Abstract
De Garengeot hernia is a rare clinical entity defined as the presence of a vermiform appendix within a femoral hernia sac. A 50-year-old woman presented to the emergency department with a painful lump over her right groin region. A bedside ultrasound was performed and soft tissue lesion was suspected. CT was performed and revealed a swollen tubular structure with fat stranding within the mass. De Garengeot hernia with acute appendicitis was diagnosed preoperatively, and an emergency appendectomy and hernioplasty were performed. Although it is usually an incidental finding during hernioplasty, De Garengeot hernia should be considered in the differential diagnosis of patients with an incarcerated femoral hernia. Mesh repair can be performed depending on the clinical situation. We report a rare case of incarcerated femoral hernia with acute appendicitis that required early surgical management to avoid associated complications.
Background
A femoral hernia presents as a sac protruding through the femoral triangle below the inguinal ligament and is incarcerated in more than half of these patients. Owing to the narrow and rigid ring, the hernia has a high risk of incarceration and strangulation.1 De Garengeot hernia, named in 1731 after the Parisian surgeon Rene Jacques Croissant De Garengeot (1688–1759), is defined as a vermiform appendix located within a femoral hernia sac with or without inflammation.2 In 1785, the first appendectomy in an incarcerated femoral hernia was performed by Hevin.1 Abnormal implantation of the appendix in the caecum leading to a pelvic appendix or a large caecum with increased mobility extending into the pelvis can further lead to incarceration of the appendix in a femoral hernia sac, and both are considered in the pathogenesis of De Garengeot hernia. It is a rare clinical entity with fewer than 100 cases reported, of which less than 15 cases have been diagnosed by preoperative CT imaging.3 4 To the best of our knowledge, this is the second case of De Garengeot hernia reported from Asia. Because early recognition of this clinical condition is important to avoid subsequent complications, we report this rare case of incarcerated femoral hernia with acute appendicitis.
Case presentation
A previously healthy 50-year-old woman presented to the emergency department with a 4 h history of sudden onset of a painful lump over her right groin region. On clinical examination, a fixed, firm, round, irreducible, tender mass approximately 3×5 cm in diameter, and located lateral and inferior to the pubic tubercle, was found. No erythaematous changes, abrasion or purulent discharge was seen. The patient did not report of abdominal pain in the right lower quadrant, nausea, vomiting, fever or diarrhoea. An old surgical scar located on the right lateral to the pubic tubercle was noted, and, according to the patient, was the result of resection of a skin lesion.
Investigations
On auscultation, bowel sounds were neither increased nor decreased. The entire abdomen was soft and non-tender. Vital signs evaluation revealed a temperature of 36.8°C, blood pressure of 149/96 mm Hg, heart rate of 90 bpm and respiratory rate of 20 breaths per minute. All laboratory results were within normal limits, including a white cell count of 6.6×109/L without a predominance of neutrophils and a C reactive protein (CRP) of <0.1 mg/dL.
Differential diagnosis
A bedside sonogram was performed and a soft tissue mass was suspected. Thus, there was a possibility of the lesion being more than an incarcerated inguinal hernia, and of it being a malignant or benign tumour. Therefore, a further CT scan was performed to determine the differential diagnosis and subsequent treatment plan. It revealed one tubular structure extending from the caecal base into the groin mass (figure 1). De Garengeot hernia was diagnosed.
Figure 1.
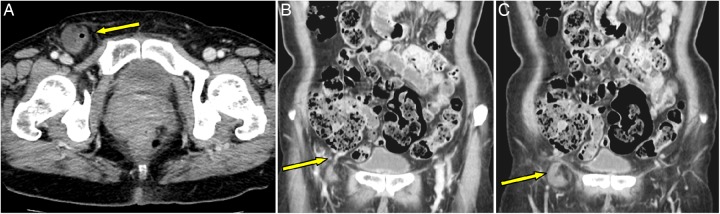
Contrast-enhanced CT scan of the abdomen. (A) Axial view: tubular structure containing gas within the femoral mass located lateral and inferior to the pubic tubercle; (B) Coronal view: tubular structure extending from the caecal base; (C) Coronal view: swelling of a tubular structure with mild fat stranding.
Treatment
The preprocedural CT confirmed the diagnosis before surgery. We decide to conduct surgery based on our previous experience and because it would provide the best outcome: appendectomy for acute appendicitis and hernioplasty for femoral hernia.
The patient immediately received intravenous fluid and antibiotics (cefazolin, 1.0 g; gentamycin, 80 mg; and metronidazole, 500 mg) and was taken into the operating room. Under general anaesthesia, a groin exploration was performed through a lower inguinal incision. When the hernia sac was opened, an inflamed and gangrenous appendix protruding through the femoral sac was seen (figures 2 and 3). A turbid fluid collection was also seen, but no obvious perforation was noted. The rigid femoral ring was identified. A routine appendectomy was performed through the femoral sac after the caecum and base of the appendix were identified. The femoral sac was transfixed with 2–0 Prolene. No mesh was used due to the possibility of a deep wound infection. The hernia defect was repaired with a non-absorbable suture using the McVay technique. The wound was closed in layers using absorbable sutures for the deep subcutaneous tissues and 3–0 Nylon for the skin. No complication, such as wound infection, pain or sepsis, was noted. The treatment outcome was assessed when the patient revisited the outpatient department of our hospital.
Figure 2.

A grossly gangrenous and inflamed appendix grasped with Babcock forceps, and a thickened hernia sac grasped with mosquito forceps.
Figure 3.
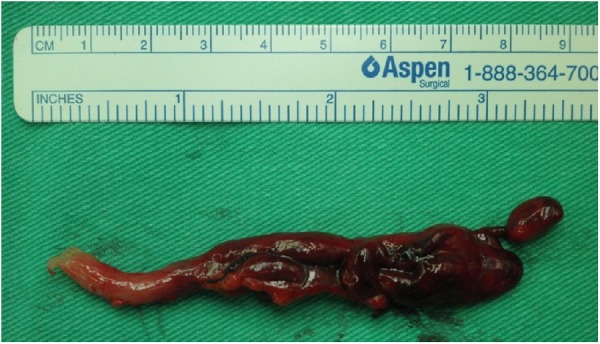
Resected appendix with gross gangrenous and inflammatory changes.
Outcome and follow-up
Histological examination revealed congestion of the appendix and haemorrhage in the periappendiceal soft tissue. The neutrophilic infiltration was inconspicuous. The postoperative course was uneventful, and the patient was discharged on postoperative day 4. She returned to the outpatient department 1 week later for suture removal, and no wound infection or other complication was found.
Discussion
Femoral hernias account for <10% of all hernias.5 De Garengeot hernia is rare, accounting for 0.8–1% of femoral hernias.2 De Garengeot hernia should not be confused with Amyand's hernia, in which the appendix lies within the inguinal hernia sac.6
Because it is a subgroup, the female-to-male incidence ratio of De Garengeot hernia is the same as for femoral hernia (3:1, female:male).4 The high prevalence among women has been attributed to body changes during pregnancy. Other risk factors include increased intra-abdominal pressure, smoking, advanced age and collagen disease.4 Most De Garengeot hernias occur on the right side.4
The rarity of De Garengeot hernia may be attributed to anatomic position and rotation of the bowel, or to anatomic variation in caecal mobility. It has been suggested that a very large caecum that expands into the pelvis can cause the appendix to enter a hernia sac.7 There are several theories about the cause of appendicitis. Some suggest that intraluminal obstruction initiates inflammatory changes in the appendix leading to subsequent migration of the appendix into the hernia sac. However, others suggest migration of the appendix is the initial event, and the narrow rigid neck of the femoral sac causes incarceration and strangulation of the appendix.8 This seems consistent with our patient because no obvious intraluminal obstruction was noted and haemorrhage in the periappendiceal soft tissue was present.
These patients usually present to the emergency department reporting of a several-day history of a painful, irreducible groin lump with local erythaematous changes. Most do not have abdominal pain, nausea, vomiting, diarrhoea or abdominal fullness. Physical examination may reveal an elevated body temperature, tachycardia and hypotension. Laboratory findings often show an elevated white cell count and CRP.1 3–20
Most De Garengeot hernias are diagnosed intraoperatively. Only 15 cases, including this one, in which the diagnosis was performed by preprocedural CT, have been reported, and only two cases are reported to have been diagnosed by sonogram.5 14 Thus, an appropriate diagnostic imaging study should be performed preoperatively to determine the differential diagnosis of an inguinal mass, which may include neoplasm, inflammatory conditions, hernia and vascular lesions.21 Abdominal radiographs may be used to exclude intestinal obstruction. Sonogram is helpful for identifying soft tissue lesions or fluid collection.4 CT has been proven to the most useful tool and to have the highest sensitivity and specificity for diagnosing De Garengeot hernia.3 The findings of a low-positioned caecum with a blind-ended tubular structure within the hernia sac and stranding of nearby fat on CT scan reportedly have 98% sensitivity and specificity16 for diagnosing or ruling out appendicitis within a hernia sac. The CT image also provides additional information about what might be encountered during surgery.12
Currently, treatment of this disease is emergency surgery. Owing to the rigid ring of the femoral hernia, a limited surgical approach is preferred in order to confine the infection within the hernia sac and avoid peritoneal contamination once perforation or abscess formation is noted. Thus, in the majority of the literature, a low-curved inguinal approach is the preferred method and provides adequate exposure.7 Occasionally, a midline or McBurney incision is needed for exposure of the caecal base. Total laparoscopic appendectomy accompanied by hernioplasty, using either a total extraperitoneal approach or transabdominal preperitoneal approach, has been reported.22 However, more studies comparing laparoscopic to open surgical techniques are needed to determine its advantages and disadvantages. The major complication of De Garengeot hernia repair is wound infection, which has been reported to occur in 14–29% of cases.1 Thus, whether or not to use mesh has become an issue in past decades. Currently, the consensus is that mesh repair is an acceptable option if there is no perforation or abscess formation. Wound infection has been related to delayed diagnosis and treatment, and is often seen in elderly patients.23 Rare but serious complications, such as necrotising fasciitis and death, have been reported.1
Learning points.
De Garengeot hernia is the presence of the appendix (normal or inflamed) within a femoral hernia sac.
It can be diagnosed when a CT scan is performed to determine the differential diagnosis of an acute groin mass. Most commonly, however, it is diagnosed intraoperatively.
Once diagnosed, an early operation should be performed to avoid serious complications and morbidity.
Footnotes
Contributors: M-JT was involved in the study supervision, patient management. CWP was involved in the data collection and analysis, data interpretation, manuscript writing. M-SS was involved in the critical review of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Sharma H, Jha PK, Shekhawat NS et al. De Garengeot hernia: an analysis of our experience. Hernia 2007;11:235–8. 10.1007/s10029-007-0208-5 [DOI] [PubMed] [Google Scholar]
- 2.Akopian G, Alexander M. De Garengeot hernia: appendicitis within a femoral hernia. Am Surg 2005;71:526–7. [PubMed] [Google Scholar]
- 3.Ahmed K, Bashar K, McHugh TJ et al. Appendicitis in De Garengeot's Hernia presenting as a nontender inguinal mass: case report and review of the literature. Case Rep Surg 2014;2014:932638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kalles V, Mekras A, Mekras D et al. De Garengeot's hernia: a comprehensive review. Hernia 2013;17:177–82. 10.1007/s10029-012-0993-3 [DOI] [PubMed] [Google Scholar]
- 5.Schafer HM, von Holzen U, Nebiker C. Swelling of the right thigh for over 30 years-the rare finding of a De Garengeot hernia. Int J Surg Case Rep 2014;5:1120–2. 10.1016/j.ijscr.2014.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caygill P, Nair R, Sajjanshetty M et al. An unusual groin exploration: De Garengeot's hernia. Int J Surg Case Rep 2011;2:74–5. 10.1016/j.ijscr.2011.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Piperos T, Kalles V, Al Ahwal Y et al. Clinical significance of de Garengeot's hernia: a case of acute appendicitis and review of the literature. Int J Surg Case Rep 2012;3:116–17. 10.1016/j.ijscr.2011.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hussain A, Slesser AA, Monib S et al. A De Garengeot hernia masquerading as a strangulated femoral hernia. Int J Surg Case Rep 2014;5:656–8. 10.1016/j.ijscr.2014.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Talini C, Oliveira LO, Faria Araújo AO et al. De Garengeot hernia: case report and review. Int J Surg Case Rep 2015;8C:35–7. 10.1016/j.ijscr.2014.12.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Snoekx R, Geyskens P. De Garengeot's hernia: acute appendicitis in a femoral hernia. Case report and literature overview. Acta Chir Belg 2014;114:149–51. [PubMed] [Google Scholar]
- 11.Ramsingh J, Ali A, Cameron C et al. De Garengeot's hernia: diagnosis and surgical management of a rare type of femoral hernia. J Surg Case Rep 2014;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hau DL, Odom SR, Hsu A et al. A combined Richter's and de Garengeot's hernia. Int J Surg Case Rep 2014;5:662–4. 10.1016/j.ijscr.2014.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah A, Sira Janardhan H. De garengeot hernia: a case report and review of literature. Indian J Surg 2013;75:439–41. 10.1007/s12262-012-0778-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erdas E, Sias L, Licheri S et al. De Garengeot hernia with acute appendicitis. G Chir 2013;34:86–9. [PubMed] [Google Scholar]
- 15.Salkade PR, Chung AY, Law YM. De Garengeot's hernia: an unusual right groin mass due to acute appendicitis in an incarcerated femoral hernia. Hong Kong Med J 2012;18:442–5. [PubMed] [Google Scholar]
- 16.Konofaos P, Spartalis E, Smirnis A et al. De Garengeot's hernia in a 60-year-old woman: a case report. J Med Case Rep 2011;5:258 10.1186/1752-1947-5-258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas B, Thomas M, McVay B et al. De Garengeot hernia. JSLS 2009;13:455–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Rajan SS, Girn HR, Ainslie WG. Inflamed appendix in a femoral hernial sac: de Garengeot's hernia. Hernia 2009;13:551–3. 10.1007/s10029-009-0472-7 [DOI] [PubMed] [Google Scholar]
- 19.Ebisawa K, Yamazaki S, Kimura Y et al. Acute appendicitis in an incarcerated femoral hernia: a case of De Garengeot Hernia. Case Rep Gastroenterol 2009;3:313–17. 10.1159/000250821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chung A, Goel A. Images in clinical medicine. De Garengeot's hernia. N Engl J Med 2009;361:e18 10.1056/NEJMicm0802611 [DOI] [PubMed] [Google Scholar]
- 21.Allen BC, Kirsch J, Szomstein S. Case 187: De Garengeot hernia. Radiology 2012;265:640–4. 10.1148/radiol.12102051 [DOI] [PubMed] [Google Scholar]
- 22.Beysens M, Haeck L, Vindevoghel K. Laparoscopic appendectomy combined with TEP for de Garengeot hernia: case report. Acta Chir Belg 2013;113:468–70. [PubMed] [Google Scholar]
- 23.Kagan Coskun A, Kilbas Z, Yigit T et al. De Garengeot's hernia: the importance of early diagnosis and its complications. Hernia 2012;16:731–3. 10.1007/s10029-011-0814-0 [DOI] [PubMed] [Google Scholar]


