Abstract
Background
Treatment of non-malignant portal vein thrombosis (PVT) in patients with cirrhosis has been neglected in the past because of the fear of bleeding complications when using anticoagulation and due to the technical difficulties associated with the implantation of the transjugular intrahepatic portosystemic shunt (TIPS). However, PVT has a negative impact on outcome and compromises liver transplantation, warranting treatment by using anticoagulation and TIPS.
Methods
This review considers studies on the treatment of PVT in cirrhosis published in the last 10 years. Unfortunately, many of these studies are limited by their retrospective design and a small sample size.
Results
Anticoagulation using low-molecular-weight heparin (LMWH) or vitamin K antagonists is effective in the treatment of patients with limited and recent PVT, resulting in a recanalization in up to 50% of the patients. TIPS (plus local measures) results in a recanalization of up to 100% and reduces the rebleeding rate considerably in patients with recent or chronic PVT.
Conclusion
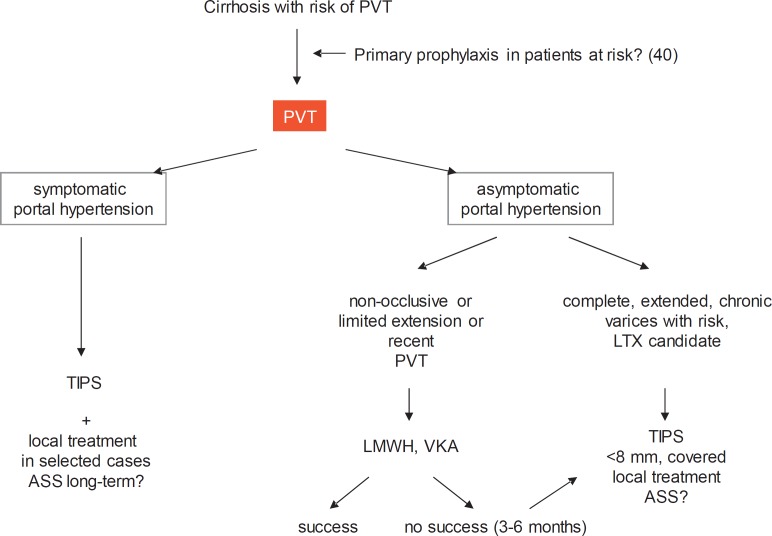
Based on the presently limited knowledge, a therapy algorithm is suggested favouring the TIPS as a first-line treatment for PVT in patients with symptomatic portal hypertension. Patients with thus far asymptomatic portal hypertension may first receive anticoagulation, preferably using LMWH. If these patients have a condition where anticoagulation is not promising (complete, extended, chronic PVT) or ineffective, or if they are candidates for liver transplantation, the TIPS may be implanted without delay.
Key Words: Portal vein thrombosis, Cirrhosis, Therapy, Algorithm, Anticoagulation, Transjugular shunt
Zusammenfassung
Hintergrund
Die nichtmaligne Pfortaderthrombose (PVT) beim Zirrhosepatienten galt bis vor wenigen Jahren als schicksalhafte Komplikation, deren spezifische Behandlung mittels Antikoagulation aus Sorge vor Blutungskomplikationen nicht durchgeführt wurde. Auch die Implantation eines transjugulären intrahepatischen portosystemischen Shunt (TIPS) galt lange Zeit aus technischen Gründen als kontraindiziert. Die Probleme, die durch den Pfortaderverschluss im Rahmen der Lebertransplantation auftraten, zwangen zum Umdenken und bewirkten die ersten Therapieversuche sowohl mit Antikoagulanzien als auch mit TIPS.
Methoden
Diese Übersichtsarbeit wertet Studien aus, die in den letzten 10 Jahren zu diesem Thema publiziert wurden. Bei den meisten Studien handelt es sich jedoch um retrospektive Auswertungen mit einer geringen Patientenzahl. Dies schränkt die Qualität der hieraus gewonnenen Empfehlung ein.
Ergebnisse
Die Antikoagulation mit niedermolekularem Heparin oder Vitamin-K-Antagonisten ist effektiv und resultiert in einer Rekanalisation bei bis zu 50% der Patienten. Die Effektivität ist abhängig vom Grad der Thrombose (partiell oder komplett), von ihrer Ausdehnung (begrenzt oder in die zuführenden Venen reichend) und von deren Alter (frisch oder chronisch). Die Anlage eines TIPS (eventuell zusammen mit lokalen Maßnahmen) kann in bis zu 100% zu einer Rekanalisation des Portalsystems führen. Bei chronischer oder kavernomatöser PVT kann ebenfalls eine TIPS-Anlage sinnvoll sein, da sie die Blutungsrate signifikant reduziert.
Schlussfolgerung
Auf der Grundlage der begrenzten Datenlage wird ein Therapiealgorithmus vorgestellt. Bei Patienten mit symptomatischer portaler Hypertension (insbesondere Varizenblutungen und Aszites) erscheint die frühe TIPS-Anlage empfehlenswert, da sie nicht nur die PVT, sondern auch die Symptome der portalen Hypertension bessert und zu einer Lebensverlängerung beitragen kann. Asymptomatische Patienten können mit einer Antikoagulation behandelt werden, wenn diese Erfolg versprechend erscheint (inkomplette und/oder begrenzte Thrombose, keine chronische PVT). Bei kompletter, ausgedehnter oder chronischer PVT, ungenügendem Ansprechen auf eine vorausgegangene Antikoagulation oder bevorstehender Lebertransplantation ist auch bei asymptomatischen Patienten an die Anlage eines dünnlumigen TIPS zu denken.
Introduction
The diagnosis of portal vein thrombosis (PVT) is increasingly made due to factors such as longer survival of cirrhotic patients, increased awareness, and improved sonographic skills and devices. Thus, PVT is now detected in up to 28% of cirrhotic patients, with a cumulative incidence of 12.8, 20, and 38.7% at 1, 5, and 8-10 years of follow-up, respectively [1]. Due to extensive collateralization before the development of the PVT, many patients are asymptomatic with respect to mesenteric ischaemia but may have an exacerbation of symptoms related to portal hypertension. In contrast to non-cirrhotic PVT where coagulation or haematologic disorders play the dominant role, a causative hypercoagulative state is rather an exception in cirrhotic patients developing PVT [2,3,4]. Instead, haemodynamic factors, i.e. decelerated blood flow, are of major importance [5]. PVT in cirrhosis has a negative effect on outcome and transplantation [5], a fact which underlines the importance of a treatment algorithm.
Treatment of PVT in Cirrhosis
Anticoagulation
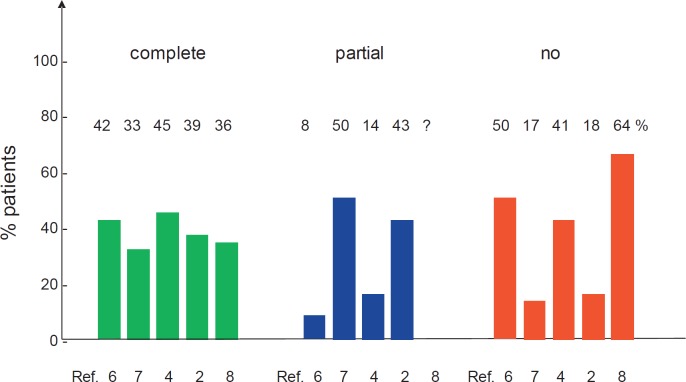
Four retrospective studies [2,4,6,7] and one prospective study [8] evaluated the effect of anticoagulation on PVT in cirrhosis (table 1) by including 176 patients receiving anticoagulation. In two of these studies, control groups not receiving anticoagulation were compared [6,8]. The proportion of patients with partial, occlusive, extensive, or cavernomatous thrombosis varied between studies. Two studies included a small proportion of patients with cavernomatous transformation of the portal vein [7,8]. Considering thrombus resolution, complete recanalization was found in 33-45% and partial recanalization in 8-50% (fig. 1). 10% of the patients receiving anticoagulation showed thrombus extension [6,7,]allowing a TIPS (transjugular intrahepatic portosystemic shunt) intervention. The effects of anticoagulation with low-molecular-weight heparin (LMWH) followed by warfarin (vitamin K antagonists (VKA)), with VKA alone, or LMWH alone were similar. In one study using LMWH, no serious side-effects were observed, particularly no bleedings [7]. In another study, however, which used LMWH or VKA, side-effects consisted of bleedings in 20% of the patients, with variceal bleedings in 9%, new onset or worsening of ascites in 15%, and hepatic encephalopathy (HE) in 9% [4]. The effect of anticoagulation correlated negatively with a delayed initiation of treatment (thrombus age) and an extension of the thrombus [4].
Table 1.
Summary of thrombosis grade of recent studies using anticoagulation for the treatment of PVT
| n | Design | Drug | Occlusion/extensiona, partial/complete/extended, % of patients | Cavernoma, % of patients | |
|---|---|---|---|---|---|
| Francoz et al., 2005 [6] | 19/10b | prospective | LMWH > VKA | 58/42/0 | 0 |
| Amitrano et al., 2010 [7] | 39 | retrospective | LMWH | 64.1/15.4/n.g. | 20.5 |
| Delgado et al., 2012 [4] | 55 | retrospective | LMWH > VKA | 75/25/55 | excluded |
| Werner et al., 2013 [2] | 28 | retrospective | VKA | n.g./71/22 | 0 |
| Senzolo et al., 2012 [8] | 35/21b | prospective | LMWH | 32/31/37 | 11 |
Partial occlusion = incomplete trunk or intrahepatic branches; extended = thrombosis extends into splenic or mesenteric veins.
Control group without anticoagulation.
LMWH > VKA = Low-molecular-weight heparin followed by vitamin K antagonist; n.g. = no information given.
Fig. 1.
Percentages of patients with complete, partial, and no recanalization on anticoagulation therapy [2,4,6,7,8]. Complete resolution of PVT was seen in 30-40% of patients.
The choice of the anticoagulant and the duration of the treatment are still under debate. In the study with a variceal bleeding rate of 9%[,] no significant correlation was found between bleeding and one of the drugs given (LMWH, VKA) [4]. One study using LMWH reports that this treatment was safe in cirrhotic patients [9]. Subcutaneous administration of LMWH, however, may lead to incompliance due to which a switch to VKA may be necessary in many patients on long-term anticoagulation. Since 38.5% of the patients develop rethrombosis after withdrawal [4], anticoagulation may be required for a longer period or even lifelong [10].
TIPS
In contrast to anticoagulation, TIPS is a treatment which corrects the pathophysiology of PVT formation by increasing the portal vein flow velocity from 0-20 to 40-60 cm/s and the portal flow from less than 1 l/min to about 2 l/min [11,12]. In addition, it may not affect HE and liver function because portal perfusion is already diminished or abolished before TIPS and compensated by an increased arterial perfusion, a mechanism which is called the ‘hepatic arterial buffer response’ [13]. This effect has also been demonstrated in patients with stagnant or reversed portal perfusion receiving TIPS who comparably had a very low rate of post-TIPS HE (9 vs. 25% in patients with prograde flow) and deterioration in liver function [14,15].
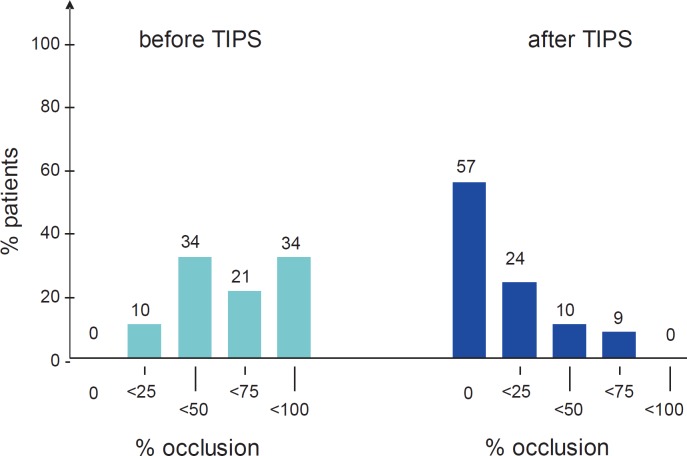
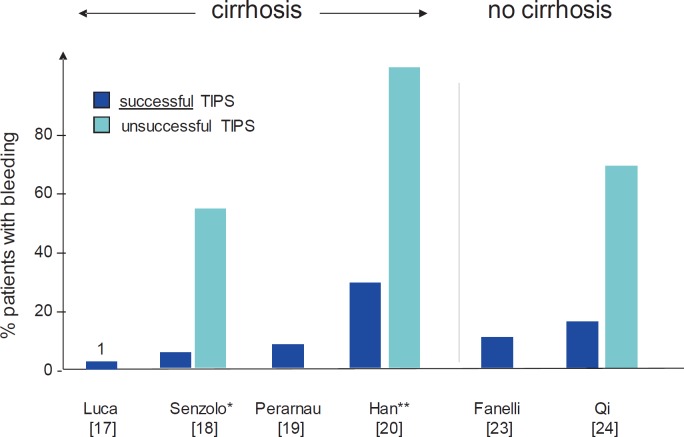
Recent studies with TIPS for PVT are summarized in table 2. TIPS is highly effective in the prevention [16] and treatment of PVT [16,17,18,19,20,21,22,] resulting in a recanalization between 67 and 100% depending on the proportion of patients with cavernoma. The largest study including 70 consecutive patients with PVT in cirrhosis found an overall response of 87% with almost complete (>75%) or complete recanalization in 81% (fig. 2). In this study, no anticoagulation was given before or after TIPS. As shown in figure 3, the rebleeding rates given in four of the studies were very low after successful TIPS and significantly higher when compared to patients with unsuccessful intervention [18,20]. In comparison, patients with non-cirrhotic PVT had a similar benefit with respect to variceal bleeding [23,24].
Table 2.
Recent retrospective studies on TIPS for PVT in cirrhosis
| n | Study period, years | Grade of occlusion/extensiona, partial/complete/extended, % of patients | Cavernoma, % of patients | |
|---|---|---|---|---|
| Luca et al., 2011 [17] | 70 | 2003–2010 | 66/34/78 | 0 |
| Senzolo et al., 2006 [18]b | 28b | 1994–2005 | 18/14/18 | 32 |
| Perarnau et al., 2010 [19] | 128 | 1990–2004 | 73/27/? | 12 |
| Han et al., 2011 [20] | 57 | 2001–2008 | 61/39/75 | 53 |
| D'Avola et al., 2012 [16] | 15 | 1995–2009 | 15/0/0 | 0 |
| Bauer et al., 2006 [21] | 9 | 1999–2005 | 22/78/100 | 44 |
Partial = <75% luminal occlusion; complete = >75% luminal occlusion.
12/28 patients with non-cirrhotic PVT.
Fig. 2.
Results of a recent study on TIPS for PVT [17] including 70 patients. Severe thrombosis (>50% occlusion) was seen in 55% of the patients before TIPS compared to 9% after TIPS. In 57% of the patients thrombosis resolved completely.
Fig. 3.
Percentages of patients with variceal bleeding after successful (dark blue) versus unsuccessful (light blue) TIPS implantation in patients with chronic PVT with cirrhosis. The study by Senzolo et al. [18] included cirrhotic and non-cirrhotic PVT. Patients without successful TIPS implantation had significantly higher bleeding rates. For comparison, two studies in patients with cavernomatous PVT without cirrhosis are also given [23,24]. *Mean follow-up: 18.1 months; **5-year bleeding rates.
Side-effects of the TIPS intervention were rare and consisted of one technical death [20] and the development of HE in 4-30% of the patients [18,19,20]. The response to TIPS was associated with the age and extension of the thrombus, the presence of varices [17,] and the degree of thrombosis in the portal trunk [20].
Technical Aspects of the TIPS Intervention
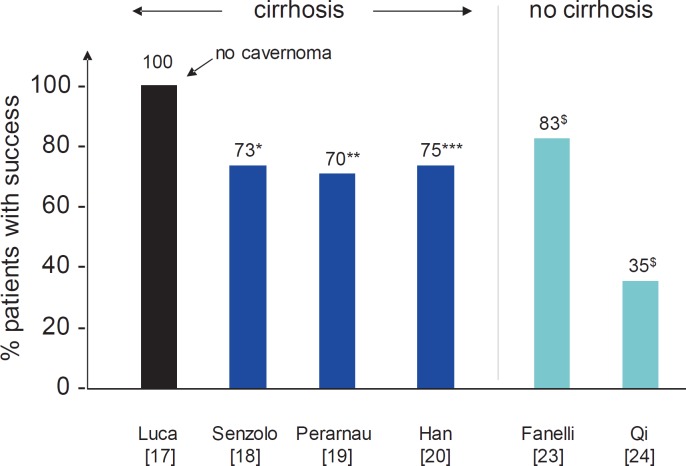
While the TIPS can be implanted in patients with non-cavernomatous PVT with a success rate of up to 100% [17], the technical procedure is much more difficult in chronic PVT with cavernoma of the portal vein. In these patients, success rates for TIPS implantation are limited, ranging from 62 to 74%, and comparable to those in patients without cirrhosis [18,19,20,23,24] (fig. 4). Therefore, from a technical point of view, the decision for TIPS treatment should be made as early as possible.
Fig. 4.
TIPS technical success rates in patients with chronic PVT with cirrhosis without (black) and with various proportions of cavernomas (dark blue). The presence of patients with cavernoma resulted in lower success rates. For comparison, two studies with non-cirrhotic cavernomatous PVT are also presented [23,24]. *9/23 with cavernoma. This study included non-cirrhotic as well as cirrhotic PVT; **15 without cavernoma: 79%, 19 with cavernoma: 63%; ***30/57 with cavernoma; $all patients had cavernoma.
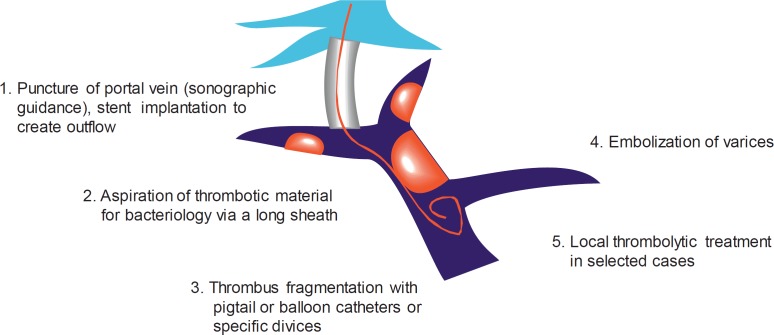
The various steps of the technical procedure are summarized in figure 5. In general, PVT makes the TIPS procedure more difficult because the intrahepatic branches of the portal vein may be narrow or occluded. Therefore, sonographic guidance is mandatory. With its help, even very small intrahepatic branches can be detected and punctured successfully. A stiff Terumo guide wire with a bent tip is then advanced through the thrombus into the portal, splenic, or mesenteric vein. After introducing a pigtail catheter, an angiography shows the portal system and the extension of the thrombosis (fig. 6).
Fig. 5.
Technical steps of the transjugular intervention for PVT. Local thrombolytic treatment using urokinase (50,000-100,000 IU/h) and heparin may be indicated in extended and occlusive thrombosis with elevated fibrinogen concentration.
Fig. 6.
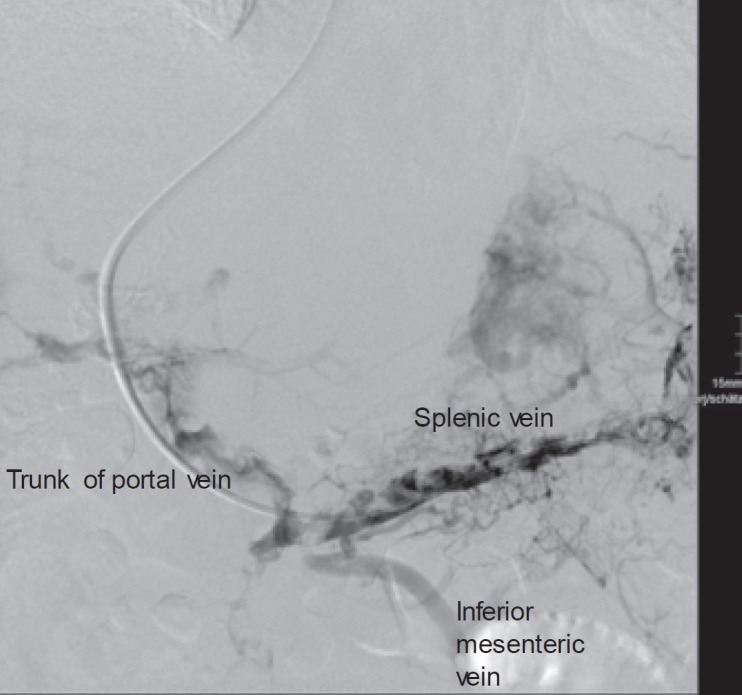
Angiography of the portal system after its puncture showing complete and extended thrombosis without cavernoma.
The next step is the dilatation (8 mm) of the puncture tract followed by the introduction of a long sheath into the portal vein. It allows an aspiration of thrombotic material. A pigtail catheter is then used to further fractionate the thrombus by rapidly moving it forward and backward through the thrombus with the aim to create some prograde flow. After the implantation of a covered stent, a final angiography should now demonstrate the blood flow through the portal system as well as the stent. If the blood flow cannot be seen, further efforts should be carried out to fragment the thrombus, e.g. by using a balloon catheter, until prograde portal flow can be seen. Clot migration resulting in significant lung embolization has not been seen or described in the past but may not be excluded entirely.
In patients with varices, selective embolization should be performed to prevent bleeding. Finally, a 4 French angiography catheter should be left in the splenic vein for a few days to control patency. It is the clinician's decision to provide local thrombolytic treatment with urokinase (50-100 × 103 U/h) together with heparin or anticoagulation with heparin only (fig. 7). In patients with normal or elevated platelet count, platelet aggregation inhibition (100 mg/day ASS) may also be an option to improve long-term patency of the TIPS and the portal vein [25].
Fig. 7.
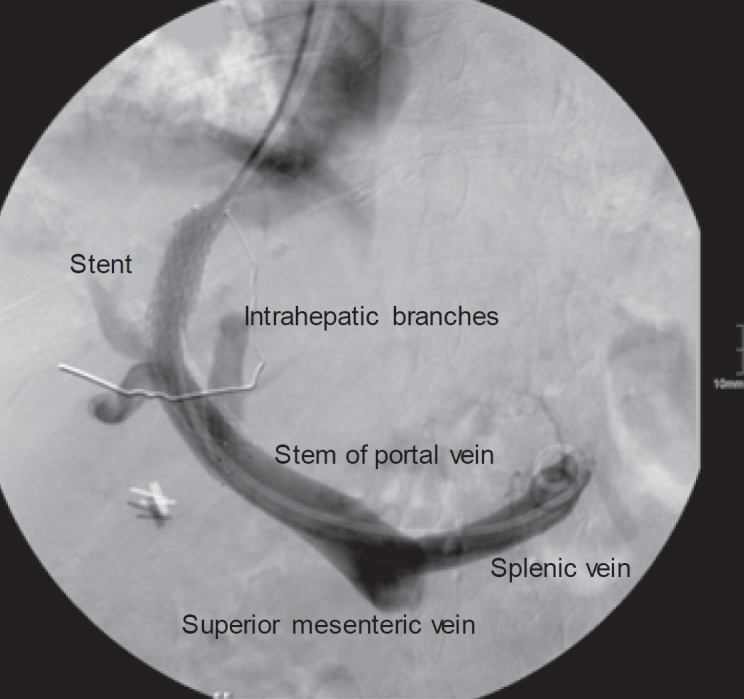
Same patient as in figure 6 after stent implantation (Viatorr), thrombus fragmentation, and thrombolytic therapy resulting in complete repermeation of the extrahepatic portal vein axis. The pigtail catheter remained in place for local treatment and control.
Which Patients with Cirrhotic, Non-Malignant PVT May Benefit from TIPS?
Patients with Symptomatic Portal Hypertension
It is most likely that findings in patients with symptomatic portal hypertension, where TIPS improves survival and resolves symptoms [26,27,28], can also be applied to patients with PVT. The addition of PVT further deteriorates the prognosis, a fact which probably augments the positive effect of the TIPS. Thus, the TIPS implantation seems to be justified in patients with variceal bleedings or tense ascites without prior use of anticoagulants.
Patients with Asymptomatic Portal Hypertension
In patients with asymptomatic portal hypertension not requiring the TIPS intervention at this moment, TIPS may be indicated when the thrombosis is extended and complete and anticoagulation is not very effective [29]. In addition, if high-grade varices are present and do not respond to β-blocker treatment and ligation, anticoagulation may increase the risk of bleeding and justify TIPS as a primary prophylactic prevention together with the treatment of the PVT. The decision for the TIPS should be made early to increase its success rate and efficacy [17,19]. Delay of TIPS until clearly indicated by the respective symptoms has a higher risk of technical failure and inefficacy due to the formation of a cavernoma. Thus, if symptoms appear at late stages or after cavernous formation, TIPS may no longer be an option as a second-line or rescue treatment. In general, a very restrictive indication for the TIPS does not seem to be justified since TIPS is not expected to induce severe shunt-related side-effects in patients with PVT. It should be emphasized that, in these patients, the diameter of TIPS should be small (<8 mm) in order to improve portal vein flow velocity. In patients with asymptomatic portal hypertension with partial or limited PVT who most likely respond to anticoagulation, TIPS may not be indicated.
Patients Awaiting Liver Transplantation
PVT complicates liver transplantation and increases post-transplant mortality [30,31,32,33]. This is in particular true for extended thrombosis with cavernoma. If TIPS is used to prevent or treat PVT in transplant candidates, the question arises whether TIPS itself influences liver transplantation. Several studies found a higher complication rate of liver transplantation in TIPS patients caused by a misplacement of the stent that, however, did not influence the outcome in most studies (table 3) [16,34,35,36,37,38,39]. In the largest study published in 2009, TIPS patients had a significant advantage with respect to graft and patient survival [38]. The high rate of stent misplacement of about 30% is mostly due to a lack of experience of the investigators and is not an intrinsic problem of the procedure. Thus, if extended thrombosis exists and does not respond to anticoagulation early, TIPS seems to be indicated in transplantation candidates to resolve the PVT as well as to prevent its extension and cavernomatous transformation.
Table 3.
Retrospective studies on the effects of TIPS on liver transplantation. Stent misplacement was frequent but did not cause significant technical difficulties
| n |
Waiting time, mean, days |
Stent misplaced intraoperatively |
Transfusions, U |
Cold ischaemic time, min |
Operation time, h |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| TIPS |
TIPS |
TIPS |
TIPS |
TIPS |
TIPS |
||||||
| yes | no | yes | no | yes | yes | no | yes | no | yes | no | |
| Freeman et al., 1994 [34] | 7 | 13 | 282 | 149 | 2 (30%) | 26 | 32 | ||||
| Millis et al., 1995 [35] | 23 | 112 | 5 (20) | 11 | 11 | ||||||
| Chiu et al., 2000 [36]a | 7 | 178 | 440 | 6 (90%) | 25 | 8.1 | 7.7 | ||||
| Tripathi et al., 2002 [37] | 29 | 53 | 77 | 6 (20%) | 15 | 10 | 675 | 713 | 6.9 | 6.3 | |
| Guerrini et al., 2012 [38] | 61 | 591 | 17 (30%) | 7 | 8 | 601 | 632 | ||||
| D'Avola et al., 2012 [16]b | 15 | 8 | 185 | 213 | 4 | 3 | 335 | 329 | |||
| Barbier et al., 2014 [39] | 72 | 136 | 131 | 103 | 23 (30%) | 3 | 3 | 5.3 | 5.5 | ||
| Total | 214 | 136 | 199 | 155 | 36%a | no difference | no difference | 6.8 | 6.5 | ||
Mostly Wallstents.
Patients had preoperative PVT; patency at liver transplantation with/without TIPS: 100%/50%.
Patients with PVT-Induced Deterioration of Liver Function or Hepatic Encephalopathy
In patients developing HE and/or liver failure together with PVT, one may suggest that portal blood flow is crucial for liver function. Therefore, TIPS may resolve the thrombosis but not the underlying problem in these patients. If anticoagulation is not sufficiently effective to regenerate portal perfusion, transjugular local thrombolytic therapy with prior occlusion of the varices may be discussed. Our own experiences are positive; however, published studies are lacking.
Concluding Remarks
In the past, PVT in patients with cirrhosis has been regarded as a stage of the disease where specific treatment is not available. Due to the disadvantages of PVT at liver transplantation, the first study using anticoagulation was performed in transplant candidates, showing reperfusion in 50% of the patients with partial or complete thrombosis and thrombus progression in only 1 patient [6]. Several subsequent studies confirmed these results, putting an end to the therapeutic nihilism of the past [2,4,7,8].
The aim of anticoagulation is not only the recanalization but also the prevention of progression and chronicity of the thrombus leading to cavernoma of the portal vein. Thrombus progression can lead to intestinal infarction, which is considered a severe complication with a potential risk of death [40]. Chronic thrombosis resulting in cavernoma complicates TIPS treatment or transplantation (if required). Anticoagulation is effective but it achieves recanalization in only about 50% of the patients, and 15% have thrombus progression during the treatment. Older age and extension of the thrombus reduce the treatment response. If the thrombus is older than 6 months, the response to anticoagulation is poor, while the response to anticoagulation is not achieved if it is older than 12 months [29]. Unfortunately, the response rate with respect to the thrombosis grade (partial, complete, extended) is not given in most publications. In complete thrombosis, the response of anticoagulation is very limited, thus questioning its use [29]. In addition, side-effects of anticoagulation are considerable, in particular in patients with platelet counts below 50 × 103 per µl, encompassing variceal bleedings and one cerebral bleeding [4,8]. Discontinuation of anticoagulation results in an early recurrence of 38% [4]. Additional issues arguing against anticoagulation are the probably limited compliance of long-term LMWH and the problem with monitoring of VKA [41].
TIPS is highly effective in the recanalization of complete as well as extended thrombosis [17]. If technically feasible, it is also effective in patients with cavernoma [18,19,20]. In addition to its positive effect on PVT, it prevents the occurrence of variceal bleeding, ascites, and related complications, and it prolongs life [12,26,27,28,42]. In patients awaiting liver transplantation, a positive effect on post-transplant outcomes has been shown in a large, retrospective study [38] while some other studies did not show a disadvantage of the TIPS [34,35,36,37,39]. Most importantly, since portal perfusion is already abolished or limited by the thrombosis, the TIPS may not exert severe negative effects on liver function or HE.
Considering the pros and cons regarding anticoagulation and TIPS, the following algorithm (fig. 8) is suggested. Patients with cirrhosis who are at a high risk for PVT may receive primary prophylaxis with LMWH, as suggested by Villa at al. [43]. If PVT occurs, patients with symptomatic portal hypertension may receive TIPS together with local treatment (mechanical fragmentation, thrombolytic treatment) as a primary therapy.
Fig. 8.
Treatment algorithm for PVT in cirrhosis. The decision for the TIPS treatment may depend mainly on the stage of liver disease (symptomatic portal hypertension or not), whether anticoagulation therapy may be promising or not (thrombus age and extension), and whether the patient is a transplant candidate or not.
Patients with asymptomatic portal hypertension should receive anticoagulation when it is promising (limited extension, recent PVT). Patients with partial thrombosis may also receive anticoagulation. However, the benefit of anticoagulation in this group may be questioned because spontaneous remission is frequent and PVT may not have a significant effect on survival [1,44]. In patients without contraindications, TIPS may be preferred when thrombosis is complete, extended, or chronic, or when patients have a high risk of bleeding complications or are candidates for liver transplantation [12]. TIPS may also be a second-line treatment if patients do not respond to anticoagulation within 3-6 months. It should be pointed out that in these asymptomatic patients, the aim of the TIPS is not to normalize portal hypertension but to normalize portal blood flow velocity. This requires only small shunts (6-8 mm) with very little reduction in the pressure gradient. It should be kept in mind that recommendations are preliminary as long as randomized studies are lacking.
Disclosure Statement
The authors MR, BB, and CK do not have any conflicts of interest to declare.
References
- 1.Maruyama H, Okugawa H, Takahashi M, Yokosuka O. De novo portal vein thrombosis in virus-related cirrhosis: predictive factors and long-term outcomes. Am J Gastroenterol. 2013;108:568–574. doi: 10.1038/ajg.2012.452. [DOI] [PubMed] [Google Scholar]
- 2.Werner KT, Sando S, Carey EJ, et al. Portal vein thrombosis in patients with end stage liver disease awaiting liver transplantation: outcome of anticoagulation. Dig Dis Sci. 2013;58:1776–1780. doi: 10.1007/s10620-012-2548-y. [DOI] [PubMed] [Google Scholar]
- 3.Chen H, Qi X, He C, Yin Z, Fan D, Han G. Coagulation imbalance may not contribute to the development of portal vein thrombosis in patients with cirrhosis. Thromb Res. 2013;131:173–177. doi: 10.1016/j.thromres.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Delgado MG, Seijo S, Yepes I, et al. Efficacy and safety of anticoagulation on patients with cirrhosis and portal vein thrombosis. Clin Gastroenterol Hepatol. 2012;10:776–783. doi: 10.1016/j.cgh.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Kinjo N, Kawanaka H, Akahoshi T, et al. Portal vein thrombosis in liver cirrhosis. World J Hepatol. 2014;6:64–71. doi: 10.4254/wjh.v6.i2.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Francoz C, Belghiti J, Vilgrain V, et al. Splanchnic vein thrombosis in candidates for liver transplantation: usefulness of screening and anticoagulation. Gut. 2005;54:691–697. doi: 10.1136/gut.2004.042796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amitrano L, Guardascione MA, Menchise A, et al. Safety and efficacy of anticoagulation therapy with low molecular weight heparin for portal vein thrombosis in patients with liver cirrhosis. J Clin Gastroenetrol. 2010;44:448–451. doi: 10.1097/MCG.0b013e3181b3ab44. [DOI] [PubMed] [Google Scholar]
- 8.Senzolo M, Sartori T, Rosetto V, et al. Prospective evaluation of anticoagulation and transjugular intrahepatic portosystemic shunt for the management of portal vein thrombosis in cirrhosis. Liver Int. 2012;32:919–927. doi: 10.1111/j.1478-3231.2012.02785.x. [DOI] [PubMed] [Google Scholar]
- 9.Bechmann LP, Sichau M, Wichert M, Gerken G, Kröger K, Hilgard P. Low-molecular-weight heparin in patients with advanced cirrhosis. Liver Int. 2011;31:75–82. doi: 10.1111/j.1478-3231.2010.02358.x. [DOI] [PubMed] [Google Scholar]
- 10.Rodriguez-Castro KI, Senzolo M. Optimal length of anticoagulation therapy in cirrhotic patients with portal vein thrombosis. Clin Gastroenterol Hepatol. 2012;10:820–821. doi: 10.1016/j.cgh.2012.02.021. [DOI] [PubMed] [Google Scholar]
- 11.Rössle M, Haag K, Ochs A, et al. The transjugular intrahepatic portosystemic stent-shunt procedure for variceal bleeding. N Engl J Med. 1994;330:165–171. doi: 10.1056/NEJM199401203300303. [DOI] [PubMed] [Google Scholar]
- 12.Rössle M. TIPS: 25 years later. J Hepatol. 2013;59:1081–1093. doi: 10.1016/j.jhep.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 13.Lautt WW. Regulatory processes interacting to maintain hepatic blood flow constancy: vascular compliance, hepatic arterial buffer response, hepatorenal reflex, liver regeneration, escape from vasoconstriction. Hepatol Res. 2007;37:891–893. doi: 10.1111/j.1872-034X.2007.00148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hassoun Z, Deschenes M, Lafortune M, et al. Relationship between pre-TIPS liver perfusion by the portal vein and the incidence of post-TIPS chronic hepatic encephalopathy. Am J Gastroenterol. 2001;96:1205–1209. doi: 10.1111/j.1572-0241.2001.03704.x. [DOI] [PubMed] [Google Scholar]
- 15.Deng D, Liao MS, Qin JP, Li XA. Relationship between pre-TIPS hepatic hemodynamics and postoperative incidence of hepatic encephalopathy. Hepatobiliary Pancreat Dis Int. 2006;5:232–236. [PubMed] [Google Scholar]
- 16.D'Avola D, Bilbao JI, Zozaya G, et al. Efficacy of transjugular intrahepatic portosystemic shunt to prevent total portal vein thrombosis in cirrhotic patients awaiting for liver transplantation. Transplant Proc. 2012;44:2603–2605. doi: 10.1016/j.transproceed.2012.09.050. [DOI] [PubMed] [Google Scholar]
- 17.Luca A, Miraglia R, Caruso S, et al. Short- and long-term effects of the transjugular intrahepatic portosystemic shunt on portal vein thrombosis in patients with cirrhosis. Gut. 2011;60:846–852. doi: 10.1136/gut.2010.228023. [DOI] [PubMed] [Google Scholar]
- 18.Senzolo M, Tibbals J, Cholongitas E, et al. Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with and without cavernous transformation. Aliment Pharmacol Ther. 2006;23:767–775. doi: 10.1111/j.1365-2036.2006.02820.x. [DOI] [PubMed] [Google Scholar]
- 19.Perarnau JM, Baju A, D'alteroche L, et al. Feasibility and long-term evolution of TIPS in cirrhotic patients with portal thrombosis. Eur J Gastroenterol Hepatol. 2010;22:1093–1098. doi: 10.1097/MEG.0b013e328338d995. [DOI] [PubMed] [Google Scholar]
- 20.Han G, Qi X, He C, et al. Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with symptomatic portal hypertension in liver cirrhosis. J Hepatol. 2011;54:78–88. doi: 10.1016/j.jhep.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 21.Bauer J, Johnson S, Durham J, et al. The role of TIPS for portal vein patency in liver transplant patients with portal vein thrombosis. Liver Transpl. 2006;12:1544–1551. doi: 10.1002/lt.20869. [DOI] [PubMed] [Google Scholar]
- 22.Liatsos C, Vlachogiannakos J, Patch D, et al. Successful recanalization of portal vein thrombosis before liver transplantation using transjugular intrahepatic portosystemic shunt. Liver Transpl. 2001;7:453–460. doi: 10.1053/jlts.2001.23914. [DOI] [PubMed] [Google Scholar]
- 23.Fanelli F, Angeloni S, Salvatori FM, et al. Transjugular intrahepatic portosystemic shunt with expanded-polytetrafluorethylene-covered stents in non-cirrhotic patient with portal cavernoma. Dig Liver Dis. 2011;43:78–84. doi: 10.1016/j.dld.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 24.Qi X, Han G, Yin Z, et al. Transjugular intrahepatic portosystemic shunt for portal cavernoma with symptomatic portal hypertension in non-cirrhotic patients. Dig Dis Sci. 2012;57:1072–1082. doi: 10.1007/s10620-011-1975-5. [DOI] [PubMed] [Google Scholar]
- 25.Siegerstetter V, Huber M, Ochs A, Blum HE, Rössle M. Platelet aggregation and platelet-derived growth factor inhibition for prevention of insufficiency of the transjugular intrahepatic portosystemic shunt: a randomized study comparing trapidil plus ticlopidin with heparin treatment. Hepatology. 1999;29:33–38. doi: 10.1002/hep.510290139. [DOI] [PubMed] [Google Scholar]
- 26.Garcia-Pagan JC, Caca K, Bureau C, et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;162:2370–2379. doi: 10.1056/NEJMoa0910102. [DOI] [PubMed] [Google Scholar]
- 27.Salerno F, Camma C, Enea A, et al. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology. 2007;133:825–834. doi: 10.1053/j.gastro.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 28.Rössle M, Ochs A, Gulberg V, Siegerstetter V, Holl J, Deibert P, Olschewski M, Reiser M, Gerbes AL. A comparison of paracentesis and transjugular intrahepatic portosystemic shunting in patients with ascites. N Engl J Med. 2000;342:1701–1707. doi: 10.1056/NEJM200006083422303. [DOI] [PubMed] [Google Scholar]
- 29.Qi X, Han G, Fan D. Degree of portal vein thrombosis might be associated with recanalization during anticoagulation. Clin Gastroenterol Hepatol. 2012;10:820. doi: 10.1016/j.cgh.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 30.Englesbe MJ, Schaubel DE, Cai S, Guidinger MK, Merion DM. Portal vein thrombosis and liver transplant survival benefit. Liver Transpl. 2010;16:999–1005. doi: 10.1002/lt.22105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lendoire J, Raffin G, Cejas N, et al. Liver transplantation in adult patients with portal vein thrombosis: risk factors, management and outcome. HPB (Oxford) 2007;9:352–356. doi: 10.1080/13651820701599033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Egawa H, Tanaka K, Kasahara M, et al. Single center experience of 39 patients with preoperative portal vein thrombosis among 404 adult living donor liver transplantations. Liver Transpl. 2006;12:1512–1518. doi: 10.1002/lt.20777. [DOI] [PubMed] [Google Scholar]
- 33.Doenecke A, Tsui T-Y, Zuelke C, et al. Pre-existent portal vein thrombosis in liver transplantation: influence of pre-operative disease severity. Clin Transplant. 2010;24:48–55. doi: 10.1111/j.1399-0012.2009.00977.x. [DOI] [PubMed] [Google Scholar]
- 34.Freeman RB, FitzMaurice SE, Greenfield AE, Halin N, Haug CE, Rohrer RJ. Is the transjugular intrahepatic portosystemic shunt procedure beneficial for liver transplant recipients? Transplantation. 1994;15:297–300. [PubMed] [Google Scholar]
- 35.Millis JM, Martin P, Gommes A, et al. Transjugular intrahepatic portosystemic shunts: impact on liver transplantation. Liver Transpl Surg. 1995;1:229–233. doi: 10.1002/lt.500010406. [DOI] [PubMed] [Google Scholar]
- 36.Chiu AKK, Rao ARN, Waugh RC, et al. Liver transplantation in patients with transjugular intrahepatic portosystemic shunts. Aust N Z J Surg. 2000;70:493–495. doi: 10.1046/j.1440-1622.2000.01857.x. [DOI] [PubMed] [Google Scholar]
- 37.Tripathi D, Therapondos G, Redhead DN, Madhavan KK, Hayes PC. Transjugular intrahepatic portosystemic stent-shunt and its effects on orthotopic liver transplantation. Eur J Gastroenterol Hepatol. 2002;14:827–832. doi: 10.1097/00042737-200208000-00003. [DOI] [PubMed] [Google Scholar]
- 38.Guerrini GP, Pleguezuelo M, Maimone S, et al. Impact of TIPS preliver transplantation for the outcome posttransplantation. Am J Transplant. 2009;9:192–200. doi: 10.1111/j.1600-6143.2008.02472.x. [DOI] [PubMed] [Google Scholar]
- 39.Barbier L, Hardwigsen J, Borentain P, et al. Impact of transjugular intrahepatic portosystemic shunting on liver transplantation: 12-year single-center experience. Clin Res Hepatol Gastroenterol. 2014;38:155–163. doi: 10.1016/j.clinre.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 40.Amitrano L, Guardascione MA, Brancaccio V, et al. Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. J Hepatol. 2004;40:736–741. doi: 10.1016/j.jhep.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 41.Tsochatzis EA, Senzolo M, Germani G, Gatt A, Burroughs AK. Systematic review: portal vein thrombosis in cirrhosis. Aliment Pharmacol Ther. 2010;31:366–374. doi: 10.1111/j.1365-2036.2009.04182.x. [DOI] [PubMed] [Google Scholar]
- 42.Rössle M, Gerbes AL. TIPS for the treatment of refractory ascites, hepatorenal syndrome and hepatic hydrothorax: a critical update. Gut. 2010;59:988–1000. doi: 10.1136/gut.2009.193227. [DOI] [PubMed] [Google Scholar]
- 43.Villa E, Camma C, Marietta M, et al. Enoxaparin prevents portal vein thrombosis and liver decompensation in patients with advanced cirrhosis. Gastroenterology. 2012;143:1253–1260. doi: 10.1053/j.gastro.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 44.Luca A, Caruso S, Milazzo M, et al. Natural course of extrahepatic nonmalignant partial portal vein thrombosis in patients with cirrhosis. Radiology. 2012;265:124–132. doi: 10.1148/radiol.12112236. [DOI] [PubMed] [Google Scholar]