Abstract
Background
The updated (2014) National Institute for Health and Care Excellence (NICE) guideline lowered the recommended threshold for statin prescription from 20% to 10% 10-year cardiovascular disease (CVD) risk.
Aim
To determine the characteristics of patients prescribed statins for primary prevention according to their CVD risk.
Design and setting
Cross-sectional study in primary care settings in the three east London CCGs (Newham, City and Hackney, and Tower Hamlets).
Method
Data were extracted from electronic health records of 930 000 patients registered with 137 of 141 general practices for a year ending 1 April 2014.
Results
Of 341 099 patients aged 30–74 years, excluding those with CVD or diabetes, 22 393 were prescribed statins and had a 10-year CVD risk recorded. Of these, 9828 (43.9%) had a CVD risk ≥20%, 7121 (31.8%) had a CVD risk of 10–19%, and 5444 (24.3%) had a CVD risk <10%. Statins were prescribed to 9828/19 755 (49.7%) of those at ≥20% CVD risk, to 7121/37 111 (19.2%) of those with CVD risk 10–19%, and to 5444/146 676 (3.7%) of those with CVD risk <10%. Statin prescription below the 20% CVD risk threshold targeted individuals in the 10–19% risk band in association with hypertension, high serum cholesterol, positive family history, older age, and south Asian ethnicity.
Conclusion
This study confirms continuing undertreatment of patients at highest CVD risk (≥20%). GPs prescribed statins to only one-fifth of those in the 10–19% risk band usually in association with known major risk factors. Only 3.7% of individuals below 10% were prescribed statins.
Keywords: cardiovascular prevention, cardiovascular risk, primary care, statins
INTRODUCTION
Before 2014, National Institute for Health and Care Excellence (NICE) guidance recommended statin treatment in individuals at a 10-year cardiovascular disease (CVD) risk of 20%.1 In 2014, NICE reduced this treatment threshold to 10%1 and in the US a CVD risk level of 5.0–7.5% was recommended based on trial evidence of CVD benefit.2,3
Two studies examined statin treatment for primary prevention in the UK up until 2010–2011.4,5 They concluded that statin prescribing for primary prevention was poorly targeted according to the guidance at the time. van Staa et al used a 2011 nationally representative sample of general practices with 300 914 patients prescribed statins, excluding those with diabetes and CVD.5 From 2007 to 2011, 30.4% of ‘eligible’ patients with a 10-year CVD risk of ≥20% were prescribed a statin. Of those with a 10–19% CVD risk, 18% were prescribed statins and in those at <10% risk, statins were prescribed for 3.5%. The authors concluded that:
‘There appeared to be a substantive overuse in patients with low CVD risk as well as underuse in those with high CVD risk.’5
Wu et al used a separate national general practice database for the earlier years 2008–2010.4 The cohort of 365 718 patients excluded those with CVD and included those with diabetes. In total, 28.5% of those with diabetes or a 10-year CVD risk of ≥20%, and 10.1% of patients below this threshold, were prescribed lipid-lowering medication. The authors concluded:
‘ … most statins are prescribed to patients who are not eligible for treatment … Overall we find more evidence to support the view that prescribing of statins is influenced more by single risk factors treated as categories (age ≥65 years; diabetes; total cholesterol ≥7 mmol/l) …’4
Since the national NHS Health Check started in 2009, statins have been promoted in the east London Clinical Commissioning Groups (CCGs) of Newham, City and Hackney, and Tower Hamlets with a systematic programme incentivising uptake and statin prescription in patients with a CVD risk of ≥20%.6 Of those aged 40–74 years who are eligible in any 1 year, 67% are currently attending an NHS Health Check.7 These three CCGs were also top in London in the 2013 national Quality and Outcomes Framework for control of CVD risk factors for patients with diabetes and coronary heart disease, with the highest per capita statin prescribing nationally.8
In these localities in which prescribing of statins above 20% CVD risk had been strongly supported, the aim of this study was to determine factors associated with statin prescribing at lower CVD risk.
How this fits in
In 2014, the recommended NICE threshold for statin treatment for the primary prevention of cardiovascular disease (CVD) changed from a 10-year CVD risk of 20% to 10%. In 2013–2014, this study found that in individuals at highest risk (≥20% 10-year CVD risk), only one-half were prescribed statins. In the 10–19% CVD risk band, one-fifth were treated with statins. The treatment of those at ≥20% CVD risk (including those aged ≥75 years) is a feasible goal. However, extension to the lower risk band is unlikely to treat most patients at 10–19% CVD risk. Nor will it address high lifetime risk in patients of younger ages for whom population measures to improve risk factors would have a greater impact.
METHOD
The study conformed to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidance on cohort studies (http://www.strobe-statement.org/). Data were used from electronic health records in 137 out of 141 general practices serving a registered population of 930 000 patients in the east London CCGs of City and Hackney, Tower Hamlets, and Newham for a period of 1 year ending on the index date of 1 April 2014. Data from four practices could not be accessed because they used a different computer system. All contributing practices used the same web-enabled record system (Egton Medical Information Services, EMIS) with agreed data-entry templates to ensure consistent data entry and coding. Data were obtained for all patients aged 30–74 years and who were registered at least 1 year before the search date. Patients with CVD (angina, ischaemic heart disease [IHD], stroke, and peripheral vascular disease), and types 1 and 2 diabetes were excluded. QRISK® was used for all CVD risk estimation. Variables included:
statin prescription within 6 months;
sex;
age group (≤44 years, 45–54 years, 55–64 years, and 65–74 years);
CCG locality;
ethnic group (white, black African/Caribbean, South Asian, other, and not stated);
national quintiles of Townsend score (1 [least deprived] to 5 [most deprived]);
presence or absence of positive IHD family history in first-degree relatives aged <60 years, with missing values considered negative;
latest smoking status (currently smoking or not);
highest recorded systolic blood pressure (<140 mmHg, 140–159 mmHg, and ≥160 mmHg);
highest recorded total cholesterol (<5.0 mmol/L, 5.0–6.9 mmol/L, and ≥7.0 mmol/L); and
antihypertensive drug treatment within 5 years.
The authors used the highest recorded QRISK® (http://www.qrisk.org/) value within 5 years, to determine 10-year CVD risk banding of:
<5%;
5–9%;
10–14%;
15–19%; and
≥20%.
Values of blood pressure and cholesterol exceeding clinical ranges were excluded.
Statistical analysis
All analyses were performed using Stata (version 12). Multivariate regression analysis was used to assess the relationship between statin prescription and explanatory variables. The model was adjusted for clustering by practice and P<0.05 was considered to represent statistical significance.
RESULTS
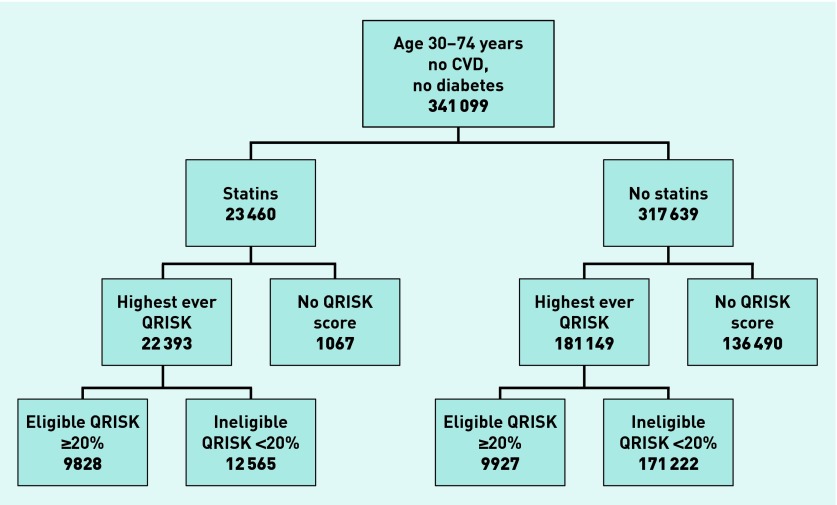
Figure 1 describes the statin prescription at each stage of the analysis by CVD risk. From a total of 341 099 patients aged 30–74 years without CVD or diabetes, 203 542 (59.6%) had their CVD risk recorded. Of the remaining 137 557 with no CVD risk calculated, 1067 (0.8%) were on statins (Figure 1).
Figure 1.
Flow chart to illustrate statin by CVD risk.
Table 1 describes the CVD risk distribution of patients who were prescribed statins in the preceding 6 months compared with those who were not. Of the 19 755 patients with a CVD risk of ≥20%, 9828 (49.7%) had been prescribed a statin in the preceding 6 months. Of those 37 111 patients in the 10–19% CVD risk band, 7121 (19.2%) were prescribed statins. Of the total 22 393 patients prescribed statins for primary prevention, 9828 (43.9%) had a CVD risk of ≥20% and conversely 56.1% were <20% CVD risk.
Table 1.
Patients in each cardiovascular disease risk group prescribed statins within the preceding 6 months
| Cardiovascular disease risk, n (%) | ||||||
|---|---|---|---|---|---|---|
| <5 | 5–9 | 10–14 | 15–19 | ≥20 | TOTAL | |
| No statins | 99 796 | 41 436 | 19 235 | 10 755 | 9927 | 181 149 |
| Statins | 1826 (1.8) | 3618 (8.0) | 3629 (15.9) | 3492 (24.5) | 9828 (49.7) | 22 393 (11.0) |
| TOTAL | 101 622 | 45 054 | 22 864 | 14 247 | 19 755 | 203 542 |
Of the 12 565 patients prescribed statins whose CVD risk was <20% 7121/12 565 (56.7%) had a CVD risk of 10–19%. Of those with CVD risk <10%, 5444/146 676 (3.7%) were prescribed statins. In other words, statin prescription in those with CVD risk <10% represented 5444/22 393 (24.3%) of total statin prescription for primary prevention.
In the unadjusted analyses of those patients prescribed statins below the 20% threshold (Table 2), females (7.8%) were more likely than males (5.9%), to be prescribed statins (P<0.001). Statin prescription below the 20% threshold was more likely in Newham (9.6%) than in the other two localities (5.4%, 5.5%); among South Asians than other ethnic groups (9.5% versus 6.3–6.9%); in those in the second least deprived quintile (14.0% versus the most deprived, 6.7%); and among those with a positive family history of premature IHD (9.0% versus in those without, 6.2% [P<0.001]).
Table 2.
Characteristics of those ineligible for statins (CVD risk <20%) by statin status
| Not on statin, n (%) | On statin, n (%) | |||
|---|---|---|---|---|
| Total | 171 222 | 12 565 | ||
|
| ||||
| Male | 86 628 | (94.1) | 5383 | (5.9) |
| Female | 84 594 | (92.2) | 7182 | (7.8) |
|
| ||||
| Locality | ||||
| Tower Hamlets | 54 289 | (94.5) | 3136 | (5.5) |
| City and Hackney | 59 870 | (94.6) | 3394 | (5.4) |
| Newham | 57 063 | (90.4) | 6035 | (9.6) |
|
| ||||
| Age group, years | ||||
| ≤44 | 73 355 | (97.8) | 1661 | (2.2) |
| 45–54 | 65 287 | (93.8) | 4291 | (6.2) |
| 55–64 | 26 430 | (85.5) | 4499 | (14.5) |
| 65–74 | 6150 | (74.4) | 2114 | (25.6) |
|
| ||||
| Ethnicity | ||||
| White | 71 917 | (93.7) | 4866 | (6.3) |
| South Asian | 37 165 | (90.5) | 3884 | (9.5) |
| Black African/Caribbean | 36 514 | (93.1) | 2698 | (6.9) |
| Other | 10 455 | (93.4) | 738 | (6.6) |
| Not stated | 3484 | (96.2) | 136 | (3.8) |
| Missing | 11 687 | 243 | ||
|
| ||||
| National Townsend quintile | ||||
| 1 least deprived | 49 | (85.0) | 8 | (14.0) |
| 2 | 364 | (85.1) | 64 | (15.0) |
| 3 | 1614 | (89.3) | 193 | (10.7) |
| 4 | 30 268 | (92.9) | 2305 | (7.1) |
| 5 most deprived | 138 614 | (93.3) | 9967 | (6.7) |
| Missinga | 313 | 28 | ||
|
| ||||
| Family history of premature IHD (aged <60 years) | ||||
| Yes | 39 432 | (91.0) | 3909 | (9.0) |
| No | 131 790 | (93.8) | 8656 | (6.2) |
|
| ||||
| Antihypertensive therapy | ||||
| Yes | 23 756 | (76.5) | 7311 | (23.5) |
| No | 147 466 | (96.6) | 5254 | (3.4) |
|
| ||||
| Smoking status | ||||
| Not smoking | 134 541 | (92.7) | 10662 | (7.3) |
| Current smoker | 36 410 | (95.0) | 1900 | (5.0) |
| Missinga | 271 | 3 | ||
|
| ||||
| Total cholesterol, mmol/L | ||||
| <5 | 38 268 | (97.9) | 830 | (2.1) |
| 5.0–6.9 | 67 319 | (90.8) | 6816 | (9.2) |
| ≥7 | 8610 | (64.1) | 4823 | (35.9) |
| Missinga | 57 025 | 96 | ||
|
| ||||
| Systolic blood pressure, mmHg | ||||
| <140 | 105 320 | (97.0) | 3247 | (3.0) |
| 140–159 | 40 213 | (90.6) | 4163 | (9.4) |
| ≥160 | 19 926 | (79.5) | 5151 | (20.5) |
| Missinga | 5763 | 4 | ||
|
| ||||
| QRISK % 10-year risk | ||||
| <5 | 99 796 | (98.2) | 1826 | (1.8) |
| 5–9 | 41 436 | (92.0) | 3618 | (8.0) |
| 10–14 | 19 235 | (84.1) | 3629 | (15.9) |
| 15–19 | 10 755 | (75.5) | 3492 | (24.5) |
% calculated without missing values. IHD = ischaemic heart disease.
Statin prescription was particularly associated with antihypertensive medication, raised blood pressure, and high cholesterol. Statins were prescribed to 23.5% of those on antihypertensive therapy versus 3.4% of those who were not; in 35.9% of those with a serum cholesterol ≥7 mmol/L versus 2.1% in those with serum cholesterol <5 mmol/L; and in 20.5% of those with a systolic blood pressure ≥160 mmHg versus 3.0% in those where it was <140 mmHg.
Table 3 shows the adjusted odds ratios (OR) for relevant variables that were significantly associated with statin prescription in patients <20% CVD risk. Statin prescription was more likely at older ages, in people of South Asian ethnicity, and in those with a positive family history of premature IHD, raised blood pressure, and treated hypertension (P<0.001). The highest OR (20.5) was associated with a cholesterol of ≥7 mmol/L, age 65–74 years (OR 7.6) and antihypertensive therapy (OR 5.0). Female sex (OR 0.76) and black African/Caribbean ethnic group (OR 0.81) were associated with significantly lower statin prescription (P<0.001). The association with deprivation was not significant.
Table 3.
Characteristics associated with statin prescribing to people with QRISK® <20%
| Characteristic | Odds ratioa | 95% CI |
|---|---|---|
| Female | 0.76 | 0.71 to 0.81 |
|
| ||
| Age, years | ||
| 45–54 | 1.96 | 1.80 to 2.14 |
| 55–64 | 3.88 | 3.53 to 4.27 |
| 65–74 | 7.62 | 6.71 to 8.65 |
|
| ||
| Ethnic group | ||
| South Asian | 2.40 | 2.10 to 2.74 |
| Black African/Caribbean | 0.81 | 0.74 to 0.88 |
|
| ||
| Family history of premature ischaemic heart disease | 1.30 | 1.21 to 1.39 |
|
| ||
| Antihypertensive treatment | 5.00 | 4.64 to 5.38 |
|
| ||
| Current smoker | 1.08 | 1.01 to 1.16 |
|
| ||
| Total cholesterol, mmol/l | ||
| 5–6.9 | 3.49 | 3.04 to 4.01 |
| ≥7 | 20. 52 | 17.95 to 23.46 |
|
| ||
| Systolic blood pressure, mmHg | ||
| 140–159 | 1.42 | 1.34 to 1.51 |
| ≥160 | 1.41 | 1.32 to 1.52 |
All reported odds ratios were significant P < 0.001 except smoking P < 0.05.
DISCUSSION
Summary
This study confirms the finding of previously published studies which show that at least half the statins for primary prevention in the UK are prescribed to patients whose risk falls below the 20% CVD risk threshold,4,5 most of which represents appropriate targeting of CVD risk according to the most recent 2014 NICE guidance.1
Of those individuals whose CVD risk was not recorded, only 0.8% were prescribed statins. Statin prescription in those with a CVD risk of <10% represented 24.3% of total statin prescriptions; in other words 75.6% of statin prescribing was within currently recommended limits ≥10% CVD risk. Like Wu et al, the authors of this study found that statin prescription below the 20% CVD risk is associated with several individual risk factors, including factors recommended by NICE guidance such as high cholesterol with a positive family history of premature IHD and hypertension.9
Strengths and limitations
As this study is more recent and covers CCGs with a better than average implementation of the NHS Health Check programme, it has resulted in high levels of statin prescribing. In those with CVD risk recorded, risk factor recording was complete in all but three individuals for smoking status, in 96.9% for blood pressure, and in 68.9% for serum cholesterol, for whom missing values were imputed. Family history assumed missing values were negative. However, like the Wu et al 4 and van Staa et al 5 studies, the current study has limited data on CVD risk for those not on statins and 40% of the eligible population aged ≥30 years did not have CVD risk estimated. This means that it was not possible to provide a detailed analysis of those eligible patients who do not use statins because of the uncertainty of their risk profile and eligibility. Differences in methods of assessing CVD risk estimation and eligible populations should also be taken into account in direct comparisons of data. The localities in the current study have higher than average uptake of NHS Health Checks illustrating that even here, statin use at highest CVD risk of ≥20% is far from optimal.
Treatment thresholds are intended to guide, not replace clinical judgement, and individual risk estimation has substantial spread below any given threshold. Current tools for CVD estimation are relatively crude at an individual level10,11 and may underestimate risk associated with extreme obesity, prediabetic states, chronic kidney disease, or other aspects such as heavy alcohol consumption or very sedentary lifestyles, which were not included in these studies.12 For primary prevention in individuals at highest risk of CVD (≥20%), 32 out of 33 will not gain from statin treatment in the next 5 years, with rapidly increasing margins of uncertainty below this level.13
Comparison with existing literature
Statin prescribing was better targeted in this 2014 study than in the two studies up to 7 years earlier. Statin prescription in patients at highest CVD risk in east London (49.7%) was higher than the 30.4% or 28.5% recorded by van Staa et al and Wu et al respectively, and the 6.8% prescription of statins to those at <20% CVD risk in the east London study, is less than the 10.1% recorded by Wu et al. Van Staa et al reported that statins were prescribed to 18.2% of those with a CVD risk of 10–19%, and to 3.5% of those with a <10% CVD risk; this is very similar to statin prescription in the current study, where the figures are 19.2% and 3.7% respectively.4,5
As in previous studies, statin prescription to patients at <20% risk in the current study was mainly directed towards those who were:
in the 10–19% CVD risk band;
older;
from South Asian ethnic groups; or
on antihypertensive treatment or with raised blood pressure, raised serum cholesterol, or a positive family history of premature IHD.
Lower rates of prescription of statins in black African/Caribbean patients has been reported in previous studies in secondary prevention.14
The current study shows that, statin prescribing below the 20% CVD threshold is targeted towards individuals in the 10–19% risk band who have associated CVD risk factors, particularly high cholesterol, (35.9%) and those on antihypertensive treatment (23.5%). Mandating lower treatment thresholds to 10% would require GPs to achieve a huge increase in workload. At present GPs are reaching fewer than one-half of the 8% of the population at ≥20% risk. Adding a further 18% of the population at 10–19% risk would more than treble this.
Implications for research and practice
Data from the current and national studies confirm that in those at lower CVD risk, GPs currently prescribe statins largely in accordance with current NICE guidance, although only a minority of those individuals are potentially eligible. It would be preferable if treatment at the 10% CVD risk level was considered a permissive rather than a mandatory requirement of programmes.1 This preference is not due to a lack of robust, cost-effective evidence of benefit at the 10% threshold or even the US recommended 5.0–7.5% threshold.15 The authors’ concern is threefold:
It is neither feasible nor politically desirable to medicalise 30–50% of the adult population while there are already very effective and feasible ways of preventing CVD in the first place.
The 20% risk threshold already means that in practice, half of those treated with statins are ‘scattered’ below this level. If a 10% CVD risk level is mandated it will result in many more individuals being treated below the 10% level, where the ratio of benefit to harm from treatment and cost effectiveness are open to some doubt.
Trying to treat three times as many patients does not make sense when currently only half at highest risk are identified and of these, only one-third are treated (that is, only 15% of those at highest risk are currently treated). Meanwhile, patients aged ≥75 years, almost all of whom have CVD risk >20%, continue to be largely ignored and are not included as part of the NHS Health Check programme. This study makes it clear that GPs are already treating a minority of patients in the 10–19% CVD risk band and the new NICE guidance, which is permissive rather than mandatory, supports this pragmatic approach, recognising the need for case-by-case assessment of estimated CVD risk, known risk factors, and patient preference.
US guidance confirms that there is trial evidence for CVD benefit from statins available down to a 5% CVD risk threshold,3 but this would involve around 50% of the UK population aged >40 years in treatment programmes. At the proposed NICE 10% CVD threshold, this would be 25–30% of the population. The NHS Health Check programme identifying those at 20% risk already targets 10% of the adult population aged 40–74 years for treatment with statins and nationally the programme is treating less than one-third of these. A previous attempt in 2004 for pharmacists to directly treat patients at a 10% CVD risk threshold failed because this was not a feasible method of delivery for large population groups.16
There is robust evidence that legislative control of dietary sugars, fats, salt, smoking, alcohol, and air pollution and improvements in the built environment to promote physical activity would have far greater impact and equity than a poorly delivered programme of statins and antihypertensives targeting patients below 20% CVD risk.17 Clinicians are already prescribing statins to some patients below the 20% threshold. But exercising informed clinical judgement is very different from mandating a treatment programme down to the 10% level.
This study considered patients in the 30–74 years age band to enable comparison with previous studies. NICE guidance recommends statin treatment in individuals aged ≥75 years as there is robust evidence that statins are highly effective in reducing CVD events in this age group.1 If statin prescription is to be systematically extended, it would be better targeted at those aged ≥75 years who are almost universally at ≥20% CVD risk, for whom it would be a feasible and highly cost-effective programme with evidence of benefit from both statin and antihypertensive treatment to 85 years, with no reason to suppose these benefits are not applicable to many of those even older.15,18
In east London in 2013–2014, statins were prescribed to 50% of patients identified as being at highest risk of CVD compared with 30% in earlier national studies. For those below this CVD risk level, statin prescription was on a similar scale to that in previous studies and largely directed to individuals with CVD risk >10%, older ages, on antihypertensive treatment, or with other increased risk factors for CVD. The problem is not so much overtreatment at lower risk levels, as undertreatment for those at highest risk.
Nationally, less than one-third of those identified as being at highest risk of CVD are treated and a systematic programme enfranchising those aged ≥75 years is not available. Improvement of current programmes targeting statin use at over 20% CVD risk and inclusion of patients aged ≥75 years in the NHS Health Check programme would yield greater and more feasible gains from the limited resources currently available in primary care than extending treatment at lower risk.
Acknowledgments
GPs and their staff were responsible for entering the data on study subjects and Keith Prescott, Manager of the Clinical Effectiveness Group and staff of this organisation supported this process by providing standard data-entry templates and support for web-based data extraction.
Funding
This research received no specific funding. The salaries of the principle investigator and other authors who contributed to this study were funded by Newham, City and Hackney, and Tower Hamlets Clinical Commissioning Groups.
Ethical approval
All data were anonymised and managed according to the UK NHS information governance requirements. Ethical approval was not required for the use of anonymised data in this observational study.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
John Robson was Chair of the 2008 NICE guideline on lipid modification (CG67) that recommended a 20% CVD risk threshold for statin treatment. John Robson was also a co-author of QRISK®. John Robson and Isabel Dostal are also evaluating the NHS Health Check programmes supported by a National Institute for Health Research grant. John Robson, Kambiz Boomla and Sally Hull have promoted the implementation of the NHS Health Check programme in east London.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.National Institute for Health and Care Excellence . Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. London: NICE; 2014. Clinical Guideline 181. https://www.nice.org.uk/guidance/CG181 (accessed 23 Jun 2015). [PubMed] [Google Scholar]
- 2.D’Agostino RB, Sr, Ansell BJ, Mora S, Krumholz HM. Clinical decisions. The guidelines battle on starting statins. N Engl J Med. 2014;370(17):1652–1658. doi: 10.1056/NEJMclde1314766. [DOI] [PubMed] [Google Scholar]
- 3.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1–45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 4.Wu J, Zhu S, Yao GL, et al. Patient factors influencing the prescribing of lipid lowering drugs for primary prevention of cardiovascular disease in UK general practice: a national retrospective cohort study. PLoS One. 2013;8(7):e67611. doi: 10.1371/journal.pone.0067611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Staa TP, Smeeth L, Ng ES, et al. The efficiency of cardiovascular risk assessment: do the right patients get statin treatment? Heart. 2013;99(21):1547–1548. doi: 10.1136/heartjnl-2013-303698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Department of Health . Putting prevention first: NHS Health Check: vascular risk assessment and management. Best practice guidance. London: Department of Health; 2009. [Google Scholar]
- 7.NHS England NHS Health Checks data 2011–13. http://www.england.nhs.uk/statistics/integrated-performance-measures-monitoring/nhs-health-checks-data/ (accessed 23 Jun 2015).
- 8.Robson J, Hull S, Mathur R, Boomla K. Improving cardiovascular disease using managed networks in general practice: an observational study in inner London. Br J Gen Pract. 2014 doi: 10.3399/bjgp14X679697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence . Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. London: NICE; 2008. Clinical Guideline 67. http://www.nice.org.uk/guidance/cg67 (accessed 23 Jun 2015). [PubMed] [Google Scholar]
- 10.Ridker PM, Cook NR. Refining the American guidelines for prevention of cardiovascular disease — Authors’ reply. Lancet. 2014;383(9917):600. doi: 10.1016/S0140-6736(14)60216-6. [DOI] [PubMed] [Google Scholar]
- 11.Jackson R, Marshall R, Kerr A, et al. QRISK or Framingham for predicting cardiovascular risk? BMJ. 2009;339:b2673. doi: 10.1136/bmj.b2673. [DOI] [PubMed] [Google Scholar]
- 12.Anand SS, Islam S, Rosengren A, et al. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study. Eur Heart J. 2008;29(7):932–940. doi: 10.1093/eurheartj/ehn018. [DOI] [PubMed] [Google Scholar]
- 13.Bandolier Statins. http://www.medicine.ox.ac.uk/bandolier/band47/b47-2.html. (accessed 1 Jul 2015).
- 14.Mathur R, Hull SA, Badrick E, Robson J. Cardiovascular multimorbidity: the effect of ethnicity on prevalence and risk factor management. Br J Gen Pract. 2011 doi: 10.3399/bjgp11X572454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cholesterol Treatment Trialists’ (CTT) Collaborators. Mihaylova B, Emberson J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581–590. doi: 10.1016/S0140-6736(12)60367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MHRA The reclassification of simvastatin 10mg (zocor heart-pro) over the counter (OTC) http://www.mhra.gov.uk/home/groups/pl-a/documents/websiteresources/con1004224.pdf (accessed 23 Jun 2015).
- 17.National Institute for Health and Care Excellence . Prevention of cardiovascular disease. London: NICE; 2010. Public Health Guidance 25. http://www.nice.org.uk/guidance/ph25 (accessed 23 Jun 2015). [Google Scholar]
- 18.Czernichow S, Zanchetti A, Turnbull F, et al. The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials. J Hypertens. 2011;29(1):4–16. doi: 10.1097/HJH.0b013e32834000be. [DOI] [PubMed] [Google Scholar]