Abstract
Background:
The contact allergic reactions from p-phenylenediamine (PPD) in hair dyes vary from mild contact dermatitis to severe life- threatening events (angioedema, bronchospasm, asthma, renal impairment).
Objectives:
To study the clinical patterns and PPD contact sensitivity in patients with hair-dye dermatitis.
Materials and Methods:
Eighty (M:F 47:33) consecutive patients aged between 18 and 74 years suspected to have contact allergy from hair dye were studied by patch testing with Indian Standard Series including p-phenylenediamine (PPD, 1.0% pet).
Results:
54 Fifty-four (M:F 21:33) patients showed positive patch tests from PPD. Eight of these patients also showed positive patch test reaction from fragrance mix, thiuram mix, paraben mix, or colophony. Fifty-seven (71%) patients affected were aged older than 40 years. The duration of dermatitis varied from < 1 month to > 1 year with exacerbation following hair coloring. Forty-nine patients had dermatitis of scalp and/or scalp margins and 23 patients had face and neck dermatitis. Periorbital dermatitis, chronic actinic dermatitis, and erythema multiforme-like lesions were seen in 4, 2, and 1 patients, respectively.
Conclusions:
Hair dyes and PPD constitute a significant cause of contact dermatitis. There is an urgent need for creating consumer awareness regarding hair-dyes contact sensitivity and the significance of performing sensitivity testing prior to actual use.
Keywords: Contact dermatitis, cosmetic dermatitis, hair colors, hair dye, periorbital dermatitis, p-phenylenediamine, PPD sensitization, periorbital dermatitis, scalp dermatitis
INTRODUCTION
Hair dyes are perhaps among the most commonly used cosmetics by elderly and the young alike - for concealing gray hair by the former or just for a fashion statement by the latter. The popularity of hair colouring can be gauged from the fact that the median age for debut was 16 years and nearly 75% of women and 18% of men had dyed their hair at some point in their lives according to a Danish population-based study.[1] This rising trend of hair colouring has resulted in an increased prevalence of hair dye-associated adverse effects accounting for 5.3% of Danish persons who dyed their hair.[1] Similarly, 42% of the respondents reported adverse reactions from use of hair dyes and the mean age of hair dye debut was 27 years in an Indian study.[2] Hair dyes include a variety of coloring agents such as 2,7-naphthalenediol, 2-aminomethyl-p-aminophenol hydrochloride, 2-chloro-p-phenylenediamine, N-phenyl-p-phenylenediamine, and o-aminophenol, p-aminophenol.[3] Although all these agents can cause allergic contact reactions, p-phenylenediamine (PPD) remains the most commonly implicated agent for the contact sensitivity. It is an arylamine derivative first described by Hoffmann in 1863. It is an effective compound for hair dyes due to its low molecular weight, high protein- binding capacity, and ability to penetrate the hair shaft. Apart from being a common constituent in varying concentrations of nearly 70% of the hair colorants available worldwide, it is also present in dyes for henna tattoos, textiles, leather and fur, and black rubbers. Being a member of 1,4-substituted benzenes, it cross-reacts with para-amino benzoic acid (PABA), sulphonamides, para-amino salicylic acid, ester anesthetics, thiazides, sesquiterpene-lactone mix, and azo dyes.[4] It is a potent contact sensitizer even in low concentration and considered a best indicator and useful patch test screening allergen for hair dye dermatitis.[5] The reported prevalence of positive patch test reactions to PPD among dermatitis patients is 4.4% in Asia, 4.1% in Europe, 6.0% in North America, and 11.5% in India.[6,7] The clinical features of hair dye dermatitis vary from mild contact dermatitis localized to one body site (hand dermatitis) or disseminated generalized dermatitis to severe life-threatening complications such as contact urticaria/angioedema, rhinitis/bronchospasm/asthma, and renal toxicity.[8,9] The most common clinical presentations include contact dermatitis localized to sites of contact or photoexposed skin, periorbital dermatitis, airborne contact dermatitis, hand dermatitis, and rarely erythema multiforme-like lesions. In this pilot study, we present our clinico-epidemiological observations and patch test results of PPD contact sensitivity in patients suspected to have hair dye dermatitis.
MATERIALS AND METHODS
Eighty (M: F 47:33) consecutive patients suspected to have hair dye allergy were enrolled for the study after obtaining informed consent. Pregnant or lactating women, and children younger than 18 years were excluded. Patients having acute dermatitis were patch tested after control of their dermatitis, when they were off systemic corticosteroids or the dose of prednisolone was <20 mg/day. Institutional Protocol Review Board and Institutional Ethics Committee approved the study. Details about age, gender, occupation, personal or family history of atopy (nasobronchial allergy, asthma, childhood eczema), use of hair dye and its duration, onset, duration, and distribution of dermatitis were noted. The enrolled patients were patch tested by Finn chambers method with Indian standard patch test series including PPD (1.0% pet) recommended by Contact Dermatitis and Occupational Dermatoses Forum of India.[10] Patches were applied on the upper back and the patients were asked to return for results after 48 hrs (D2) and 72 hrs (D3). The results were graded according to the International Contact Dermatitis Research Group criteria.[11] Only reactions persisting on D3 were considered positive for final analysis. Relevance of a positive patch test results was determined clinically. Side effects such as adhesive tape reaction, discomfort and itching, flare of dermatitis, angry back phenomenon, active sensitization, and pigment alteration at test site, when they occurred, were recorded.
RESULTS AND OBSERVATIONS
The study included 47 (58.8%) males aged between 19 and 74 years and 33 (41.2%) females aged between 18 to 74 years. Their baseline characteristics are tabulated in Table 1. The majority, that is, 57 (71%) patients were older than 40 years, while whereas 23 (29%) were younger than 40 years, the youngest being a 19-year-old male. Forty six (57.5%) patients were from an urban background and 34 (42.5%) patients belonged to a rural background. Among the males, 21 (44.7%) were office goers, 9 (19.1%) shopkeepers, and 6 (12.7%) defence personnel. Among females 30 (90.9%) were housewives and 3 (9.09%) were students. Eighteen (33.3%) patients had a history of atopy. The duration of hair dye usage varied from less than one month in 11 (13.8%) to more than three years in 17 (21.2%) patients. Other 52 (65%) patients were using hair dyes for variable period of 1 month to 3 years. The duration of dermatitis varied from <1 month in 11 (13.8%) patients and >1 year in 27 (33.7%) patients; forty-two (52.5%) patients had dermatitis between one month and one year. Clinically, characteristic acute (erythematous, edematous, oozy, crusted eczematous plaques), subacute and chronic dermatitis (hyperpigmented, lichenified eczematous lesions) involving multiple sites such as scalp, scalp margins, forehead, eyelids, beard, neck, upper back, and/or hands was observed in all cases. Additionally, the most common patterns of hair dye dermatitis observed were contact dermatitis localized to scalp and/or scalp margins in 49, followed by dermatitis of face (including beard and periorbital skin) and neck in 23 and hands and/or feet in 12 patients, respectively. Other patterns observed were airborne contact dermatitis in 9, hand dermatitis in 5, eyelid dermatitis in 4, and discoid dermatitis and disseminated dermatitis in 1 (1.85%) patient each. One patient had generalized diffuse dermatitis and another patient showed erythema multiforme-like lesions. None of the patients had followed the manufacturer's instructions to perform sensitivity testing prior to applying the hair dye.
Table 1.
Baseline characteristics of the patients studied
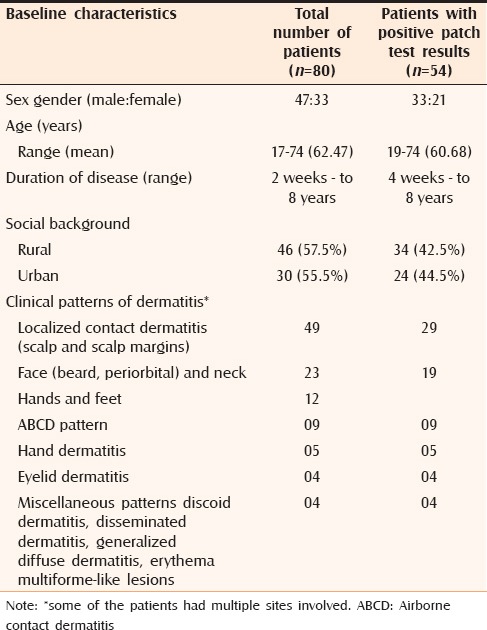
Only 54 (67.5%) patients comprising 33 (61%) males and 21 (39%) females aged between of 19 and 74 years showed positive results to patch testing with PPD. Other 3 patients showed irritant reactions that subsided on day 3 post application. Eight of these patients also showed positive patch test reaction to other allergens; fragrance mix in 5, thiuram mix in 3, and paraben mix and colophony in 1 patient each. Thirty (55.5%) patients belonged to urban populations and 24 (44.5%) patients were from rural background. The common clinical patterns noted were: (a) Dermatitis localized to the scalp, face, neck or hands, (b) airborne dermatitis, (c) chronic actinic dermatitis (actinic reticuloid), (d) generalized diffuse dermatitis, and (e) erythema multiforme-like dermatitis [Figures 1 to 5].
Figure 1.

PPD contact dermatitis localized to face, cheeks, nose, neck, and dorsal hands in photodistributed pattern
Figure 5.

PPD induced erythema multiforme-like lesions over (a) upper back and (b) palms. Patch test showed 3+ reaction to PPD
Figure 2.

PPD contact dermatitis localized to eyelids and periorbital skin
Figure 3.

PPD contact dermatitis localized over neck. She also had dermatitis involving the scalp skin
Figure 4.
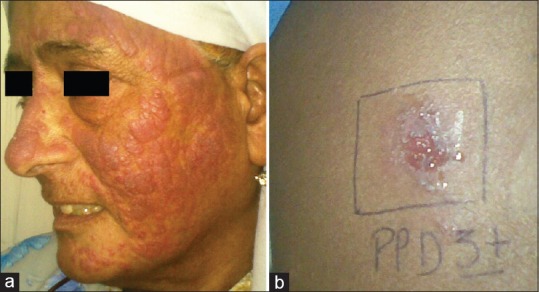
(a) Chronic actinic dermatitis (actinic reticuloid) due to PPD. (b) Patch test shows 3+ reaction to PPD
DISCUSSION
The use of hair colorants has increased exponentially over the last few decades due to increased societal pressure and changing fashion trends. Over the years, the colouring agents have diversified in nature with the arrival of oxidative hair dyes that include many synthetic and natural agents. The more commonly used hair dye agents include resorcinol, henna, hydroquinone, lead acetate, m-aminophenol, N-phenyl-p-phenylenediamine, o-aminophenol, p-aminophenol, and PPD or related para-amino compounds such as toluene-2,5-diamine sulfate.[10,11] However, PPD remains the most common contact sensitizer across studies.[12,13,14] Nearly 5% of 21,515 individuals were allergic to PPD in a multicentric European study.[10] Similarly, PPD was the commonest sensitizer among cosmetics in two separate Indian studies.[13,14] Hairdressers and textile dye workers are particularly at risk and have high prevalence of PPD contact dermatitis varying between of 15% and 45% or as high as 58% because of high occupational exposure.[15,16,17] Apart from hair colorants, sensitization may also occur from PPD in textile or fur dyes, black rubber, temporary tattoos, and photocopying and printing inks. Similarly, hair dye dermatitis is observed among urban dwellers more often than in their rural counterparts; a prevalence of 84% versus 16% among urban versus rural population has been observed in a previous study.[13] This trend may be because of easy availability of hair dyes, increased awareness, and peer pressure to look younger among the urban population. Sensitization from PPD can occur at any age including among children as it depends mainly upon exposure to the allergen. The weighted average of PPD sensitization in the general population is estimated to be 1.0%.[18] However, the prevalence of PPD sensitivity varies according to cultural and occupational practices and a higher prevalence is seen in Asia (2%–12%), particularly among Asian males.[7,19] Most cases occur in middle-aged individuals between 30 and 50 years of age and males are affected two times more than the females.[7,20] This increased prevalence in middle-aged people has been attributed to the frequent use of hair dye in order to camouflage their greying hair. Higher sensitization to hair dye among males is probably due to the more frequent applications that are required for facial (beard) hair as compared to scalp hair. All our patients in the study had more or less similar demographic characteristics.
Clinically, hair dye dermatitis can present as both irritant dermatitis and allergic contact dermatitis. It may also cause severe clinical contact reactions ranging from anaphylaxis to oedema of the scalp, face, and eyelids. Scalp and scalp margins, and beard skin are the reported sites that are commonly affected due to hair dye usage, while hands and other body sites may be affected among persons not using gloves while dying hair. Mild to moderate contact reactions such as erythema, oozing, and ulceration typically at the scalp margin, and on the ears and neck are common as a result of direct contact.[21,22] Ho et al.[23] observed that hair dye dermatitis primarily involved the face and neck (28%), and hands (25%), whereas widespread dermatitis occurred in 17% of patients. Airborne contact dermatitis, irritant contact dermatitis, photocontact dermatitis, periorbital eczema, hand eczema, lichenoid lesions, and lichen planus pigmentosus-like pigmentary changes were the commonly observed clinical patterns of hair dye dermatitis, whereas contact leukcoderma, contact urticaria, lymphomatoid papulosis, erythema multiforme-like or prurigo nodularis-like lesions, and anaphylaxis have occurred atypically with PPD.[22,23,24,25,26] Localized contact dermatitis was observed in nearly all our patients, particularly involving the scalp and/or scalp margin in 49 patients, face, beard, and periorbital skin in 23, and hands and feet in 12 patients. Uncommon patterns such as airborne contact dermatitis (9 patients), hand dermatitis (5 patients), eyelid dermatitis (4 patients), disseminated dermatitis and erythema multiforme-like lesions (1 patient each) were also observed in this series. Although PPD is not considered photosensitizing, dermatitis localized to photoexposed skin and chronic actinic dermatitis (actinic reticuloid) in a few patients suggests its possible photosensitizing potential. It is also possible that persistence of allergen and photoaggravation of dermatitis is responsible for photolocalization of PPD induced dermatitis in some individuals. Contact sensitivity to fragrance mix, colophony, paraben mix, and thiuram mix, observed in eight patients was perhaps due to prior sensitisation as they are present in most topical medications, cosmetics, perfumes, and pharmaceuticals.
The exact nature of the haptens associated with PPD sensitivity remains poorly understood. Prohaptens and their metabolites in the skin, particularly the p-benzoquinone, are considered responsible for its allergenicity and cross-reactivity. Another postulation is that Bandrowski's base, a trimer of PPD formed on exposure, is perhaps responsible for its allergenicity.[27] However, patch testing with these agents individually is negative in a sizeable population of patients who had tested positive to for PPD. Recently, benzoquinone diamine intermediates have been implicated in its allergenicity.[28] A genetic polymorphism in the cutaneous metabolism of PPD too has been suggested to explain why only a few persons using hair dyes develop contact sensitivity or variable allergic responses from to it.[29] Penchalaiah et al.[14] reported a personal history of atopy in 24% of their patients with cosmetic contact sensitivity. Atopic individuals are perhaps at an enhanced risk of for cosmetic contact sensitivity because of increased allergen penetration through impaired skin barrier. A personal history of atopy was observed in 18 (33%) patients in our study.
Contact sensitivity from PPD is becoming a prevalent health problem. Strict regulations are required to regulate its concentration in cosmetic products. The European Union Cosmetic Directive allows a maximum concentration of 6% PPD in hair dyes, while the Bureau of Indian Standards has set a maximum permissible limit of 30% and not less than 3% PPD after dilution of the powder form and a maximum of 4% and not less than 1.2% after dilution of the oxidation liquid type. However, many manufacturers fail to comply with these standards, and a strict legislation is perhaps needed for adherence to safe limits of PPD in hair dyes. It is also desirable that manufacturers print directions in bold text over the product package regarding safe use of the hair dye. There is also an urgent need to increase awareness among consumers regarding the adverse effects of hair dyes, the available safer alternatives, and the significance of performing sensitivity testing prior to actual use, in adherence of usage instructions.
Limitations
The hair dyes usually have two separate components, the colorant and the developer that are mixed before application. Other than PPD, many other chemical agents are used for the two components. Any of them could have caused allergic reactions. We did not patch test these agents in our study and that might have been responsible for negative patch test results in 26 of our patients. Unavailability of hair dye allergens other than PPD, the small number of patients, and not testing with patient's own hair colorant or other cosmetics may have resulted in our missing some cases of compound allergy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Søsted H, Hesse U, Menné T, Andersen KE, Johansen JDSosted H, Hesse U, Menne T, Andersen KE, Johansen JD. Contact dermatitis to hair dyes in an adult Danish population-: An interview-based study. Br J Dermatol. 2005;153:132–5. doi: 10.1111/j.1365-2133.2005.06588.x. [DOI] [PubMed] [Google Scholar]
- 2.Patel D, Narayana S, Krishnaswamy B. Trends in use of hair dye: A cross-sectional study. I Int J Trichologynt J Trichol. 2013;5:140–3. doi: 10.4103/0974-7753.125610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sosted H, Basketter DA, Estrada E, Johansen JD, Patlewicz GY. Ranking of hair dye substances according to predicted sensitization potency-quantitative structure-activity relationships. Contact Dermatitis. 2004;51:241–54. doi: 10.1111/j.0105-1873.2004.00440.x. [DOI] [PubMed] [Google Scholar]
- 4.Xie Z, Hayakawa R, Sugiura M, Kojima H, Konishi H, Ichihara G, Takeuchi Y, et al. Experimental study on skin sensitization potencies and cross-reactivities of hair-dye-related chemicals in guinea pigs. Contact Dermatitis. 2000;42:270–5. doi: 10.1034/j.1600-0536.2000.042005270.x. [DOI] [PubMed] [Google Scholar]
- 5.Koopmans AK, Bruynzeel DP. Is PPD a useful screening agent? Contact Dermatitis. 2003;48:89–92. doi: 10.1034/j.1600-0536.2003.480207.x. [DOI] [PubMed] [Google Scholar]
- 6.Thyssen JP, White JM. Thyssen JP, White JM, editors. European Society of Contact Dermatitis. Epidemiological data on consumer allergy to p-phenylenediamine. Contact Dermatitis. 2008;59:327–43. doi: 10.1111/j.1600-0536.2008.01427.x. [DOI] [PubMed] [Google Scholar]
- 7.Sharma VK, Chakrabarti A. Common contact sensitizers in Chandigarh, India. A study of 200 patients with the European standard series. Contact Dermatitis. 1998;38:127–31. doi: 10.1111/j.1600-0536.1998.tb05677.x. [DOI] [PubMed] [Google Scholar]
- 8.Helaskoski E, Suojalehto H, Virtanen H, Airaksinen L, Kuuliala O, Aalto-Korte K, et al. Occupational asthma, rhinitis, and contact urticaria caused by oxidative hair dyes in hairdressers. Ann Allergy Asthma Immunol. 2014;112:46–52. doi: 10.1016/j.anai.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 9.Barrientos N, Abajo P, de Vega MM, Dominguez J. Erythema multiforme-like eruption following allergic contact dermatitis in response to para-phenylenediamine in a temporary henna tattoo. Int J Dermatol. 2014;53:e348–509. doi: 10.1111/ijd.12285. [DOI] [PubMed] [Google Scholar]
- 10.Sharma VK, Sethuraman G, Garg T, Verma KK, Ramam M. Patch testing with the Indian standard series in New Delhi. Contact Dermatitis. 2004;51:319–21. doi: 10.1111/j.0105-1873.2004.0459k.x. [DOI] [PubMed] [Google Scholar]
- 11.Wilkinson DS, Fregert OS, Magnusson B, Bandmann HJ, Calnan CD, Cronin E, et al. Terminology of contact dermatitis. Acta Derm Venereol. 1970;50:287–92. [PubMed] [Google Scholar]
- 12.Thyssen JP, Andersen KE, Bruze M, Diepgen T, Giménez-Arnau AM, Gonçalo M, Gimenez-Arnau AM, Goncalo M, et al. p-phenylenediamine sensitization is more prevalent in central and southern European patch test centers than in Scandinavian: Results from a multicentre study. Contact Dermatitis. 2009;60:314–9. doi: 10.1111/j.1600-0536.2009.01547.x. [DOI] [PubMed] [Google Scholar]
- 13.Dogra A, Minocha YC, Kaur S. Adverse reactions to cosmetics. Indian J Dermatol Venereol Leprol. 2003;69:165–7. [PubMed] [Google Scholar]
- 14.Penchalaiah K, Handa S, Lakshmi SB, Sharma VK, Kumar B, Penchalaiah K, Handa S, Lakshmi B. Sensitizers commonly causing contact dermatitis from cosmetics. Contact Dermatitis. 2000;43:3110–3. [PubMed] [Google Scholar]
- 15.Uter W, Lessmann H, Geier J, Schnuch A. Contact allergy to ingredients of hair cosmetics in female hairdressers and clients-an 8-year analysis of IVDK data. Contact Dermatitis. 2003;49:236–40. doi: 10.1111/j.0105-1873.2003.0233.x. [DOI] [PubMed] [Google Scholar]
- 16.Nettis E, Marcandrea M, Colanardi MC, Paradiso MT, Ferrannini A, Tursi ANettis E, Marcandrea M, Colanardi MC, Paradiso MT, Ferrannini A, Tursi A. Results of standard series patch testing in patients with occupational allergic contact dermatitis. Allergy. 2003;58:1304–7. doi: 10.1046/j.1398-9995.2003.00346.x. [DOI] [PubMed] [Google Scholar]
- 17.Valks R, Conde-Salazar L, Malfeito J, Ledo SValks R, Conde-Salazar L, Malfeito J. Contact dermatitis in hairdressers, 10 years later: Patch-test results in 300 hairdressers (1994 to 2003) and comparison with previous study Contact dermatitis in hairdressers. Dermatitis. 2005;16:28–31. [PubMed] [Google Scholar]
- 18.de Groot AC. Contact allergy to cosmetics: Causative ingredients. Contact Dermatitis. 1987;17:26–34. doi: 10.1111/j.1600-0536.1987.tb02640.x. [DOI] [PubMed] [Google Scholar]
- 19.Basketter DA, Duangdeeden I, Gilmour NJ, Kullavanijaya P, McFadden JP. Prevalence of contact allergy in an adult Thai population. Contact Dermatitis. 2004;50:128–9. [Google Scholar]
- 20.Handa S, De D, Mahajan R. Epidemiological trends in contact dermatitis to hair dye: Comparing para-phenylenediamine positivity after a decade long intervalEpidemiological trends in hair dye dermatitis: Comparing paraphenylenediamine positivity after a decade long interval. Indian J Dermatol Venereol Leprol. 2012;77:511–2. doi: 10.4103/0378-6323.82386. [DOI] [PubMed] [Google Scholar]
- 21.Søsted H, Agner T, Andersen KE, Menné T, Sosted H, Agner T, Andersen KE, Menne T. 55 cases of allergic reactions to hair dye: A descriptive, consumer complaint-based study. Contact Dermatitis. 2002;47:299–303. doi: 10.1034/j.1600-0536.2002.470508.x. [DOI] [PubMed] [Google Scholar]
- 22.Wilkinson SM, Beck MH. Contact Dermatitis-allergic: p-phenylenediamine and related dyes. In: Tony B, Stephen B, Neil C, Christopher G, editors. Rook's Textbook of Dermatology. 8th ed. Oxford: Blackwell Publishing: Oxford; 2010. pp. 26.60–26.62. [Google Scholar]
- 23.Ho SGY, Basketter DA, Jefferies D, Ryrcroft RJG, White IR, McFadden JP. Analysis of para-phenylenediamine allergic patients in relation to strength of patch test reaction. Br J Dermatol. 2005;153:364–7. doi: 10.1111/j.1365-2133.2005.06742.x. [DOI] [PubMed] [Google Scholar]
- 24.Handa S, Mahajan R, De D. Contact dermatitis to hair dye: An update. Indian J Dermatol Venereol Leprol. 2012;78:583–90. doi: 10.4103/0378-6323.100556. [DOI] [PubMed] [Google Scholar]
- 25.Ghosh S, Mukhopadhyay S. Chemical leucoderma: A clinico-aetiological study of 864 cases in the perspective of a developing country. Br J Dermatol. 2009;160:40–7. doi: 10.1111/j.1365-2133.2008.08815.x. [DOI] [PubMed] [Google Scholar]
- 26.Fukunaga T, Kawagoe R, Hozumi H, Kanzaki T. Contact anaphylaxis due to para-phenylenediamine. Contact Dermatitis. 1996;35:185–6. doi: 10.1111/j.1600-0536.1996.tb02348.x. [DOI] [PubMed] [Google Scholar]
- 27.Basketter DA, Liden C. Further investigations of the prohapten concept: Reactions to benzene derivatives in man. Contact Dermatitis. 1992;27:90–7. doi: 10.1111/j.1600-0536.1992.tb05216.x. [DOI] [PubMed] [Google Scholar]
- 28.Eilstein J, Giménez-Arnau E, Duché D, Rousset F, Lepoittevin J, PEilstein J, Gimenez-Arnau E, Duche D, Rousset F, Lepoittevin JP. Mechanistic studies on the lysine induced N-formylation of 2,5-dimethyl-p-benzoquinonediimine. Chem Res Toxicol. 2007;20:1155–61. doi: 10.1021/tx700040s. [DOI] [PubMed] [Google Scholar]
- 29.Kawakubo Y, Nakamori M, Schöpf E, Ohkido MKawakubo Y, Nakamori M, Schopf E, Ohkido M. Acetylator phenotype in patients with p-phenylenediamine allergy. Dermatology. 1997;195:43–5. doi: 10.1159/000245683. [DOI] [PubMed] [Google Scholar]


