Abstract
Objectives
Kidney stones affect nearly one in 11 persons in the United States, and among those experiencing symptoms, emergency care is common. In this population, little is known about the incidence of and factors associated with repeat emergency department (ED) visits. The objective was to identify associations between potentially mutable factors and the risk of an ED revisit for patients with kidney stones in a large, all-payer cohort.
Methods
This was a retrospective cohort study of all patients in California initially treated and released from EDs for kidney stones between February 2008 and November 2009. A multivariable regression model was created to identify associations between patient-level characteristics, area health care resources, processes of care, and the risk of repeat ED visits. The primary outcome was a second ED visit within 30 days of the initial discharge from emergent care.
Results
Among 128,564 patients discharged from emergent care, 13,684 (11%) had at least one additional emergent visit for treatment of their kidney stone. In these patients, nearly one in three required hospitalization or an urgent temporizing procedure at the second visit. On multivariable analysis, the risk of an ED revisit was associated with insurance status (e.g., Medicaid vs. private insurance, OR 1.52, 95% CI = 1.43 to 1.61; P < 0.001). Greater access to urologic care was associated with lower odds of an ED revisit (highest quartile OR 0.88, 95% CI = 0.80 to 0.97; P < 0.01, vs. lowest quartile). In exploratory models, performance of a complete blood count was associated with a decreased odds of revisit (OR = 0.86, 95% CI = 0.75 to 0.97; P = 0.02).
Conclusions
Repeat high-acuity care affects one in nine patients discharged from initial emergent evaluations for kidney stones. Access to urologic care and processes of care are associated with lower risk of repeat emergent encounters. Efforts are indicated to identify preventable causes of ED revisits for kidney stone patients and design interventions to reduce the risk of high-cost, high-acuity, repeat care.
INTRODUCTION
Kidney stones inflict excruciating pain at least once in the lifetime of nearly one in 11 people in the United States.1 The burden of this disease falls largely on the working-age population,2,3 and the economic effect of treating patients with kidney stones is substantial.4 The agony of stone passage is increasingly common: on a population-adjusted basis, the rate of emergency department (ED) visits for stones has nearly doubled, in parallel with the rising prevalence of stone disease.1,5
ED visits for patients with kidney stones are common.5 More than 90% of patients evaluated in EDs for stones are released after treatment.6,7 However, little is known about what happens after discharge from the ED. Some patients are able to pass their stones,8 while others require procedural intervention. While awaiting resolution, some patients experience recurrent renal colic, necessitating repeat ED visits. From the patient perspective, revisits for pain are at best inconvenient and costly. Preventing ED repeated visits is important from the policy perspective because they contribute to inefficient and potentially costly care.9
Given this context, we sought to characterize the frequency of ED revisits in a large, all-payer cohort. We also sought identify potentially independent associations between ED revisits and both clinical and non-clinical factors. To the extent that these factors are mutable, our overarching goal was to identify potential targets for improving emergency care for patients with kidney stones.
METHODS
Study Design
This was a retrospective cohort study. The institutional review boards of the University of California, Los Angeles and Duke University determined that the study design was exempt from review.
Study Setting and Population
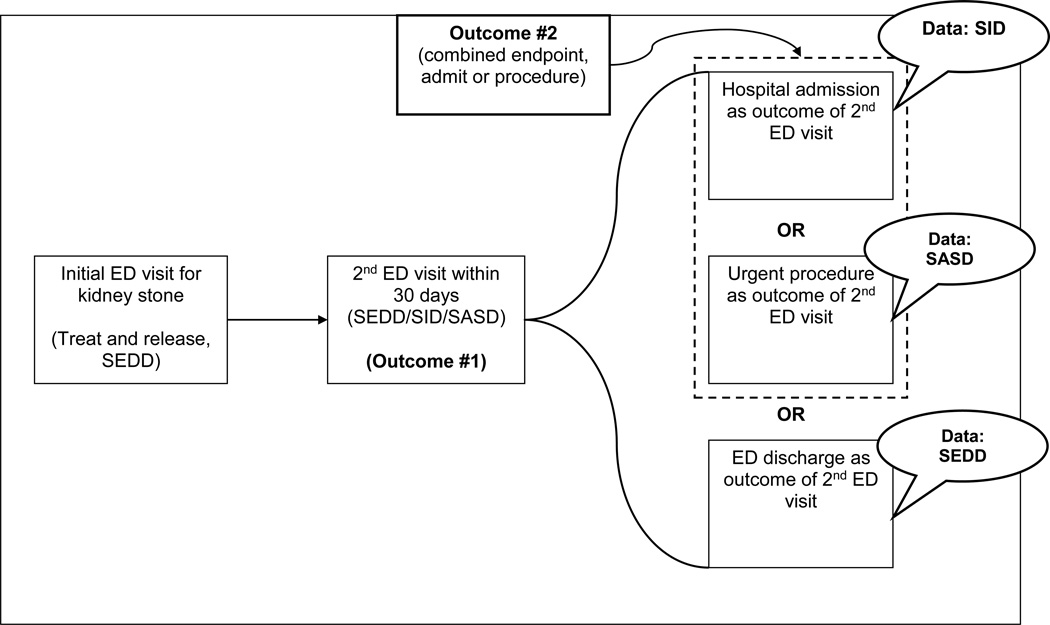
We used data from the California State Emergency Department Database (SEDD), the California State Inpatient Database (SID), and the State Ambulatory Surgery Database (SASD), part of the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality. The SEDD data consist of a 100% sample of ED visits to nonfederal, short-term, general, and specialty hospitals that do not result in inpatient admission; ED visits resulting in admission appear in the SID (Figure 1). Finally, we used the SASD to identify ED revisits that resulted in urgent ambulatory procedures (i.e., ureteral stent placement). These data include identifiers for hospitals, as well as masked patient identifiers that permit linkage of health care encounters across time, between different care settings, and between different facilities. We used the masked patient identifiers to obtain a cohort of patients initially seen and released from ED visits for stones, and then followed for outcome events in all three datasets.
Figure 1. Study design: outcome definitions and data sources.
SID = State Inpatient Database; SASD = State Ambulatory Surgery Database; SEDD = State Emergency Department Database.
The study population consisted of individuals who had initial ED visits for suspected kidney stones in 2008 or 2009 using the SEDD data (Figure 1). We identified patients using established claims algorithms based on diagnostic codes for their visits (Data Supplement).10 Patients aged younger than 18 years or older than 89 years were excluded. We excluded visits in January 2008 in order to avoid left censoring; initial visits in December 2009 were also excluded in order to permit a full 30-day window for follow up.
Our study had two aims. First, we sought to describe the incidence of and variation in ED revisits following an initial treat-and-release ED evaluations. Our primary outcome was thus a second ED visit within 30 days of an initial emergent encounter to treat a kidney stone. While some patients had multiple revisits, we only included the first revisit as an outcome event. ED revisits could appear in the SEDD, SID, or SASD, depending on outcome (i.e., hospital admission; see Study Population and Setting). The SID and SASD include an indicator for encounters originating in the ED. We used this indicator and all three datasets to identify all ED revisits for the cohort (Figure 1).
Our second aim was to characterize clinical outcomes of these revisits. Since death from a kidney stone is a rare event, we instead created a composite outcome of hospital admission or urgent procedure (specifically, placement of temporizing ureteral stent or percutaneous nephrostomy tube, based on established algorithms;10 see Data Supplement) as a result of the revisit (Figure 1). Implicitly, patients with kidney stones who are discharged from initial ED evaluations are deemed clinically suitable for outpatient follow-up. When these patients return to the ED, and then require admission or urgent procedures, these outcomes potentially represent preventable failures of care delivery. In addition, these outcomes are high-acuity, high-cost health care events, and are therefore important from both the patient and health policy perspectives.
Covariates
Patient-level covariates included age, sex, and race and ethnicity as reported by HCUP. We included race and ethnicity data because important variation in the prevalence of kidney stones exists among persons from different backgrounds.1 We included primary payer as reported by HCUP, categorizing as private payer, Medicare, Medicaid, and self-pay/other. As a proxy for socioeconomic status, we included median household income quartile as reported by HCUP. We decided to not explicitly control for comorbid conditions in this analysis for two reasons. First, identifying comorbid conditions from a single ED encounter claim is unreliable, and records from other encounters, such as outpatient clinic visits or inpatient hospitalizations, were not available for all patients in these data. Second, prior claims-based analyses of patients with kidney stones demonstrate that approximately 90% of patients with kidney stones have Charlson scores of 0 or 1, among both commercially insured and Medicare beneficiaries.11–13 Weekend care may differ from weekday care, so we included a variable identifying initial weekend ED visits. Local health care system resources may also influence revisit probability. For example, limited access to urologic care in rural areas negatively affects care outcomes.14,15 Therefore, we included urban-rural classification and also included the per capita density of urologists at the Federal Information Processing Standards level, grouped in quartiles, as reported in the Area Resource File.
In addition to these patient- and area-level covariates, we hypothesized that processes of care, such as diagnostic testing, could influence the probability of a revisit. Therefore, we examined associations between the probability of a revisit and specific diagnostic tests performed at the initial ED encounter. Laboratory and imaging tests were identified using Common Procedural Terminology (CPT) codes (Data Supplement). We created four variables denoting the receipt of diagnostic testing implicit in current guidelines. Current guidelines16,17 suggest that CT scan has the highest diagnostic performance for identifying kidney stones, although renal ultrasound and plain abdominal radiography are acceptable alternatives depending on clinical context (e.g., renal ultrasound for pregnant women). Therefore, we created an indicator variable for receipt of any potentially appropriate imaging test (Data Supplement). Current guidelines also recommend urinalysis (for bacteriuria), assessment for signs of infection or sepsis, such as leukocytosis, and measurement of renal function.18 For each of these three tests, we created a separate indicator variable (Data Supplement). Since the reliability of identifying laboratory tests in ED claims data may be uncertain, we performed several sensitivity analyses (see Data Analysis).
Data Analysis
We calculated the frequency of revisits for each baseline characteristic, and then compared these using the chi-square test. Subsequently, we modeled the binary response of a repeat visit using a generalized linear mixed model with a logit link, controlling for age, sex, race, urban-rural classification, primary payer, household income, weekend visit, and per capita urologist density, accounting for clustering of outcomes at the facility level by adding a random intercept. The rates of missing data were extremely low for these covariates (sex, age, payer, urban-rural location, weekend admission, and urologist density all <1%; race 5%), and therefore we excluded cases with missing data. We subsequently used an identical approach to model the probability of the combined outcome of hospitalization or urgent procedure as a result of the ED revisit.
We then constructed a separate generalized linear mixed model with a logit link to examine associations between the probability of an ED revisit and receipt of guidelines-based diagnostic testing at the initial visit, again controlling for age, sex, race, urban-rural classification, primary payer, household income, weekend visit, and per capita urologist density, and accounting for clustering of outcomes at the facility level. Each ED visit record reports the number of procedure codes on the claim, and not all claims for the initial visits reported procedure codes. Therefore, we designated tests as missing if the visit records reported no procedure codes. Given that the reliability of coding for diagnostic tests is uncertain in these ED data, and may vary substantially between different facilities, we elected to perform a sensitivity analysis to assess the robustness of our results. To explore the stability of the initial estimates, we created a model using only records from patients seen at facilities that reported a median of at least four procedure codes per record. This sensitivity analysis therefore limited observations to patients evaluated at facilities that consistently coded procedures, and conceptually could reduce ascertainment bias. All statistical testing was two-sided, with a Type 1 error rate set to 0.05. We used SAS version 9.2 for all analyses.
RESULTS
The study population consisted of 128,564 subjects who had initial treat-and-release visits to EDs for kidney stones during the study period (Table 1). Among these, 61% were male and over 80% were aged between 18 and 59 years. Nearly two-thirds were white, non-Hispanic, and an additional 25% were Hispanic. More than half (58%) were privately insured.
Table 1.
Characteristics of Study Cohort, n (%)
| Characteristic | Overall (N=128,564) |
Revisit: No (n=114,880) |
Revisit: Yes (n=13,684) |
P value |
|---|---|---|---|---|
| Age group, yrs | ||||
| 18 to 39 | 46,775 (36.4) | 41,508 (36.1) | 5,267 (38.5) | <0.001 |
| 40 to 59 | 58,912 (45.8) | 52,727 (45.9) | 6,185 (45.2) | |
| 60 to 75 | 18,193 (14.2) | 16,402 (14.3) | 1,791 (13.1) | |
| 75 to 89 | 4,684 (3.6) | 4,243 (3.7) | 441 (3.2) | |
| Sex | ||||
| Male | 78,429 (61.3) | 70,162 (61.4) | 8,267 (60.6) | 0.056 |
| Female | 49,509 (38.7) | 44,123 (38.6) | 5,386 (39.4) | |
| Race/Ethnicity | ||||
| White, Non-Hispanic | 75,040 (61.7) | 66,514 (61.3) | 8,526 (64.4) | <0.001 |
| Black, Non-Hispanic | 5,344 (4.4) | 4,836 (4.5) | 508 (3.8) | |
| Hispanic | 29,878 (24.6) | 26,747 (24.7) | 3,131 (23.6) | |
| Other | 11,408 (9.4) | 10,328 (9.5) | 1,080 (8.2) | |
| Urban-Rural Classification | ||||
| Large metro | 93,061 (72.6) | 83,386 (72.8) | 9,675 (70.9) | <0.001 |
| Small metro | 30,797 (24.0) | 27,369 (23.9) | 3,428 (25.1) | |
| Micropolitan | 2,902 (2.3) | 2,555 (2.2) | 347 (2.5) | |
| Non metro/micro | 1,411 (1.1) | 1,216 (1.1) | 195 (1.4) | |
| Primary payer | ||||
| Medicare | 15,401 (12.0) | 13,809 (12.0) | 1,592 (11.6) | <0.001 |
| Medicaid | 13,260 (10.3) | 11,386 (9.9) | 1,874 (13.7) | |
| Private insurance | 75,043 (58.4) | 67,543 (58.8) | 7,500 (54.8) | |
| Other | 24,824 (19.3) | 22,111 (19.3) | 2,713 (19.8) | |
| Household income | ||||
| First quartile (low) | 28,647 (22.8) | 25,525 (22.7) | 3,122 (23.3) | 0.009 |
| Second quartile | 32,127 (25.5) | 28,681 (25.5) | 3,446 (25.7) | |
| Third quartile | 32,307 (25.7) | 28,804 (25.6) | 3,503 (26.1) | |
| Fourth quartile (high) | 32,756 (26.0) | 29,429 (26.2) | 3,327 (24.8) | |
| Urologists per capita | ||||
| First quartile (low) | 33,597 (26.2) | 29,752 (26.0) | 3,845 (28.2) | <0.001 |
| Second quartile | 30,525 (23.8) | 27,206 (23.8) | 3,319 (24.4) | |
| Third quartile | 35,255 (27.5) | 31,638 (27.6) | 3,617 (26.6) | |
| Fourth quartile (high) | 28,699 (22.4) | 25,862 (22.6) | 2,837 (20.8) | |
| Day of visit | ||||
| Mon-Fri | 91,697 (71.3) | 81,893 (71.3) | 9,804 (71.6) | 0.379 |
| Sat/Sun | 36,867 (28.7) | 32,987 (28.7) | 3,880 (28.4) |
Within 30 days of the initial ED visit, 13,684 (11%) subjects each had at least one additional emergent visit for treatment of their kidney stones (Table 1). ED revisits were more common among younger patients. There was no difference in revisit proportions between males and females; small differences in revisits were noted across racial and ethnic groups. Revisits were lowest among subjects with private insurance and highest among Medicaid beneficiaries (10% vs. 14%, p < 0.001). Revisits were also more common in rural areas and where the local urology workforce supply was low. At the facility level, the mean revisit rate varied considerably (11%, SD ±4.7%), and more than two-thirds of EDs had repeat visit rates between 6% and 16%.
Differences in the probability of an ED revisit persisted after controlling for important covariates (Table 2). ED revisits remained more likely among younger and white, non-Hispanic subjects. The odds of an ED revisit were 52% higher among Medicaid beneficiaries (OR 1.52, 95% CI = 1.43 to 1.61), as compared with those with private insurance. A high per capita density of urologists was associated with lower odds of an ED revisit (highest quartile OR 0.88, 95% CI = 0.80 to 0.97 vs. lowest quartile). There was no difference in the odds of an ED revisit when the initial evaluation occurred on the weekend.
Table 2.
Characteristics Associated with ED Revisit
| Characteristic | Odds Ratio (95% CI) | P value |
|---|---|---|
| Age group, yrs | <0.001 | |
| 18 to 39 | 1 (referent) | |
| 40 to 59 | 0.95 (0.91–0.99) | |
| 60 to 75 | 0.86 (0.80–0.92) | |
| 75 to 89 | 0.78 (0.69–0.88) | |
| Female | 0.98 (0.95–1.02) | 0.35 |
| Race/Ethnicity | <0.001 | |
| White, Non-Hispanic | 1 (referent) | |
| Black, Non-Hispanic | 0.78 (0.70–0.86) | |
| Hispanic | 0.87 (0.83–0.91) | |
| Other | 0.82 (0.77–0.88) | |
| Primary payer | <0.001 | |
| Private insurance | 1 (referent) | |
| Medicare | 1.13 (1.05–1.22) | |
| Medicaid | 1.52 (1.43–1.61) | |
| Other | 1.12 (1.07–1.18) | |
| Urban-rural classification | 0.12 | |
| Large metro | 1 (referent) | |
| Small metro | 0.94 (0.86–1.03) | |
| Micropolitan | 0.95 (0.82–1.11) | |
| Non metro/micro | 1.14 (0.95–1.38) | |
| Household Income | 0.11 | |
| First quartile | 1 (referent) | |
| Second quartile | 1.01 (0.95–1.06) | |
| Third quartile | 1.03 (0.97–1.09) | |
| Fourth quartile | 0.96 (0.90–1.03) | |
| Urologists per capita | 0.005 | |
| First quartile | 1 (referent) | |
| Second quartile | 0.99 (0.90–1.09) | |
| Third quartile | 0.90 (0.82–1.00) | |
| Fourth quartile | 0.88 (0.79–0.97) | |
| Weekend visit | 0.99 (0.95–1.03) | 0.68 |
Outcomes of Revisits
Among the 13,684 subjects who experienced ED revisits, 3,069 (29%) were either admitted to the hospital or underwent an urgent procedure as a result of the revisit. These outcomes varied substantially by clinical and non-clinical factors on multivariable analysis (Table 3). As compared with young subjects, the odds of hospitalization or urgent procedures were very high among those aged at least 75 years (OR 3.90, 95% CI = 3.03 to 5.02). Females were more likely to be admitted or undergo urgent procedures than males (OR 1.82, 95% CI = 1.67 to 2.00). When subjects returned to the ED, those living in areas with the highest per capita supply of urologists were most likely to be hospitalized or undergo a procedure (OR 1.77, 95% CI = 1.38 to 2.27).
Table 3.
Characteristics Associated with Hospitalization or Urgent Procedure as a Result of ED Revisit
| Characteristic | Odds Ratio (95% CI) | P value |
|---|---|---|
| Age group, yrs | ||
| 18 to 39 | 1 (referent) | |
| 40 to 59 | 1.59 (1.44–1.75) | |
| 60 to 75 | 1.91 (1.64–2.22) | <0.001 |
| 75 to 89 | 3.90 (3.03–5.02) | |
| Female | 1.82 (1.67–1.99) | <0.001 |
| Race/Ethnicity | ||
| White, Non-Hispanic | 1 (referent) | |
| Black, Non-Hispanic | 0.94 (0.74–1.18) | |
| Hispanic | 0.85 (0.76–0.95) | 0.05 |
| Other | 0.94 (0.80–1.10) | |
| Primary payer | ||
| Private insurance | 1 (referent) | |
| Medicare | 1.39 (1.19–1.63) | |
| Medicaid | 1.13 (0.99–1.29) | <0.001 |
| Other | 0.73 (0.64–0.82) | |
| Urban-rural classification | ||
| Large metro | 1 (referent) | |
| Small metro | 1.03 (0.83–1.27) | |
| Micropolitan | 0.64 (0.42–0.97) | 0.11 |
| Non metro/micro | 0.94 (0.59–1.48) | |
| Household income | ||
| First quartile | 1 (referent) | |
| Second quartile | 1.06 (0.93–1.21) | |
| Third quartile | 0.95 (0.83–1.09) | 0.40 |
| Fourth quartile | 1.00 (0.86–1.16) | |
| Urologists per capita | ||
| First quartile | 1 (referent) | |
| Second quartile | 1.22 (0.97–1.54) | |
| Third quartile | 1.54 (1.20–1.97) | <0.001 |
| Fourth quartile | 1.77 (1.38–2.27) | |
| Initial weekend visit | 1.00 (0.91–1.10) | 0.96 |
Diagnostic testing
Among the diagnostic tests recommended for the evaluation of a patient with a suspected kidney stone, only performance of a blood count was associated with the probability of an ED revisit (Table 4). Patients who had a white blood cell count performed at the initial visit had 14% lower odds of experiencing an ED revisit (OR 0.86, 95% CI = 0.75 to 0.97). This association remained stable when restricting the analysis to facilities reporting a median of at least four procedure codes on each claim (OR 0.86, 95% CI = 0.76 to 0.98). In contrast, urinalysis, imaging, and assessment of renal function were not associated with the odds of an ED revisit.
Table 4.
Associations between performance of guideline-recommended testing and ED revisit*
| Test | Odds Ratio (95% CI) | P value |
|---|---|---|
| Imaging | 1.03 (0.96–1.10) | 0.41 |
| Complete blood count | 0.86 (0.75–0.97) | 0.02 |
| Renal function | 1.12 (0.99–1.27) | 0.08 |
| Urinalysis | 0.95 (0.89–1.03) | 0.22 |
Controlling for age, sex, race, payer, urban-rural classification, household income, urologist density per capita, weekend visit, and clustering at facility level.
DISCUSSION
We report the novel finding that up to one in nine patients requires repeat ED care within 30 days of a first ED visit for a kidney stone; among these patients, nearly one in three requires an urgent procedure or hospitalization as a result of the revisit. The probability of a repeat ED visit varies substantially among facilities. The probability of a revisit is associated with non-clinical factors, such as insurance status and local urologic health care resources. Non-use of a complete blood cell count was associated with increased risk for an ED revisit. These key findings suggest that repeat ED care is an important problem, and a potential quality of care marker for patients with kidney stones.
From the patient perspective, an ED visit for a kidney stone is a significant event, typically prompted by excruciating pain. This burden of acute disease falls primarily on a working-age population (over 80% of patients in our sample) and likely imposes substantial indirect costs, in addition to the high direct costs of emergent care.3,6 Our findings suggest that after being treated and released the first time, more than 10% of patients experience additional symptoms within the next month that require an additional ED visit.
The costs of care for patients with kidney stones are substantial, and thus repeat ED visits and their sequelae are health-policy relevant. Aggregate expenditures for treating patients with kidney stones are among the greatest for any urologic condition; data from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Urologic Diseases in America project estimated charges in excess of $10 billion annually.4 Hospitalizations and procedures constitute the largest proportion of this spending. An important opportunity to reduce costs and improve outcomes exists, to the extent that these ED revisits and their sequelae can be reduced by optimizing care.
The hypothesis that some of these ED revisits are affected by non-clinical factors is supported by key findings from our investigation. At the ED level, revisit frequencies varied widely, with more than two-thirds of facilities falling in the range of 6% to 16% revisit probability. Insurance status was strongly associated with risk of revisits, and notably these risks were higher for patients with Medicaid or no insurance coverage, as compared to privately insured individuals. Insurance coverage may be a proxy for access to primary care, or urologic care, either of which could reduce the likelihood that a follow-up visit occurs in the ED setting. In areas with the lowest physician supply of urologists, the odds of an ED revisit were 14% higher than in areas with the highest urologist supply. We noted an intriguing association between receipt of complete blood count testing and a decreased risk of revisit. This finding must be interpreted cautiously as hypothesis-generating. A plausible clinical explanation for this association is not recognizing impending systemic infection could potentially result in an emergent revisit because of delays in treatment, such as antibiotics. Using clinical data, a recent cohort study of patients evaluated in the ED for a symptomatic stone found that leukocytosis was associated with the risk of ED revisit.19 A 2007 guideline recommends evaluation for signs of systemic infection,18 but no specific guidance was provided on which test(s) should be ordered, and the guideline authors rated this as Level IV evidence (i.e. expert panel opinion). This finding may also be limited by ascertainment bias. To explore the potential for ascertainment bias further, we performed a sensitivity analysis limiting the population to hospitals with relatively high frequencies of diagnostic test codes on the discharge record (median ≥4 per record). In this sensitivity analysis, the OR remained stable and statistically significant. We believe this finding should, at a minimum, prompt rigorous assessment of the clinical utility of leukocytosis in the management of acute renal colic, and its potential relationship with quality of care for these patients.
Another important consideration for interpretation of these results is the outcome of hospitalization or urgent procedure, which occurred in nearly one in three patients with second ED visits. Only 10% of patients are admitted as a result of their first ED visits,5–7 and thus the second ED visit carries nearly triple the risk of hospitalization or urgent intervention. If hospitalization occurs due to poor access to urologic or primary care, or an incomplete evaluation for signs of infection, then this outcome may be potentially avoidable if different care is provided at the index visit. Alternately, hospitalization could represent a clinically appropriate escalation of best prior care, albeit the result of an inefficient, costly, and inconvenient second ED visit. Instead of a second ED visit, a more efficient and higher quality strategy would be escalation through a usual source of primary care, or through access to urologic care. Future investigations should more closely explore the role of primary care and urologic care access for the management of symptomatic kidney stone patients who are discharged from the ED.
LIMITATIONS
These data represent a single large state, and therefore may not generalize to treatment of patients with kidney stones in other areas, or nationally. The dataset lacks potentially important clinical detail, particularly with respect to clinical history, physiological information, disease severity, or indications for return. Therefore, the association between laboratory testing and revisits must be regarded as hypothesis-generating. The National Hospital Ambulatory Medical Care Survey (NHAMCS) queries whether patients were seen in the ED within 72 hours before the sampled visit, although detailed information about the reason for the prior visit is not recorded. In reports from NHAMCS, about 10% of subjects evaluated emergently for stones report prior ED visits,5,6 suggesting that the revisit frequency of 11% observed in our more granular data retains validity. Some factors, such as insurance status, could change between visits; we only included data from the first visit in our analysis. Missing data could bias results, although the proportion of observations was very low. We observe variation in risk of ED revisits, hospitalizations, and urgent procedures along racial and ethnic lines; since these traits are immutable, and observed associations are likely a proxy for other factors, further investigation to understand these risk differences is warranted.
Our analysis pertains only to those patients discharged from initial ED visits, although this constitutes 90% of patients receiving emergent care for stones.5–7 We used an area-level measure of socioeconomic status, which is imperfect due to heterogeneity within geographic areas. Nonetheless, our findings highlight the previously poorly described phenomenon of repeat ED visits for patients with kidney stones.
CONCLUSIONS
Our findings suggest that ED revisits are not uncommon for kidney stone patients who are initially treated and released. ED revisits are fairly likely to result in hospital admission or urgent procedures. Furthermore, observed associations between revisit risk and markers for access and quality of care suggest that mutable factors, such as care processes, may influence patient- and policy-relevant outcomes. These results should motivate efforts to identify preventable causes of ED revisits for patients with kidney stones and design interventions to reduce the risk of high-cost, high-acuity, repeat care.
Supplementary Material
Acknowledgments
This work was initiated while Dr. Scales was a Robert Wood Johnson Foundation/VA Clinical Scholar at the David Geffen School of Medicine at UCLA.
FUNDING / SUPPORT
Dr. Scales was supported by the Robert Wood Johnson Foundation and the VA Office of Academic Affiliations through the VA/Robert Wood Johnson Clinical Scholars Program.
Dr. Mangione received support from the UCLA Robert Wood Johnson Clinical Scholars Program and the U.S. Department of Veterans Affairs (Grant #67799), the University of California at Los Angeles (UCLA), Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly under National Institutes of Health (NIH)/NIA Grant P30-AG021684, and from NIH/National Center for Advancing Translational Sciences UCLA Clinical and Translational Science Institute Grant UL1TR000124. Dr. Mangione holds the Barbara A. Levey and Gerald S. Levey Endowed Chair in Medicine, which partially supported her work.
The Urologic Diseases in America Project is supported by grant HHSN276201200016C from the National Institute of Diabetes and Digestive and Kidney Diseases and the National Library of Medicine.
The views expressed in this article are those of the authors and do not necessarily reflect the position and policy of the United States Federal Government or the Department of Veterans Affairs. No official endorsement should be inferred.
ROLE OF THE SPONSORS:
The funding sources had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation or review of the manuscript; or decision to submit for publication. The Robert Wood Johnson Foundation and US Department of Veterans Affairs had no role in approval of the manuscript. The Executive Committee of the Urologic Diseases in America Project includes representatives from the National Institute of Diabetes and Digestive and Kidney Diseases; the Executive Committee approves project manuscripts based on technical considerations alone but otherwise has no role in the study.
* GROUP INFORMATION
The members of the NIDDK Urologic Diseases in America Project are: Mark S. Litwin, MD MPH, Department of Urology, David Geffen School of Medicine and Fielding School of Public Health, University of California, Los Angeles; Christopher S. Saigal, MD MPH, Department of Urology, David Geffen School of Medicine, UCLA and RAND Corporation; Paul Eggers, PhD, National Institute of Diabetes and Digestive and Kidney Diseases, Washington, DC; Tamara Bavendam, MD, National Institute of Diabetes and Digestive and Kidney Diseases, Washington DC; Ziya Kirkali, MD, National Institute of Diabetes and Digestive and Kidney Diseases, Washington, DC.
Footnotes
Prior Presentations: none
None of the authors have conflicts of interest to disclose.
REFERENCES
- 1.Scales CD, Jr, Smith AC, Hanley JM, Saigal CS. Prevalence of kidney stones in the United States. Eur Urol. 2012;62(1):160–165. doi: 10.1016/j.eururo.2012.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 2003;63:1817–1823. doi: 10.1046/j.1523-1755.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 3.Saigal CS, Joyce G, Timilsina AR. Direct and indirect costs of nephrolithiasis in an employed population: opportunity for disease management? Kidney Int. 2005;68:1808–1814. doi: 10.1111/j.1523-1755.2005.00599.x. [DOI] [PubMed] [Google Scholar]
- 4.Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Washington, DC: US Government Printing Office; 2012. NIH Publication No. 12–7865. [Google Scholar]
- 5.Fwu CW, Eggers PW, Kimmel PL, Kusek JW, Kirkali Z. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;83:479–486. doi: 10.1038/ki.2012.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hyams ES, Matlaga BR, Korley FK. Practice patterns in the emergency care of kidney stone patients: an analysis of the National Hospital Ambulatory Medical Care Survey (NHAMCS) Can J Urol. 2012;19:6351–6359. [PubMed] [Google Scholar]
- 7.Brown J. Diagnostic and treatment patterns for renal colic in US emergency departments. Int Urol Nephrol. 2006;38:87–92. doi: 10.1007/s11255-005-3622-6. [DOI] [PubMed] [Google Scholar]
- 8.Hollingsworth JM, Rogers MA, Kaufman SR, et al. Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet. 2006;368:1171–1179. doi: 10.1016/S0140-6736(06)69474-9. [DOI] [PubMed] [Google Scholar]
- 9.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 10.Pearle MS, Calhoun EA, Curhan GC. Urologic diseases in America project: urolithiasis. J Urol. 2005;173:848–857. doi: 10.1097/01.ju.0000152082.14384.d7. [DOI] [PubMed] [Google Scholar]
- 11.Scales CD, Jr, Krupski TL, Curtis LH, et al. Practice variation in the surgical management of urinary lithiasis. J Urol. 2011;186:146–150. doi: 10.1016/j.juro.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scales CD, Jr, Saigal CS, Hanley JM, et al. The impact of unplanned postprocedure visits in the management of patients with urinary stones. Surgery. 2014;155:769–775. doi: 10.1016/j.surg.2013.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scales CD, Jr, Lai JC, Dick AW, et al. Comparative effectiveness of shock wave lithotripsy and ureteroscopy for treating patients with kidney stones. JAMA Surg. 2014;149(7):648–653. doi: 10.1001/jamasurg.2014.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Odisho AY, Cooperberg MR, Fradet V, Ahmad AE, Carroll PR. Urologist density and county-level urologic cancer mortality. J Clin Oncol. 2010;28:2499–2504. doi: 10.1200/JCO.2009.26.9597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Odisho AY, Fradet V, Cooperberg MR, Ahmad AE, Carroll PR. Geographic distribution of urologists throughout the United States using a county level approach. J Urol. 2009;181:760–765. doi: 10.1016/j.juro.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 16.Coursey CA, Casalino DD, Remer EM, et al. Acute onset flank pain - suspicion of stone disease. Ultrasound Q. 2012;28(3):227–233. doi: 10.1097/RUQ.0b013e3182625974. [DOI] [PubMed] [Google Scholar]
- 17.Fulgham P, Assimos DG, Pearle MS, Preminger GM. Clinical effectiveness protocols for imaging in the management of ureteral calculous disease. J Urol. 2013;189(4):1203–1213. doi: 10.1016/j.juro.2012.10.031. [DOI] [PubMed] [Google Scholar]
- 18.Preminger GM, Tiselius HG, Assimos DG, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007;178:2418–2434. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 19.Sfoungaristos S, Hidas G, Gofrit ON, et al. A novel model to predict the risk of readmission in patients with renal colic. J Endourology. 2014;28:1011–1015. doi: 10.1089/end.2014.0082. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.