Abstract
Introduction
Type 2 diabetes mellitus (T2DM) affects more than 1.1 million Canadians aged ≥65 years. Group Medical Visits are an emerging health service delivery method. Recent systematic reviews show that they can significantly reduce glycated haemoglobin (HbA1c) levels, but Group Visits have not been evaluated within primary care. We intend to determine the clinical effectiveness, quality of life and economic implications of Group Medical Visits within a primary care setting for older people with T2DM.
Methods and analysis
A 2-year proof-of-concept, single-blinded (measurement team) randomised control trial to test the efficacy of Group Medical Visits in an urban Canadian primary care setting. Participants ≥65 years old with T2DM (N=128) will be equally randomised to either eight groups of eight patients each (Group Medical Visits; Intervention) or to Individual visits (Standard Care; Controls). Those administering cointerventions are not blinded to group assignment. Our sample size is based on estimates of variance (±1.4% for HbA1c) and effect size (0.9/1.4=0.6) from the literature and from our own preliminary data. Forty participants per group will provide a β likelihood of 0.80, assuming an α of 0.05. A conservative estimation of an effect size of 0.7/1.4 changes the N in the power calculation to 59 per group. Hence, we aim to enrol 64 participants in each study arm. We will use intention-to-treat analysis and compare mean HbA1c (% glycosylated HbA1c) (primary outcome) of Intervention/Control participants at 12 months, 24 months and 1 year postintervention on selected clinical, patient-rated and economic measures.
Trial registration number
Keywords: PRIMARY CARE, PUBLIC HEALTH
Strengths and limitations of this study.
First randomised controlled trial (RCT) to evaluate Group Medical Visits with a general practitioner lead in diabetes management.
The intervention addresses a Chronic Care Model by combining an interprofessional team-based medical care, patient self-management, life skills development and disease-specific education, with a focus on physical activity and nutrition.
The content of the intervention is based on the successful Trento model with an additional focus using our expertise from 10 years of physical activity interventions (group-based and individual).
To the best of our knowledge, this is the first study to evaluate the efficacy of Group Medical Visits to promote physical activity as measured objectively (SenseWear accelerometer).
Currently, the study is limited to one geographic location with a relatively homogeneous population. Given that a single specific physician is leading the intervention, the findings may not be generalisable to other practitioners.
Introduction
If our health care system had evolved differently, had it evolved dealing with chronic diseases—which is the issue today—rather than acute diseases, we probably would have started with Group Visits. And now, someone would probably be preaching about the benefits of an individual office visit as a better model for acute disease management.
∼Edward Noffsinger, PhD, Group Medical Visits pioneer
Diabetes mellitus affects all age groups worldwide.1 More than 1.1 million people diagnosed with diabetes mellitus (DM) in Canada are over the age of 65.2–5 According to the Public Health Agency of Canada, the overall prevalence rate for type 2 DM (T2DM) in Canada is 6.8%; yet starting at age ∼55, rates increase exponentially from 14% to a high of 28.5% among those individuals aged 75–79. Rates of T2DM in older people are accelerating even when adjusted for age.6 7 The American Diabetes Association (ADA) estimated that there were nearly 17.5 million people living in the USA with diagnosed type 1 or type 2 diabetes in 2007, at an estimated cost of $174 billion in higher medical costs and lost productivity.8 In 2012, the estimated total economic cost of diagnosed diabetes increased by 41% to $245 billion. The financial burden of DM to the Canadian healthcare system will approach $17 billion/year by 2020.7 9 10
Good metabolic control of diabetes prevents complications.1 2 11 12 Combinations of drug treatment, physical activity (PA),13 nutrition advice and body weight management14 15 reduce risk factors, delay onset of disease and lessen the rate of complications.11 16–18 Lifestyle interventions focused on bodyweight control, PA and dietary modification can prevent or postpone the manifestation of type 2 diabetes.19 During the 10-year follow-up of the US Diabetes Prevention Programme (DPP), cumulative diabetes incidence rates were ‘reduced by 34% (24–42%) in the lifestyle group and 18% (7–28%) in the metformin group compared with placebo’.20 The DPP and the Diabetes Prevention Study (DPS) in Finland both reported a ‘58% risk reduction after interventions aimed at weight loss, dietary change, and increased physical activity’.21
In Canada, the usual clinical care for diabetes is via individual patient consultations combined with the potential for unstructured educational advice during a family practice appointment or referral to an educational support programme, if available. Evaluation of traditional primary care delivery highlights that many patients do not receive guideline care.22–24 Moreover, traditional individual physician appointments are not based on the principles of the Chronic Care Model.25–27
Traditional one-to-one clinical encounters will always have a place in health service delivery. However, we ask the question, ‘Is there a more effective way to encourage successful patient self-management for older people withT2DM?’.25 Group Medical Visits (GMVs) or Shared Medical Appointments may contribute to improved T2DM care for older people in the primary care setting.
GMVs are organised for a group of people living with a specific condition and a proactive interprofessional team which supports the group.28 The structure and formats of GMVs vary; typically, in lieu of an individual visit, a patient will participate in a longer (60–120 min) group visit with 6–14 other patients, led by a physician and/or other healthcare practitioner. The group component emphasises medical care (ie, interprofessional team-based care), disease-specific education and life skill development.
The most compelling clinical trial data for GMVs providing superior control of HbA1c come from Dr Trento and Dr Porta, University of Turin, Italy.29–31 Patients who attended structured Group Medical Visits decreased their HbA1c by 0.9% (Effect size 0.56) compared with control group counterparts.29 In their ROMEO clinical trial,32 the Turin investigators concluded that Group Care when compared to ‘Usual Care’ represented a ‘cost-neutral approach to the outpatient management of T2DM’.32
Building on those data, we highlight four additional elements that are of interest. First, the studies in Turin and around Italy31 took place in ‘hospital-based clinics’, not regular primary care settings. An endocrinologist led the GMVs; primary care was not part of the team. Second, participants in the Turin studies averaged 64 years of age. Third, the Turin studies did not include a generic quality of life measure (eg, EQ-5D) and did not estimate health utilities, including complications, hospital admissions or adjunctive therapies. Fourth, health economic implications cannot easily be extrapolated from the Italian health system to that in other countries.
To the best of our knowledge, there has been no published RCT of GMVs for any condition in Canada—certainly not for T2DM. In a systematic review of RCTs of GMVs for T2DM, Housden et al33 reported a 0.46% reduction in HbA1c across 10 RCTs that met their inclusion criteria. However, in a 12-month US Veteran Affairs Medical Centre trial, Group Medical Visit patients had only a 0.3% improvement over patients randomised to individual care (effect size 0.21).34 Study duration was the main difference between the US and the University of Turin studies appeared similar. Housden reported that the duration of GMVs (ie, 24 months) was significantly associated with outcome (approximately 0.25% lower HbA1c per year), but the number of Group Medical Visits was not. This provides the rationale for an RCT across 2 years.
Therefore, we designed this study to answer the question ‘Do Primary Care-led GMVs provided seven times over 2 years improve metabolic control in diabetes?’
Methods
We aim to conduct a 24-month, single-blinded (measurement team), efficacy RCT to provide Canadian evidence for GMVs in the Primary care setting. The intervention patients (GMVs) will receive seven (7) GMVs sced quarterly. Each appointment combines specific medical advice with a targeted educational unit and life skills training to guide patients’ self-management; patients in the control arm will receive seven traditional one-to-one physician appointments (Usual Care). The primary clinical outcome for the ‘GMV’ RCT is HbA1c (%) at 24 months.
Participants
Our population of interest is patients aged ≥65 years with T2DM treated using oral hypoglycaemic agents and diet or diet alone.
Inclusion and exclusion criteria
Inclusion: M/F aged ≥65 years with a >12-month history of T2DM based on Canadian Diabetes Guidelines. Diagnostic criteria (any one of): (1) Fasting plasma glucose (FPG): ≥7.0 mmol/L where fasting=no caloric intake for at least 8 h. (2) HbA1c: ≥6.5% using a standardised validated assay in the absence of factors that affect the accuracy of A1c and not for suspected type 1 diabetes. (3) Oral glucose tolerance test: A 2 h plasma glucose level of ≥11.1 mmol/L after a 75 g oral glucose tolerance test. (4) Random plasma glucose: ≥11.1 mmol/L, where random is defined as any time of day without respect to when the last meal was taken. In addition, individuals must (1) have attended the general practitioner (GP) practice(s) in Abbotsford, BC (Canada), for at least 1 year (2) be community-dwelling and live within 30 km of their Abbotsford area GP clinic; (3) be able to comply with scheduled visits, treatment plans, and other procedures; (4) be able to read, write and speak English with acceptable auditory and visual acuity; (5) provide signed/dated informed consent; (6) be able to walk independently. Inclusion will be based on medical history, vital signs and physical examination by study physicians, and written recommendation by family physician indicating the appropriateness to participate.
Participants will need to have a working proficiency in English as group discussions, accompanying texts and instructions will all be in English. To provide adequate translation services for these elements in one or more other languages is beyond our budget and may also influence the dynamics of the GMV. It could be considered in a future iteration of this research programme.
Exclusion criteria: (1) using insulin (2) at high risk for cardiac complications during exercise/Class C of the American Heart Risk Stratification Criteria; (3) Mini-Mental State Examination (MMSE) score of ≤24 at screening;35 (3) have clinically significant peripheral neuropathy or severe musculoskeletal or joint disease that impairs mobility; (4) taking medications that may negatively affect the ability to safely undertake a simple walking programme; (5) planning to participate, or already enrolled in, a clinical drug trial concurrent to this study.
We have received ethics approval from UBC's Clinical Research Ethics Board.
The participating centres were selected based on their proximity and relationship to the lead physician (AW). The lead physician is a qualified MD experienced in PA promotion and prevention. Participating healthcare professionals were selected based on their expertise, interest in GMVs and preventive medicine/non-pharmacological treatments, proximity to the intervention setting and availability.
Recruitment
We are currently recruiting 128 (+13 for a contingency) community-dwelling adults aged ≥65 years who meet the inclusion and exclusion criteria.
Six members of our team have an established track record as study PIs who have recruited adults (50–90 years) to participate in RCTs (Khan, Davis, Dawes, Hoppmann, Liu-Ambrose, Madden). Madden and Khan and our Abbotsford lead Primary Care physician Dr WINDT will recruit from two designated Family Practice clinics in Abbotsford (Gateway/Whatcom Place). A recent review indicated that there are over 650 patients in the Gateway Clinic alone.
A trained research assistant (RA) will conduct detailed chart reviews of identified eligible patients at both clinics. Eight clinic physicians have agreed to assist with recruitment by flagging charts of current patients who may qualify. Eligible patients will be mailed an information package, including the consent form. Those who meet our inclusion criteria and are considered eligible after screening will be scheduled for baseline assessments.
Intervention (GMV)
We will schedule groups of eight patients for seven 90 min Group Visits over 2 years (spaced quarterly). The physician (AW) will lead each GMV in collaboration with an exercise professional, a nutritionist or a pharmacist. Sessions consist of ‘clinical time’ and ‘group education/discussion time’. In the clinical time, the physician responds to specific health questions from patients. Some patients may schedule additional time before or after the session to review their individual clinical results with the physician. Within Canada, family physicians are taught to be ‘Health Advocates’, as part of the ‘CanMeds Family Medicine Roles.’
The exercise professional/nutritionist/pharmacist will cofacilitate discussions around PA/healthy nutrition/medication management. The physician is responsible for the curriculum content which has been developed with all grant members, clinical advisors and the literature.29 36
Key elements of the curriculum include the following: (1) Patients complete a preappointment questionnaire that the interdisciplinary team uses to identify each patient's educational needs; (2) the patients are encouraged to use goal-setting techniques to initiate and maintain healthy eating and PA behaviours (guided by coinvestigator Hoppmann); (3) educational goals and specific health and learning objectives are identified in each GMV. Only one or two core concepts are covered in each GMV, with a direct connection to the goal-setting component of the GMV. Patients also receive a single page worksheet in each GMV; (4) we emphasise PA in each Group Visit; (5) each patient completes a feedback form that assesses the learning objectives of the class; feedback is used to adapt the next class based on patient needs.
We used the successful Trento model29 30 as the basis by which to standardise the content and overall structure of the Group Visits. One of our innovations will be to place greater emphasis on PA promotion.
The family physician in this study has created a checklist with seven key elements of the management plan based on the Canadian Diabetes Management Guidelines. He will use the checklist as he discusses items in the GMV. He will make notes about individual patient discussions in the notes at the end of the GMV. A separate clinically trained RA will review the patient notes between group visits and record what percentage of the items from the checklist was addressed. The same checklist will be provided to the physicians caring for patients in the individual appointment arm of the study. The same RA will review the patient notes from this arm of the study.
Control (usual care)
Participants will receive seven traditional one-to-one physician appointments over 2 years. They will see their physician quarterly as per usual care in BC practices. They will be referred to ancillary services such as nutrition advice, educational counselling and PA promotion according to ‘usual care’ practice.
In addition to reducing attrition, we will organise four 1 h social events for participants in both arms of the study annually.
Study setting
GMV (Intervention) will take place in a classroom setting at the local recreation centre (http://www.abbotsford.ca; Abbotsford, BC).
Research hypotheses
Compared with the Individual Appointment arm, participants receiving GMVs will have lower Hba1c after the 24-month intervention.
Objectives
- Primary outcome measure (all at 24 months):
- Patients’ control (decreased levels) of HbA1c (clinical)
- Secondary outcome measures:
- Resting systolic/diastolic blood pressure (mm Hg)
- Electrical activity of the heart (ECG)
- C reactive protein (mg/L); plasma glucose (mmol/L); high-density lipoprotein-cholesterol (HDL-C; mmol/L); fasting low-density lipoprotein (LDL; mmol/L); triglycerides (mmol/L)
- Height (cm); weight (kg); waist and hip circumference (cm); fat and muscle mass (g)
- Quality of life (as measured by the health state utility values of the EQ-5D3 L questionnaire (patient-reported quality of life/economic))
- Health Care Utilisation (HRU questionnaire)
- Anxiety (GMVD-7); Depression (GDS); Satisfaction with Life (Scale)
- PA (PASE questionnaire/SenseWear accelerometer)
- Goal Setting and Action Planning (questionnaire)
- Food Intake (self-reported three-day diary)
- Patient Self-Management (Patient Activation Measure (PAM))
Measurement
As per our pilot baseline assessments, all measurement will be conducted in Abbotsford using our Mobile Research Laboratory. We will conduct measurements at 0 (baseline), 12 (mid-intervention) and 24 (end of-intervention) months. We assess primary outcomes at 24 months but will follow-up to evaluate change at 36 months (12-month follow-up). In addition, we will obtain three-monthly data for blood tests as part of routine patient management before each of the three-monthly GMVs (Intervention) and at patient appointments (Control).
Assessments—Demographic information: Under the supervision of the Principal Investigator (PI), research staff will collect demographic information (Patient Information Form) and ensure that the consent form is completed.
Assessments—Medical history: The physician will perform a screening medical examination on each participant. He will obtain a relevant medical history that includes cardiovascular and smoking history, diabetes complications, comorbidities and current medications, and evaluate symptoms. He will also determine vaccination status, and conduct retinopathy and foot examinations. The physician will issue a laboratory requisition to the participant to be completed at their local laboratory within 3 days for ECG and blood work (HbA1c (%); C reactive protein (mg/L); serum glucose (mmol/L); high-density lipoprotein-cholesterol (HDL-C; mmol/L); low-density lipoprotein (LDL; mmol/L); triglycerides (mmol/L)).
We will obtain a 12-lead ECG from the pathology laboratory in Abbotsford within 2 weeks of baseline measurement. We will measure diastolic/systolic blood pressure using the automated BP device BPTRU. Patients will be asked to rest 5 min between measurements, which will be taken twice on each arm as per standard protocol.
Assessments—Body composition: (1) Height (cm): Wall-mounted stadiometer (Rosscraft Inc) using standard techniques; (2) Weight (kg): electronic scale (Seca Model 242, Hanover, Maryland, USA) with their feet together. Weight is recorded to the nearest 0.1 kg. For height and weight, duplicate measures are taken unless measures differ by ±0.4 cm (height) or ±0.2 kg (weight), when a third measure is taken. We will calculate body mass index (BMI) as wt/ht2; (3) Waist circumference (cm): We use a flexible steel tape (Rosscraft Inc). We obtain two measures during minimal respiration and record to the nearest 0.1 cm. We perform a third measure if the difference between the first two measures is greater than 0.2 cm. We use the mean of two and median of three measurements for analysis for all measures; (4) Total body fat and muscle mass (g): dual-energy X-ray absorptiometry (DXA) (Hologic QDR 4500W, Hologic Inc, Waltham, Massachusetts, USA), using standard protocols37 across all years. An anthropomorphic phantom is scanned daily for quality control. Precision (with repositioning) in healthy adults was 1.9% for total body fat mass and 0.33% for total body lean mass (CHHM Bone Health Research Group, unpublished data).
Assessments—Cognitive, Physical activity, Nutritional Intake, Self-Management:
Cognitive—Mini-Mental State Examination (MMSE), used to assess eligibility. Participants will need to have a score of >24 at screening to be eligible;
Physical activity—We will assess PA with the valid and reliable Physical Activities Scale for the Elderly (PASE) questionnaire.38 PASE was designed for those aged 65 years and older; participants use a 12-item scale to self-report the hours per day (average) spent participating in leisure, household and occupational physical activities over the previous 7-day period. PA is an important covariate in this study.
The investigators will assess PA with the valid and reliable SenseWear armband accelerometer, measuring the total number of steps; PA levels and duration; total energy expenditure (kcal/min); active energy expenditure (kcal/min); METS; sleep duration and efficiency; lying down time; on/off body time. During the week before each assessment, participants will wear the armband for seven consecutive days, including while sleeping.
Nutritional intake—We will instruct participants on how to fill out a 3-day food diary, which they will need to start the day after their blood work has been taken.
Patient self-management—Investigators will administer the Patient Activation Measure (PAM). The PAM has been tested extensively across a number of different languages, cultures and demographic groups, and among people with different health conditions.39–51
Assessments—Health economics/quality of life: Participants will answer the EQ5D-3L52 53 and Health Resource Utilization (HRU) questionnaires. Our team has used both these instruments previously54 55 to assess the quality of life. Our economic evaluation will examine the incremental costs and benefits generated by using GMVs versus Individualised care. The outcome of our cost utility analysis is the incremental cost-effectiveness ratio (ICER). By definition, an ICER is the difference between the mean costs of providing the competing interventions divided by the difference in effectiveness (ie, QALYs), where the ICER=ΔCost/ΔEffect.56 Dr Marra and Dr Davis will conduct a prospective economic evaluation alongside the clinical trial to (1) estimate the mean/participant and total healthcare resource utilisation and costs associated with both the intervention and control groups; (2) determine the QoL as measured by health state utility values (via EQ-5D); and (3) conduct a cost-utility analysis.
The cost-utility analysis will be assessed in terms of incremental cost per quality adjusted life year (QALY). QALYs are calculated based on the quality of life of a patient (measured using health utilities) in a given health state and the time spent in that health state. The EQ-5D enables QALYs to be estimated. This captures the gains from reduced morbidity and reduced mortality by assigning quality weights at specific time points to an intervention that are based on preferences, anchored on perfect health and death, and measured on an interval scale. Economic analyses will be conducted from the BC Ministry of Health perspective and will capture the time horizon of the trial (24 months).
Assessments—Depression & anxiety: (1) Depression: The investigators will assess depression with the recommended Geriatric Depression Scale (GDS). The GDS is a 30-item self-report assessment used to identify depression in the elderly. JA Yesavage and others developed the scale in 1982; (2) Anxiety: We will assess depression and anxiety with the recommended Generalized Anxiety Disorder 7-item (GMVD-7) scale. Using the threshold score of 10, the GMVD-7 has a sensitivity of 89% and a specificity of 82% for generalised anxiety disorder. It is moderately good at screening three other common anxiety disorders—panic disorder (sensitivity 74%, specificity 81%), social anxiety disorder (sensitivity 72%, specificity 80%) and post-traumatic stress disorder (sensitivity 66%, specificity 81%);57 (3) Satisfaction With Life Scale (SWLS) is a measure of life satisfaction developed by Ed Diener and colleagues (Diener, Emmons, Larsen & Griffin, 1985). The SWLS consists of 5-items that are completed by the individual whose life satisfaction is being measured.
Assessments—Goal setting and action planning: Patients will answer goal setting/psychology questionnaires and discuss their lifestyle goals. UBC Assistant Professor and Canada Research Chair HOPPMANN leads the behavioural aspects of the study. From her experience in psychological ageing research and everyday health behaviours,58–60 she designs GMVs to help patients (1) set realistic health goals; (2) identify good opportunities to translate those health goals into action (action planning); and (3) proactively map out strategies that maintain health behaviours in the face of challenges (coping with planning).61
Methods—Measurement team training: Prior to each measurement period, we will conduct a four-hour training session in Abbotsford for a measurement team of six to eight RAs. The RAs will be trained to administer questionnaires, instructed in the correct techniques for anthropometric and physical measures and be advised on the ethics of data collection. They will be provided the opportunity to practise all measurements during the training session under supervision. We have DXA-trained technologists and a central core of RAs at CHHM whom we will retain for all measurements.
Methods—Sample size: Our sample size calculation is based on estimates of variance (±1.4% for HbA1c) and effect size (0.9/1.4=0.6 from the literature29 and from our own preliminary data from GMVs with primary care leads in the Vancouver Mid-Main Clinic and at the West Coast Family Medicine Clinic in Sooke, BC. HbA1C values for an extracted sample of 100 consecutive patients with T2DM in Abbotsford averaged 7.5% with an SD of 1.5.
Trento et al29 reported an HbA1c SD of ±1.4% in the mean baseline HbA1c of 7.4 across groups. In the intervention group, HbA1c in 43 patients increased to 7.5±1.4. In the control group, HbA1c increased to 8.3±1.8. These data reflect a Cohen's d effect size of (0.9/1.6=0.56). Thus, assuming an α of 0.05, 40 participants per group will provide a β likelihood of 0.80. However, we aim to be conservative with our estimate of effect size; an effect size of 0.7/1.4 changes the N in the power calculation to 59 per group. Hence, we aim to enrol 64 participants in each study arm following baseline measurement and randomisation. This provides a contingency for a smaller effect size than in previous studies. Note that our preliminary data relating to Hba1c levels in patients (Summary of Progress) are consistent with the data from Dr Trento (Turin, Italy).
Methods—Randomisation/blinding: Using remote randomisation, 64 patients with signed consent will be randomised to eight groups of eight patients each (GMV; Intervention); another 64 patients will be randomised to Individual Appointments (Usual Care; Controls). Figure 1 provides the flow of participants (consort type diagram). This is a single-blinded (measurement team) RCT. Those administering cointerventions will not be blinded to group assignment.
Figure1.
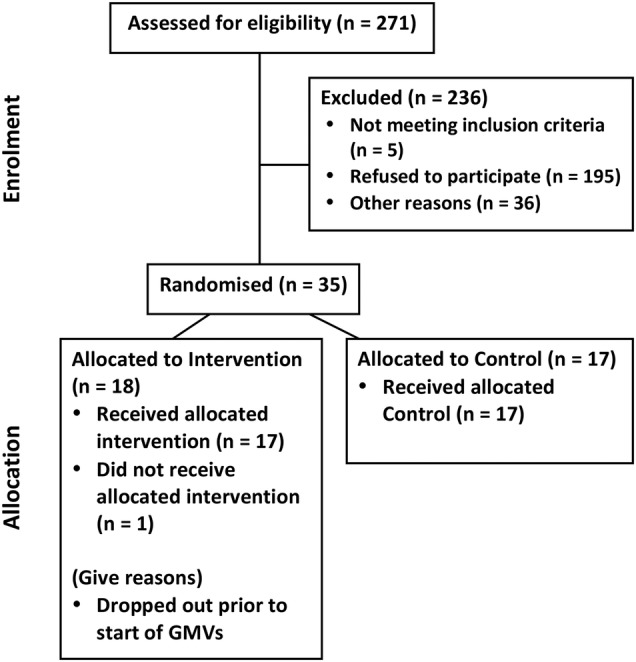
CONSORT—Group Medical Visits (GMVs) in primary care: protocol for an randomised controlled trial of group-based versus individual appointments to reduce glycated haemoglobin in older people.
Using a central, web-based randomisation service will conceal allocation. A UBC statistician independent of the trial will generate the randomisation sequence; permuted blocks of varying size will be employed to ensure balance over time.
Methods—Primary statistical analyses: We will use intention-to-treat analysis and compare mean HbA1c (% glycosylated HbA1c) of GMV participants with those of Control participants. By intention-to-treat analysis, we mean all randomised participants, regardless of protocol adherence (as per the SPIRIT protocol). Change from baseline to 24 months will be assessed using analysis of covariance that incorporates (controls for) baseline measures of the dependent variable and selected covariates. Observing a statistically significant difference in mean HbA1c between groups at 24 months will be considered evidence of efficacy. We will report variance, covariance and effect sizes. We will sample feasibility (ie, ease of recruitment, recruitment rate, withdrawal rate). These data will inform sampling for future trials.
After the trial is over, we will evaluate whether participant outcomes change 12 months after cessation of the intervention. This is similar to a ‘washout’ or ‘offset’ period in a drug trial that we found important in two previous clinical trials, which included a behavioural intervention. In both studies, trial benefits persisted further than expected beyond the intervention.62 63
Methods—Secondary statistical analyses: The secondary outcomes analyses will assess differences between groups in those secondary outcome measures listed in C) Objectives, above.
Methods—Analysis of population who are non-adherent: We will use intention-to-treat analysis. As our primary analysis involves change from baseline to 24 months, missing values at midpoint will not need to be imputed. Participants who attended at midpoint measurement (or who have clinical HbA1c data subsequently), but not at final measurement, will be excluded from the primary analysis.
Methods—Health economic statistical analysis: We will characterise healthcare resource utilisation by HRU for GMV and Individual Appointment arms. Costs will be assigned to each resource according to the 2013 BC Medical Guide for Fees (if related to physician billing or laboratory/procedure data); a fully allocated hospital cost model (if related to hospitalisation); and the BC PharmaCare formulary (for pharmaceutical costs). Since our analysis is focused on the Ministry of Health perspective, we are not interested in characterising non-covered direct medical costs and direct non-medical costs.
Methods—Adverse events monitoring: We will ask participants to log all adverse events from PA or dietary changes. Participants in GMVs are encouraged to discuss adverse events with the nurse/exercise professional at the next GMV. Similarly, Control participants will be asked at their appointments whether they suffered any adverse events in the previous 3 months. Investigators will modify the intervention for a given trial participant, depending on the nature of the need and request. Any changes will be (1) specific to the need; (2) made by the PI in consultation with the other investigators; and (3) will be officially documented within UBC ethics through their postapproval process. A participant will be withdrawn from the study if requested by the participant or if the PI deems the participant's continued involvement as an unreasonable risk to their safety and/or well-being.
Methods—Contingency plan
Recruitment: As a contingency, we have access to four additional practices in Abbotsford should they be required (12 000 patients in total; approximately 20% over age 65 years).
Should we fall short of our recruitment goal (deemed unlikely), we will add two additional clinics with five primary care physicians and 1300 total patients (all ages) in neighbouring Mission. There is also the potential to add a site on Vancouver Island (Sooke, BC). Clearly, additional sites have implications for consistency, and this will be taken into account in the design (stratification by site, planning meetings, training, teleconferences to support consistency) should it be needed.
Contamination: GMV-care for T2DM is not available elsewhere in Abbotsford. However, we will ask participants to ensure that GMVs are only being received in the research setting during the trial period.
Power: We have based 80% power on a conservative estimate of effect size. Housden et al33 used meta-regression to show that duration of GMV attendance was associated with a 0.25% change in HbA1c annually. Our intervention is planned to run for 2 years and replicates a study with an effect size of 0.56.29
Generalisability: We are translating elements of the Italian curriculum to the Canadian context. We will receive expert advice from educationalist Dr Trento at the University of Turin who will work closely with geriatric psychologist coinvestigator Hoppmann to ensure that we appropriately translate their more than 10 years of experience and clinical success to the Canadian context.
Methods—Intervention adherence/discontinuation
Our local RA will record attendance at each GMV and follow-up as appropriate with absent participants. The RA will also follow-up with all participants to book their assessments and rebook when needed.
Patients who discontinue from the study will not be contacted. Investigators will invite those individuals who deviate from protocol to participate in assessments; their data will be collected and included within the findings as appropriate.
Methods—Protocol amendments
The PI will submit protocol amendments to the UBC Clinical Ethics Board for approval. Changes will then be communicated to other investigators and participants as necessary through the most appropriate means possible, for example, email, posted letter, phone call, etc.
Methods—Data collection/storage
Study participants’ identities will be protected with the use of a unique study code. Research-related documents will not be derived from personal identifiers, such as Social Insurance Number, DOB, health plan number, etc, nor will they include information that would allow the subject to be identified. Any information which correlates subject names with the study code will be kept on the locked premises at UBC or in a secured electronic form.
RA will audit data entry. Data will be stored in a locked cabinet in a locked room to prevent unauthorised access, and in electronic form will have password protected limited access. The data will be securely stored and kept for 5 years after publication. After 5 years, all research-related study documents will be confidentially shredded and electronic data will be deleted. There are no plans for the future use of the data beyond this research.
Methods: Monitoring—Data monitoring committee: There are no plans for a data monitoring committee as both arms of the trial include management of T2DM using currently accepted methods. We consider this trial to provide minimal risk.
Methods: Monitoring—interim analysis: There are no plans for interim analyses. We do not anticipate potentially serious outcomes (as above). An argument against interim analysis is the increased risk of type 1 error.
Methods—Harms: We have not attributed harms as primary or secondary outcomes. We anticipate some participants having some muscle soreness associated with exercise but that is not dangerous. We will question side effects from the participants in the clinical encounters (group visits and usual care visits).
Methods—Auditing: We propose one independent review at the study midpoint when half of the total number of patients we aim to recruit have completed 1 year in the trial. The auditor (Canada Research Chair Linda Li) will independently verify participant enrolment, consent, eligibility and allocation to study groups; adherence to trial protocols, adherence to policies to protect participants, including reporting of harms; and completeness, accuracy and timeliness of data collection.
Results/Trial status: We have already recruited and randomised 34 participants within a single primary care clinic. The first two Intervention Groups (N=17) have finished their sixth GMV (6/7). Dr WINDT co-led each Group Visit along with an Exercise Professional (Visit #1) and a Nutritionist (Visits #2 and #4). Visit #3 focused on medical/medication management. We will continue to recruit for the other 92 participants from the same clinic along with a secondary primary care clinic as stated earlier in this protocol.
Discussion
Interpretation
Despite the clinical burden of T2DM among older Canadians, and the potential for the primary care system to deliver multidisciplinary care and education, there have been no randomised controlled trials (RCTs) using GMVs as a treatment tool in T2DM. Housden et al's systematic review and meta-analysis provides the foundation for our study.33
Is HbA1c the best primary outcome for an RCT examining metabolic control of T2DM in older people? HbA1c has been used for over 30 years as a marker of cumulative glycaemic exposure over the previous period of 2–3 months. In terms of monitoring management, HbA1c is a widely accepted method and its use as the primary outcome in Housden et al's systematic review attests to the measure's suitability. HbA1c is ‘now used ubiquitously for monitoring effective glycemic control as a cornerstone of diabetes care’.64 A 1% difference in HbA1c is important because it associates with a 15–21% reduction in relative risk of cardiovascular disease.65 66 There is, however, a vigorous debate among endocrinologists as to whether HbA1c should be used to diagnose T2DM.67 The authors of this excellent debate point out the limitations of the test in certain ethnicities and in certain clinical settings.
Therefore, we will address the (1) absence of Canadian data from RCTs in any GMV setting; (2) absence of Canadian data about the efficacy of GMV in older persons (aged >65 years) with diabetes; and (3) absence of evidence where the clinical GMV are led by a primary care physician (ie, the pivotal international studies had a specialist as the head of the healthcare team which limits the potential to ‘scale up’ the intervention).
This study will be the first RCT to evaluate GMV with a GP lead in diabetes management (previous comparable studies used an endocrinologist29 30 or internal medicine specialist.34 68 Also, no previous RCT has examined the trio of outcome categories (1) metabolic control (by HbA1c); (2) patient reported quality of life (EQ-5D); and (3) cost-utility (using QALYs calculated from the EQ-5D). It will also be one of the first studies to evaluate the efficacy of GMVs in promoting PA as measured objectively (SenseWear accelerometer).69 70
This study is an efficacy trial that if successful is intended to inform a potential province-wide (BC) implementation of this particular GMV healthcare service delivery model. Given this larger intention, it makes sense to have ‘Usual Care’ (individual visits) as our comparator given that Usual Care is the current standard of practice.
Our choice of single-blinding (measurement team) is the most reasonable in the light of the impossibility of the care providers leading the GMV to not know who was in their particular arm of the study. With 34 of 128 participants recruited, we have only a single physician within a single clinic involved in the study. At this point, there is no unequal expertise of care providers or centres in each group. We address the limitations below.
Limitations/generalisability
Currently, our RCT is limited to one geographic location and one clinical setting with a relatively homogeneous population; findings may not be generalisable to other regions, settings and/or demographic populations. Given that a single physician along with other specific healthcare professionals is leading the intervention, the findings may not be generalisable to other practitioners.
Conclusion
Our study will apply conceptual clinical innovations in GMV in the primary care setting to the health need of older adults with diabetes. There is a need for quantitative Canadian research in GMV broadly and we target the substantial clinical problem—diabetes in older people. Do primary care-led GMV reduce HbA1c and improve quality of life—and do they do so at a reasonable price? If the answer is encouraging, there is potential to ‘scale up’ the model via divisions, provinces and, ultimately, nationwide.
Footnotes
Contributors: KMK provided overall supervision for the protocol, advising on design, implementation, statistical analysis and the final manuscript and was the lead author of the manuscript. AW advised on study design and recruitment and led the Group Medical Visits. JCD oversaw the planned statistical analysis and advised on the final manuscript. MD, TL-A, KM, CAM, LH, CH and DJA advised on the design and implementation of the study, and on the final manuscript. All authors have approved the final article.
Funding: This study is funded through the UBC Endowment Fund (private donor). The BC Ministry of Health provided funding for Exercise is Medicine BC, through which this study was also partially funded. AW is supported through a UBC Department of Family Practice Clinician Scholar Award. TLA is CIHR Canada Research Chair in Physical Activity, Mobility, and Cognitive Neuroscience. JCD is funded by an MSFHR and a CIHR postdoctoral fellowship. Our Research Assistant is the recipient of a Canada Graduate Scholarships-Master's award. UBC's Department of Family Practice and Centre of Hip Health & Mobility provide operational support for the researchers. No funder played any role in the design, delivery or evaluation of the study.
Competing interests: None declared.
Ethics approval: UBC Clinical Research Ethics Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: We are open to data sharing as may be indicated for a meta-analysis, for example, in the future.
References
- 1.Booth G, Cheng AYY, Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2013 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes 2013; 37(Suppl 1):S4–7. [DOI] [PubMed] [Google Scholar]
- 2.Public Health Agency of Canada. Diabetes in Canada: facts and figures from a public health perspective 2011. Ottawa: Government of Canada, 2011. [Google Scholar]
- 3.Lysy Z, Booth G, Shah B et al. The impact of income on the incidence of diabetes: a population based study. Diabetes Res Clin Pract 2013;99:372–9. 10.1016/j.diabres.2012.12.005 [DOI] [PubMed] [Google Scholar]
- 4.Dyck R, Karunanayake C, Pahwa P et al. Prevalence, risk factors and co-morbidities of diabetes among adults in rural Saskatchewan: the influence of farm residence and agriculture-related exposures. BMC Public Health 2013;13:7 10.1186/1471-2458-13-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cauch-Dudek K, Victor JC, Sigmond M et al. Disparities in attendance at diabetes self-management education programs after diagnosis in Ontario, Canada: a cohort study. BMC Public Health 2013;13:85 10.1186/1471-2458-13-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meneilly G. Diabetes in the elderly. In: JE M, ed. Medical clinics of North America—geriatric medicine. Philadelphia, PA: Elsevier Saunders, 2006:909–23. [DOI] [PubMed] [Google Scholar]
- 7.Doucet G, Beatty M. The cost of diabetes in Canada: the economic tsunami. Can J Diabetes 2010;34:27–9. 10.1016/S1499-2671(10)41005-9 [DOI] [Google Scholar]
- 8.American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033–46. 10.2337/dc12-2625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caro J, Getsios D, Caro I et al. Economic evaluation of therapeutic interventions to prevent type 2 diabetes in Canada. Diabet Med 2004;21:1229–36. 10.1111/j.1464-5491.2004.01330.x [DOI] [PubMed] [Google Scholar]
- 10.Moffatt E, Shack L, Petz G et al. The cost of obesity and overweight in 2005: a case study of Alberta Canada. Can J Public Health 2011;102:144–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knowler WC. Prevention of type 2 diabetes: comment on Lifestyle modification and prevention of type 2 diabetes in overweight Japanese with impaired fasting glucose levels. Arch Intern Med 2011;171:1361–2. 10.1001/archinternmed.2011.367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steinsbekk A, Rygg L, Lisulo M et al. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with metaanalysis. BMC Health Serv Res 2012;12:213 10.1186/1472-6963-12-213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Umpierre D, Ribeiro P, Schaan B et al. Volume of supervised exercise training impacts glycaemic control in patients with type 2 diabetes: a systematic review with meta-regression analysis. Diabetologia 2013;56:242–51. 10.1007/s00125-012-2774-z [DOI] [PubMed] [Google Scholar]
- 14.Ferchak C, Meneghini L. Obesity, bariatric surgery and type 2 diabetes—a systematic review. Diabetes Metab Res Rev 2004;20:438–45. 10.1002/dmrr.507 [DOI] [PubMed] [Google Scholar]
- 15.Staimez L, Weber M, Narayan K et al. A systematic review of overweight, obesity, and type 2 diabetes among Asian American subgroups. Curr Diabetes Rev 2013;9:312–31. 10.2174/15733998113099990061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knowler W, Barrett-Connor PE, Fowler S et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403. 10.1056/NEJMoa012512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buehler A, Cavalcanti A, Berwanger O et al. Effect of tight blood glucose control versus conventional control in patients with type 2 diabetes mellitus: a systematic review with metaanalysis of randomized controlled trials. Cardiovasc Ther 2013;31:147–60. 10.1111/j.1755-5922.2011.00308.x [DOI] [PubMed] [Google Scholar]
- 18.Sayah FA, Williams B, Johnson J. Measuring health literacy in individuals with diabetes: a systematic review and evaluation of available measures. Health Educ Behav 2013;40:42–55. 10.1177/1090198111436341 [DOI] [PubMed] [Google Scholar]
- 19.Lindstroöm J, Ilanne-Parikka P, Peltonen M et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 2006;368:1673–9. 10.1016/S0140-6736(06)69701-8 [DOI] [PubMed] [Google Scholar]
- 20.Sanz C, Gautier JF, Hanaire H. Physical exercise for the prevention and treatment of type 2 diabetes. Diabetes Metab 2010;36:346–51. 10.1016/j.diabet.2010.06.001 [DOI] [PubMed] [Google Scholar]
- 21.Tabák A, Herder C, Rathmann W et al. Prediabetes: a high-risk state for diabetes development. Lancet 2012;379:2279–90. 10.1016/S0140-6736(12)60283-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alexander G, Sehgal N, Moloney R et al. National trends in treatment of type 2 diabetes mellitus, 1994–2007. Arch Intern Med 2008;168:2088–94. 10.1001/archinte.168.19.2088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Furler J, Hii J, Liew D et al. The “cost” of treating to target: cross-sectional analysis of patients with poorly controlled type 2 diabetes in Australian general practice. BMC Fam Pract 2013;14:32 10.1186/1471-2296-14-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teoh H, Després JP, Dufour R et al. Identification and management of patients at elevated cardiometabolic risk in canadian primary care: how well are we doing? Can J Cardiol 2013;29:960–8. 10.1016/j.cjca.2012.12.001 [DOI] [PubMed] [Google Scholar]
- 25.Bodenheimer T, Lorig K, Holman H et al. Patient self-management of chronic disease in primary care. JAMA 2002;288:2469–75. 10.1001/jama.288.19.2469 [DOI] [PubMed] [Google Scholar]
- 26.Bodenheimer T, Wagner E, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA 2002;288:1909–14. 10.1001/jama.288.15.1909 [DOI] [PubMed] [Google Scholar]
- 27.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002;288:1775–9. 10.1001/jama.288.14.1775 [DOI] [PubMed] [Google Scholar]
- 28.Northern Health Authority. The group medical appointment manual. 1st edn Northern Health Authority, 2007. [Google Scholar]
- 29.Trento M, Passera P, Tomalino M et al. Group visits improve metabolic control in type 2 diabetes: a 2-year follow-up. Diabetes Care 2001;24:995–1000. 10.2337/diacare.24.6.995 [DOI] [PubMed] [Google Scholar]
- 30.Trento M, ssera P, Borgo E et al. A 5-year randomized controlled study of learning, problem solving ability, and quality of life modifications in people with type 2 diabetes managed by group care. Diabetes Care 2004;27:670–5. 10.2337/diacare.27.3.670 [DOI] [PubMed] [Google Scholar]
- 31.Trento M, Gamba S, Gentile L et al. Rethink Organization to iMprove Education and Outcomes (ROMEO): a multicenter randomized trial of lifestyle intervention by group care to manage type 2 diabetes. Diabetes Care 2010;33:745–7. 10.2337/dc09-2024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sicuro J, Bondonio P, Charrier L et al. Cost analysis of group versus usual care in patients with type 2 diabetes in the ROMEO clinical trial. Nutr Metab Cardiovasc Dis 2013;23:e13–4. 10.1016/j.numecd.2012.11.005 [DOI] [PubMed] [Google Scholar]
- 33.Housden L, Wong S, Dawes M. Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. CMAJ 2013;185:E635–44. 10.1503/cmaj.130053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Edelman D, McDuffie J, Oddone E et al. Shared medical appointments for chronic medical conditions: a systematic review. VAESP Project #09-010, ed. Washington DC: Department of Veterans Affairs (US), 2012. [PubMed] [Google Scholar]
- 35.Folstein M, Folstein S, McHugh P. ‘Mini-mental state’: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 36.Blair S, Dunn A, Marcus B et al. Active living every day. Windsor: Human Kinetics, 2001. [Google Scholar]
- 37.Hologic Inc. Hologic QDR user's guide. Bedford, MA: Hologic Inc; 2000. [Google Scholar]
- 38.Washburn R, McAuley E, Katula J et al. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol 1999;52:643–51. 10.1016/S0895-4356(99)00049-9 [DOI] [PubMed] [Google Scholar]
- 39.Greene J, Hibbard J. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med 2011;27:520–6. 10.1007/s11606-011-1931-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood) 2013;32:207–14. 10.1377/hlthaff.2012.1061 [DOI] [PubMed] [Google Scholar]
- 41.Mosen D, Schmittdiel J, Hibbard J et al. Is patient activation associated with outcomes of care for adults with chronic conditions? J Ambulatory Care Manage 2007;30:21–9. 10.1097/00004479-200701000-00005 [DOI] [PubMed] [Google Scholar]
- 42.Deen D, Lu WH, Rothstein D et al. Asking questions: the effect of a brief intervention in community health centers on patient activation. Patient Educ Couns 2011;84:257–60. 10.1016/j.pec.2010.07.026 [DOI] [PubMed] [Google Scholar]
- 43.Hibbard J, Stockard J, Mahoney E et al. Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39: (4 Pt 1):1005–26. 10.1111/j.1475-6773.2004.00269.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Green C, Perrin N, Polen M et al. Development of the patient activation measure for mental health. Adm Policy Ment Health 2010;37:327–33. 10.1007/s10488-009-0239-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen J, Mortensen K, Bloodworth R. Exploring contextual factors and patient activation- evidence from a nationally representative sample of patients with depression. Health Educ Behav 2014;41:614–24. 10.1177/1090198114531781 [DOI] [PubMed] [Google Scholar]
- 46.Dixon A, Hibbard J, Tusler M. How do people with different levels of activation. Patient 2009;2:257–68. 10.2165/11313790-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 47.Kukla M, Salyers M, Lysaker P. Levels of patient activation among adults with schizophrenia: associations with hope, symptoms, medication adherence, and recovery attitudes. J Nerv Ment Dis 2013;201:339–44. 10.1097/NMD.0b013e318288e253 [DOI] [PubMed] [Google Scholar]
- 48.Wong S, Peterson S, Black C. Patient activation in primary healthcare. A comparison between healthier individuals and those with a chronic illness. Med Care 2011;49:469–79. 10.1097/MLR.0b013e31820bf970 [DOI] [PubMed] [Google Scholar]
- 49.Donald M, Ware R, Ozolins L et al. The role of patient activation in frequent attendance at primary care: a population-based study of people with chronic disease. Patient Educ Couns 2011;83:217–21. 10.1016/j.pec.2010.05.031 [DOI] [PubMed] [Google Scholar]
- 50.Hibbard J, Gilburt H. Supporting people to manage their health. An introduction to patient activation. London, UK: The King's Fund, 2014. [Google Scholar]
- 51.Hibbard JH, Mahoney E. Toward a theory of patient and consumer activation. Patient Educ Couns 2010;78:377–81. 10.1016/j.pec.2009.12.015 [DOI] [PubMed] [Google Scholar]
- 52.[No authors listed]. Reliability and validity of a diabetes quality-of-life measure for the diabetes control and complications trial (DCCT). The DCCT Research Group. Diabetes Care 1988;11:725–32. 10.2337/diacare.11.9.725 [DOI] [PubMed] [Google Scholar]
- 53.Dolan P, Roberts J. Modelling valuations for Eq-5d health states: an alternative model using differences in valuations. Med Care 2002;40:442–6. 10.1097/00005650-200205000-00009 [DOI] [PubMed] [Google Scholar]
- 54.Davis J, Liu-Ambrose T, Khan K et al. SF-6D and EQ-5D result in widely divergent incremental cost-effectiveness ratios in a clinical trial of older women: implications for health policy decisions. Osteoporos Int 2012;23:1849–57. 10.1007/s00198-011-1770-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Davis J, Marra C, Robertson M et al. Economic evaluation of dose-response resistance training in older women: a cost-effectiveness and cost-utility analysis. Osteoporos Int 2011;22:1355–66. 10.1007/s00198-010-1356-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Drummond M, Sculpher M, Torrance G et al. Methods for the economic evaluation of health care programmes. 3rd edn New York: Oxford University Press, 2005. [Google Scholar]
- 57.Kroenke K, Spitzer R, Williams J et al. Anxiety disorders in primary care: prevalence, imirment, comorbidity, and detection. Ann Intern Med 2007;146:317–25. 10.7326/0003-4819-146-5-200703060-00004 [DOI] [PubMed] [Google Scholar]
- 58.Hoppmann C, Coats A, Blanchard-Fields F. Goals and everyday problem solving: examining the link between age-related goals and problem-solving strategy use. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn 2008;15:401–23. 10.1080/13825580701533777 [DOI] [PubMed] [Google Scholar]
- 59.Slade L. Time-sampling research in health psychology: potential contributions and new trends. Eur Health Psychol 2011;13:65–9. [Google Scholar]
- 60.Hoppmann C, Gerstorf D. Spousal goals, affect quality, and collaborative problem solving: evidence from a time-sampling study with older couples. Res Hum Dev 2013;10:70–87. 10.1080/15427609.2013.760260 [DOI] [Google Scholar]
- 61.Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol 2008;57:1–29. 10.1111/j.1464-0597.2007.00325.x [DOI] [Google Scholar]
- 62.Liu-Ambrose T, Khan K, Eng J et al. The beneficial effects of group-based exercises on fall risk profile and physical activity persist 1year postintervention in older women with low bone mass: follow-up after withdrawal of exercise. J Am Geriatr Soc 2005;53:1767–73. 10.1111/j.1532-5415.2005.53525.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Davis J, Marra C, Beattie B et al. Sustained cognitive and economic benefits of resistance training among community-dwelling senior women: a 1-year follow-up study of the Brain Power study. Arch Intern Med 2010;170:2036–8. 10.1001/archinternmed.2010.462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pradhan A, Rifai N, Buring J et al. Hemoglobin A1c predicts diabetes but not cardiovascular disease in nondiabetic women. Am J Med 2007;120:720–7. 10.1016/j.amjmed.2007.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khaw K, Wareham N, Bingham S et al. Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk. Ann Intern Med 2004;141:413–20. 10.7326/0003-4819-141-6-200409210-00006 [DOI] [PubMed] [Google Scholar]
- 66.Kodama S, Horikawa C, Fujihara K et al. Use of high-normal levels of hemoglobin A1C and fasting plasma glucose for diabetes screening and prediction—a meta-analysis. Diabetes Metab Res Rev 2013;29:680–92. 10.1002/dmrr.2445 [DOI] [PubMed] [Google Scholar]
- 67.Bonora E, Tuomilehto J. The pros and cons of diagnosing diabetes with A1C. Diabetes Care 2011;34:S184–90. 10.2337/dc11-s216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Edelman D, Gierisch J, McDuffie J et al. Shared medical appointments for patients with diabetes mellitus: a systematic review. J Gen Intern Med 2015;30:99–106. 10.1007/s11606-014-2978-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Trost SG, O'Neil M. Clinical use of objective measures of physical activity. Br J Sports Med 2014;48:178–81. 10.1136/bjsports-2013-093173 [DOI] [PubMed] [Google Scholar]
- 70.Lee IM, Shiroma EJ. Using accelerometers to measure physical activity in large-scale epidemiological studies: issues and challenges. Br J Sports Med 2014;48:197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]


