Abstract
Background and purpose
Poor outcomes have been linked to errors in rotational alignment of total knee arthroplasty components. The aims of this study were to determine the correlation between rotational alignment and outcome, to review the success of revision for malrotated total knee arthroplasty, and to determine whether evidence-based guidelines for malrotated total knee arthroplasty can be proposed.
Patients and methods
We conducted a systematic review including all studies reporting on both rotational alignment and functional outcome. Comparable studies were used in a correlation analysis and results of revision were analyzed separately.
Results
846 studies were identified, 25 of which met the inclusion criteria. From this selection, 11 studies could be included in the correlation analysis. A medium positive correlation (ρ = 0.44, 95% CI: 0.27–0.59) and a large positive correlation (ρ = 0.68, 95% CI: 0.64–0.73) were found between external rotation of the tibial component and the femoral component, respectively, and the Knee Society score. Revision for malrotation gave positive results in all 6 studies in this field.
Interpretation
Medium and large positive correlations were found between tibial and femoral component rotational alignment on the one hand and better functional outcome on the other. Revision of malrotated total knee arthroplasty may be successful. However, a clear cutoff point for revision for malrotated total knee arthroplasty components could not be identified.
About 1 in 5 TKA patients are dissatisfied with the outcome (Bourne et al. 2010). A systematic review by the European Arthroplasty Register reported the results of 6 national joint registry datasets. A combined revision rate of 1.3 revisions per 100 observed component years after primary TKA was reported, and revision rates of about 6% after 5 years and 12% after 10 years are to be expected (Labek et al. 2011). Many possible causes of painful or malfunctioning TKAs have been defined, but the true cause often remains unknown (Thornhill 2002, Dennis 2004, Toms et al. 2009). Rotational errors of TKA components are frequently overlooked as the origin of problems, which can lead to unnecessary procedures (Bedard et al. 2011). Poor outcomes and major complications—e.g. patellofemoral pain, instability, and stiffness after TKA—have been linked to errors in rotational alignment of the components (Mochizuki and Schurman 1979, Rhoads et al. 1990, Berger et al. 1998, Miller et al. 2001, Sikorski 2008). Thus, the aims of the present study were (1) to examine the correlation between rotational alignment of the TKA component and outcome, (2) to review the results of revision operations for rotational malaligned TKA, and (3) to investigate whether practical recommendations can be made to guide treatment of a rotational malaligned TKA.
Patients and methods
Identification of studies
A comprehensive literature search was performed with the assistance of a medical librarian, using the following search terms: arthroplasty, replacement, knee, total knee, prosthesis, TKA, TKP, TKR, primary, revision, rotation, rotational error, axis, angle, malalignment, posterior condylar angle, posterior condylar line, surgical epicondylar axis, condylar twist angle, and rotational alignment. The search was limited to adults in the following databases: PubMed/Medline, the Cochrane Clinical Trial Register, and Embase. Studies were searched in the period from 1993 to May 2014. The reference lists obtained of retrieved publications were manually checked for additional references that possibly met the inclusion criteria, which were missed in the electronic search.
Inclusion and exclusion criteria
We used Prisma methodology for the analysis and reporting of the systematic review (Moher et al. 2009). Titles and abstracts from potentially relevant studies were reviewed using a set of predefined inclusion and exclusion criteria. All articles from 1993 onward that presented data on rotational errors in primary and revision TKA and outcome scores were included for further data extraction if the criteria were met. Rotational alignment of the components had to have been judged according to a specific protocol with the results presented as rotational degrees of malalignment and a functional objective and/or subjective validated outcome measure had to have been used. The year 1993 was chosen as a cutoff point because in that year, a standardized CT method was introduced that assessed rotational alignment in TKA (Berger et al. 1993b). Revision was defined as any surgical procedure that resulted in the removal or exchange of any of the arthroplasty components. All types of TKAs and all reasons for the primary or revision operation were included. Radiological studies presenting CT and/or MRI data were included. Radiological studies presenting data from conventional X-ray imaging and articles confined to the clinical judgement of rotation were excluded since these methods are less accurate. Review articles and expert opinions were excluded because these articles do not report on original patient data. Abstracts from scientific meetings without a full-text published article were also excluded. The search was restricted to articles written in English, German, French, or Dutch. Articles presenting data supposedly presented previously were used once. 2 reviewers (KV and SB) independently reviewed the literature searches, using the titles and abstracts to identify relevant articles for full review. From the full text, the reviewers independently selected articles for inclusion in this review using the above-mentioned criteria. Disagreement was resolved by group discussion; with arbitration by a third author (MB) when differences of opinion remained. Studies were not coded regarding author, affiliation, and source.
Data extraction
After the initial assessment for inclusion, the following data were extracted from the articles selected: number of procedures, time from index operation, primary TKA and/or revision TKA, prosthesis type (cruciate retaining, posterior stabilized), bearing type (mobile, fixed), patella resurfacing, study inclusion criteria, functional assessment, type of rotational malalignment measured (femoral, tibial, combined, and mismatch) (Nicoll and Rowley 2010) and imaging protocol. Studies with similar protocols for determining both the rotation of the individual TKA components and the functional outcome were used in the correlation analysis. Data on the results of revision for TKA malrotation were also analyzed separately.
The methodological quality of the studies included was assessed by assigning levels of evidence as defined by the Oxford Centre for Evidence-Based Medicine (Howick et al. 2011). Levels of evidence were assigned by KV and SB. Disagreement was resolved by consensus. Based on the levels of evidence, some recommendations for clinical practice were formulated. A grade was added, based on the evidence supporting that recommendation (Guyatt et al. 2008).
Statistics
Statistical analysis was done using IBM SPSS version 21.0. The mean femoral or tibial rotation, the mean total Knee Society score (KSS), and the number of patients from each article selected was entered in SPSS. In the analysis, the rotation and total KSS were weighted by the number of patients. Normal distribution was tested by calculating the skew and kurtosis, evaluating frequency histograms, and performing the Shapiro-Wilcoxon test. Degree of correlation (with 95% confidence intervals (CIs)) between femoral rotation and total KSS and between tibial rotation and total KSS was calculated. The preferred test for correlation analysis depends on the distribution of the data; Pearson’s correlation assumes equal interval data that are normally distributed. Spearman’s rho (ρ) is used on the ranks of the data. It is a non-parametric estimation of the correlation and is thereby less sensitive to outliers than Pearson’s correlation coefficient. Because the variables were not normally distributed, a Spearman’s rho bivariate correlational statistical method was used. In this analysis for non-parametric correlations, cases were weighted by the number of patients in the study and significance was set at the 1% (0.01) level. A small effect size is defined as rho between 0.10 and 0.30, a medium effect size as rho between 0.30 and 0.50, and a large effect size is operationally defined as one that yields rho ≥ 0.50 (Cohen 1988).
Registration
This systematic review was registered and published on the Prospero database (number CRD42014007096) (Booth et al. 2013).
Results
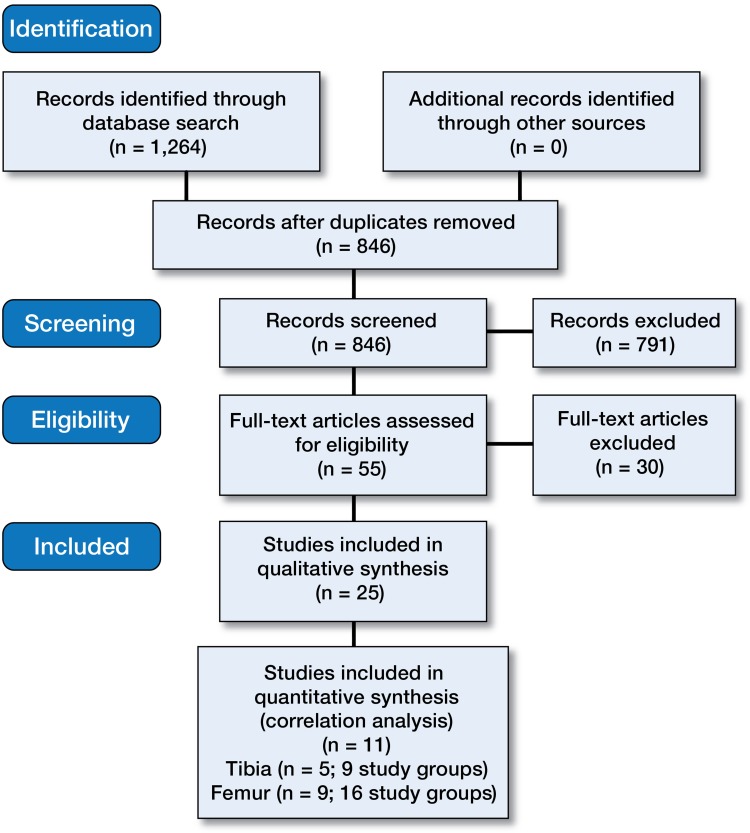
The primary search, performed in May 2014, yielded 846 unique studies (Figure 1). 25 studies finally met the inclusion criteria and were included (Table 1, see Supplementary data). No more articles could be identified after manually checking the retrieved publications for additional references that might meet the inclusion criteria.
Figure 1.
Prisma flow diagram of the systematic literature review.
The 25 studies included were published over 12 years. 2 studies were classified as level I, 7 as level II, 9 as level III, and 7 as level IV. These studies each involved 13–146 knees and together they covered 1,494 knees that had both rotational and functional assessment after TKA. 7 studies compared malrotation and asymptomatic cohorts, 2 compared malrotation and aseptic loosening cohorts, 4 compared computer-assisted surgery (CAS) with jig-based TKA, 1 compared CAS with articular surface-mounted CAS, 1 compared patient-specific instrumentation with jig-based TKA, and 2 compared fixed-bearing with mobile-bearing TKA. 4 symptomatic cohorts and 4 random TKA cohorts were reported. The mean documented time from the index surgery varied from 6 months to 10 years. The inclusion criteria in the studies were: (anterior) knee pain, stiffness, failure of patella prosthesis, instability, and primary TKA for osteoarthritis.
The functional assessments were done with the (inverted) Oxford 12-item knee questionnaire, the Hospital for Special Surgery knee score (HSS), the Western Ontario and McMaster Universities arthritis index (WOMAC), and the KSS. The KSS has 3 components (knee, function, and pain) and the studies reported separate components and combinations of components. Femoral rotation was measured in 24 studies, tibial rotation in 18 studies, combined rotation in 9 studies, and mismatch in rotation in 7 studies. For both femur and tibia, 5 different CT rotation protocols were used to measure component rotation. Due to limited numbers of comparable studies reporting combined rotation and mismatch in rotation, a corresponding quantitative analysis was not possible. 8 studies could not be included in the correlation analysis due to either inconsistent reporting of the measured rotation impeding linkage to the functional assessment (Hofmann et al. 2003, Longstaff et al. 2009, Bedard et al. 2011), or inconsistent reporting of the KSS total score impeding linkage to the measured rotation (Sensi et al. 2011). Furthermore, 4 studies were excluded because only the Knee Society knee score was reported instead of the combined knee and function score (Matsuda et al. 2001, Lakstein et al. 2010, Matsuda et al. 2010, Pietsch and Hofmann 2012).
11 studies could be included in the quantitative analysis (Barrack et al. 2001, Kienapfel et al. 2003, Mizu-uchi et al. 2008, Fosco et al. 2010, Nicoll and Rowley 2010, Harvie et al. 2011, Sternheim et al. 2012, Zhang et al. 2012, Lad et al. 2013, Huang et al. 2013, Woolson et al. 2014). These studies used similar protocols for determination of both the rotation of the individual TKA components and the functional outcome. In this quantitative correlation analysis of the tibia (Barrack et al. 2001, Fosco et al. 2010, Nicoll and Rowley 2010, Sternheim et al. 2012, Zhang et al. 2012) and the femur (Kienapfel et al. 2003, Mizu-uchi et al. 2008, Fosco et al. 2010, Harvie et al. 2011, Sternheim et al. 2012, Zhang et al. 2012, Lad et al. 2013, Huang et al. 2013, Woolson et al. 2014), 9 and 16 study groups, respectively, were included (11 articles). In these study groups, CT scans were used to assess the rotational alignment of the components and the KSS consisted of a combination of the knee score and the functional score for functional assessment. The studies included used the CT scan protocols according to the Berger protocol without sex differences, and the identical Perth CT protocol for measurement of femoral rotation. For the tibial component, the Berger protocol was used. In the Perth CT protocol (Chauhan et al. 2004), tibial rotation is described relative to the femoral component rather than relative to a bony landmark. Isolated tibial rotation is therefore not measured. These combinations of CT scan and functional assessment yielded the most study groups for analysis.
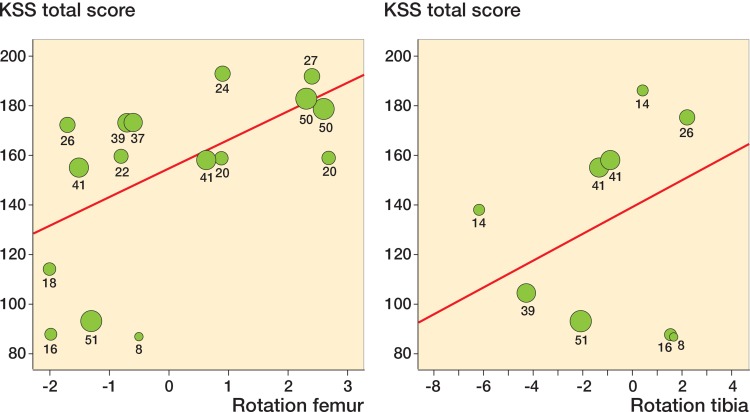
In the tibial correlation analysis, 9 study groups involving 250 patients were included. There was a positive correlation between more external rotation of the tibial component and higher total KSS (ρ = 0.44, 95% CI: 0.27–0.59). In the femoral correlation analysis, 16 study groups with a total of 490 patients were included. There was a positive correlation between more external rotation of the femoral component and higher total KSS (ρ = 0.68, 95% CI: 0.64–0.73) (Figure 2).
Figure 2.
Correlation scatter plot of total KSS score and rotational alignment for femur (left) and tibia (right). Femur rotation of 0° represents alignment parallel to the surgical transepicondylar axis. Tibial rotation of 0° represents neutral alignment according to the Berger CT protocol (18° of internal rotation relative to the tibial tuberosity). Negative rotation represents internal rotation; positive rotation represents external rotation. Cases were weighted by number of patients, and numbers of cases are shown under the dots.
6 studies could be identified that had results of revision for malrotation (Table 2, see Supplementary data). These studies represented the results of 173 patients. In cases where data were missing, the original data from the studies were used to calculate rotational measurements and functional outcomes when available. All the revision studies used the Berger protocol for assessment of component rotation. For assessment of tibial rotation the revision studies used Berger protocol. However, for assessment of femoral rotation, some studies used the Berger protocol with sex differences (Lakstein et al. 2010, Bedard et al. 2011) and others did not (Hofmann et al. 2003, Pietsch and Hofmann 2012, Sternheim et al. 2012). The data of Fosco et al. (2010) were available, and recalculations were done according to the Berger protocol without sex differences, in order to give more valuable data. Indications for operation were stiffness (Fosco et al. 2010, Bedard et al. 2011, Pietsch and Hofmann 2012, Sternheim et al. 2012), instability (Hofmann et al. 2003), and pain (Hofmann et al. 2003, Fosco et al. 2010, Lakstein et al. 2010, Sternheim et al. 2012) combined with component malrotation of more than 2 (Sternheim et al. 2012), 3 (Lakstein et al. 2010), 4 (Pietsch and Hofmann 2012), or 5 (Hofmann et al. 2003) degrees or combined malrotation of more than 3 (Sternheim et al. 2012) or 4 (Fosco et al. 2010) degrees. All studies reported improvement in functional results according to the KSS and its subdivisions (knee, function, and pain) and the HSS score.
Discussion
We found positive correlations between rotational alignment of the tibial and femoral components on the one hand and the KSS on the other. We also found that revision of malrotated total knee arthroplasty may be a successful procedure. However, due to several limitations, a clear cutoff point for revision of malrotated total knee arthroplasty components could not be identified.
CT rotation protocol
Because of the differences in assessments and CT protocols in the studies included, it is difficult to compare and meta-analyze the results. Most studies used Berger’s CT protocol to measure the rotation of components (Berger et al. 1993b, Berger and Crossett 1998). In this protocol, different native rotation values of the posterior condylar angle for males and females are used as a reference. These values were based on a cadaveric study with 20 male femurs and 15 female femurs (Berger et al. 1993a). Sex differences for the posterior condylar angle could not be confirmed in other studies (Yoshioka et al. 1987, Mantas et al. 1992, Poilvache et al. 1996, Griffin et al. 1998, 2000, Boisgard et al. 2003). Thus, studies reporting mean results of the original Berger CT protocol with sex differences have little value, because inaccuracy is introduced. The studies that used Berger’s CT protocol to measure rotation without sex differences—combined with the surgical transepicondylar axis as a reference—could be compared. In recent studies, the value of the surgical transepicondylar axis could be confirmed (Victor 2009, Victor et al. 2009b). Recently, Konigsberg et al. (2014) examined the inter-observer and intra-observer reliability (repeatability) of the CT rotational protocol of TKA components by Berger, and found variable results. With the same observer assessing the same scan twice, there was a 12-degree difference in combined rotation. The authors also found poor inter-observer variability for the femoral component (0.39) and good inter-observer variability (0.67) for the tibial component. Roper et al. (2013) could improve the inter- and intra-observer reliability for measuring the tibial component rotation with a 3D modification of Berger’s protocol, but to date 3D reconstructions have not been able to improve registration errors of the epicondylar axis (Wai Hung et al. 2009). The value of the tibial reference points used in Berger’s CT protocol remain unclear (Incavo et al. 2003, Akagi et al. 2005, Siston et al. 2006, Cobb et al. 2008, Graw et al. 2010, Lawrie et al. 2011, Kawahara et al. 2012, Sahin et al. 2012, Howell et al. 2013). Victor et al. (2009a) described a low inter- and intra-observer variability in the CT registration of landmarks that define the coordinate system of the femur and tibia. In the femur, the surgical and anatomical transepicondylar axis and the posterior condylar line could be determined precisely. In the tibia, the least variability was found in the tibial transverse axis. The posterior condylar line of the tibia and the tibial tubercle axis exceeded 3 degrees (maximal error) and could therefore not be recommended as reliable landmarks. The authors also confirmed the tibial transverse axis as previously described by Cobb et al. (2008). A cadaver study also confirmed that the tibial transverse axis was closely related to the projected surgical transepicondylar axis of the femur (Victor et al. 2009b), but to date no postoperative CT rotational protocol for tibial rotation relative to the tibial transverse axis has been described.
Knee Society score
In most of the studies included, the KSS (Insall et al. 1989) was used for assessment of the outcome. The KSS is a responsive and reliable outcome measure that has been validated (Kreibich et al. 1996, Ryd et al. 1997). However, it suffers from high inter- and intra-observer variation when the assessments are performed by less experienced doctors and nurses (Liow et al. 2000). Furthermore, Sasaki et al. (2014) showed that it is difficult to evaluate TKA patients only with objective scales such as the KSS, because they have a low correlation with patients’ reported quality of life. The new KSS was developed in 2011 as a patient-derived outcome measure to better characterize satisfaction, expectations, and physical activities after total knee arthroplasty (Noble et al. 2012, Scuderi et al. 2012). Although the first study to use this questionnaire has been published (Kawahara et al. 2012), showing reduced scores for functional activities and slightly reduced scores for satisfaction after internal rotation of the femoral component, further research on this questionnaire is required.
Correlation analysis
The relationship between tibial and femoral rotation and functional outcome could be examined with correlation analysis. 11 studies gave 9 study groups for the tibial analysis and 16 study groups for the femoral analysis. A correlation can range between −1 (a perfect negative relationship) and +1 (a perfect positive relationship), with 0 indicating no straight-line relationship. A positive correlation would indicate that a higher degree of external rotation coincides with a higher total KSS. Correlation analysis has been used previously to assess sagittal and coronal alignment in TKA (Lotke and Ecker 1977, Fuchs et al. 2002). In the current study, a correlation of 0.44 (95% CI: 0.27–0.59) for tibial rotation and of 0.68 (95% CI: 0.64–0.73) for femoral rotation was found. The confidence interval for the tibial correlation was wider than that for the femur, which indicates lower precision of the tibial correlation estimate in our analysis. According to Cohen’s classification (Cohen 1988), this is a medium correlation for the tibial rotation and a large correlation for the femoral rotation. This finding is in accordance with previous studies (Laskin 1995, Akagi et al. 1999), which concluded that femoral components that were externally rotated relative to the posterior condylar line performed better. A trend of better function was demonstrated by Longstaff et al. (2009) if the femoral component rotation is placed within 2 degrees of the surgical transepicondylar axis. Recently, Kim et al. (2014) showed that less than 2 degrees of external rotation of the femoral and tibial components are risk factors for component failure. However, in this study the tibial component rotation was defined as the angle between the posterior margins of the tibial plateau and the tibial bearing. This technique is unreliable (Victor et al. 2009a). The optimal rotation angle for femur and tibia remains unknown.
Some limitations of this correlation analysis should be taken into account. First of all, it should be realized that the outcome of a TKA is affected by the alignment of all components in every plane. This is true for the alignment of the components in the coronal and sagittal planes, but the rotational alignment of each component also has an effect and makes it difficult to attribute effects to alignment of any individual component in a single plane—and results in omitted variable bias. This is well illustrated by the 2 patient groups with anterior knee pain from Fosco’s study, who represented the biggest outliers in both correlation analyses (Fosco et al. 2010). A second limitation is the fact that studies with unknown follow-up or limited follow-up of 6 months were included. It is unlikely that early follow-up assessments represent an endpoint, and an unknown follow-up might also influence the results. The strength of this analysis lies in the numbers of patients included, which exceeded those in any individual study reporting on the effect of rotation of TKA components on the functional outcome.
Revision studies
All studies reported postoperative improvement of the KSS and HSS. Although some authors use broader intervals (Insall et al. 1979, Ranawat et al. 1993), more commonly narrow intervals are used to assign patients to a category (excellent, good, fair, or poor) based on the KSS numeric score (Wright et al. 1990, Konig et al. 1997). When a classification with narrow intervals is used, the postoperative KSS knee score would be fair in 3 study groups and good in 2 study groups. As for the KSS functional score, it would be poor in 3 study groups and good in 3 study groups. Due to the inter-observer and intra-observer variability, we cannot be confident that a change is real unless it exceeds 23 points for intra-observer assessments and 16 points for inter-observer assessments of the KSS knee score. The same is true for the KSS functional score, where the cutoff point is 30 points for the inter-observer variability and 19 points for the intra-observer variability (Liow et al. 2000). Of the revision studies (Table 2 see Supplementary data), the improvement in 2 studies remained lower than the cutoff point of the inter- and intra-observer variability of the KSS function score (Bedard et al. 2011). We compared the recalculated mean rotations from the data presented in the study by Fosco et al. (2010) with their inclusion criteria for both study groups. The mean combined rotation in the patella resurfacing and total revision group was 1.1 degrees of external rotation and 0.4 degrees of internal rotation. Solid conclusions from this study can therefore not be drawn. In the study by Lakstein et al. (2010), the Berger CT protocol with sex differences was used for calculation of the femoral rotation. Thus, only the results of revision indicated for tibial component malalignment are credible.
A further limitation to the interpretation of the results of revision is that only Bedard et al. (2011) reported the postoperative rotational alignment measured with CT scan. It therefore remains uncertain whether the improved outcome in the other revision studies was due to a correction of rotational malalignment. Finally, it remains unknown whether the improvements were clinically significant. The minimal important change (MIC) is defined as the smallest change in a measurement that signifies an important improvement in a symptom or a sign. We have not found any reports on MIC for the KSS scores and the HSS score.
In conclusion, a medium positive correlation was found between the rotational alignment of the tibial component and KSS, and a large positive correlation was found between the rotational alignment of the femoral component and KSS. External rotation of the TKA components results in better outcome. Furthermore, a revision of a TKA for malrotated components may be a successful procedure. However, there were only 2 studies reporting improvement after TKA revision exceeding the inter- and intra-observer variability of the KSS when we included studies with malrotation measurements according to the Berger CT protocol without sex differences (Lakstein et al. 2010). According to these studies, it appears that TKA revision for an internal malrotation of the tibial component of 4.3 degrees and for an internal malrotation of the femoral component of 7.1 degrees results in significant improvement. Due to several limitations, however, we cannot accept these values as being clear cutoff points indicating a TKA revision. The repeatability of the Berger CT protocol and the value of its tibial reference points is questionable, the MIC of the KSS and HSS used in studies to report outcome of revision for malrotated TKA components remains unknown, and omitted variable bias is inevitable. Furthermore, the combined sample size of these studies was low—with just 38 patients—and the level of evidence of these studies was III—IV. Therefore, taking into account the low quality of evidence, a weak recommendation can be assigned to these tibial and femoral cutoff points. Based on the available literature, no recommendations can be made regarding combined malrotation, mismatch malrotation, and external rotational malalignment of either component due to the low numbers of studies reporting on these topics.
Based on the current systematic review and correlation analysis, we can make some recommendations for further research. First, there is no reliable protocol to assess the rotational alignment of the tibial tray; the optimal intraoperative anatomical landmarks as well as the optimal postoperative radiological reference points are yet to be determined. Furthermore, large prospective cohort studies are needed to allow subgroup analysis in which the effect of separate parameters can be examined while other parameters remain within acceptable limits. These cohort studies should incorporate both functional and subjective outcome measures. After such studies, conclusions can be drawn regarding identification of optimal rotations for both components. Finally, studies reporting on revision for malalignment should report both preoperative and postoperative rotational alignment measured with CT scan.
Supplementary data
Tables 1 and 2, are available at Acta’s website (www.actaorthop.org), identification number 7862.
Acknowledgments
KV: study design, collection and analysis of data, writing of manuscript, and main author. SB: data collection and editing of manuscript. MB: study design and editing of manuscript. WT: data analysis, statistical analysis, and editing of manuscript. RG: study design and editing of manuscript.
No competing interests declared.
References
- Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T. Effect of rotational alignment on patellar tracking in total knee arthroplasty . Clin Orthop Relat Res. 1999;366(9):155–63. doi: 10.1097/00003086-199909000-00019. [DOI] [PubMed] [Google Scholar]
- Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C. Variability of extraarticular tibial rotation references for total knee arthroplasty . Clin Orthop Relat Res. 2005;436(7):>172–6. doi: 10.1097/01.blo.0000160027.52481.32. [DOI] [PubMed] [Google Scholar]
- Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L. Component rotation and anterior knee pain after total knee arthroplasty . Clin Orthop Relat Res. 2001;392(11):46–55. doi: 10.1097/00003086-200111000-00006. [DOI] [PubMed] [Google Scholar]
- Bedard M, Vince KG, Redfern J, Collen SR. Internal rotation of the tibial component is frequent in stiff total knee arthroplasty . Clin Orthop Relat Res. 2011;469(8):>2346–55. doi: 10.1007/s11999-011-1889-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell SW, Young P, Drury C, Smith J, Anthony I, Jones B, Blyth M, McLean A. Component rotational alignment in unexplained painful primary total knee arthroplasty . Knee. 2014;21(1):271–7. doi: 10.1016/j.knee.2012.09.011. [DOI] [PubMed] [Google Scholar]
- Berger RA, Crossett LS. Determining the rotation of the femoral and tibial components in total knee arthroplasty: a computer tomography technique. Op Tech Orthop. 1998;8(3):128–33. [Google Scholar]
- Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis . Clin Orthop Relat Res. 1993a;286(1):40–7. [PubMed] [Google Scholar]
- Berger RA, Seel MJ, Schleiden M, Britton CA, Crossett LS, Rubash HE. Determination of femoral component rotation in total knee arthroplasty using computer tomography. Orthop Trans. 1993b;17(3):1174. [Google Scholar]
- Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty . Clin Orthop Relat Res. 1998;356(11):144–53. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- Bhattee G, Moonot P, Govindaswamy R, Pope A, Fiddian N, Harvey A. Does malrotation of components correlate with patient dissatisfaction following secondary patellar resurfacing? . Knee. 2014;21(1):247–51. doi: 10.1016/j.knee.2012.12.006. [DOI] [PubMed] [Google Scholar]
- Boisgard S, Moreau PE, Descamps S, Courtalhiac C, Silbert H, Moreel P, Michel JL, Levai JP. Computed tomographic study of the posterior condylar angle in arthritic knees: its use in the rotational positioning of the femoral implant of total knee prostheses . Surg Radiol Anat. 2003;25(3-4):330–4. doi: 10.1007/s00276-003-0144-8. [DOI] [PubMed] [Google Scholar]
- Boldt JG, Stiehl JB, Hodler J, Zanetti M, Munzinger U. Femoral component rotation and arthrofibrosis following mobile-bearing total knee arthroplasty . Int Orthop. 2006;30(5):420–5. doi: 10.1007/s00264-006-0085-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth A, Clarke M, Dooley G, Ghersi D, Moher D, Petticrew M, Stewart L. PROSPERO at one year: an evaluation of its utility . Syst Rev. 2013;2:4. doi: 10.1186/2046-4053-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? . Clin Orthop Relat Res. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan SK, Clark GW, Lloyd S, Scott RG, Breidahl W, Sikorski JM. Computer-assisted total knee replacement. A controlled cadaver study using a multi-parameter quantitative CT assessment of alignment (the Perth CT Protocol) . J Bone Joint Surg Br. 2004;86(6):818–23. doi: 10.1302/0301-620x.86b6.15456. [DOI] [PubMed] [Google Scholar]
- Cobb JP, Dixon H, Dandachli W, Iranpour F. The anatomical tibial axis: reliable rotational orientation in knee replacement . J Bone Joint Surg Br. 2008;90(8):1032–8. doi: 10.1302/0301-620X.90B8.19905. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, New Jersey. 1988.
- Dennis DA. Evaluation of painful total knee arthroplasty . J Arthroplasty. 2004;19(4 Suppl 1):35–40. doi: 10.1016/j.arth.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Fosco M, Tigani D, Rimondi E. Revision of knee prostheses with components malrotation: Treatment algorithm using a computed tomographic analysis. Eur Orthop Traumatol. 2010;1(2):61–8. [Google Scholar]
- Fuchs S, Floren MG, Chylarecki C, Bettin D. Is there a correlation between clinical results or quality of life and radiological findings after implantation of a total knee prosthesis? . Biomed Tech (Berl) 2002;47(4):97–101. doi: 10.1515/bmte.2002.47.4.97. [DOI] [PubMed] [Google Scholar]
- Graw BP, Harris AH, Tripuraneni KR, Giori NJ. Rotational references for total knee arthroplasty tibial components change with level of resection . Clin Orthop Relat Res. 2010;468(10):2734–8. doi: 10.1007/s11999-010-1330-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin FM, Insall JN, Scuderi GR. The posterior condylar angle in osteoarthritic knees . J Arthroplasty. 1998;13(7):812–5. doi: 10.1016/s0883-5403(98)90036-5. [DOI] [PubMed] [Google Scholar]
- Griffin FM, Math K, Scuderi GR, Insall JN, Poilvache PL. Anatomy of the epicondyles of the distal femur: MRI analysis of normal knees . J Arthroplasty. 2000;15(3):354–9. doi: 10.1016/s0883-5403(00)90739-3. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberati A, Schunemann HJ. Going from evidence to recommendations . BMJ. 2008;336(7652):1049–51. doi: 10.1136/bmj.39493.646875.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvie P, Sloan K, Beaver RJ. Three-dimensional component alignment and functional outcome in computer-navigated total knee arthroplasty: a prospective, randomized study comparing two navigation systems . J Arthroplasty. 2011;26(8):1285–90. doi: 10.1016/j.arth.2010.12.022. [DOI] [PubMed] [Google Scholar]
- Hofmann S, Romero J, Roth-Schiffl E, Albrecht T. Rotational malalignment of the components may cause chronic pain or early failure in total knee arthroplasty . Orthopade. 2003;32(6):469–76. doi: 10.1007/s00132-003-0503-5. [DOI] [PubMed] [Google Scholar]
- Howell SM, Chen J, Hull ML. Variability of the location of the tibial tubercle affects the rotational alignment of the tibial component in kinematically aligned total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2288–95. doi: 10.1007/s00167-012-1987-5. [DOI] [PubMed] [Google Scholar]
- Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H. “Explanation of the 2011 Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence (Background Document)”. Oxford Centre for Evidence-Based Medicine 2011. http://www.cebm.net/index.aspx?o=5653
- Huang TW, Kuo LT, Peng KT, Lee MS, Hsu RW. Computed tomography evaluation in total knee arthroplasty: computer-assisted navigation versus conventional instrumentation in patients with advanced valgus arthritic knees . J Arthroplasty. 2013;29(12):2363–8. doi: 10.1016/j.arth.2013.12.014. [DOI] [PubMed] [Google Scholar]
- Incavo SJ, Coughlin KM, Pappas C, Beynnon BD. Anatomic rotational relationships of the proximal tibia, distal femur, and patella: implications for rotational alignment in total knee arthroplasty . J Arthroplasty. 2003;18(5):643–8. doi: 10.1016/s0883-5403(03)00197-9. [DOI] [PubMed] [Google Scholar]
- Insall J, Tria AJ, Scott WN. The total condylar knee prosthesis: the first 5 years? Clin Orthop Relat Res. 1979. pp. 14568–77. [PubMed]
- Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system . Clin Orthop Relat Res. 1989;248:13–4. [PubMed] [Google Scholar]
- Kawahara S, Matsuda S, Okazaki K, Tashiro Y, Mitsuyasu H, Nakahara H, Iwamoto Y. Relationship between the tibial anteroposterior axis and the surgical epicondylar axis in varus and valgus knees . Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2077–81. doi: 10.1007/s00167-011-1826-0. [DOI] [PubMed] [Google Scholar]
- Kienapfel H, Springorum H-P, Ziegler A, Klose K-J, Georg C, Griss P. Effect of rotation of the femoral and tibial components on patellofemoral malalignment in knee arthroplasty . Orthopade. 2003;32(4):312–8. doi: 10.1007/s00132-002-0441-7. [DOI] [PubMed] [Google Scholar]
- Kim D, Seong SC, Lee MC, Lee S. Comparison of the tibiofemoral rotational alignment after mobile and fixed bearing total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc. 2012;20(2):337–45. doi: 10.1007/s00167-011-1750-3. [DOI] [PubMed] [Google Scholar]
- Kim YH, Park JW, Kim JS, Park SD. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis . Int Orthop. 2014;38(2):379–85. doi: 10.1007/s00264-013-2097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konig A, Scheidler M, Rader C, Eulert J. The need for a dual rating system in total knee arthroplasty . Clin Orthop Relat Res. 1997;345(12):161–7. [PubMed] [Google Scholar]
- Konigsberg B, Hess R, Hartman C, Smith L, Garvin KL. Inter- and intraobserver reliability of two-dimensional CT scan for total knee arthroplasty component malrotation . Clin Orthop Relat Res. 2014;472(1):212–7. doi: 10.1007/s11999-013-3111-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreibich DN, Vaz M, Bourne RB, Rorabeck CH, Kim P, Hardie R, Kramer J, Kirkley A. What is the best way of assessing outcome after total knee replacement? . Clin Orthop Relat Res. 1996;331(10):221–5. doi: 10.1097/00003086-199610000-00031. [DOI] [PubMed] [Google Scholar]
- Labek G, Thaler M, Janda W, Agreiter M, Stockl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets . J Bone Joint Surg Br. 2011;93(3):293–7. doi: 10.1302/0301-620X.93B3.25467. [DOI] [PubMed] [Google Scholar]
- Lad DG, Thilak J, Thadi M. Component alignment and functional outcome following computer assisted and jig based total knee arthroplasty . Indian J Orthop. 2013;47(1):77–82. doi: 10.4103/0019-5413.106915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakstein D, Zarrabian M, Kosashvili Y, Safir O, Gross AE, Backstein D. Revision total knee arthroplasty for component malrotation is highly beneficial. A case control study . J Arthroplasty. 2010;25(7):1047–52. doi: 10.1016/j.arth.2009.07.004. [DOI] [PubMed] [Google Scholar]
- Laskin RS. Flexion space configuration in total knee arthroplasty . J Arthroplasty. 1995;10(5):657–60. doi: 10.1016/s0883-5403(05)80211-6. [DOI] [PubMed] [Google Scholar]
- Lawrie CM, Noble PC, Ismaily SK, Stal D, Incavo SJ. The flexion-extension axis of the knee and its relationship to the rotational orientation of the tibial plateau . J Arthroplasty. 2011;26(Suppl 6):53–8. doi: 10.1016/j.arth.2011.04.026. [DOI] [PubMed] [Google Scholar]
- Liow RY, Walker K, Wajid MA, Bedi G, Lennox CM. The reliability of the American Knee Society Score . Acta Orthop Scand. 2000;71(6):603–8. doi: 10.1080/000164700317362244. [DOI] [PubMed] [Google Scholar]
- Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function . J Arthroplasty. 2009;24(4):570–8. doi: 10.1016/j.arth.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement . J Bone Joint Surg Am. 1977;59(1):77–9>. [PubMed] [Google Scholar]
- Lützner J, Kirschner S, Günther KP, Harman MK. Patients with no functional improvement after total knee arthroplasty show different kinematics . Int Orthop. 2012;36(9):1841–7. doi: 10.1007/s00264-012-1584-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantas JP, Bloebaum RD, Skedros JG, Hofmann AA. Implications of reference axes used for rotational alignment of the femoral component in primary and revision knee arthroplasty . J Arthroplasty. 1992;7(4):531–5. doi: 10.1016/s0883-5403(06)80075-6. [DOI] [PubMed] [Google Scholar]
- Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y. Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees . Am J Knee Surg. 2001;14(3):152–6. [PubMed] [Google Scholar]
- Matsuda S, Mizu-uchi H, Fukagawa S, Miura H, Okazaki K, Matsuda H, Iwamoto Y. Mobile-bearing prosthesis did not improve mid-term clinical results of total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc. 2010;18(10):1311–6. doi: 10.1007/s00167-010-1143-z. [DOI] [PubMed] [Google Scholar]
- Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE. Optimizing femoral component rotation in total knee arthroplasty . Clin Orthop Relat Res. 2001;392(11):38–45. doi: 10.1097/00003086-200111000-00005. [DOI] [PubMed] [Google Scholar]
- Mizu-uchi H, Matsuda S, Miura H, Okazaki K, Akasaki Y, Iwamoto Y. The evaluation of post-operative alignment in total knee replacement using a CT-based navigation system . J Bone Joint Surg Br. 2008;90(8):1025–31. doi: 10.1302/0301-620X.90B8.20265. [DOI] [PubMed] [Google Scholar]
- Mochizuki RM, Schurman DJ. Patellar complications following total knee arthroplasty. J Bone Joint Surg Am. 1979;61(6A):879–83. [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement . J Clin Epidemiol. 2009;62(10):1006–12. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Nicoll D, Rowley DI. Internal rotational error of the tibial component is a major cause of pain after total knee replacement . J Bone Joint Surg Br. 2010;92(9):1238–44. doi: 10.1302/0301-620X.92B9.23516. [DOI] [PubMed] [Google Scholar]
- Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, Lonner JH, Chadha P, Daylamani DA, Scott WN, Bourne RB. Development of a new Knee Society scoring system . Clin Orthop Relat Res. 2012;470(1):20–32. doi: 10.1007/s11999-011-2152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietsch M, Hofmann S. Early revision for isolated internal malrotation of the femoral component in total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1057–63. doi: 10.1007/s00167-011-1637-3. [DOI] [PubMed] [Google Scholar]
- Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE. Rotational landmarks and sizing of the distal femur in total knee arthroplasty . Clin Orthop Relat Res. 1996;331(10):35–46. doi: 10.1097/00003086-199610000-00006. [DOI] [PubMed] [Google Scholar]
- Ranawat CS, Flynn WF, Saddler S, Hansraj KK, Maynard MJ. Long-term results of the total condylar knee arthroplasty. A 15-year survivorship study . Clin Orthop Relat Res. 1993;286(1):94–102. [PubMed] [Google Scholar]
- Rhoads DD, Noble PC, Reuben JD, Mahoney OM, Tullos HS. The effect of femoral component position on patellar tracking after total knee arthroplasty . Clin Orthop Relat Res. 1990;260(11):43–51. [PubMed] [Google Scholar]
- Romero J, Stahelin T, Binkert C, Pfirrmann C, Hodler J, Kessler O. The clinical consequences of flexion gap asymmetry in total knee arthroplasty . J Arthroplasty. 2007;22(2):235–40. doi: 10.1016/j.arth.2006.04.024. [DOI] [PubMed] [Google Scholar]
- Roper GE, Bloemke AD, Roberts CC, Spangehl MJ, Clarke HD. Analysis of tibial component rotation following total knee arthroplasty using 3D high definition computed tomography . J Arthroplasty. 2013;28(Supp l8):106–11. doi: 10.1016/j.arth.2013.04.053. [DOI] [PubMed] [Google Scholar]
- Ryd L, Karrholm J, Ahlvin P. Knee scoring systems in gonarthrosis. Evaluation of interobserver variability and the envelope of bias. Score Assessment Group . Acta Orthop Scand. 1997;68(1):41–5. doi: 10.3109/17453679709003973. [DOI] [PubMed] [Google Scholar]
- Sahin N, Atici T, Ozturk A, Ozkaya G, Ozkan Y, Avcu B. Accuracy of anatomical references used for rotational alignment of tibial component in total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc. 2012;20(3):565–70. doi: 10.1007/s00167-011-1606-x. [DOI] [PubMed] [Google Scholar]
- Sasaki E, Tsuda E, Yamamoto Y, Meada S, Otsuka H, Ishibashi Y. Relationship between patient-based outcome score and conventional objective outcome scales in post-operative total knee arthroplasty patients . Int Orthop. 2014;38(2):373–8. doi: 10.1007/s00264-013-2064-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN. The new Knee Society Knee Scoring System . Clin Orthop Relat Res. 2012;470(1):3–19. doi: 10.1007/s11999-011-2135-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sensi L, Buzzi R, Giron F, De LL, Aglietti P. Patellofemoral function after total knee arthroplasty. Gender-related differences . J Arthroplasty. 2011;26(8):1475–80. doi: 10.1016/j.arth.2011.01.016. [DOI] [PubMed] [Google Scholar]
- Sikorski JM. Alignment in total knee replacement . J Bone Joint Surg Br. 2008;90(9):1121–7. doi: 10.1302/0301-620X.90B9.20793. [DOI] [PubMed] [Google Scholar]
- Siston RA, Goodman SB, Patel JJ, Delp SL, Giori NJ. The high variability of tibial rotational alignment in total knee arthroplasty . Clin Orthop Relat Res. 2006;452(11):65–9. doi: 10.1097/01.blo.0000229335.36900.a0. [DOI] [PubMed] [Google Scholar]
- Sternheim A, Lochab J, Drexler M, Kuzyk P, Safir O, Gross A, Backstein D. The benefit of revision knee arthroplasty for component malrotation after primary total knee replacement . Int Orthop. 2012;36(12):2473–8. doi: 10.1007/s00264-012-1675-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornhill TS. Painful total knee arthroplasty . Orthopedics. 2002;25(9):965–7. doi: 10.3928/0147-7447-20020901-33. [DOI] [PubMed] [Google Scholar]
- Toms AD, Mandalia V, Haigh R, Hopwood B. The management of patients with painful total knee replacement . J Bone Joint Surg Br. 2009;91(2):143–50. doi: 10.1302/0301-620X.91B2.20995. [DOI] [PubMed] [Google Scholar]
- Victor J. Rotational alignment of the distal femur: A literature review . Orthop Traumatol Surg Res. 2009;95(5):365–72. doi: 10.1016/j.otsr.2009.04.011. [DOI] [PubMed] [Google Scholar]
- Victor J, Van DD, Labey L, Innocenti B, Parizel PM, Bellemans J. How precise can bony landmarks be determined on a CT scan of the knee? Knee. 2009a;16(5):358–65. doi: 10.1016/j.knee.2009.01.001. [DOI] [PubMed] [Google Scholar]
- Victor J, Van DD, Labey L, Van GF, Parizel P, Bellemans J. A common reference frame for describing rotation of the distal femur: A CT-based kinematic study using cadavers . J Bone Joint Surg Br. 2009b;91(5):683–90. doi: 10.1302/0301-620X.91B5.21827. [DOI] [PubMed] [Google Scholar]
- Wai Hung CL, Wai PY, Kwong YC, Hon BL, Lei Sha LW, Ho Man SW. Interobserver and intraobserver error in distal femur transepicondylar axis measurement with computed tomography . J Arthroplasty. 2009;24(1):96–100. doi: 10.1016/j.arth.2007.11.014. [DOI] [PubMed] [Google Scholar]
- Woolson ST, Harris AH, Wagner DW, Giori NJ. Component alignmentduring total knee arthroplasty with use of standard or custom instrumentation: a randomized clinical trial using omputed tomography for postoperative alignment measurement . J Bone Joint Surg Am. 2014;96(5):366–72. doi: 10.2106/JBJS.L.01722. [DOI] [PubMed] [Google Scholar]
- Wright RJ, Lima J, Scott RD, Thornhill TS. Two- to four-year results of posterior cruciate-sparing condylar total knee arthroplasty with an uncemented femoral component . Clin Orthop Relat Res. 1990;260(11):80–6. [PubMed] [Google Scholar]
- Yoshioka Y, Siu D, Cooke TD. The anatomy and functional axes of the femur . J Bone Joint Surg Am. 1987;69(6):873–80. [PubMed] [Google Scholar]
- Zhang XL, Zhang W, Shao JJ. Rotational alignment in total knee arthroplasty: nonimage-based navigation system versus conventional technique . Chin Med J (Engl ) 2012;125(2):236–43. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.