Abstract
Topical latanoprost is a most effective and commonly used antiglaucoma medication. Use of prostaglandin analogues (PGA) in the early postoperative period is controversial due to its proinflammatory properties. We report a case of a 64-year-old man with primary open angle glaucoma, post-trabeculectomy 17 years prior, with good intraocular pressure (IOP) control on topical levobunolol 0.5% and latanoprost 0.005%. He underwent a clear corneal phacoemulsification surgery in his left eye and the PGA was stopped. He had an uneventful postoperative course and was prescribed eyeglasses at 4-week follow-up. Two weeks later, he presented to the emergency department with decreased vision in the left eye, flat anterior chamber, IOP of 00 mm Hg and 360° choroidal detachment. The continued use of topical latanoprost in the operated eye was implicated as the cause. This case illustrates the serious vision-threatening side effect of PGA when used in the early postoperative period.
Background
Latanoprost is a prostaglandin analogue (PGA) that helps to reduce intraocular pressure (IOP) by increasing the uveoscleral outflow.1 It is considered as a first-line drug in primary open angle glaucoma (POAG). It is known to cause several ocular side effects such as conjunctival hyperaemia, hypertrichosis and hyperpigmentation of periorbital skin, conjunctiva and iris. Postoperative use is known to cause intraocular inflammation and cystoid macular oedema.2 Uveal effusion after cataract surgery is associated with ocular injury, chronic uveitis, vascular diseases such as Sturge-Weber syndrome, malignancy and scleral abnormality of nanophthalmos or uveal effusion syndrome.3 Spontaneous choroidal detachment following an uncomplicated cataract surgery in an eye with normal ocular biometry is extremely rare. We report a case of extensive choroidal detachment with hypotony and severe visual disturbance following use of PGA after uneventful cataract surgery. The proinflammatory property along with the IOP lowering ability of PGA was implicated in the pathogenesis of this rare complication.
Case presentation
A 64-year-old man with known POAG, had trabeculectomy in both eyes 17 years prior. Currently, the IOP was under control with two topical antiglaucoma medications in both eyes. He was on levobunolol 0.5% eye drops two times per day and latanoprost 0.003% eye drops once at bedtime. Systemically, he had a 25-year history of type 2 diabetes mellitus controlled with oral medications.
He presented to us with symptoms of difficulty in distance and near vision in both eyes. His corrected visual acuity was 20/60 for distance and N12 for near with intraocular pressure of 14 mm Hg in both eyes. Anterior segment examination of both eyes showed low-to-flat trabeculectomy blebs and nuclear sclerosis grade II with 20% posterior subcapsular cataract. Gonioscopy revealed open angles in both eyes with patent superior osteum. Fundus examination showed 0.7 cup–disc ratio (CDR) with inferior notch in right eye and 0.8 CDR with inferior notch in left eye, with corresponding visual field defects. The patient underwent an uneventful topical clear corneal phacoemulsification with foldable posterior chamber intraocular lens (PCIOL) implantation in the left eye. The 2.8 mm clear corneal incision in the superonasal quadrant was closed with one 10-0 nylon suture, in order to prevent postoperative wound leak or hypotony. Postoperatively, the topical β-blocker medication was continued in both eyes and topical PGA was stopped in the operated left eye and continued only in the right eye. The routine postoperative medications, topical antibiotic eye drops for a week and tapering doses of topical steroids over 4 weeks were prescribed for his left eye. At 1 month postoperative follow-up, the patient's left eye had best corrected vision of 20/20, N6 with −1.75 dioptre cylinder at 85° and near addition of +3.00 dioptre sphere. IOP was 16 mm Hg in both eyes. He was advised to continue antiglaucoma medication (topical β-blocker medication in both eyes and topical PGA only in the right eye) and was advised to review after 2–3 months.
However, 2 weeks following this visit, the patient presented to the emergency department with a history of decreased vision in the left eye over 10 days. On examination, his left eye distance visual acuity was 20/200, improving to 20/100 with pin hole. Anterior segment examination revealed clear cornea with flat anterior chamber (AC) and 4 mm pupil, sluggishly reacting to light (figure 1), with resolving inflammatory membrane and pigments on the PCIOL. The IOP measured was 00 mm Hg in the left eye. The right eye had a deep AC and IOP was 16 mm Hg. Fundus examination revealed 360° peripheral choroidal detachment in the left eye.
Figure 1.
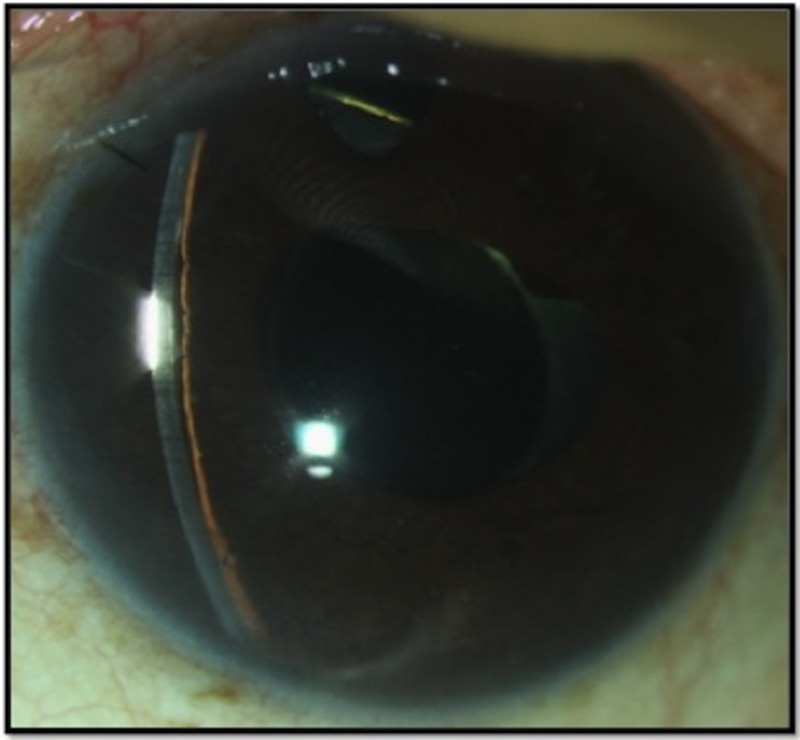
Slit lamp photograph showing flat anterior chamber with peripheral iridocorneal touch at presentation.
Investigations
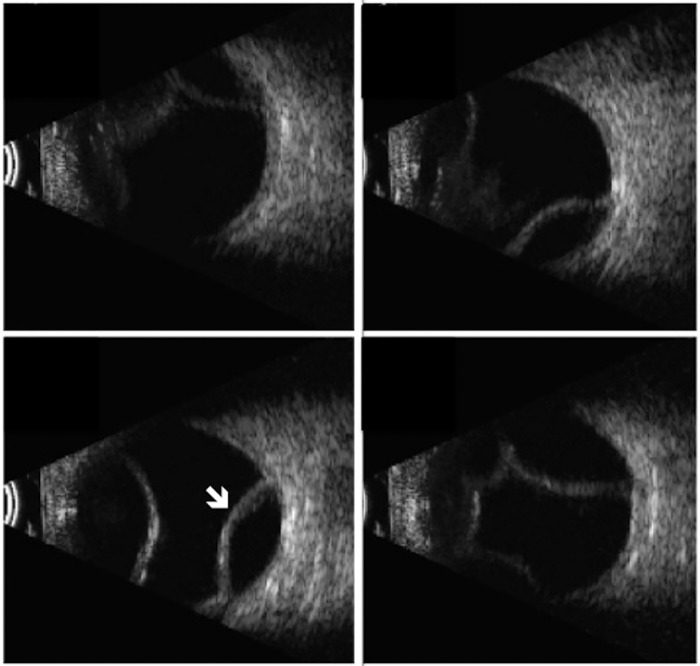
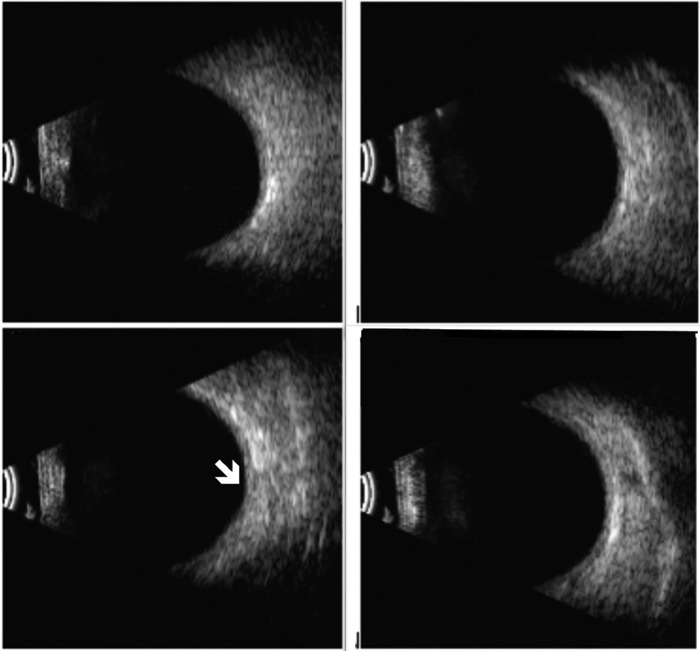
B-scan ultrasonography confirmed 360° choroidal detachment without retinal detachment (figure 2). Ultrasound biomicrosopy (UBM) revealed a flat AC with total iridocorneal touch, anterior rotation of the ciliary body and circumferential anterior choroidal detachment with inflammatory membranes in the suprachoroidal space (figure 3A, B).
Figure 2.
B scan ultrasonography showing 360° choroidal detachment without any retinal detachment (white arrow) at presentation.
Figure 3.
(A and B) Ultrasound biomicroscopy showing flat anterior chamber with peripheral iridocorneal touch (A) and multiple inflammatory membranes (white arrow) in the suprachoroidal space (B) at presentation.
Differential diagnosis
It would be prudent to rule out bleb leak or overfiltration of the bleb in an eye with prior filtration surgery. There was no evidence of thin cystic bleb or bleb leak in our case. There was no history of inadvertent trauma to the eye, which can cause hypotony with cyclodialysis cleft. Use of any sulfonamide group of medications, such as oral acetazolamide or topiramate, which may cause idiosyncratic reaction and uveal effusion, was also ruled out. Moreover, unilateral presentation in our case ruled out systemic medication as a causative factor.
Diagnosis
On revisiting the history, the patient gave a history of having restarted the topical PGA in the operated eye 10 days after the cataract surgery. Thus, use of topical PGA was implicated in the pathogenesis of this rare complication and the drug was discontinued in both eyes (to avoid even the contralateral effect of the drug).
Treatment
The patient was started on topical prednisolone acetate 1% every hourly and topical atropine 1% three times per day. He was also started on oral prednisolone 60 mg once a day with oral ranitidine hydrochloride 150 mg two times per day. The physician monitored his blood sugar levels and his blood pressure regularly.
Outcome and follow-up
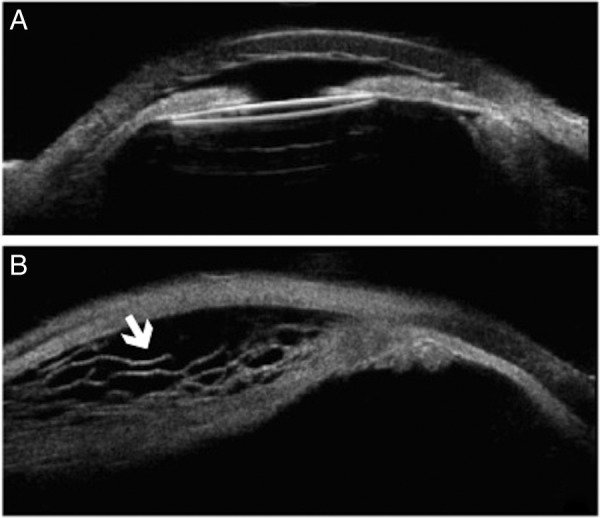
In the left eye, there was significant visual improvement up to 20/50 within 1 week of starting the treatment. The IOP was 03 mm Hg, with centrally deepened AC, but was still shallow peripherally. The choroidals were regressing, and more posterior compared with the first visit. The patient was advised to continue tapering doses of oral and topical steroids along with topical atropine 1% three times per day. By 12 weeks, his best-corrected vision returned to 20/20 with well-formed AC both centrally and peripherally (figure 4). IOP was 14 mm Hg with complete resolution of choroidal detachment on B scan (figure 5) and UBM (figure 6).
Figure 4.
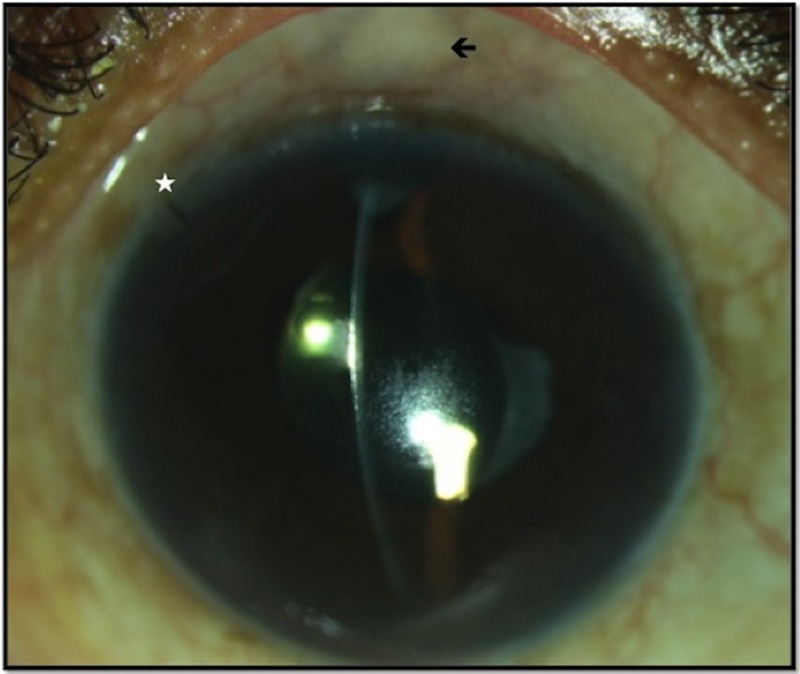
Slit lamp photograph showing deepened anterior chamber both centrally and peripherally (white asterisk showing one 10-0 nylon suture at the surgical entry site; black arrow showing low-to-flat bleb) by 12 weeks.
Figure 5.
B scan ultrasonography showing complete resolution of choroidal detachment (white arrow) by 12 weeks.
Figure 6.
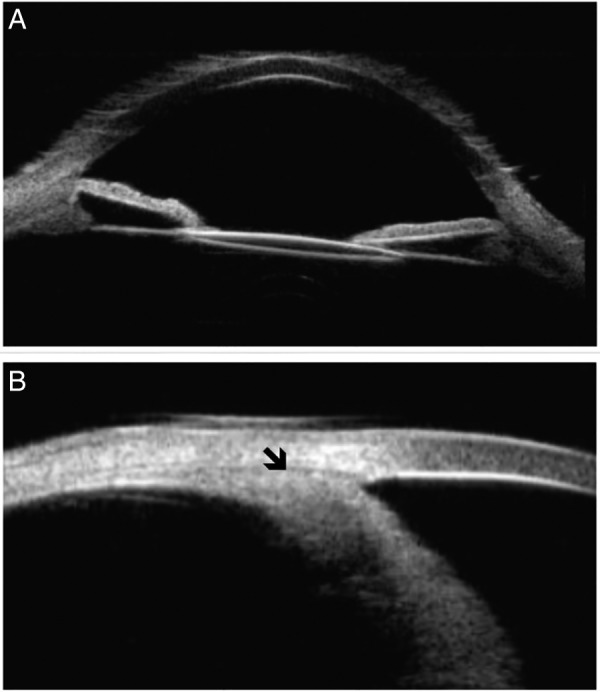
Ultrasound biomicroscopy showing deep AC (A) and a completely resolved choroidal detachment, as shown by black arrow (B) by 12 weeks.
Discussion
This case illustrates the rare association of topical PGA with choroidal effusion after uneventful cataract surgery. Latanoprost is a prostaglandin F2α analogue that reduces the IOP by increasing the uveoscleral outflow. Its mechanism of IOP reduction is complex and possibly mediated by its action on the extracellular matrix of the ciliary muscle, by activation of matrix metalloproteinases. As this is an IOP-independent mechanism, IOP may decrease much below the episcleral venous pressure.1
Our patient presented 7 weeks post-cataract surgery with flat AC with severe hypotony and 360° anterior ciliochoroidal detachment. The use of PGA in the early postoperative period was implicated as the cause for the inflammation and extensive ciliochoroidal detachment. There were extensive membranes noted in the suprachoroidal space (inflammatory) on UBM, which supports the inflammatory nature of the condition. Although PGA was started 10 days after the cataract surgery, the presentation was after 7 weeks, when the topical steroids were stopped. The topical steroids probably masked the proinflammatory effect of PGA, which flared up once it was discontinued.
Wu and Morrell have described a similar case with choroidal detachment following cataract extraction with continued use of PGA in an eye with POAG and previous trabeculectomy. The presentation was at 6 weeks, with a deep and quiet AC, IOP of 00 mm Hg, choroidal detachment in two quadrants and visual acuity of 20/80. Stopping the PGA and starting a short course (4 weeks) of topical steroids helped in the management. The sudden and significant (>50%) IOP reduction as a response to PGA in the postoperative period was postulated as the cause of choroidal detachment in this case and not the inflammatory response.4
Presentation of ciliochoroidal effusion on UBM with similar inflammatory membranes in the suprachoroidal space has been reported in a case of Sturge-Weber syndrome with glaucoma following use of PGA. This was spontaneous and had no history of intraocular surgery.3 Latanoprost-induced increased uveoscleral outflow in the presence of elevated episcleral venous pressure resulted in aqueous accumulation in the suprachoroidal space with resultant ciliochoroidal effusion and inflammation.
PGA being the first line of antiglaucoma medications in subjects with POAG,2 and considering the fact that many of these patients undergo cataract surgery, knowledge about this serious complication is very important. It would be safer to stop the PGA after cataract surgery and replace it with other antiglaucoma medications, such as aqueous suppressants, for 2–3 months until the blood aqueous barrier stabilises.5
Learning points.
Extensive choroidal detachment can occur with continued use of prostaglandin analogue after cataract surgery.
Choroidal detachment with severe hypotony and flat anterior chamber can be serious and vision-threatening.
Stopping the offending drug and conservative treatment with oral and topical steroids, and cycloplegics, would help to treat this rare complication successfully.
It may be ideal to stop prostaglandin analogue and preferably switch to another class of antiglaucoma medication in the early postoperative period.
Footnotes
Contributors: SS, RK and CSG contributed in conception, design, acquisition and interpretation of data. SS and RK contributed in drafting the article and revising it critically for important intellectual content to get the article published.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Yalvac IS, Tamcelik N, Duman S. Acute angle-closure glaucoma associated with latanoprost. Jpn J Ophthalmol 2003;47:530–1. 10.1016/S0021-5155(03)00127-8 [DOI] [PubMed] [Google Scholar]
- 2.Alm A, Stjernschantz J. Effects on intraocular pressure and side effects of 0.005% latanoprost applied once daily, evening or morning. A comparison with timolol. Scandinavian Latanoprost Study Group. Ophthalmology 1995;102:1743–52. 10.1016/S0161-6420(95)30798-1 [DOI] [PubMed] [Google Scholar]
- 3.Sakai H, Sakima N, Nakamura Y et al. . Ciliochoroidal effusion induced by topical latanoprost in a patient with sturge-weber syndrome. Jpn J Ophthalmol 2002;46:553–5. 10.1016/S0021-5155(02)00542-7 [DOI] [PubMed] [Google Scholar]
- 4.Wu G, Morrell A. Severe hypotony following cataract extraction in a patient on latanoprost. Eye 2000;14(Pt 6):915–16. 10.1038/eye.2000.255 [DOI] [PubMed] [Google Scholar]
- 5.Gupta R, Vernon SA. Choroidal detachment following extracapsular cataract extraction in a patient treated with latanoprost. Br J Ophthalmol 2001;85:1268 10.1136/bjo.85.10.1268 [DOI] [PMC free article] [PubMed] [Google Scholar]