Player, Marshal Model, by the investigator in a separate room in the hospital. In the control group, GCS scores were measured without auditory stimulation with the same intervals (four times daily) [Figure 1]. Information gathering tools included a demographic characteristics form, and Glasgow Coma Scale tool to measure the level of consciousness that its validity and reliability has been approved in many studies.[11] This Randomized clinical trial was registered with the site IRCT2013110415280N1 code. The mean scores of the GCS before and after the intervention in both intervention and control groups were determined. Statistical analyzes were performed using SPSS-15, Chi-square test, t-test and paired test and analysis of variance with repeated measures.
Figure 1.
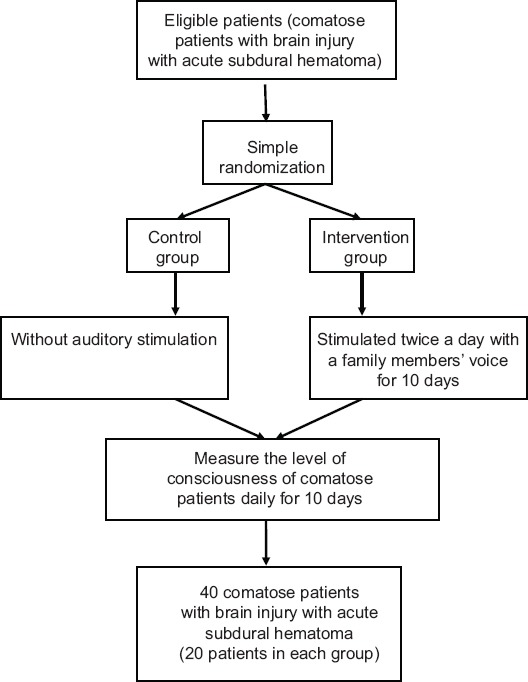
The flowchart of study groups
RESULTS
The results of this study showed that the mean age of the patients in the intervention group were 38.05 ± 7.43 and in the control group 34.80 ± 5.91, respectively. Independent t-test showed no statistically significant differences between two groups with respect to age (P = 0.13). The highest percentage of patients was in 30-44 age group range (70%). In this study, the majority of participants were male in both groups (80%). The results of Chi-square test showed that in terms of sex (P = 0.69) and age (P = 0.47) there was no significant differences; these results showed the homogeneity of the two groups in terms of age and gender. The results showed that means of GCS's scores in patients before of the study on the 1st day in the intervention and control groups were 6.25 ± 1.25 and 6.30 ± 1.03, respectively. Independent t-test showed that there was no statistically significant difference between means of GCS's scores of the 1st day in both groups (P = 0.89), these results indicated the homogeneity of two groups in means of GCS's scores on the first day [Table 1]. Means of GCS's scores after the onset of the study on the 10th day in the intervention group and control group were 10.25 ± 1.37 and 7.75 ± 0.78, respectively. The Independent t-test showed significant differences between the two groups (P = 0.0001) [Table 2]. The results of paired t-test, which was used to compare means of GCS's scores on the 1st and 10th days in both groups showed that in the intervention group between means of GCS's scores on the 1st day, before the intervention (6.25 ± 1.25) and the mean of the 10th day after intervention (10.25 ± 1.37) there was a statistically significant difference (P = 0/0001) [Table 3]. In the control group, the results of paired t- test showed that between means of GCS's scores on the 1st day, before the study (6.30 ± 1.03) and the 10th day after the beginning of the study (7.75 ± 0.78) there was a statistically significant difference (P = 0.0001) [Table 4]. The ANOVA with the repeated measures on the effect of time and changes in the means of GCS's scores and the interactive effect of time on GCS showed that the effect of time was significant and the changes of means of GCS's scores in both groups during the time was significant (P = 0.0001). The interactive effect of time on groups was significant as changes of means of GCS's scores in both groups during the different times was different (P = 0.0001). Also, totally changes of means of GCS's scores between two groups during ten days, revealed a significant difference (P = 0/003) [Figure 2].
Table 1.
Comparison the level of consciousness scores mean on the 1st day, before the study of comatose patients in the intervention and control groups
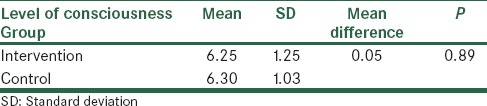
Table 2.
Comparison the level of consciousness scores mean on the 10th day, after the beginning of the study in the intervention and control groups
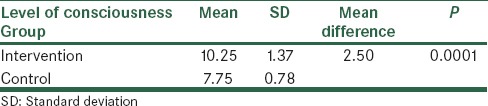
Table 3.
Comparison the level of consciousness scores mean on the 1st day, before the intervention and the 10th day, after the intervention in the intervention group
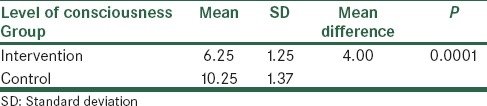
Table 4.
Comparison the level of consciousness scores mean on the 1st day, before the study and the 10th day, after the study in control group
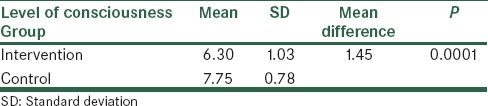
Figure 2.
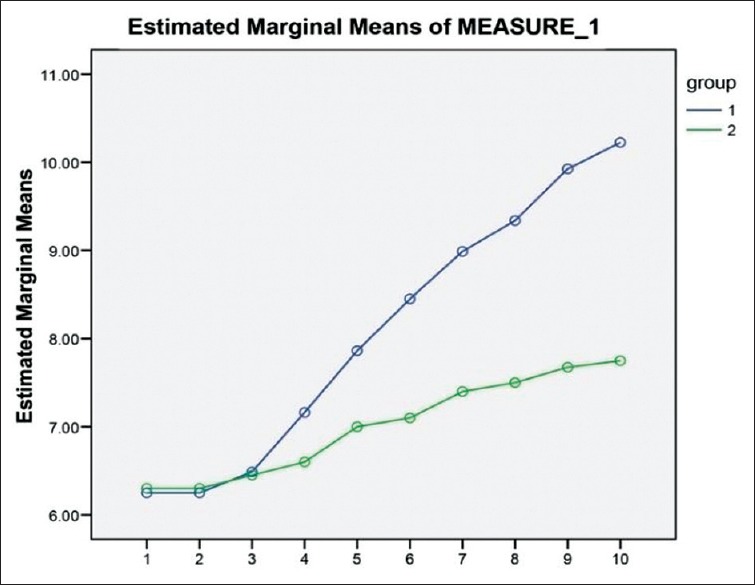
Diagram of changes in the level of consciousness scores mean during ten days of the study in both groups
DISCUSSION
The findings of this study showed that the majority of patients with traumatic coma aged 30-44 years and the majority of participants in both groups were male. In line with the present study in Bassampoor et al., (2007) study the majority of traumatic coma patients were between 25-44 years and males were the majority.[12] In this study, the patients’ GCS scores mean before the beginning of the intervention on the 1st day in both groups showed no statistically significant difference. This result indicated the homogeneity of the two groups which was similar to Bassam poor et al., (2007) and Hosseinzadeh et al., (2013) and Heidari Gorji et al., (2014) studies.[12,6,13] The results of this study among the means of GCS's scores on the 10th day after the beginning of the study on the patients in both groups indicated a significant difference (P = 0.0001), in the intervention group the mean was more than the control. Karma and Rawat (2006) in their study reached to this conclusion that the means of GCS's scores on the 14th day in both control and intervention groups were significantly difference and this mean in the intervention group was more than control group.[14] These results were followed by the current study. Urbenjaphol et al., (2009) in their study found that two weeks after the programs of sensory stimulation on traumatic brain injury patients, the mean of GCS's scores were significantly more than those in the control group (P < 0.05).[15] Megha et al., reported that there was significant difference in mean of GCS scores between intervention group that received multimodal coma stimulationin after 2 weeks and control group.[16] Thus, these findings showed a positive effect of the voice of family members on the level of consciousness of comatose patients with acute subdural hematoma. Another part of the results showed that there were significant differences between the means of GCS's scores of both groups on the 1st day, before the intervention and the 10th day, after the intervention but on the 10th day of the study, the mean of GCS's scores of the patients in the intervention group were more than the control group. So that in the intervention group, the mean daily GCS's scores on the 10th day were more than 8 (this is, the patients have come out of coma), but this mean in the control group was lower than 8 (this is, the patients who were still in coma). Therefore, the positive effect of the voice of family members on the improvement of the level of consciousness in comatose patients was realized. In the study, Bassampoor et al., (2007) by comparing the mean level of consciousness scores on the 1st day before the intervention with the mean scores of consciousness level on the 14th day after the intervention showed that in the intervention group there was a significant difference (P < 0.001) this result was similar to the result of the current study, but in the control group there was no significant difference (P = 0.769) and this result was not in line with the current study.[12] The findings of this study on the changes in the level of consciousness during a ten- day study revealed that increasing the mean daily of patients’ GCS scores in the intervention group compared with the control group was different from the 4rd day onwards. From the 4rd day of the study, the high increasing was seen in the mean daily GCS scores in the intervention group compared with the control group. As it can be seen in Figure 1, on the 10th day of the study the mean daily of patients’ GCS scores in the control group had reached approximately 7.75 which this mean was the same for intervention group on the 5th day of the study. It showed that the patients in the intervention group reached to a higher level of consciousness in the shorter time than the control group. These results showed that the interference had positive results. According to Figure 1, the mean daily of GCS's score of 8 was seen in the intervention group from the 6th day of the study onwards, meanwhile, even on the 10th day of the study, in the control group the mean daily of GCS's score was below 8, that is, the patients are still in a coma. Results of the study of Hosseinzadeh et al., (2013) showed that in the intervention group the mean GCS's scores increased from the 4th to 10th day which was in accordance with the present study.[6] In present study, the findings showed that the effect of time on GCS score was significant and the mean changes of GCS score in both groups during the time were significant. Also, the interactive effect of time on groups was significant and totally mean changes of GCS scores between two groups during ten days revealed a significant difference. In our study, two groups were homogenized. Because of significant difference between the mean scores of consciousness level of patients in two groups, it can be said that family voices on the improvement of level of consciousness in comatose patients with acute subdural hematoma had positive effect. In Hosseinzadeh et al. (2013) study which was in line with the present study, the ten-day study period in both intervention and control groups led to significantly increase in the levels of GCS scores (P < 0.001). Intervention alone and under the influence of time led to a significant increase in the level of GCS's scores (P < 0.001).[6] In the study of Davis and Jimenez (2003), the findings of the study between the mean daily of GCS's scores in both groups were no significant differences (P = 0.14) which was not in line with the present study.[11] In the present study, the mean of level of consciousness scores on the 10th day compared with the 1st day in intervention group was significantly different that showed a positive impact of family members’ voice on the level of consciousness of comatose patients with an acute subdural hematoma. Therefore, based on the results of this study, this method can be used in intensive care units along with the other treatment methods and nursing care to improve the patients’ level of consciousness and prevent the complications resulting from loss of consciousness and coma. The limitations of this study were the relatively small sample size, less willing of families to participate in the study.
ACKNOWLEDGEMENT
This article is an extract from a thesis. We would like to thank Shahid Sadoughi University of Medical Sciences, Yazd, Iran because of supporting this survey.
Footnotes
Source of Support: This article is supported by Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Conflict of Interest: None declared.
REFERENCES
- 1.Mandeep PK. Effectiveness of early intervention of coma arousal therapy in traumatic head injury patients. Int J Head Neck Surg. 2012;3:137–42. [Google Scholar]
- 2.Ebrahimifakhar H. The outcome of patients hospitalized with severe head injury in Valiasr Hospital according to Glascow Coma Scale in 2005-2006. Arak Med Univ J (AMUJ) 2010;12:1–9. [Google Scholar]
- 3.Skandaroghli B, Novrozi V, Sharghi A, Amani F. Study of Effective Factors on Treatment Outcomes of Acute Traumatic Subdural and Epidural Hematomas in Patients with Head Trauma at Fatemi Hospital in Ardabil City. J Ardabil Univ Med Sci. 2011;11:105–12. [Google Scholar]
- 4.Shirazi MM. Surgical results of acute subdural hematomas in Qazvin Shahid Rajaee Hospital. Qazvin Univ Med Sci. 2003;7:33–7. [Google Scholar]
- 5.Hossein Zadeh E, Mahmoodi Shan G, Vakili M, Kazem Nejad K, Mohammadi M, Taziki M, et al. The effect of voice auditory stimulation on the consciousness of the coma patients suffering from head injury. J Res Dev Nurs Midwifery. 2013;10:1–9. [Google Scholar]
- 6.Goudarzi F, Bassampoor S, Zakaeri Moghadam M, Faghih Zadeh S, Rezayi F, Mohamadzade F. Changes in the level of consciousness during coma for 14 days with the familiar sound of auditory stimulation. J Nurs Midwifery Iran Univ Med Sci. 2003;23:43–50. [Google Scholar]
- 7.Taylor C, Lillis C, LeMone P. Philadelphia: Lippincott Williams and Wilkins; 2005. Fundamentals of nursing: The art and science of nursing care; pp. 907–20. [Google Scholar]
- 8.Crisp J, Taylor C, Douglas C, Rebeiro G. New South Wales, Australia: Elsevier; 2005. Fundamentals of nursing. [Google Scholar]
- 9.Hasanzadeh F, Hoseini Azizi T, Esmaily H, Ehsaee M. The impact of familiar sensory stimulation on level of Consciousness in patients with head injury in ICU. J North Khorasan Univ Med Sci. 2012;4:121–33. [Google Scholar]
- 10.Oh H, Seo W. Sensory stimulation programme to improve recovery in comatose patients. J Clin Nurs. 2003;12:394–404. doi: 10.1046/j.1365-2702.2003.00750.x. [DOI] [PubMed] [Google Scholar]
- 11.Davis AE, Gimenez A. Cognitive-behavioral recovery in comatose patients following auditory sensory stimulation. J Neurosci Nurs. 2003;35:202–14. doi: 10.1097/01376517-200308000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Bassampoor S, Zakaeri Moghadam M, Faghih Zadeh S, Goudarzi F. The effect of auditory stimulation on the level of consciousness of coma patients. J Nurs Midwifery Tehran Univ Med Sci. 2007;13:15–22. [Google Scholar]
- 13.Gorji MH, Araghiyansc F, Jafari H, Gorgi AH, Yazdani J. Effect of auditory stimulation on traumatic coma duration in intensive care unit of Medical Sciences University of Mazandarn, Iran. Saudi J Anesth. 2014;8:69–72. doi: 10.4103/1658-354X.125940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karma D, Rawat AK. Effect of Stimulation in Coma. Indian Pediatr. 2006;43:856–60. [PubMed] [Google Scholar]
- 15.Urbenjaphol P, Jitpanya C, Khaoropthum S. Effects of the Sensory Stimulation Program on Recovery in Unconscious Patients with Traumatic Brain Injury. J Neurosci Nurs. 2009;41:E10–6. [Google Scholar]
- 16.Megha M, Harpreet S, Nayeem Z. Effect of frequency of multimodal coma stimulation on the consciousness levels of traumatic brain injury comatose patients. Brain Inj. 2013;27:570–7. doi: 10.3109/02699052.2013.767937. [DOI] [PubMed] [Google Scholar]


