Abstract
Background:
There is an inverse relation between the uterine cervical length during pregnancy and the frequency of preterm delivery. The purpose of this study was to construct a chart and evaluate the cervical length at 8 to 38 weeks of normal gestation in the center of Iran.
Materials and Methods:
Uterine cervical length was measured on 930 asymptomatic pregnant women by abdominal ultrasonographic technique. For statistical evaluation, regression analysis and calculation of percentiles were performed.
Results:
Our data show a significant decrease in uterine cervical length with increasing gestational age. The mean uterine cervical length exhibits minimal changes from 10 to 24 weeks for most women in this study, although the shortening is more prominent at 33 to 38 weeks’ gestation. The mean shortening of the uterine cervical length between the second and the ninth months was 14.82% (P < 0.05). Also, the cervical length means in trimesters 1, 2 and 3 were 39.30 ± 4.33, 38.28 ± 5.13 and 36.58 ± 4.58 mm, respectively. The third trimester showed a significant reduction (P < 0.05) in cervical length compared to the first and second trimesters (6.92% and 4.44%, respectively). New charts with the 5th, 10th, 50th, 90th, and 95th percentile are presented.
Conclusion:
Our study provides a new chart and reference values for normal uterine cervical length throughout gestation based on a large sample in the center of Iran. There was a progressive decrease in mean uterine cervical length with increasing gestational age in the population of this study. Our established charts for uterine cervical length throughout gestation might be more useful than a single cut-off value for more efficient prevention and management of preterm birth.
Keywords: Cervical-length, gestation, reference range, ultrasonography
INTRODUCTION
Measuring of cervical length and finding of cervical funneling may be of particular value in predicting and managing of placenta previa, preterm labor, and cervical incompetence. A large amount of the evidence indicates that there is an inverse relation between the length of the uterine cervix during pregnancy and the frequency of preterm delivery. The relative risk of preterm birth increases with decreasing cervical length.[1,2] Previous studies have suggested that an ultrasound examination can present a more accurate assessment of the uterine cervical length and wedging than a digital examination.[3,4] Moreover, ultrasonographic assessment of uterine cervical length is an accurate procedure that provides additional information about cervical competency in comparison to digital examination.[5] Although there are no standards for uterine cervical length by increasing of gestational age, many studies have prepared reference ranges for cervical length measured by transvaginal ultrasound in large populations of women with singleton pregnancies.[1,6] Transvaginal ultrasound is the most reliable method to evaluate uterine cervical length, but it is not available in all locations and adding transvaginal ultrasound to routine pregnancy exam cause patient discomfort.[1] Transabdominal sonography, however, is routinely performed at midtrimester and it can provide an effective means of assessing the cervix, and fetal anatomy (18-20 weeks’ gestation). Transabdominal sonography does not need additional equipment, is well-accepted by women, and provides a noninvasive method of detecting individuals at risk for preterm.[1,7,8]
There are some reasons for the necessity to improve longitudinal charts of cervical length during normal gestation. Firstly, there are different reports about the longitudinal changes of the uterine cervical length, and secondly uterine cervical length seems to differ in various populations.[9,10,11] Nevertheless, few studies have examined cervical changes during normal gestation in various populations. These studies have reported different uterine cervical length in pregnancy in the same weeks and months.[6,12,13,14,15,16] On the other hand, the cervical length can be affected by parity, age, gestational age, race, and populations.[14,17] Therefore, it is appropriate to define a nomogram of mean uterine cervical lengths and their standard deviations for every week of gestation in order to detect deviations from the normal range clinically, determine preterm labor, perform cerclage, prevent unnecessary tocolysis, reduce time of hospitalization, and to indicate lung maturation treatment more precisely based on the uterine cervical length as early as possible.
To the best of our knowledge, there is no study on the normal pattern of change in uterine cervical length during normal pregnancy in the center of Iran. On the other hand, reference ranges established throughout gestation might be more useful than a single cut-off value for more efficient prevention and management of preterm birth. Therefore, this study constructed charts and evaluated cervical length means and percentiles for uterine cervical length at 8 to 38 weeks of the normal gestation in the center of Iran (Isfahan) by transabdominal ultrasound device.
MATERIALS AND METHODS
This study was conducted between March 2012 and February 2013. Pregnant volunteer subjects (N = 30 for each week) were recruited based on the following criteria. The exclusion criteria were major fetal abnormalities, regular pain, a history of ruptured membranes, abruption placenta, uterine structural abnormalities, cervical cerclage, placenta previa, polyhydramnios.[1,7,10,16] Abdominal ultrasonography uterine cervical length was performed at 8 to 38 weeks’ gestation on 930 asymptomatic pregnant women at the time of each routine pregnancy ultrasound examination. In our study the cases were not followed up. Transabdominal ultrasound was performed using a Voluson 730 expert machine of GE Company. A 3.5-5 MHz probe was used to determine the uterine cervical length. The bladder of participants was semi distended to displace the fetal head superiorly. The cervix was viewed as an echogenic line extending from the internal to external os. All measurements were done three times for at least 5 min and measured by a single radiologist expert in this field in a sagittal plane and a mean of the three times was taken. The study was approved by Isfahan University of Medical Sciences Ethics Committee and all volunteers gave their written consent.
All data for determining uterine cervical length and percentiles were analyzed with the use of SPSS 20 (SPSS Inc., Chicago, IL, USA) statistical package. The uterine cervical length measurements were expressed as mean ± SD, range, and percentiles. Regression analysis was used for the mean uterine cervical length and weeks of gestation assessments. For practical use of uterine cervical length charts, we interpolated our data. The mean, the 5th and 95th percentiles were fitted by a quadratic curve. P < 0.05 was considered statistically significant.
RESULTS
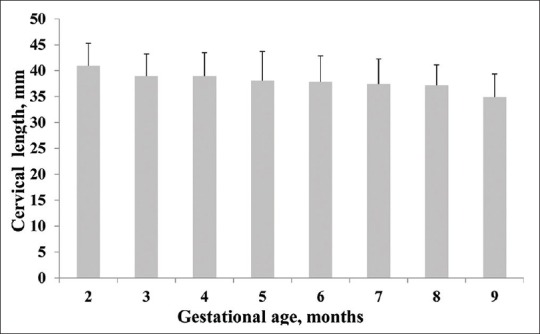
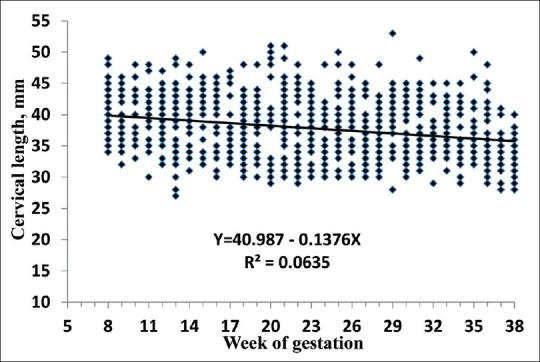
In this study, the mean maternal age of subjects was 28.9 ± 4.7 years. Table 1 and Figure 1 show the relationship between the uterine cervical length and weeks’ gestation and months in normal pregnancy, respectively. Also, the regression line between uterine cervical length and weeks of gestation is shown in Figure 2. There is a spontaneous shortening in the pregnant women cervix from the beginning to the termination of pregnancy. The mean uterine cervical length exhibited minimal changes from 10 to 24 weeks for most pregnant volunteer subjects in this study. Also, the shortening was seen in pregnant volunteer subjects at 33 to 38 weeks’ gestation [Table 1 and Figure 1]. The average shortening of the uterine cervical length between the second and the ninth months was 14.82% (P < 0.05). Also, the mean of uterine cervical length in trimesters 1, 2 and 3 were 39.30 ± 4.33, 38.28 ± 5.13 and 36.58 ± 4.58, respectively [Figure 3]. In addition, the minimum and maximum length of cervix in each trimesters were 27 and 49 mm, 29 and 51 mm, 28 and 53 mm, respectively. The third trimester showed a significant reduction (P < 0.05) in uterine cervical length compared to the first and second trimesters (6.92% and 4.44%, respectively). Also, the third trimester showed a significant reduction (P < 0.05) compared to the second trimester. Cervical length measurements corresponding to the 5th, 10th, 50th, 90th, and 95th centiles against gestational age are shown in Figure 4. Also, the mean, the 5th and 95th percentiles were fitted by a quadratic curve [Figure 5].
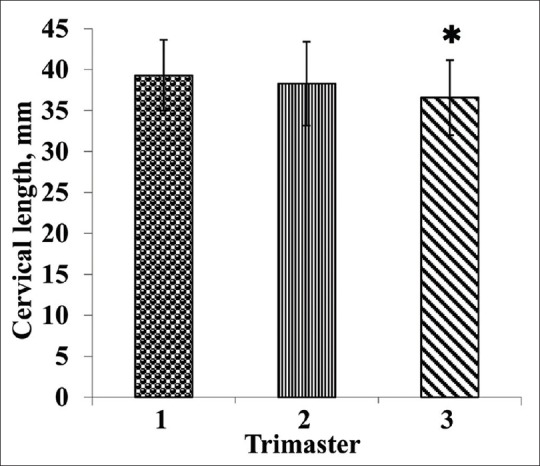
Table 1.
Descriptive statistics of uterine cervical length measurements across gestational age
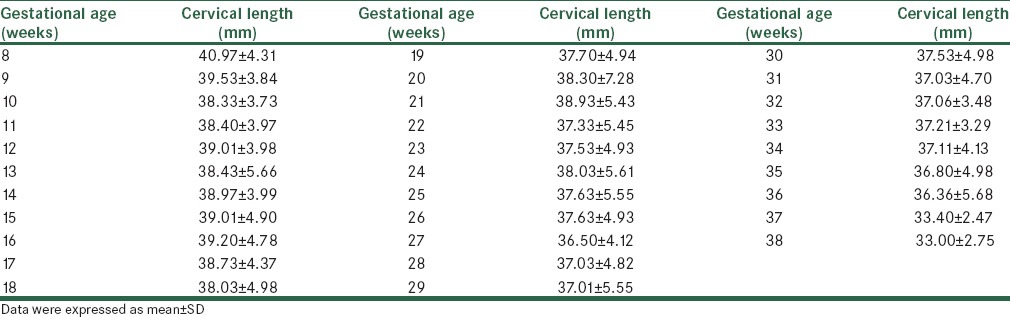
Figure 1.
The mean uterine cervical length changes from 2 to 9 months. Data were expressed as mean ± SD
Figure 2.
Relationship between uterine cervical length and week of gestation
Figure 3.
The mean uterine cervical length in trimesters. Data were expressed as mean ± SD. *P<0.05 compared with the corresponding values in the first and second trimesters
Figure 4.
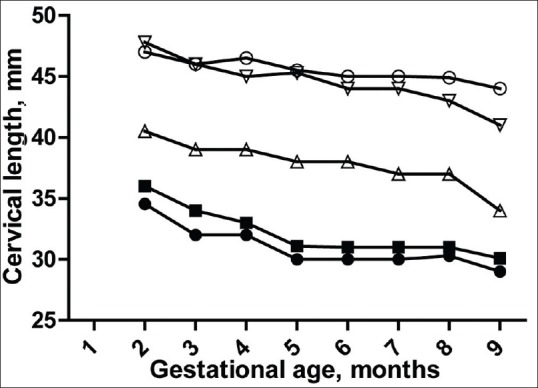
Charts for uterine cervical length at the 5th (•), 10th (▄), 50th (Δ), 90th (∇), and 95th (○) percentiles across gestation
Figure 5.
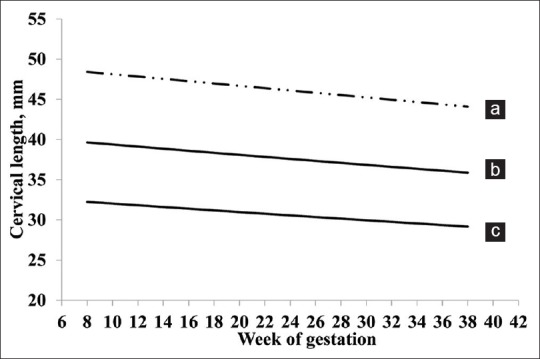
Interpolation quadratic curves for mean (B), the 5th (C) and 95th (A) percentiles
DISCUSSION
Transabdominal ultrasound is an original method for visualizing the gravid cervix although there are limitations for the abdominal approach, including the following: (a) the apparent artificial lengthening of the cervix resulting from the patient's filled bladder, and (b) the difficulty of visualizing a shortened cervix. Despite these limitations, several recent studies[3,5] have reported the clinical benefit of transabdominal assessment of uterine cervical length[7] in that it is accurate and more acceptable to some patients than cervical evaluation via a transvaginal probe. Additionally, transabdominal assessment of uterine cervical length is less invasive, less cumbersome, and well accepted by patients compared with transvaginal assessment.[7]
In recent decade, large studies with measurements of the uterine cervical length were performed on asymptomatic women in different weeks of gestation. Nevertheless, there are different cut off levels and different definitions of preterm birth in different populations. Preterm delivery is a major cause of neonatal morbidity and mortality, especially, in the United States.[18] Today, a large body of evidence indicates that uterine cervical length early in pregnancy is an important predictor of subsequent preterm delivery.[19] Cervical lengths <25 mm at 22–24 weeks of gestation considered as prediction of preterm delivery.[20] The results of this study confirmed previous findings that uterine cervical length changes throughout pregnancy are indicative of physiological decrease.[8] In this study, cervical length at 20 weeks’ gestation was 38.30 ± 7.28 mm [Table 1] which is in accordance with 38.50 ± 8.00 mm reported by Hibbard et al.[21] Also, Iams et al.[22] reported mean cervical length to be 35.2 ± 8.3 mm at 24 weeks but in this study it was 37.03 ± 4.62 mm. On the other hand, Andersen et al., reported that a cervix of less than 39 mm before 30 weeks’ gestation was a significant risk factor for early delivery[19] whereas in this study cervical length at 30 weeks’ gestation was 37.53 ± 4.98 mm [Table 1]. Also, Ozdemir et al., reported that the mean uterine cervical lengths at 10-14 and 20-24 weeks’ gestation were 40.5 and 37.1mm, respectively[23] whereas in our study values were 38.92 and 37.82 mm, respectively. Additionally, Carvalho et al.,[6] measured the uterine cervical length transvaginally in a longitudinal study of 529 women at 11 to 14 and 22 to 24 weeks’ gestation. They reported the mean uterine cervical length 42.4 and 38.6 mm, respectively whereas in our study values were 38.82 and 37.29 mm, respectively [Table 1]. In another study Carvalho et al.,[6] observed a 3.8 mm shortening of the cervix from the first to the second measurement but in our study shortening of the cervix from the first to the second was 1.02 mm. In our study, the mean of uterine cervical length in trimesters 1, 2 and 3 were 39.30 ± 4.33, 38.28 ± 5.13 and 36.58 ± 4.58, respectively [Figure 3]. In another study, median uterine cervical length in the second trimester was reported to be 35-38 mm which is consistent with our results.[24] On the other hand, in the current study the cervical shortening in trimester 3 was 2.72 mm compared to trimester 1 which is close to value 3.1 mm reported by Ozdemir et al.,[23] Additionally, Iams et al.,[22] reported the 10th and 5th percentiles 26 and 22 mm at 20 weeks whereas in our study values were 31 and 30 mm, respectively [Figure 4]. Also, Hibbard et al.,[21] reported that the 10th and 5th percentiles of uterine cervical length at 20 weeks were 30 and 27 mm, respectively. Besides, based on large number of observational studies in low-risk populations, it proposed that the 50th percentile of the cervical length is 35 mm at 24 weeks of gestation,[9] which is consistent with our results in the same week (37 mm at 24 weeks). In a recent study in Greece,[16] Souka et al., reported that the cervical length exhibits minimal changes from 11 to 24 weeks’ gestation which is in line with our results in the same weeks. As mentioned before, the uterine cervical length can be affected by parity, age, gestational age, race, and populations.[14,17] Therefore, the observed differences for uterine cervical length and percentiles in different studies may be due to maternal characteristics, age, gestational age, race, and populations. Therefore, it seems that we need different charts for uterine cervical length throughout gestation in various populations based on maternal characteristics, age, gestational age, race and etc. These charts can be used for observing women at high risk for preterm delivery and for clearly identifying a significant deviation or decline in the centiles for these subjects.
CONCLUSION
Our study provides new charts and reference values for normal uterine cervical length throughout gestation based on a large sample in the center of Iran. A chart established for uterine cervical length throughout gestation might be more useful than a single cut-off value for more efficient prevention and management of preterm birth. We should remember, however, that different pathways can lead to preterm delivery. Therefore, measurement of the cervix should never be the only assessment in a patient with the risk of preterm delivery.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Slager J, Lynne S. Assessment of cervical length and the relationship between short cervix and preterm birth. J Midwifery Womens Health. 2012;57(Suppl 1):S4–11. doi: 10.1111/j.1542-2011.2012.00209.x. [DOI] [PubMed] [Google Scholar]
- 2.Vaisbuch E, Romero R, Mazaki-Tovi S, Erez O, Kusanovic JP, Mittal P, et al. The risk of impending preterm delivery in asymptomatic patients with a nonmeasurable cervical length in the second trimester. Am J Obstet Gynecol. 2010;203:446.e1–9. doi: 10.1016/j.ajog.2010.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pandis GK, Papageorghiou AT, Ramanathan VG, Thompson MO, Nicolaides KH. Preinduction sonographic measurement of cervical length in the prediction of successful induction of labor. Ultrasound Obstet Gynecol. 2001;18:623–8. doi: 10.1046/j.0960-7692.2001.00580.x. [DOI] [PubMed] [Google Scholar]
- 4.Roman H, Verspyck E, Vercoustre L, Degre S, Col JY, Firmin JM, et al. Does ultrasound examination when the cervix is unfavorable improve the prediction of failed labor induction? Ultrasound Obstet Gynecol. 2004;23:357–62. doi: 10.1002/uog.1008. [DOI] [PubMed] [Google Scholar]
- 5.Berghella V, Tolosa JE, Kuhlman K, Weiner S, Bolognese RJ, Wapner RJ. Cervical ultrasonography compared with manual examination as a predictor of preterm delivery. Am J Obstet Gynecol. 1997;177:723–30. doi: 10.1016/s0002-9378(97)70259-x. [DOI] [PubMed] [Google Scholar]
- 6.Carvalho MH, Bittar RE, Brizot ML, Maganha PP, Borges da Fonseca ES, Zugaib M. Cervical length at 11-14 weeks’ and 22-24 weeks’ gestation evaluated by transvaginal sonography, and gestational age at delivery. Ultrasound Obstet Gynecol. 2003;21:135–9. doi: 10.1002/uog.32. [DOI] [PubMed] [Google Scholar]
- 7.Saul LL, Kurtzman JT, Hagemann C, Ghamsary M, Wing DA. Is transabdominal sonography of the cervix after voiding a reliable method of cervical length assessment? J Ultrasound Med. 2008;27:1305–11. doi: 10.7863/jum.2008.27.9.1305. [DOI] [PubMed] [Google Scholar]
- 8.Silva SV, Damiao R, Fonseca EB, Garcia S, Lippi UG. Reference ranges for cervical length by transvaginal scan in singleton pregnancies. J Matern Fetal Neonatal Med. 2010;23:379–82. doi: 10.3109/14767050903177169. [DOI] [PubMed] [Google Scholar]
- 9.Hoesli I, Tercanli S, Holzgreve W. Cervical length assessment by ultrasound as a predictor of preterm labour−is there a role for routine screening? Bjog. 2003;110(Suppl 20):61–5. doi: 10.1016/s1470-0328(03)00032-6. [DOI] [PubMed] [Google Scholar]
- 10.Salomon LJ, Diaz-Garcia C, Bernard JP, Ville Y. Reference range for cervical length throughout pregnancy: Non-parametric LMS-based model applied to a large sample. Ultrasound Obstet Gynecol. 2009;33:459–64. doi: 10.1002/uog.6332. [DOI] [PubMed] [Google Scholar]
- 11.To MS, Skentou C, Liao AW, Cacho A, Nicolaides KH. Cervical length and funneling at 23 weeks of gestation in the prediction of spontaneous early preterm delivery. Ultrasound Obstet Gynecol. 2001;18:200–3. doi: 10.1046/j.1469-0705.2001.00437.x. [DOI] [PubMed] [Google Scholar]
- 12.Crane JM, Hutchens D. Transvaginal sonographic measurement of cervical length to predict preterm birth in asymptomatic women at increased risk: A systematic review. Ultrasound Obstet Gynecol. 2008;31:579–87. doi: 10.1002/uog.5323. [DOI] [PubMed] [Google Scholar]
- 13.Demirci O, Unal A, Demirci E, Sozen H, Akdemir Y, Boybek E, et al. Sonographic measurement of cervical length and risk of preterm delivery. J Obstet Gynaecol Res. 2011;37:809–14. doi: 10.1111/j.1447-0756.2010.01440.x. [DOI] [PubMed] [Google Scholar]
- 14.Guzman ER, Mellon C, Vintzileos AM, Ananth CV, Walters C, Gipson K. Longitudinal assessment of endocervical canal length between 15 and 24 weeks’ gestation in women at risk for pregnancy loss or preterm birth. Obstet Gynecol. 1998;92:31–7. doi: 10.1016/s0029-7844(98)00120-3. [DOI] [PubMed] [Google Scholar]
- 15.Hernandez-Andrade E, Romero R, Ahn H, Hussein Y, Yeo L, Korzeniewski SJ, et al. Transabdominal evaluation of uterine cervical length during pregnancy fails to identify a substantial number of women with a short cervix. J Matern Fetal Neonatal Med. 2012;25:1682–9. doi: 10.3109/14767058.2012.657278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Souka AP, Papastefanou I, Michalitsi V, Salambasis K, Chrelias C, Salamalekis G, et al. Cervical length changes from the first to second trimester of pregnancy, and prediction of preterm birth by first-trimester sonographic cervical measurement. J Ultrasound Med. 2011;30:997–1002. doi: 10.7863/jum.2011.30.7.997. [DOI] [PubMed] [Google Scholar]
- 17.Scheerer L, Bartolucci L. Ultrasound evaluation of the cervix. In: Callen PW, editor. Ultrasonography in obstetrics and gynecology. 4th ed. Philadelphia, PA: WB Saunders; 2000. [Google Scholar]
- 18.Guyer B, Hoyert DL, Martin JA, Ventura SJ, MacDorman MF, Strobino DM. Annual summary of vital statistics−1998. Pediatrics. 1999;104:1229–46. doi: 10.1542/peds.104.6.1229. [DOI] [PubMed] [Google Scholar]
- 19.Andersen HF, Nugent CE, Wanty SD, Hayashi RH. Prediction of risk for preterm delivery by ultrasonographic measurement of cervical length. Am J Obstet Gynecol. 1990;163:859–67. doi: 10.1016/0002-9378(90)91084-p. [DOI] [PubMed] [Google Scholar]
- 20.Di Tommaso M, Berghella V. Cervical length for the prediction and prevention of preterm birth. Expert Rev Obstet Gynecol. 2013;8:345–55. [Google Scholar]
- 21.Hibbard JU, Tart M, Moawad AH. Cervical length at 16-22 weeks’ gestation and risk for preterm delivery. Obstet Gynecol. 2000;96:972–8. doi: 10.1016/s0029-7844(00)01074-7. [DOI] [PubMed] [Google Scholar]
- 22.Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334:567–72. doi: 10.1056/NEJM199602293340904. [DOI] [PubMed] [Google Scholar]
- 23.Ozdemir I, Demirci F, Yucel O, Erkorkmaz U. Ultrasonographic cervical length measurement at 10-14 and 20-24 weeks gestation and the risk of preterm delivery. Eur J Obstet Gynecol Reprod Biol. 2007;130:176–9. doi: 10.1016/j.ejogrb.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 24.Norman JE. Preterm labour. Cervical function and prematurity. Best Pract Res Clin Obstet Gynaecol. 2007;21:791–806. doi: 10.1016/j.bpobgyn.2007.03.002. [DOI] [PubMed] [Google Scholar]


