Abstract
Background:
About 25–45% of patients of chronic urticaria (CU) have been stated to have histamine releasing autoantibodies in their blood. The term autoimmune urticaria is increasingly being accepted for this subgroup of patients. Review of the literature suggests high autologous serum skin test (ASST) positivity and presence of antithyroid microsomal antibodies in patients with autoimmune urticaria.
Aims:
To study prevalence of ASST positivity and antithyroid microsomal antibodies in chronic “idiopathic” urticaria and to study the correlation between the two parameters.
Methods:
All patients of chronic idiopathic urticaria satisfying inclusion/exclusion criteria were enrolled in the study after written informed consent. Patients of CU secondary to infections and infestations, physical urticaria including dermatographism, mastocytosis, urticarial vasculitis and those on treatment with immunosuppressive drugs for urticaria were excluded from the study. In all of these patients, complete blood count; ASST, serum T3/T4/thyroid stimulating hormone levels, antithyroid microsomal antibody (AMA) levels were done. Statistical analysis was done by Chi-square test, Fisher exact test and Kappa statistics.
Results:
Study included 24 males and 26 females with mean age of 39.54 years. Majority of patients belonged to 20–40 years of age. Females showed more ASST positivity. A total of 12 out of 50 (24%) patients showed positive ASST. A total of four out of 12 (33.33%) had positive ASST and raised AMA levels.
Conclusion:
Only 25% of patients of chronic idiopathic urticaria had positive ASST. ASST and AMA levels were positively correlated in our study. Further studies are required to authenticate this association.
Keywords: Autologous serum skin test, antithyroid microsomal antibody, chronic urticaria, chronic autoimmune urticaria
INTRODUCTION
Urticaria is a common immunological disorder in dermatology practice that is characterized by pruritic erythematous edematous plaques (hives or wheals), with individual lesions lasting <24–48 h. There is now strong evidence that up to 30% of so-called chronic “idiopathic” urticaria is of autoimmune origin. Sera of 30-60% of patients with chronic “idiopathic” (ordinary) urticaria have been shown to cause a wheal, probably due to histamine, when injected intradermally into the patient's skin (autologous serum skin test [ASST]).[1]
ASST detects autoimmune urticaria. It has been suggested that chronic autoimmune urticaria (CAU) in some patients may be associated with systemic autoimmune disorders, commonly Hashimoto's thyroiditis.[2,3,4,5] It may thus be hypothesized that a positive ASST in CAU may be associated with the presence of antithyroid microsomal antibodies (AMA) in the serum. The current study is aimed at establishing such an association.
METHODS
The cross-sectional study included 50 patients of chronic urticaria (CU) attending the dermatology outpatient department of a tertiary care hospital and a referral center over a period of two years from December 2008 to November 2010. Written informed consent was obtained from all patients. The study protocol, patient information sheet and consent form were approved by the Institutional Ethics Committee.
A detailed history and clinical examination was recorded for each patient. Patients of chronic idiopathic urticaria were identified based on history, examination and routine laboratory investigations. Investigations included complete blood count, stool examination, urine microscopy etc., to rule out possible causes of urticaria. Patients having acute urticaria (<6 weeks), physical urticaria including symptomatic dermographism (mechanical urticaria), solar urticaria, cold urticaria, pressure urticaria, cholinergic urticaria, contact urticaria syndromes, urticaria pigmentosa (mastocytosis), urticarial vasculitis, and those on immunosuppressives during the last four weeks were excluded form the study. All patients who were identified as chronic idiopathic urticaria were further subjected to the following investigations: ASST, serum thyroid stimulating hormone (TSH) and serum anti-thyroid peroxidase or antithyroid microsomal antibodies (AMA).
A test was defined as positive when the diameter of the wheal at the serum injected site was 1.5 mm greater than that of the wheal bleb at the saline injected site [Figure 1].
Figure 1.
Autologous serum skin test and anti-microsomal antibody in urticaria patients
Serum TSH was done by IRMA, DPC kit Inc. USA™. Normal levels of serum TSH range from 0.46 uIU/ml to 5 uIU/ml. Serum AMA was estimated by Chemilumniscence Immunoassay (Aculite CLIA®, Monbind Incorporation™, USA). Normal levels range upto 40 IU/ml.
Fisher's exact test, a nonparametric test, and Kappa statistic was applied to qualitative data. P < 0.05 was considered to be statistically significant. Sensitivity and specificity analysis was done whenever required.
RESULTS
A total of 50 patients of chronic idiopathic urticaria including 24 males and 26 females were enrolled in the study. Majority of patients included in the study belonged to the 20-30 years age group. The mean age of presentation was 35.54 years.
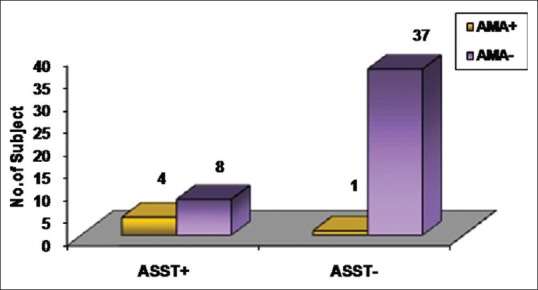
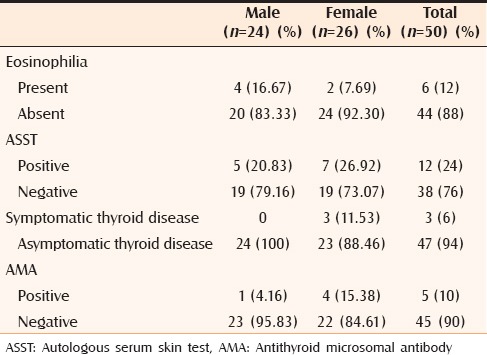
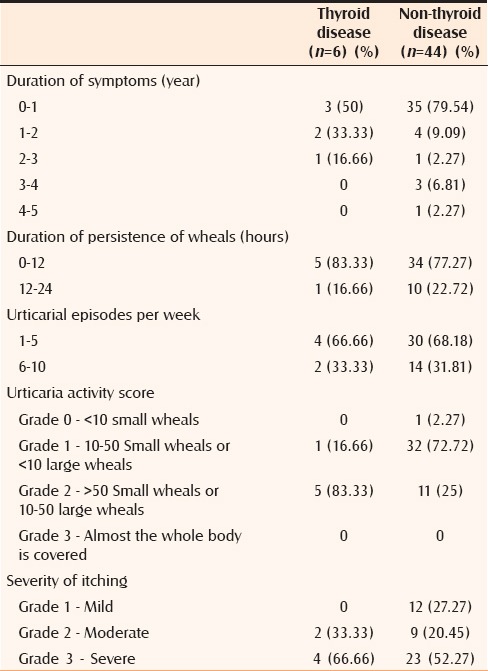
A total of 24% subjects (12 out of the 50) of chronic idiopathic urticaria showed positive ASST. Females showed more ASST positivity (7 out of the 12, 58.33%). Only 10% patients (5 out of 50) had thyroid autoimmunity as evaluated by serum AMA. Thyroid autoimmunity was common in females (80%). A total of four patients of 12 (33.33%) had positive ASST and raised AMA levels. Only 24% of patients of chronic idiopathic urticaria had positive ASST [Figure 2 and Table 1]. In our study that ASST positivity is significantly associated with thyroid disease with sensitivity of 83.33% and specificity of 84.09%. The correlation between ASST and AMA was found to be statistically significant (P < 0.002, Kappa statistics) with sensitivity and specificity of ASST in AMA positive patients being 80% and 82.22% respectively. CU associated with thyroid autoimmunity was found to be severe as compared to nonthyroid patients as assessed by urticaria activity score. Some of the important gender differences with regard to various parameters of urticaria are depicted in Tables 2 and 3.
Figure 2.
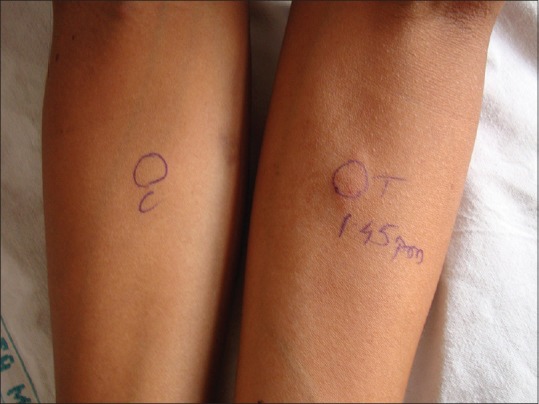
Photograph showing positive autologous serum skin test
Table 1.
Laboratory profile of chronic urticaria patients with thyroid diseases viz. non-thyroid disease
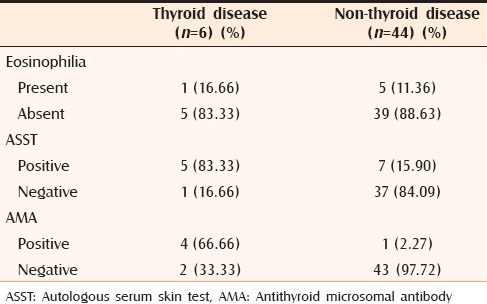
Table 2.
Clinical profile of chronic urticaria in males and females
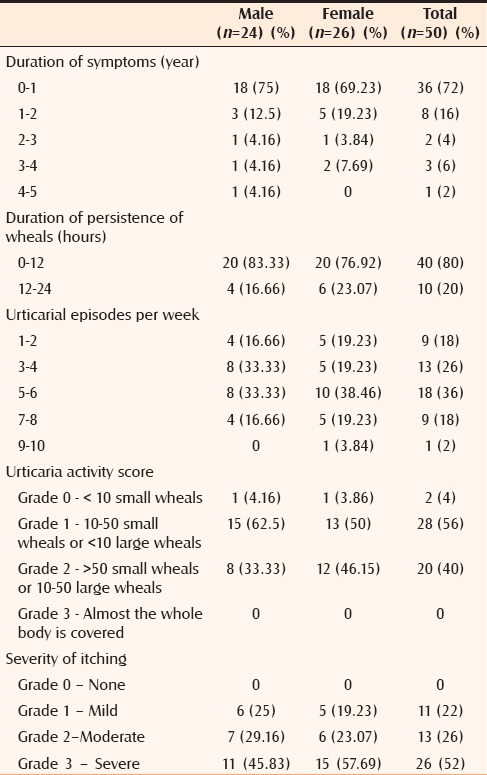
Table 3.
Laboratory profile of chronic urticaria in males and females
DISCUSSION
This study correlated ASST and antithyroid microsomal antibodies the serum of patients with chronic idiopathic urticaria in which 50 patients of chronic “idiopathic” urticaria were enrolled over a period of two years at a tertiary care hospital and referral centre in central India.
Mean age of the patients in our study was 35.94 years. Other studies on CU also showed similar age distribution. Mean age was 34 years in a study by Mamatha et al.[6] whereas it was 45 years in a study by Sabroe et al.[7] Almost 64% patients were in 2nd and 3rd decade of life compared to with 14/34 (50%) in a study by Mamatha et al.[6]
In our study, CU was present in 26 females and 24 males. Out of 12 patients who were ASST positive, 7 females were ASST positive (58.33%) [Table 3]. Mamatha et al.[6] in their study noted that 18 out of the 34 ASST-positive patients (52.94%) were females. Nettis et al.[8] in their study found no significant differences between female (41.25%) and male (40.91%) patients who were ASST positive. The findings in our study are comparable with those of the above mentioned studies. Higher prevalence noted in females is probably because women have a higher prevalence of autoimmune diseases.[9]
We screened 50 consecutive patients of CU for this study of which 12 patients exhibited positive ASST reactions (24%). This figure is nearly similar to that observed by Godse (26.67%), who also found that ASST positivity was less than that reported in the western literature.[10] Our figure is lower than that reported by Bajaj et al.[11] (49.5%), Mamatha et al.[6] (34%), Nettis et al.[8] (41.2%) and O’Donnell et al.[12] (60%).
Autologous serum skin test has a sensitivity of approximately 70% and a specificity of 80%. It may be used as a reasonably predictive clinical test to indicate the presence of functional circulating autoantibodies.[7]
The mean duration of disease in all patients of chronic idiopathic urticaria was 13.32 ± 13.95 SD months. Mean duration of disease in ASST positive patients was 19.16 ± 18.94 SD months while the mean duration in ASST negative patients was 11.47 ± 11.68 SD months. The study by Mamatha et al.[6] showed contrasting findings in which the mean durations of ASST positive and ASST negative urticaria was 12 and 15 months respectively. However the findings in our study were comparable with Sabroe et al. and Bajaj et al. (2.5 years).[11] This states the fact that mean duration of the disease is relatively more in ASST positive patients of urticaria. Thus ASST could be used as a pointer towards chronicity of urticaria. However, more studies would be required to authenticate this observation. In our study 18/50 (36%) [Table 2] had daily attacks of urticaria whereas in the study by Mamatha et al.[6] 24/34 (70.58%) with positive ASST had almost daily attacks.
In the present study, we found that the proportion of patients with urticaria activity score of 2 (UAS-2) that is, 50 small wheals or 10–50 large wheals is higher in patients with thyroid autoimmunity (83.33%) as compared to nonthyroid patients (25%) [Table 4]. This observation was statistically significant (P < 0.002, Kappa statistics). It can be inferred from our study that CU associated with thyroid autoimmunity can be more severe as assessed by urticaria activity score. However it has been observed that the patients with autoimmune CU generally had more severe symptoms than those with idiopathic CU.[13] Few studies have been done to evaluate the relationship of severity of urticaria with thyroid autoimmunity. A study done by Aamir et al.[14] in 2008 showed that the frequencies of antithyroid antibodies was significantly higher in patients with CU than in healthy subjects.
Table 4.
Clinical profile of chronic urticaria patients with thyroid diseases viz. non-thyroid disease
Our study showed that only five out of 50 urticaria patients had thyroid autoimmunity (12%) with high AMA positivity (80%). Leznoff and Sussman[5] reported 90 of 624 urticaria patients (14.4%) had AMA positivity. In another study done recently, Turktas et al.[15] explored the association of CU or angioedema with thyroid autoimmunity by measuring thyroid function tests and thyroid autoantibodies in 94 patients with CU or angioedema with 80 age and sex matched healthy volunteers. Eleven patients (11.7%) were found to have thyroglobulin antibodies and nine patients (9.57%) antithyroid microsomal antibodies in the CU and/or angioedema group, findings closely similar to ours. However, Turktas et al. attempted to find autoimmunity by estimating thyroglobulin antibodies. We could not estimate thyroglobulin antibodies due to cost constraints.
In present study, we observed that ASST positivity is present in 5 out of 6 (83.33%) patients with thyroid autoimmunity as compared to 7 out of 44 (15.90%) in patients with nonthyroid diseases (P < 0.002, significant - Kappa statistics). Thus it is observed in our study that ASST positivity is significantly associated with thyroid disease. Sensitivity-specificity analysis of ASST positivity and thyroid disease has revealed high sensitivity of 83.33% and specificity of 84.09%.
We found that AMA positivity is present in 4 out of 6 (66.66%) patients with thyroid autoimmunity as compared to 1 out of 44 (2.27%) patients with nonthyroid diseases (P < 0.002, Kappa statistics). This emphasizes the fact that AMA has sensitivity of 66.66% and specificity of 97.72% for the detection of thyroid autoimmunity.
In the present study, we correlated relationship of ASST with AMA in patients of CU. Out of 12 ASST positive patients, four patients (33.33%) had both ASST and AMA positivity. Similarly 37 patients of CU had both ASST and AMA negativity. Thus the correlation between ASST and AMA was found to be statistically significant (P < 0.002, Kappa statistics). Sensitivity of ASST in AMA positive patients was 80% and specificity was 82.22%. In our study, this significantly establishes the fact that ASST is capable of detecting thyroid autoimmunity (as routinely done by serum AMA estimation). Ours was the only second study after Bakos and Hillander[16] who evaluated usefulness of ASST in detection of thyroid autoimmunity. More such studies would be required to confirm our observations. This is important because ASST can be employed as a simple and cost-effective tool for the diagnosis of CAU associated with thyroid autoimmunity.
In our study it was observed that ASST is capable of identifying the subset of CAU from the so called chronic “idiopathic” urticaria. More such studies would be required to confirm our observations. Similarly, apart from thyroid autoimmunity, association of ASST in other autoimmune diseases such as Addison's disease, diabetes mellitus, pernicious anemia and vitiligo needs to be assessed by further studies. This will help in evaluating usefulness of ASST in the detection of CAU from chronic idiopathic urticaria.
In summary, the correlation between ASST and AMA was found to be statistically significant with sensitivity and specificity of ASST in AMA positive patients being 80% and 82.22% respectively. Our study suggests that ASST is capable of detecting thyroid autoimmunity (as routinely done by serum AMA estimation). ASST can be employed as a simple and cost-effective tool for the diagnosis of CAU associated with thyroid autoimmunity. Our study has a few limitations. Serum thyroglublin antibodies were not estimated. Similarly antibodies for the diagnosis of other autoimmune diseases were not estimated. The advantage of ASST is that it is a simple and easy test to detect autoimmune urticaria in the resource-poor settings. In our study we concluded that ASST positivity is significantly associated with thyroid disease. CU associated with thyroid autoimmunity is more severe as compared that in nonthyroid patients.
ACKNOWLEDGMENT
Dr. Pramod Gandhi. MD(Medicine), DM(Endocrinology) Nagpur.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Niimi N, Francis DM, Kermani F, O’Donnell BF, Hide M, Kobza-Black A, et al. Dermal mast cell activation by autoantibodies against the high affinity IgE receptor in chronic urticaria. J Invest Dermatol. 1996;106:1001–6. doi: 10.1111/1523-1747.ep12338544. [DOI] [PubMed] [Google Scholar]
- 2.Heymann WR. Chronic urticaria and angioedema associated with thyroid autoimmunity: Review and therapeutic implications. J Am Acad Dermatol. 1999;40:229–32. doi: 10.1016/s0190-9622(99)70193-3. [DOI] [PubMed] [Google Scholar]
- 3.Rumbyrt JS, Katz JL, Schocket AL. Resolution of chronic urticaria in patients with thyroid autoimmunity. J Allergy Clin Immunol. 1995;96:901–5. doi: 10.1016/s0091-6749(95)70226-1. [DOI] [PubMed] [Google Scholar]
- 4.Leznoff A, Josse RG, Denburg J, Dolovich J. Association of chronic urticaria and angioedema with thyroid autoimmunity. Arch Dermatol. 1983;119:636–40. [PubMed] [Google Scholar]
- 5.Leznoff A, Sussman GL. Syndrome of idiopathic chronic urticaria and angioedema with thyroid autoimmunity: A study of 90 patients. J Allergy Clin Immunol. 1989;84:66–71. doi: 10.1016/0091-6749(89)90180-2. [DOI] [PubMed] [Google Scholar]
- 6.George M, Balachandran C, Prabhu S. Chronic idiopathic urticaria: Comparison of clinical features with positive autologous serum skin test. Indian J Dermatol Venereol Leprol. 2008;74:105–8. doi: 10.4103/0378-6323.39690. [DOI] [PubMed] [Google Scholar]
- 7.Sabroe RA, Seed PT, Francis DM, Barr RM, Black AK, Greaves MW. Chronic idiopathic urticaria: Comparison of the clinical features of patients with and without anti-FcepsilonRI or anti-IgE autoantibodies. J Am Acad Dermatol. 1999;40:443–50. doi: 10.1016/s0190-9622(99)70495-0. [DOI] [PubMed] [Google Scholar]
- 8.Nettis E, Dambra P, D’Oronzio L, Cavallo E, Loria MP, Fanelli M, et al. Reactivity to autologous serum skin test and clinical features in chronic idiopathic urticaria. Clin Exp Dermatol. 2002;27:29–31. doi: 10.1046/j.0307-6938.2001.00962.x. [DOI] [PubMed] [Google Scholar]
- 9.Juhlin L. Recurrent urticaria: Clinical investigation of 330 patients. Br J Dermatol. 1981;104:369–81. doi: 10.1111/j.1365-2133.1981.tb15306.x. [DOI] [PubMed] [Google Scholar]
- 10.Godse KV. Autologous serum skin test in chronic idiopathic urticaria. Indian J Dermatol Venereol Leprol. 2004;70:283–4. [PubMed] [Google Scholar]
- 11.Bajaj AK, Saraswat A, Upadhyay A, Damisetty R, Dhar S. Autologous serum therapy in chronic urticaria: Old wine in a new bottle. Indian J Dermatol Venereol Leprol. 2008;74:109–13. doi: 10.4103/0378-6323.39691. [DOI] [PubMed] [Google Scholar]
- 12.O’Donnell BF, Barr RM, Black AK, Francis DM, Kermani F, Niimi N, et al. Intravenous immunoglobulin in autoimmune chronic urticaria. Br J Dermatol. 1998;138:101–6. doi: 10.1046/j.1365-2133.1998.02033.x. [DOI] [PubMed] [Google Scholar]
- 13.Sharma YK, Gera V, Tiwari VD. Chronic urticaria: Expanding the autoimmune kaleidoscope. Med J Armed Forces India. 2004;60:372–8. doi: 10.1016/S0377-1237(04)80015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aamir IS, Tauheed S, Majeed F, Atif A. Serum antithyroid antibodies in female patients with chronic urticaria. J Coll Physicians Surg Pak. 2008;18:498–501. [PubMed] [Google Scholar]
- 15.Turktas I, Gokcora N, Demirsoy S, Cakir N, Onal E. The association of chronic urticaria and angioedema with autoimmune thyroiditis. Int J Dermatol. 1997;36:187–90. doi: 10.1046/j.1365-4362.1997.00187.x. [DOI] [PubMed] [Google Scholar]
- 16.Bakos N, Hillander M. Comparison of chronic autoimmune urticaria with chronic idiopathic urticaria. Int J Dermatol. 2003;42:613–5. doi: 10.1046/j.1365-4362.2003.01759.x. [DOI] [PubMed] [Google Scholar]


