Abstract
Background
Patient–doctor continuity is valued by both parties, yet the effect of the depth of the patient–doctor relationship on the content of consultations in general practice is unknown.
Aim
To assess whether differences in the depth of relationship between a patient and their GP affects the length of consultations, and the number and type of problems and issues raised during a consultation.
Design and setting
Cross-sectional study in 22 GP practices in the UK.
Method
GP consultations (n = 229) were videotaped and the number of problems and aspects of those problems and issues identified. Patients completed the Patient–Doctor Depth of Relationship (PDDR) and General Practice Assessment Questionnaire-communication (GPAQc) scales. Associations were explored using multivariable linear and logistic regression.
Results
Complete data were available on 190 participants consulting 30 GPs. In unadjusted analysis, patients with a deep relationship with their GP discussed more problems (mean 2.8) and issues (mean 4.7) compared with those with a moderate (2.4 problems; 4.0 issues) or shallow (2.3 problems; 3.8 issues) relationship. Patients with deep relationships had consultations that were on average 118 seconds (95% CI = 1 to 236) longer than those with shallow relationships. Adjustment for participant and GP factors attenuated these relationships, although the main trends persisted.
Conclusion
A greater number of problems and issues may be raised in a consultation when patients have a deeper relationship with their GP. Over several clinical encounters each year, this may be associated with significant benefits to patients and efficiencies in GP consultations and warrants further investigation.
Keywords: consultation, continuity of care, doctor-patient relations, general practice
INTRODUCTION
The interaction between a patient and their GP is an important element of the therapeutic relationship. From the patient’s perspective, the key elements of the patient–doctor relationship include the doctor’s knowledge of the patient and their background, their trust in the doctor and their abilities, the patient’s feelings of loyalty towards the doctor, and the regard which the patient has for the doctor.1 Continuity of care between a patient and their GP is generally valued by both parties1–4 and this may promote the key positive elements of this relationship.5
A number of studies have assessed the effect of the patient–doctor relationship on various outcomes, using different measures. Relational continuity of care has been shown to improve outcomes for older patients,6–8 those with diabetes,9,10 and patients with heart failure.11,12 Continuity of care has also been shown to have a variable impact on patient satisfaction.1,2 A better patient–doctor relationship has also been suggested to reduce avoidable admissions,13 healthcare costs,14 and duplication of medications.15
A review by Eveleigh et al in 2012 found 19 different instruments used to measure the patient–doctor relationship.6 These measures often assess the longitudinal element of the relationship by determining how long a patient has been seeing a particular GP, and how often. The number or proportion of encounters with the same doctor says little, however, about the quality of the relationship, so-called relational continuity.1,16 Ridd and colleagues developed and validated a conceptually-based and psychometrically robust measure, called the Patient–Doctor Depth of Relationship (PDDR) scale: an easy to complete, 8-item questionnaire that captures patients’ perceptions of their relationship with their GP.5
The effect of the patient–doctor relationship on GP consultations has not been studied. In 2013, Salisbury et al reported on a cross-sectional study that described the content of GP consultations.17 Building on this original piece of research, this study aimed to assess whether differences in the depth of relationship between a patient and their GP, as measured by the PDDR scale, are related to the number of problems and issues raised during a consultation, and the length of these consultations. The effect of depth of relationship on the types of problems and issues raised during consultations was also examined.
METHOD
Data collection
This research was performed using data collected from a recent original cross-sectional study of routine GP consultations by Salisbury et al, full details of the setting, selection, and recruitment of GPs and patients, and assessment of the content of GP consultations have been described previously.17 In brief, the researchers purposefully selected practices and GPs, seeking to recruit a representative sample in terms of deprivation (based on practice postcodes mapped to the Index of Multiple Deprivation),18 and GP characteristics such as age, sex, and years since qualification. Patients had to be aged ≥18 years and have a pre-booked appointment to be eligible. A proforma was developed to analyse the content of consultations, as described elsewhere.19 An initial validation of the assessment method conducted by two independent researchers in the first 60 consultations demonstrated acceptable levels of inter-rater reliability, with intraclass correlation coefficients for inter-rater reliability for number of problems, agreement about International Classification of Primary Care (ICPC) coding and issue types of 0.93, 0.85, and 0.80, respectively.17 The remaining consultations were coded by one researcher.
How this fits in
Previous research has shown that GPs deal with an average of 2.5 problems per consultation with a patient. The effect of relational continuity on duration and content of GP consultations has not been previously investigated. This study found that more issues may be raised in GP consultations in which a patient perceives a deep-relationship with their GP. Depth of the patient–doctor relationship was also associated with more discussion of emotional and psychological issues and less discussion of preventive behaviours.
The proforma recorded the numbers of ‘problems’ and ‘issues’ that were raised in each consultation, and whether these were raised by the GP or the patient. A ‘problem’ was defined as a topic requiring the GP to make a decision or diagnosis, to provide treatment, or to undertake monitoring or administration. Within each ‘problem’, one or more ‘issues’ were then discussed in the consultation.17 These were different aspects of the problem. For example, a patient with diabetes (the ‘problem’), may consult their GP regarding their blood sugar levels and medications, and the GP may take the opportunity to discuss health behaviours to prevent diabetic complications (covering three ‘issues’: physical, medications, and behaviours). Problems were classified using the second version of the ICPC system.20 Specific sample size calculations for the aims of this particular study were not undertaken as this was a secondary analysis of data from a previous project.
In addition to giving consent to the videotaping of their consultation, participants also completed a questionnaire afterwards comprising the PDDR scale (0–32)5 and the communication section of the General Practice Assessment Questionnaire (GPAQc).21 Based on PDDR scores, participants were divided by the 33rd and 67th percentile scores into those with a deep relationship (PDDR = 32), a moderate relationship (PDDR 25–31) or a shallow relationship (PDDR<25). This is a different method from the original validation study by Ridd et al (which dichotomised patients into a deep or shallow relationship around a cut-point of 31/32)5 and was done to enable more discrimination in the analysis of depth of relationship between patient and their GP.
Statistical methods
Student t and χ2 tests were used to compare the key characteristics of the included and excluded participants, and to compare the incidence of ICPC problem types between the included participants based on the depth of relationship. Two-level (patients nested within GPs) multivariable linear regression analyses explored the relationship between depth of relationship as the explanatory variable (three levels distinguished by two dummy covariates) and consultation characteristics as the outcome measure (length, number of problems, number of issues, each in turn), adjusting for participant age and sex, and area deprivation. The unit of analysis for these regression models was the patient, one consultation having been recorded per patient. Multivariable, three-level (problem/issue nested within patient nested within GP) logistic regression modelling was used to investigate the relationship between the depth of relationship (as the explanatory variable, included as two dummy covariates as in the previous models), and the types of problems and issues raised in a consultation (as the outcome measure, an unordered categorical variable).
The unit of analysis for these models was the problem or issue. Models were adjusted for any confounding by participant age and sex, the GP’s age, sex, and years worked at the practice, and the deprivation area of the practice. Random effects were assumed to have a normal distribution. In sensitivity analyses, confidence intervals were calculated using the percentile bootstrap technique to ensure that skewed dependent variables were not causing spurious results. All analyses were done using Stata (version 13).
RESULTS
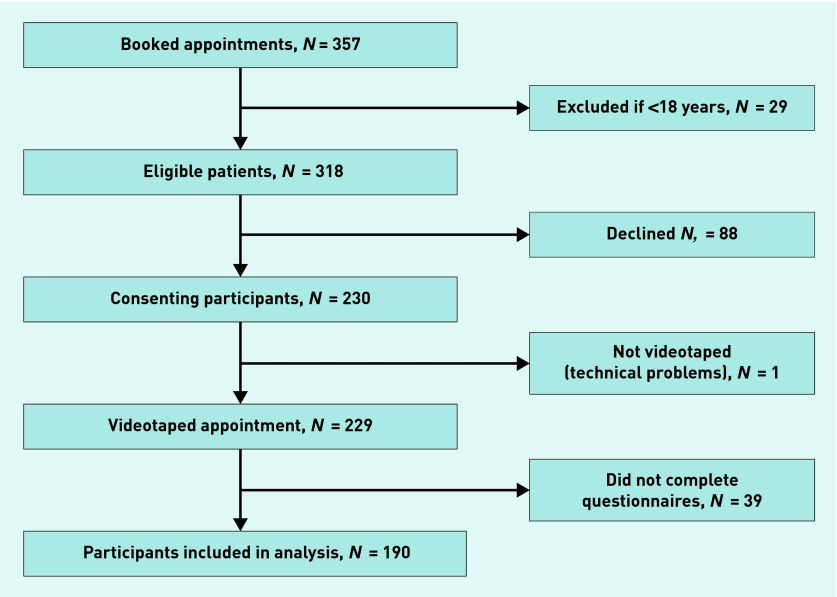
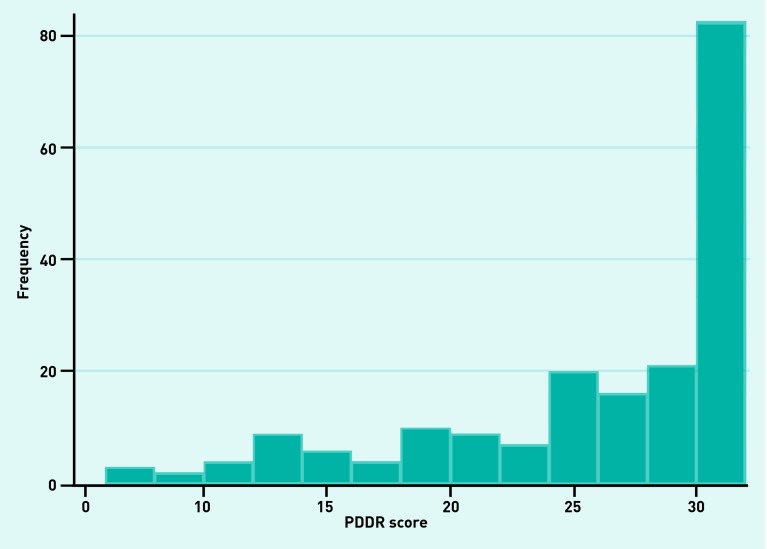
The flow of participants into this study is shown in Figure 1. Videotapes and questionnaire data were complete for 190 of the 229 (82.9%) participants from the original study. Compared with the included patients, those who did not complete questionnaires were older (P = 0.02), but there were no differences in sex, deprivation, ethnic group, or whether they were seeing their usual GP (Table 1). Most GPs with whom they consulted were >40 years of age (83.3%), and of white ethnic group (96.7%). There were no significant differences in the GPs’ sex or years working at the current practice (Table 1). Median PDDR score was 29 (SD 6.9; range 6–32) and the median GPAQc score was 97.5 (SD 14.0; range 0–100). The distribution of PDDR scores was negatively skewed (Figure 2), as were the GPAQc scores. PDDR scores were categorised into patients with deep (58, 30.2%), intermediate (66, 34.2%), or shallow (69, 35.6%) relationships. Most of the included patients (78.9%) stated that they were seeing their usual GP, and those seeing their usual GP were significantly more likely to report a deep relationship with the doctor (P<0.01).
Figure 1.
Patient selection flow diagram.
Table 1.
Differences in characteristics of participants and GPs
| Included participants | Excluded participantsa | P-value | |
|---|---|---|---|
| Patient characteristics | (n = 190) | (n = 17) | |
| Mean age, years (SD) | 56.0 (18.8) | 66.9 (15.8) | 0.02 |
|
| |||
| Female sex, n (%) | 108 (56.8) | 12 (70.6) | 0.27 |
|
| |||
| White ethnic group, n (%) | 182 (95.8) | 15 (88.2) | 0.16 |
|
| |||
| Usual GP, Yes, n (%) | 150 (78.9) | 13 (86.7) | 0.48 |
|
| |||
| Deprivation area of practice, n (%) | |||
| Deprived | 74 (38.9) | 7 (41.2) | |
| Moderate | 54 (28.5) | 5 (29.4) | 0.96 |
| Affluent | 62 (32.6) | 5 (29.4) | |
|
| |||
| GP characteristics (n = 30) | |||
| Age >40 years, n (%) | 25 (83.3) | ||
|
| |||
| Female sex, n (%) | 15 (50) | ||
|
| |||
| White ethnic group, n (%) | 29 (96.7) | ||
|
| |||
| Years worked at the GP practice, n (%) | |||
| <5 | 2 (6.7) | ||
| 5–14 | 8 (26.7) | ||
| 15–19 | 8 (26.7) | ||
| 20–24 | 3 (10) | ||
| 25–29 | 7 (23.2) | ||
| ≥30 | 2 (6.7) | ||
Demographic data missing for 22 out of 39 excluded patients.
Figure 2.
Distribution of Patient–Doctor Depth of Relationship scale (PDDR).
Overall, the median recorded consultation length was 678.5 seconds (11.3 minutes, [SD 331.9 seconds]) long, with a range of 174 (2.9 minutes) to 1829 (30.5 minutes) seconds. A mean of 2.5 problems (SD 1.3) and 4.1 issues (SD 2.0) were discussed per consultation.
In the unadjusted analysis (Table 2), compared with patients reporting a shallow relationship, patients with deep and moderate relationships reported more problems (mean deep 2.8, moderate 2.4, and shallow 2.3) and issues (mean deep 4.7, moderate 3.9, and shallow 3.7). There was also some evidence of patients with a deep relationship having longer consultations compared with those reporting shallow relationships (mean difference 118 seconds, 95% CI = 1 to 236 seconds). After adjusting for potential confounding variables (Table 2), these trends persisted, but their strength was attenuated and they were consistent with chance.
Table 2.
Regression analysis of difference in means of consultation characteristics between PDDR groups, controlling for GP clustering
| Relationship | Crude difference in means (95% CI) | P-value | Adjusted for age of participants (95% CI) | P-value | Adjusted for participant factors (95% CI)a | P-value | Adjusted for GP factors (95% CI)b | P-value | Adjusted for all confounders (95% CI)c | P-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Consult length, seconds | |||||||||||
| Shallow | Reference | Reference | Reference | Reference | Reference | ||||||
|
| |||||||||||
| Moderate | 24 (−89 to 136) | 0.05 | −4 (−107 to 100) | 0.49 | −4 (−108 to 100) | 0.51 | 4 (−101,109) | 0.15 | −15 (−119 to 90) | 0.54 | |
|
| |||||||||||
| Deep | 118 (1 to 236) | 58 (−57 to 173) | 57 (−59 to 172) | 99 (−14 to 211) | 46 (−70 to 161) | ||||||
|
| |||||||||||
| Number of problems | |||||||||||
| Shallow | Reference | Reference | Reference | Reference | Reference | ||||||
|
| |||||||||||
| Moderate | 0.2 (−0.3 to 0.6) | 0.02 | 0.1 (−0.3 to 0.5) | 0.34 | 0.1 (−0.3 to 0.5) | 0.36 | 0.2 (−0.3 to 0.6) | 0.06 | 0.1 (−0.3 to 0.5) | 0.48 | |
|
| |||||||||||
| Deep | 0.5 (0.1 to 0.8) | 0.3 (−0.1 to 0.8) | 0.3 (−0.1 to 0.8) | 0.5 (0.1 to 1) | 0.3 (−0.2 to 0.8) | ||||||
|
| |||||||||||
| Number of issues | |||||||||||
| Shallow | Reference | Reference | Reference | Reference | Reference | ||||||
|
| |||||||||||
| Moderate | 0.2 (−0.5 to 0.8) | 0.01 | 0.1 (−0.5 to 0.8) | 0.14 | 0.1 (−0.5 to 0.8) | 0.14 | 0.2 (−0.5 to 0.9) | 0.02 | 0.1 (−0.6 to 0.7) | 0.22 | |
|
| |||||||||||
| Deep | 1 (0.2 to 1.7) | 0.7 (0 to 1.5) | 0.7 (0 to 1.5) | 0.9 (0.2 to 1.7) | 0.6 (−0.1 to 1.4) | ||||||
Adjusted for age and sex of participants, and deprivation area of practice.
Adjusted for GP’s age, sex of participants, and years worked at the practice.
Adjusted for age and sex of participants, deprivation area of practice, GP’s age, sex, and years worked at the practice. OR = odds ratio. PDDR = Patient–Doctor Depth of Relationship.
There was no significant difference (P<0.05) in the proportions of types of problems raised during consultations for different levels of depth of relationship (Table 3). In respect of types of issues (Table 4), however, there was weak evidence that psychological and/or emotional issues were more likely to be discussed for patients reporting a deep relationship (OR 1.8, 95% CI = 0.9 to 3.5) with their GP relative to those with a shallow relationship, while health prevention issues were less likely to be discussed (OR 0.4, 95% CI = 0.2 to 0.8).
Table 3.
Frequency of International Classification of Primary Care (ICPC) problem type in recorded consultations
| ICPC Group | Overall | Shallow | Moderate | Deep | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| n | % | n | % | n | % | n | % | ||
| A | General and unspecified | 85 | 15.2 | 33 | 16.8 | 23 | 12.4 | 29 | 16.6 |
| B | Blood and immune mechanism | 8 | 1.4 | 5 | 2.6 | 0 | 0.0 | 3 | 1.7 |
| D | Digestive | 46 | 8.2 | 15 | 7.6 | 15 | 8.1 | 16 | 9.1 |
| F | Eye | 11 | 2.0 | 4 | 2.0 | 3 | 1.6 | 4 | 2.3 |
| H | Ear | 9 | 1.6 | 2 | 1.0 | 2 | 1.1 | 5 | 2.9 |
| K | Cardiovascular | 34 | 6.1 | 11 | 5.6 | 12 | 6.4 | 11 | 6.3 |
| L | Musculoskeletal | 107 | 19.2 | 37 | 18.8 | 42 | 22.6 | 28 | 16.0 |
| N | Neurological | 24 | 4.3 | 9 | 4.6 | 7 | 3.8 | 8 | 4.6 |
| P | Psychological | 42 | 7.5 | 15 | 7.6 | 13 | 7.0 | 14 | 8.0 |
| R | Respiratory | 42 | 7.5 | 21 | 10.7 | 12 | 6.5 | 9 | 5.1 |
| S | Skin | 45 | 8.1 | 17 | 8.6 | 14 | 7.5 | 14 | 8.0 |
| T | Endocrine/metabolic and nutritional | 35 | 6.3 | 9 | 4.6 | 19 | 10.2 | 7 | 4.0 |
| U | Urological | 19 | 3.4 | 6 | 3.1 | 8 | 4.3 | 5 | 2.9 |
| W | Pregnancy, childbearing, family planning | 16 | 2.9 | 6 | 3.1 | 6 | 3.2 | 4 | 2.3 |
| X | Female genital | 12 | 2.2 | 3 | 1.5 | 5 | 2.7 | 4 | 2.3 |
| Y | Male genital | 11 | 2.0 | 1 | 0.5 | 2 | 1.1 | 8 | 4.6 |
| Z | Social problems | 12 | 2.2 | 3 | 1.5 | 3 | 1.6 | 6 | 3.4 |
| Total | 558 | 197 | 186 | 175 | |||||
χ2 test for difference between shallow, moderate, and deep groups (32 degrees of freedom) = 26.75, P> 0.05.
Table 4.
Adjusted analysis of effect of depth of relationship on issue types
| Issue type | Relationship | ORa (95% CI) | P-value |
|---|---|---|---|
| Physical | Shallow | Reference | 0.82 |
| Moderate | 0.9 (0.6 to 1.3) | ||
| Deep | 1 (0.7 to 1.6) | ||
|
| |||
| Emotional/psychological | Shallow | Reference | 0.12 |
| Moderate | 1.4 (0.7 to 2.7) | ||
| Deep | 1.8 (0.9 to 3.5) | ||
|
| |||
| Social | Shallow | Reference | 0.40 |
| Moderate | 1.8 (1 to 3.1) | ||
| Deep | 1.3 (0.7 to 2.4) | ||
|
| |||
| Administrative | Shallow | Reference | 0.85 |
| Moderate | 1 (0.5 to 2.1) | ||
| Deep | 1.1 (0.5 to 2.4) | ||
|
| |||
| Medication related | Shallow | Reference | 0.33 |
| Moderate | 1 (0.7 to 1.5) | ||
| Deep | 0.8 (0.5 to 1.2) | ||
|
| |||
| Order/refer for tests | Shallow | Reference | 0.52 |
| Moderate | 1 (0.6 to 1.8) | ||
| Deep | 1.1 (0.7 to 2.1) | ||
|
| |||
| Discuss test results/treatment | Shallow | Reference | 0.89 |
| Moderate | 1 (0.6 to 1.6) | ||
| Deep | 1 (0.6 to 1.7) | ||
|
| |||
| Behavioural health prevention | Shallow | Reference | 0.16 |
| Moderate | 0.9 (0.6 to 1.4) | ||
| Deep | 0.7 (0.4 to 1.1) | ||
|
| |||
| Medicalised health prevention | Shallow | Reference | 0.01 |
| Moderate | 0.9 (0.5 to 1.6) | ||
| Deep | 0.4 (0.2 to 0.8) | ||
|
| |||
| Third party issues | Shallow | Reference | 0.29 |
| Moderate | 1.4 (0.5 to 4.2) | ||
| Deep | 1.8 (0.6 to 5.3) | ||
Adjusted for age and sex of participants and GPs, years the GP has worked at the practice, and deprivation area of practice. Controlled for GP clustering. OR = odds ratio.
DISCUSSION
Summary
This is the first study to explore the relationship between the depth of doctor–patient relationships and the content of GP consultations. Evidence was found that a deep relationship between a patient and their GP compared with a shallow relationship was associated with more problems and issues being raised in a consultation and with more discussion of psychological or emotional issues, but less discussion of health prevention issues. Evidence for these associations was weaker after adjustment for confounding factors.
Strengths and limitations
A strength of this study is the high patient participation rate and level of completion of the survey questionnaires. Aside from being older, participants who did not complete the questionnaires were not significantly different from those who did. Doctors who agree to take part in this type of research may be atypical, however. In addition, because data for this study were not collected for the purpose of exploring continuity–consultant content associations, the study may be subject to a type 2 error, that is, be underpowered to detect differences where they exist. A type 1 error could also have occurred because of the multiple statistical tests performed, especially when assessing associations with different problem and issue types, that is, the null hypothesis may have been falsely rejected because of a chance result. Given the cross-sectional nature of this study, the possibility of reverse causality (that is, patients with more problems raised and discussed by their GP feel they have a deeper relationship) cannot be excluded.
It is notable that most of the associations observed were maintained after adjustment for patient and GP factors, but they were attenuated and may have been a result of chance. This could reflect the limited power of the study, but also suggests some confounding between patient and GP characteristics and both depth of relationship and the content and duration of consultations.
The PDDR scale provides a validated measure of the patient’s perceptions of the strength of the relationship they have with their GP.5 This measure arguably gives a better indication of the patient–doctor relationship compared with longitudinal measures, as seeing the same doctor is not a guarantor of the quality of the relationship. Because of the negatively skewed distribution of PDDR scores, it was chosen to analyse outcomes in relation to shallow, moderate, and deep levels of patient–doctor relationship. Such skewed distributions have been observed in previous published studies5,22 and similarly skewed GPAQc scores were seen in this and other research.
The ethnic group of participants and GPs in this study was almost exclusively white. The patient population, and the sample that this study is based on, is not representative of the ethnic makeup of the population in the UK. The difficulties faced in the recruitment of black and minority ethnic (BME) participants into research is not a unique or new issue,23 but the effect of the depth of relationship between a BME patient and a GP on consultations cannot be confidently assessed from this study.
Comparison with existing literature
Multiple potential benefits to a deep, ongoing relationship between a patient and their GP have been identified in the literature.24 Many patients have a preference to see the GP of their choice, particularly older patients and patients with chronic medical or psychological conditions.3 Previous research has suggested that GPs who have a deep relationship with a patient should have a better understanding of their past medical history, personality, and preferences for treatment.25,26 This extra knowledge may allow them to consider more issues in a single consultation, providing better and more efficient primary medical care. It is perhaps not so surprising that psychological and/or emotional issues may be more likely to be raised and discussed in consultations between patients and GPs with a deeper relationship. A deeper patient–doctor relationship was associated with a lower probability of considering health prevention measures affecting the patient’s wellbeing. This could simply be a result of the cross-sectional nature of the study (that is, these issues have been discussed in a previous consultation), or it could represent some collusion between patients and doctors who know each other in avoiding potentially challenging discussions. In other studies, it has been shown that GPs are concerned about potentially detrimental effects for the patient–doctor relationship in giving lifestyle advice to patients they know well,27 and there are many barriers to the effective delivery of health promotion advice and lifestyle counselling.28,29 Patients report that a more personal relationship with their GP ‘created motivation and an obligation to change’, however, with the delivery of lifestyle counselling in primary care settings.30
Implications for research and practice
The present findings suggest that more issues may be discussed per consultation when the patient perceives that they have a deep relationship with their GP, potentially translating into more efficient consultations. Over the course of an average of 5.3 consultations per year31 (more for older and people with multiple problems who are most likely to seek and benefit from seeing the same doctor), this could translate into important efficiencies. The possibility of reverse causality needs to be explored, but, if substantiated in future studies, the difference between an unknown (shallow relationship) and well-known (deep relationship) doctor would mean an additional 2.6 problems and 5.3 issues being discussed each year. This could potentially translate into saving an additional consultation each year according to the mean of 2.5 problems per visit overall, albeit at the cost of possibly longer consultations for each visit. This warrants further research, given the rising demands for GP consultations,32 difficulties recruiting GPs in some areas, and the pressures on continuity of care from a trend towards more part-time, salaried GPs.33 Similarly, future research should seek to explore the balance of potential benefits and harms to be struck from possibly more patient-centred consulting, dealing with more of the types of problems and issues patients might want to discuss (psychological and emotional), at the expense of time spent on more doctor/public health-centric issues such as preventive behavioural and lifestyle counselling.
Acknowledgments
We thank all the reviewers of this article for their insightful comments.
Funding
No funding was received in the conduct of this particular study; however, the original piece of research was funded by the National Institute of Health Research (NIHR) School of Primary Care Research (reference number NIHR SPCR). The grant reference is NIHR SPCR62.
Ethical approval
The original piece of research had ethical approval from South West Central Bristol local research ethics committee (reference number 10/H0106/14).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Ridd M, Shaw A, Lewis G, Salisbury C. The patient–doctor relationship: a synthesis of the qualitative literature on patients’ perspectives. Br J Gen Pract. 2009 doi: 10.3399/bjgp09X420248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adler R, Vasiliadis A, Bickell N. The relationship between continuity and patient satisfaction: a systematic review. Fam Pract. 2010;27(2):171–178. doi: 10.1093/fampra/cmp099. [DOI] [PubMed] [Google Scholar]
- 3.Aboulghate A, Abel G, Elliott MN, et al. Do English patients want continuity of care, and do they receive it? Br J Gen Pract. 2012;62(601):567–575. doi: 10.3399/bjgp12X653624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delva D, Kerr JR, Schultz K. Continuity of care. Can Fam Physician. 2011;57:e915–921. [PMC free article] [PubMed] [Google Scholar]
- 5.Ridd MJ, Lewis G, Peters TJ, Salisbury C. Patient–Doctor Depth-of-Relationship Scale: development and validation. Ann Fam Med. 2011;9(6):538–545. doi: 10.1370/afm.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eveleigh RM, Muskens E, van Ravesteijn H, et al. An overview of 19 instruments assessing the doctor-patient relationship: different models or concepts are used. J Clin Epidemiol. 2012;65(1):10–15. doi: 10.1016/j.jclinepi.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 7.Wolinsky FD, Bentler SE, Liu L, et al. Continuity of care with a primary care physician and mortality in older adults. J Gerontol Series A. 2010;65A(4):421–428. doi: 10.1093/gerona/glp188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Worrall G, Knight J. Continuity of care is good for elderly people with diabetes. Can Fam Physician. 2011;57:e16–e20. [PMC free article] [PubMed] [Google Scholar]
- 9.Lin W, Huang I-C, Wang SL, et al. Continuity of diabetes care is associated with avoidable hospitalizations: evidence from Taiwan’s National Health Insurance scheme. Int J Qual Health Care. 2010;22(1):3–8. doi: 10.1093/intqhc/mzp059. [DOI] [PubMed] [Google Scholar]
- 10.Hong J-S, Kang H-C. Continuity of ambulatory care and health outcomes in adult patients with type 2 diabetes in Korea. Health Policy. 2013;109(2):158–165. doi: 10.1016/j.healthpol.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Uijen AA, Bischoff EWMA, Schellevis FG, et al. Continuity in different care modes and its relationship to quality of life: a randomised controlled trial in patients with COPD. Br J Gen Pract. 2012;62(599) doi: 10.3399/bjgp12X649115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McAlister FA, Youngson E, Bakal JA, et al. Impact of physician continuity on death or urgent readmission after discharge among patients with heart failure. CMAJ. 2013;185(14):E681–689. doi: 10.1503/cmaj.130048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng S-H, Chen C-C, Hou Y-F. Longitudinal examination of continuity of care and avoidable hospitalization. Arch Int Med. 2010;170(18):1671–1677. doi: 10.1001/archinternmed.2010.340. [DOI] [PubMed] [Google Scholar]
- 14.Chen C-C, Cheng S-H. Better continuity of care reduces costs for diabetic patients. Am J Managed Care. 2011;17(6):420–427. [PubMed] [Google Scholar]
- 15.Cheng S-H, Chen C-C. Effects of continuity of care on medication duplication among the elderly. Medical Care. 2013;52:149–156. doi: 10.1097/MLR.0000000000000042. [DOI] [PubMed] [Google Scholar]
- 16.Haggerty JL, Reid RJ, Freeman GK, et al. Continuity of care: a multidisciplinary review. BMJ. 2003;327:1219–1221. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salisbury C, Procter S, Stewart K, et al. The content of general practice consultations: cross-sectional study based on video recordings. Br J Gen Pract. 2013 doi: 10.3399/bjgp13X674431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.GOV.UK English indices of deprivation 2010. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed 7 Jul 2015).
- 19.Procter S, Stewart K, Reeves D, et al. Complex consultations in primary care: a tool for assessing the range of health problems and issues addressed in general practice consultations. BMC Fam Pract. 2014;15(1):105. doi: 10.1186/1471-2296-15-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Classification Committee of the World Organization of Family Doctors . ICPC-2: International Classification of Primary Care. Oxford: Oxford University Press; 1998. [Google Scholar]
- 21.University of Cambridge General Practice Assessment Questionnaire (GPAQ). http://www.phpc.cam.ac.uk/gpaq/ (accessed 11 Jun 2015).
- 22.Mead N, Bower P, Roland M. The General Practice Assessment Questionnaire (GPAQ) — development and psychometric characteristics. BMC Fam Pract. 2008;9(1):13. doi: 10.1186/1471-2296-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MacNeill V, Nwokoro C, Griffiths C, et al. Recruiting ethnic minority participants to a clinical trial: a qualitative study. BMJ Open. 2013;3(4) doi: 10.1136/bmjopen-2013-002750. e002750–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guthrie B, Saultz JW, Freeman GK, Haggerty JL. Continuity of care matters. BMJ. 2008;337:548–549. doi: 10.1136/bmj.a867. [DOI] [PubMed] [Google Scholar]
- 25.Ridd M, Shaw A, Salisbury C. Two sides of the coin — the value of personal continuity to GPs: a qualitative interview study. Fam Pract. 2006;23(4):461–468. doi: 10.1093/fampra/cml010. [DOI] [PubMed] [Google Scholar]
- 26.Hjortdahl P. Continuity of care: general practitioners’ knowledge about, and sense of responsibility towards their patients. Fam Pract. 1992;9(1):3–8. doi: 10.1093/fampra/9.1.3. [DOI] [PubMed] [Google Scholar]
- 27.Lawlor DA, Keen S, Neal RD. Can general practitioners influence the nation’s health through a population approach to provision of lifestyle advice? Br J Gen Pract. 2000;50:455–459. [PMC free article] [PubMed] [Google Scholar]
- 28.Geense WW, van de Glind IM, Visscher TLS, van Achterberg T. Barriers, facilitators and attitudes influencing health promotion activities in general practice: an explorative pilot study. BMC Fam Pract. 2013;14(20):1–10. doi: 10.1186/1471-2296-14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lambe B, Collins C. A qualitative study of lifestyle counselling in general practice in Ireland. Fam Pract. 2010;27(2):219–223. doi: 10.1093/fampra/cmp086. [DOI] [PubMed] [Google Scholar]
- 30.Walseth LT, Abildsnes E, Schei E. Patients’ experiences with lifestyle counselling in general practice: A qualitative study. Scand J Prim Health Care. 2011;29(2):99–103. doi: 10.3109/02813432.2011.553995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hippisley-Cox J, Fenty J, Heaps M. Trends in general practice consultation rates 1995 to 2006: analysis of QResearch database. Leeds: NHS Information Centre; 2007. [Google Scholar]
- 32.The King’s Fund Medical workforce. http://www.kingsfund.org.uk/time-to-think-differently/trends/professional-attitudes-and-workforce/medical-workforce (accessed 11 Jun 2015).
- 33.NHS Securing the future GP workforce — delivering the mandate on GP expansion: GP taskforce final report. http://hee.nhs.uk/wp-content/blogs.dir/321/files/2014/07/GP-Taskforce-report.pdf (accessed 13 Jul 2015).