Abstract
Background and purpose
A complete and correct national arthroplasty register is indispensable for the quality of arthroplasty outcome studies. We evaluated the coverage, completeness, and validity of the Dutch Arthroplasty Register (LROI) for hip and knee arthroplasty.
Patients and methods
The LROI is a nationwide population-based registry with information on joint arthroplasties in the Netherlands. Completeness of entered procedures was validated in 2 ways: (1) by comparison with the number of reimbursements for arthroplasty surgeries (Vektis database), and (2) by comparison with data from hospital information systems (HISs). The validity was examined by conducting checks on missing or incorrectly coded values in the LROI.
Results
The LROI contains over 300,000 hip and knee arthroplasties performed since 2007. Coverage of all Dutch hospitals (n = 100) was reached in 2012. Completeness of registered procedures was 98% for hip arthroplasty and 96% for knee arthroplasty in 2012, based on Vektis data. Based on comparison with data from the HIS, completeness of registered procedures was 97% for primary total hip arthroplasty and 96% for primary knee arthroplasty in 2013. Completeness of revision arthroplasty was 88% for hips and 90% for knees in 2013. The proportion of missing or incorrectly coded values of variables was generally less than 0.5%, except for encrypted personal identity numbers (17% of which were missing) and ASA scores (10% of which were missing).
Interpretation
The LROI now contains over 300,000 hip and knee arthroplasty procedures, with coverage of all hospitals. It has a good level of completeness (i.e. more than 95% for primary hip and knee arthroplasty procedures in 2012 and 2013) and the database has high validity.
In 2007, the Dutch Arthroplasty Register (LROI) was started by the Netherlands Orthopaedic Association (NOV) to register patient, surgical procedure, and implant characteristics for hip and knee arthroplasty in the Netherlands (LROI-Report 2012 Insight into Quality of Orthopaedic Care in the Netherlands 2013). The LROI contributes to the quality of orthopedic care by continuous monitoring of prostheses and feedback to orthopedic surgeons via an online web-based interface. This shows orthopedic surgeons the aggregated data on patient and prosthesis characteristics for all registered arthroplasty procedures in their hospital relative to the averaged data from all other hospitals in the Netherlands. It thereby provides a benchmark for each orthopedic department. Furthermore, national reports with mainly descriptive statistics are published annually (www.lroi.nl).
The need for completeness of a national arthroplasty registry is undisputed, for assessment of the quality of orthopedic arthroplasty care (Herberts and Malchau 2000). It is important to evaluate the quality of the data and to validate them on a regular basis (Goldberg et al. 1980). To obtain high-quality data, it is important to identify any systematic errors of data reporting or data entry, or missing data, and to correct them.
In order to ensure reliable results from research using data from the LROI, there must be complete and correct registration of both primary and revision arthroplasty in all hospitals in the Netherlands. This prevents inclusion bias, the importance of which is stressed even more for survival analysis, where time between primary and revision arthroplasty is calculated. Furthermore, a complete and valid registration of all prostheses used in the Netherlands is necessary for traceability purposes, in case there is a recall of an implant.
Evaluation of the completeness of an arthroplasty register can be done in several ways, depending on the possibilities and legalities in a particular country (e.g. privacy laws). Comparison of national registry data with data from national patient administrative systems or comparison with local data that are available in patient records are the most common methods. In the Netherlands, it is not permitted by law to compare data at the patient level automatically. Thus, alternative methods must be used, such as comparison with the aggregated data from each hospital information system and/or comparison with aggregated surgical reimbursement data from the health insurance companies organization.
We determined the degree of national coverage and completeness of the LROI for hip and knee arthroplasty by comparing the LROI data with 2 independent external data sources: (1) reimbursement data from health insurance companies, and (2) data on date of operation from hospital information systems. Furthermore, we evaluated the validity of the LROI data and also problems with data collection and data entry in the 100 Dutch hospitals.
Methods
Data collection and storage by the Dutch Arthroplasty Register
The Dutch Arthroplasty Register (LROI) is a nationwide population-based registry with information on joint arthroplasties in the Netherlands. Registration is performed with a paper-based form to collect patient and surgery characteristics, which are subsequently entered into a central database (a Microsoft SQL server) at the hospital using the ProMISe system (www.msbi.nl/Promise). ProMISe (‘Project Manager Internet Server’) is a generic internet-based application for the design, maintenance, and use of (clinical) data management projects. It has been developed and is maintained by the Department of Medical Statistics of the Leiden University Medical Center, at the Section of Advanced Data Management (ADM). ADM is NEN7510 certified and ProMISe meets the requirements on data safety and privacy imposed by Dutch national law and professional guidelines.
The LROI contains information on patient characteristics such as age, sex, and general health (ASA score). In mid-2013, body mass index, smoking behavior, orthopedic vitality (i.e. Charnley score), and postal code were also added to the database. The privacy of all patients is assured by using a trusted third party (ZorgTTP) to encrypt the personal identity number (a number given by the Dutch government to each inhabitant of the Netherlands). Hospital of surgery, anonymized (encrypted) surgeon, type of surgery, date of surgery, surgical approach, fixation, and characteristics of the prosthesis (as specified below) are also registered.
The acetabular cup, femoral stem, femoral head, and inlay component of a hip prostheses can be registered, whereas the tibial, femoral, inlay, and patellar component can be registered for knee prostheses. Furthermore, cement can be registered in cases of cemented fixation. Stickers that were placed on the prosthesis components by the manufacturer can be attached to the registration form. The sticker of each prosthesis component contains a product number (REF number) and batch number (LOT number). The product number is used to identify the characteristics of the prosthesis and the batch number is used to identify the specific production details of prostheses. Prosthesis characteristics are derived from an implant library within the LROI, which contains several core characteristics of all prostheses used in the Netherlands since 2007. The characteristics include the name of the prosthesis, the manufacturer, the component, the type, the material, the coating of the prosthesis, the method of sterilization of the polyethylene, and the diameter of the femoral head (for hip prostheses). The characteristics were supplied by all the implant manufacturers or distributors in the Netherlands.
The Vektis database on healthcare
Vektis, the national insurance database on healthcare, is an information system for healthcare data in the Netherlands. It contains reimbursement data on all medical treatments paid for by Dutch insurance companies (www.vektis.nl). Almost all (99%) of Dutch inhabitants have private healthcare insurance (see http://statline.cbs.nl), and hip and knee arthroplasty are procedures that are paid for by these health insurance companies. Thus, Vektis contains national data concerning all the hip and knee arthroplasty surgeries performed at each hospital. However, “date of surgery” is defined as the date of the start of financial reimbursement, which coincides with the indication for primary or revision arthroplasty at the outpatient clinic, and not with the actual date of surgery.
Hospital information system
Every hospital in the Netherlands has its own electronic hospital information system (HIS), which contains patient medical records. Each HIS contains administrative patient information (including name and date of birth) and administration of hospital visits (including diagnostic procedures, date and type of surgery, and surgeon performing arthroplasty). It also contains the administration of the facturation, which includes date, number, and type of arthroplasty surgeries.
Completeness and coverage
There is no gold standard available in the Netherlands to determine the completeness of the LROI database. We therefore used 2 alternative methods. The data from the LROI were validated against reimbursement data from the national insurance database on healthcare (Vektis). We also compared the data from the LROI with surgical date data from the HIS of each hospital. Completeness of registration in the LROI was calculated by comparing the number of registrations in the LROI with the number of arthroplasty surgeries based on national health insurance data (Vektis), and with data from the HIS of each hospital in the Netherlands (for definitions, see box, for surgical codes see Table 2). Completeness based on Vektis data was calculated for the period 2009–2012, while completeness based on HIS data was calculated for 2012 and 2013.
Definitions
| Completeness based on Vektis data = Number of registered procedures in the LROI / Number of reimbursed procedures based on data from Vektis |
| Completeness based on HIS data = Number of registered procedures in the LROI / Number of performed procedures in the HIS of all hospitals in the Netherlands |
| Coverage = Number of participating hospitals / Number of hospitals performing hip and or knee arthroplasty surgeries based on data from Vektis |
A primary hip arthroplasty was defined as the first time a total, hemi-, or resurfacing prosthesis is placed, to replace a hip joint or part of a hip joint. A primary knee arthroplasty was defined as the first time a unicondylar, patellofemoral, or total prosthesis is placed, to replace a knee joint or part of a knee joint. Revision arthroplasty was defined as any change (replacement, removal, or addition) of 1 or several components of the joint prosthesis. As an aid to selecting the correct surgical procedures from the HIS, specific codes from the diagnosis treatment coding system used in Dutch healthcare were offered at hospitals.
Data from the LROI were retrieved in May 2014 and compared with data from Vektis for hip and knee arthroplasties performed at each hospital. In the analyses, counts were based on the total number of primary and revision arthroplasties (separately for hip and knee joints). Then, for the comparison with data from the HIS in each hospital in the Netherlands, primary and revision arthroplasties were analyzed separately for hip and knee joints. For primary hip arthroplasty, only total hip arthroplasties (THAs) were considered. In cases where the number of registrations per hospital in the LROI exceeded the amount of arthroplasty registrations in the Vektis or HIS data, the number in Vektis/HIS was considered the maximum number. Overall annual results and also hospital-specific results were calculated. Coverage of the LROI (participation of hospitals; see box for definition) was calculated by comparing the number of participating hospitals with the number of hospitals that performed arthroplasty procedures based on Vektis data for each year.
Validity
The accuracy and degree of completeness of the registered data is the validity of the data registered. The validity of the LROI database was examined by conducting checks on important variables concerning incorrect or missing values. Required variables included date, type of surgery, and side of surgery. Variables in the LROI database that were checked for validity were sex, date of birth, hospital patient number, encrypted personal identity number, diagnosis, ASA score, type of prosthesis, fixation, cemented component (in cases of hybrid fixation), product number of component and cement, type of revision, revised component, and conversion to THA or conversion to total knee arthroplasty (TKA). Missing and incorrect values and combinations thereof were defined and examined. Values were labeled as incorrect when a value other than the answering possibilities was registered. Furthermore, date of birth was labeled as incorrect when age at date of surgery was less than 10 years or more than 110 years. Date of surgery was labeled as incorrect when the date registered was before January 1, 2000 or after the day of conducting the validation check.
In a random sample in 8 hospitals (mainly those suboptimally performing on completeness), the validity of the LROI was evaluated by checking the values of the important variables (the same variables as mentioned above) in the database with the paper forms available in the hospital. In total, 355 records concerning primary hip arthroplasty (n = 105), primary knee arthroplasty (n = 120), revision hip arthroplasty (n = 70), and revision knee arthroplasty (n = 60) were reviewed. Furthermore, a manual record-by-record comparison was performed in 11 hospitals, to examine the surgical procedures not registered in the LROI and those not registered in the HIS. Based on on-site visits and semi-structured interviews with orthopedic surgeons and registration clerks, problems concerning the registration in the LROI were identified.
Results
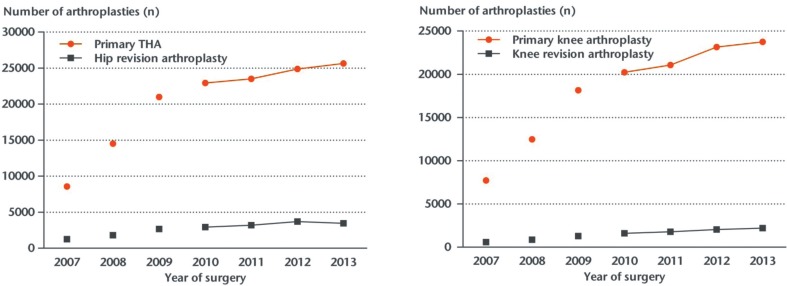
Data on 311,890 joint replacements were reported to the LROI during the period 2007–2013, covering 141,075 primary THAs (45%); 14,740 hemiarthroplasties (5%); 19,049 revision hip arthroplasties (6%); 113,092 primary TKAs (37%); 10,002 unicondylar knee arthroplasties (3%); 3,484 patellofemoral, other, and unknown primary knee arthroplasties (1%); and 10,448 revision knee arthroplasties (3%) (Table 1). The number of annually reported hip and knee arthroplasties increased to 58,003 in 2013 (Figure 1).
Table 1.
Number of data entry records (i.e. hip and knee registrations) in the LROI
| Year | Hip arthroplasty |
Knee arthroplasty |
|||||
|---|---|---|---|---|---|---|---|
| Primary THA | Hemiarthro-plasties | Revision hip | Primary TKA | Primary unicondylar | Primary othera | Revision knee | |
| 2007 b | 8,579 | 921 | 1,267 | 6,688 | 678 | 358 | 594 |
| 2008 b | 14,516 | 1,379 | 1,813 | 10,942 | 1,115 | 420 | 878 |
| 2009 b | 21,007 | 2,056 | 2,675 | 16,020 | 1,524 | 611 | 1,296 |
| 2010 | 22,932 | 2,328 | 2,940 | 17,872 | 1,697 | 669 | 1,617 |
| 2011 | 23,510 | 2,376 | 3,192 | 18,907 | 1,598 | 568 | 1,790 |
| 2012 | 24,889 | 2,748 | 3,708 | 21,009 | 1,586 | 556 | 2,058 |
| 2013 | 25,642 | 2,932 | 3,454 | 21,654 | 1,804 | 302 | 2,215 |
| Total | 141,075 | 14,740 | 19,049 | 113,092 | 10,002 | 3,484 | 10,448 |
THA: Total hip arthroplasty; TKA: Total knee arthroplasty
Primary other included patellofemoral, other, and unknown primary knee arthroplasties
2007–2009: run-in phase of the LROI
Figure 1.
Number of primary total hip arthroplasties (THA) and revision hip arthroplasties (left panel) and number of primary knee arthroplasties and revision knee arthroplasties (right panel) in 2007–2013 registered in the LROI. The period 2007–2009 was the run-in phase of the LROI and therefore the registration is known to be incomplete for those years.
Coverage
After the starting phase of the LROI in the period 2007–2009, the proportion of participating hospitals has been more than 98%; 100% coverage was reached in 2012. Thus, 96 Dutch hospitals performing hip arthroplasties and 100 Dutch hospitals performing knee arthroplasties report to the LROI (Table 3, see Supplementary data).
Completeness
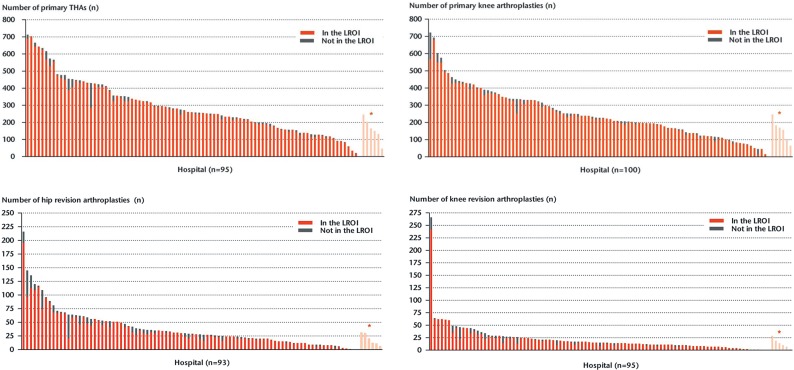
A comparison of the LROI database for 2009–2012 with the Vektis data showed that for hip and knee arthroplasty (primary and revision), the completeness was 88% for hip arthroplasty and 89% for knee arthroplasty in 2009. This increased to 98% for hip arthroplasty and 96% for knee arthroplasty in 2012 (Table 4, see Supplementary data). Furthermore, a comparison with data from the HIS showed that completeness was 97% for primary THA and 96% for primary knee arthroplasty in 2013. For revision arthroplasty, the completeness in 2013 was 88% for procedures to the hip and 90% for procedures to the knee (Table 5, see Supplementary data). Completeness differed widely between hospitals, ranging from 67% to 100% for primary THA and primary knee arthroplasty, except for one small private hospital that started in 2013 (with a completeness of 30% for primary knee arthroplasty). For revision hip and knee arthroplasty, completeness ranged from 35% to 100%. The number of hospitals with more than 10% missing records was 6 (7%) for THA and 7 (8%) for primary knee arthroplasty. For revision hip arthroplasty, 10 hospitals (11%) had more than 25% missing records; for revision knee arthroplasty, 14 hospitals (15%) had more than 25% missing records (Figure 2).
Figure 2.
Number of procedures performed and registered in the LROI per hospital for primary total hip arthroplasty (THA), hip revision arthroplasty, primary knee arthroplasty, and knee revision arthroplasty. * No data available from the hospital information system for comparison. Only hospitals which performed primary, revision, hip or knee arthroplasty are shown.
Reasons for missing records in the LROI were operations on patients admitted through the emergency department, new registration employees in a hospital, and logistic difficulties in entering data in the web-based database due, for example, to loss of registration forms. Furthermore, the record-by-record comparison in 11 hospitals showed that the number of surgical procedures registered in the LROI database, but not registered in the HIS, was 4% for primary hip arthroplasty, 2% for primary knee arthroplasty, 12% for revision hip arthroplasty, and 23% for revision knee arthroplasty.
Validity
In the period 2007–2013, the proportion of missing and incorrectly coded values of patient-related and surgery-related variables in the LROI database was generally small (< 0.5%) for most of these variables. However, 17% of encrypted personal identity numbers were missing, with some hospitals lacking almost all the encrypted personal identity numbers, while many hospitals only had a small proportion missing. The proportion of missing values for encrypted personal identity numbers decreased from 33% in 2007 to 9% in 2013. ASA score was missing in 10% of records, while diagnosis for primary arthroplasty, fixation, and type of prosthesis were missing in 3–5% of records.
The proportion of product numbers missing for hip prosthesis components was small (ranging from 0.7% for acetabular cup components to 2.1% for femoral head components). However, the proportion of product numbers missing for cement used in hip arthroplasty was 6.6%. For knee arthroplasty, the proportion of missing product numbers was less than 1.0% for all components, although 14% of the product numbers of bone cement for knee arthroplasty were missing. Completeness of data for the variables diagnosis for primary arthroplasty, ASA score, fixation, and product number of cement for both hip and knee arthroplasty increased during the period 2007–2013 (Table 5, see Supplementary data).
The random sample analysis showed small discrepancies (around 2.5%) between the paper registration form and the LROI database for most variables. A discrepancy of almost 10% was found for the variable diagnosis for primary THA. Furthermore, 5–8% of checked values were wrongly entered for the variable type of prosthesis, ASA score, hospital patient number, and the variables concerning product numbers (Table 6, see Supplementary data).
Discussion
The overall completeness of the national LROI database was over 95%. A comparable high degree of completeness of the registration of procedures performed has been found in the Scandinavian arthroplasty registries. The Swedish Hip Arthroplasty Register reported a completeness of 96% in 2012 for primary THA (Swedish Hip Arthroplasty Register Annual Report 2012). The Swedish Knee Arthroplasty Register reported a persistent degree of completeness of 97% for primary knee arthroplasties up to 2011 and good validity of the data entered (Swedish Knee Arthroplasty Register Annual Report 2013). The Norwegian Arthroplasty Register had a completeness of 98% for primary and revision hip arthroplasties and of 99% for primary and revision knee arthroplasties, based on a comparison with the Norwegian Patient Register from hospital administrations during the years 1999–2002 (Espehaug et al. 2006). Validity of the Norwegian Arthroplasty Register was good, based on a comparison with data from one local hospital (Arthursson et al. 2005). Furthermore, diagnoses were confirmed in 90% of THA procedures in young adults registered in the Norwegian Arthroplasty Register (Engesaeter et al. 2011, Lehmann et al. 2012). The Danish Knee Arthroplasty Register had a completeness of 97% for primary TKA in 2012 (Dansk Hoftealloplastik Register Årsrapport 2013). The Danish Hip Arthroplasty Register (DHAR) had a completeness of 94% based on a comparison with the Danish National Registry of Patients for 1995–2000, based on linkage of databases using the patient civil registration (personal identity) numbers (Pedersen et al. 2004). Validity of a random sample of data from the DHAR, assessed using medical records and preoperative radiographs, showed that the diagnosis had been correctly registered in 30–100% of diagnoses (Pedersen et al. 2004). In the UK-Wales, the compliance based on levies from implant sales increased from 43% in 2003–2004 to 91% in 2012–2013 (National Joint Registry for England, Wales and Northern Ireland, 10th Annual Report 2013). Since these external validity checks on completeness of registration of procedures performed are done differently by the Dutch Arthroplasty Register (LROI), the Scandinavian registries, and the UK registry, comparisons of completeness between these registries are not possible.
In Sweden and Denmark, personal identity numbers can be used to match patients in different databases (Pedersen et al, 2004, Swedish Hip Arthroplasty Register Annual Report 2012, Swedish Knee Arthroplasty Register Annual Report 2013), which is not possible in other countries including the Netherlands. A record-by-record comparison would not be feasible. Thus, comparisons with the aggregated data from each hospital information system or comparisons with aggregated reimbursement data from health insurance companies are the best alternatives we have at the moment in the Netherlands. The use of 2 independent data sources for comparison makes our validity check stronger than a validation using only one source.
Next to differences in external checks on the validity of data entered, data entry itself also differs between these countries. In the Netherlands, data entry in the LROI by orthopedic surgeons is voluntary. This requires that the full support of the national orthopedic association is necessary, since surgeons bear the major burden of registration (Kolling et al. 2007). The LROI was initiated by the Netherlands Orthopaedic Association (NOV), and almost all Dutch orthopedic surgeons are members. Apart from this, the LROI is directed by an independent, professional board of active orthopedic surgeons. This ensures the support of surgeons and it therefore has a high degree of completeness, which is similar to that of many other registries including the Swedish Hip Arthroplasty Register (Herberts and Malchau 2000). Contribution of data to an arthroplasty register by hospitals is voluntary in most countries, including the Netherlands. However, in some countries such as Finland, Denmark, and also England, Wales and Northern Ireland, it is mandatory to take part in the registry by law (Kolling et al. 2007).
We used 2 external data validation techniques to check the completeness of entered procedures. First, health insurance data (Vektis) based on financial hospital reimbursement data to health insurance companies were used. Although this appears to be an excellent external data source for validation, 100% match is not possible since the surgical procedure date is entered in the LROI database, while the date of the start of financial reimbursement of the hospital is entered in the Vektis database (which is the date of indication for a primary or revision arthroplasty). The second external validation source for the LROI was the collected surgical procedure data from 2012 and 2013, from the hospital information systems (HISs) of every hospital in the Netherlands. The HIS contains the exact date of surgery, which makes an exact match with LROI data possible. Although comparison with the HIS data source appears to be a better validation technique than comparison with Vektis data (due to coding of the date of surgery), HIS data may have an actual mismatch with the LROI data, since each hospital has made a selection of surgical procedures based on codes offered (i.e. for financing purposes) for hip and knee arthroplasty. For the purpose of external validation, the LROI board clearly defined the definitions for primary and revision hip and knee arthroplasty and requested all possible treatment codes for surgical arthroplasty procedures on the hip and knee. Nevertheless, some procedures may have been missed or added incorrectly, which is especially true for revision procedures, with a complicated group of nationally used surgical codes in the HIS and hospitals being able to use several different codes to cover such revision procedures. In addition, a revision hip or knee procedure is defined in the LROI as any replacement, removal, or addition of 1 or several components of a prosthesis. In the HIS, however, 1 revision procedure often involves removal and addition of a component—performed at 2 different operations. The complicated HIS coding system would explain the lower external validation level of completeness for entries on revision arthroplasties in the LROI than for entries on primary hip and knee arthroplasty.
One disadvantage of a comparison at the group level may be an overestimation of the completeness, since it is not certain that specific patients have been registered in both data sources. Thus, the completeness calculated in this study is probably somewhat overestimated compared to that in a study using patients who can be personally identified (Pedersen et al. 2004). However, the accuracy of administrative coding is high for hip and knee arthroplasty (Singh and Ayub 2010, Daneshvar et al. 2012). Furthermore, for primary hip and knee arthroplasty the number of arthroplasties registered in the LROI database but not registered in the HIS was small.
Most (national) arthroplasty registries have mainly focused on completeness of data entry as a measure of the quality of their database, since checking the accuracy of variables in large databases is extremely time consuming. However, the accuracy and degree of completeness of the data registered is important, since inaccurate or missing data tend to bias associations towards the null hypothesis (Sorensen et al. 1996) In the LROI, the proportion of missing and/or incorrectly coded values of variables was generally small (< 0.5%). As of 2013, we have clearly stated the definitions of variables (e.g. diagnosis, ASA score) of primary and revision arthroplasty on the registration forms of the LROI as well as on the web-based entry forms. This was done because surgeons and registration staff may have several different interpretations of a variable. Some surgeons interpreted revision as “exchange of component(s)” and therefore did not register the removal or addition of a component. Furthermore, revision procedures were sometimes wrongly registered as primary procedures. Thus, validity of the LROI and for that matter any registry, can be improved by succinct communication with all hospitals concerning the definitions of primary and revision hip and knee arthroplasty. Obvious and clear definitions will reduce the amount of missed records and records registered in the wrong category. For this reason, every data entry form has a library of definitions. The orthopedic department of each hospital, including the orthopedic surgeons and their registration team, is responsible for complete and correct data entry into the LROI database. Consistent and timely registration by well-qualified and stable secretarial staff largely improved the quality of registration. ASA score was missing in 10% of the records (in either hip or knee arthroplasty). This was possibly due to the anesthesiologist defining the ASA score of the patient and the orthopedic staff forgetting to check this with the anesthesiologist while filling in the LROI form during the postoperative administration. Checking of the data in the LROI database, especially the diagnosis and reason for revision, by review of medical records could further investigate and improve the validity of the LROI database.
Survival of the prosthesis can be calculated by linking primary and revision procedures of a patient (joint- and side-specific). For correct linkage, the encrypted personal identity number is necessary for detection of any revision surgery performed in the Netherlands following primary arthroplasty. Missed primary-revision matches will result in an overestimation of the survival of prostheses. It is therefore essential that the encrypted personal identity number is completely and correctly registered in the LROI. The increase in the proportion of registered encrypted personal identity numbers from 70% in 2007–2009 to 90% in 2012–2013 is therefore encouraging, but it should still be improved further. A proportion of encrypted personal identity numbers will probably always remain missing in the LROI, since most hospitals have some patients with an unknown personal identity number. Besides, completeness of the encrypted personal identity number data differed between hospitals, which might result in a systematic error. Thus, matching based on patient and hospital number in the LROI (both numbers generated by the LROI system) can be used to detect primary and revision procedures in the same patient, performed in one hospital. Furthermore, probability matching can be used to match primary and revision procedures in patients who have undergone revision surgery at a different hospital than the hospital for their primary procedure. Using these matching techniques would probably reduce bias to a minimum. The mandatory legal requirement of hospitals to be responsible for the traceability of all implanted prostheses in patients underscores the importance of the value of the LROI.
In conclusion, the Dutch Arthroplasty Register (LROI) now has over 300,000 hip and knee arthroplasty procedures registered since its inception in 2007, and it covers all hospitals. The LROI had a good degree of completeness of registered procedures (more than 95% of primary hip and knee arthroplasty procedures) in 2012 and 2013, and a high validity of the data entered. Completeness and validity increased over time. To improve the quality of the Dutch Arthroplasty Register further, general feedback and audits—including record-by-record checks—will be performed.
Supplementary data
Tables 2–6, are available at Acta’s website (www.actaorthop.org), identification number 8011.
Acknowledgments
LS, GD, FJ, and WM planned the study. SR, GD, JM, and RN were responsible for the dataset. LS and AS performed the analyses. LS wrote the manuscript with substantial contributions from all authors, who also participated in interpretation of the results.
No competing interests declared.
References
- Arthursson AJ, Furnes O, Espehaug B, Havelin LI, Soreide JA. Validation of data in the Norwegian Arthroplasty Register the Norwegian Patient Register: 5,134 primary total hip arthroplasties and revisions operated at a single hospital between 1987 and 2003 . Acta Orthop Scand. 2005;76(6):823–8. doi: 10.1080/17453670510045435. [DOI] [PubMed] [Google Scholar]
- Daneshvar P, Forster AJ, Dervin GF. Accuracy of administrative coding in identifying hip and knee primary replacements and revisions . J Eval Clin Pract. 2012;18(3):555–9. doi: 10.1111/j.1365-2753.2010.01622.x. [DOI] [PubMed] [Google Scholar]
- Dansk Hoftealloplastik Register Årsrapport 2013. http://www.dhr.dk/Ny%20mappe/rapporter/DHR%20årsrapport%202012%20final-2982012.pdf. Dansk Hoftealloplastik Register. Overgaard S, Pedersen AB, Haagen Hjelm A. 2013 [PubMed]
- Engesaeter IO, Lehmann T, Laborie LB, Lie SA, Rosendahl K, Engesaeter LB. Total hip replacement in young adults with hip dysplasia: age at diagnosis, previous treatment, quality of life, and validation of diagnoses reported to the Norwegian Arthroplasty Register between 1987 and 2007 . Acta Orthop Scand. 2011;82(2):149–54. doi: 10.3109/17453674.2011.566146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espehaug B, Furnes O, Havelin LI, Engesaeter LB, Vollset SE, Kindseth O. Registration completeness in the Norwegian Arthroplasty Register . Acta Orthop Scand. 2006;77(1):49–56. doi: 10.1080/17453670610045696. [DOI] [PubMed] [Google Scholar]
- Goldberg J, Gelfand HM, Levy PS. Registry evaluation methods: a review and case study . Epidemiol Rev. 1980;2:210–20. doi: 10.1093/oxfordjournals.epirev.a036224. [DOI] [PubMed] [Google Scholar]
- Herberts P, Malchau H. Long-term registration has improved the quality of hip replacement: a review of the Swedish THR Register comparing 160,000 cases . Acta Orthop Scand. 2000;71(2):111–21. doi: 10.1080/000164700317413067. [DOI] [PubMed] [Google Scholar]
- Kolling C, Simmen BR, Labek G, Goldhahn J. Key factors for a successful National Arthroplasty Register . J Bone Joint Surg Br. 2007;89(12):1567–73. doi: 10.1302/0301-620X.89B12.19409. [DOI] [PubMed] [Google Scholar]
- Landelijke Registratie Orthopedische Implantaten (Dutch Arthroplasty Register) www.lroi.nl. accessed 01-08-2014.
- Lehmann TG, Engesaeter IO, Laborie LB, Lie SA, Rosendahl K, Engesaeter LB. KTotal hip arthroplasty in young adults, with focus on Perthes’ disease and slipped capital femoral epiphysis: follow-up of 540 subjects reported to the Norwegian Arthroplasty Register during 1987–2007 . Acta Orthop Scand. 2012;83(2):159–64. doi: 10.3109/17453674.2011.641105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Steenbergen LN, Denissen GAW, van der Togt CR, van Rooden SM. LROI-Report 2012 Insight into Quality of Orthopaedic Care in the Netherlands. Nederlandse Orthopaedische Vereniging; LROI: ‘s- Hertogenbosch: 2013. LROI-Report 2012 Insight into Quality of Orthopaedic Care in the Netherlands. [Google Scholar]
- Porter M, Borroff M, Gregg P, Howard P, MacGregor A, Tucker K. National Joint Registry for England, Wales and Northern Ireland. National Joint Registry for England, Wales and Northern Ireland, 10th Annual Report 2013; 2013. [Google Scholar]
- Pedersen A, Johnsen S, Overgaard S, Soballe K, Sorensen HT, Lucht U. Registration in the danish hip arthroplasty registry: completeness of total hip arthroplasties and positive predictive value of registered diagnosis and postoperative complications . Acta Orthop Scand. 2004;75(4):434–41. doi: 10.1080/00016470410001213-1. [DOI] [PubMed] [Google Scholar]
- ProMISe. www.msbi.nl/Promise. accessed 15-08-2014.
- Singh JA, Ayub S. Accuracy of VA databases for diagnoses of knee replacement and hip replacement . Osteoarthritis Cartilage. 2010;18(12):1639–42. doi: 10.1016/j.joca.2010.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen HT, Sabroe S, Olsen J. A framework for evaluation of secondary data sources for epidemiological research . Int J Epidemiol. 1996;25(2):435–42. doi: 10.1093/ije/25.2.435. [DOI] [PubMed] [Google Scholar]
- Statistics Netherlands. http://statline.cbs.nl/StatWeb/publication/?DM=SLNL&PA=71430NED&D1=2-3&D2=0&D3=0&D4=0&D5=a&VW=T. accessed 15-07-2014.
- Garellick G, Rogmark C, Kärrholm J, Rolfson O. Swedish Hip Arthroplasty Register. Swedish Hip Arthroplasty Register Annual Report 2012; 2013. [Google Scholar]
- Sundberg M, Lidgren L, W-Dahl A, Robertsson O. Swedish Knee Arthroplasty Register. Swedish Knee Arthroplasty Register Annual Report 2013; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vektis. www.Vektis.nl. >accessed 01-07-2014.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.