Abstract
In 2011–2012, only 34% of 13–17 years olds in the United States (US) received seasonal influenza vaccine. Little is known about the link between parents' sources of health information, their vaccine-related attitudes, and vaccination of their adolescent against influenza. This study seeks to determine the relationship between number of sources of information on influenza vaccine, parental attitudes toward influenza vaccine, and influenza vaccine uptake in adolescents. We conducted a telephone and web-based survey among US parents of students enrolled in 6 middle and 5 high schools in Georgia. Bivariate and multivariable analyses were conducted to examine associations between the number of information sources about influenza vaccine and vaccine receipt and whether parent vaccine-related attitudes act as a mediator. The most commonly reported sources of information were: a physician/medical professional (95.0%), a family member or friend (80.6%), and television (77.2%). Parents who had higher attitude scores toward influenza vaccine were 5 times as likely to report their adolescent had ever received influenza vaccine compared to parents who had lower attitude scores (adjusted odds ratio (aOR) 5.1; 95% confidence intervals (CI) 3.1–8.4; P < 0.01). Parent vaccine-related attitudes were a significant mediator of the relationship between sources of information and vaccine receipt. In light of the low response rate and participation in an adolescent vaccination intervention, findings may not be generalizable to other populations. This study shows the importance of multiple sources of information in influencing parental decision-making about influenza vaccine for adolescents. Harnessing the power of mass media and family members and friends as health advocates for influenza vaccination can potentially help increase vaccination coverage of adolescents.
Keywords: adolescents, attitudes, influenza, media, mediation, vaccine
Abbreviations
- ACIP
Advisory Committee on Immunization Practices
- HPV
Human Papillomavirus
- aOR
Adjusted Odds Ratio
- CI
Confidence Intervals
- HBM
Health Belief Model
- TRA
Theory of Reasoned Action
Introduction
Despite efforts to increase seasonal influenza vaccination uptake, influenza remains a significant health burden in the United States.1 Research indicates that vaccinating school-aged children against influenza not only protects them directly, but may also reduce transmission to contacts, especially persons at high risk for complications such as infants and the elderly.2,3 In 2008, the federal Advisory Committee on Immunization Practices (ACIP) recommended seasonal influenza vaccination for all school-aged children.4 Despite this, only 34% of 13–17 years olds received an influenza vaccine in 2011–2012,5 which is well below the Healthy People 2020 goal of 70%.6
Recent studies have shown that some ethnic and racial minority populations, as well as those in lower socioeconomic positions, are less likely to be vaccinated at all ages than their counterparts in other groups.7-9 However, there have been few studies conducted to understand the influence of the communication environment, especially sources of information, on influenza vaccination rates among socioeconomically and racially diverse adolescents. The decision to vaccinate children can be affected by parental sources of information including exposure to media, and by their information-seeking behavior.10 Complex processes govern parents' decision-making process regarding vaccination and the data is mixed in terms of the role that information alone plays.11-14 The literature indicates that people with greater access to media information and who obtain sufficient information by actively researching that information tend to have a higher rate of vaccine uptake than those with less access or those who are less active in their search.8,15
Vaccine-related information can come from several sources. One of the most common and influential sources is a physician or medical professional.16-19 In addition to physicians or medical professionals, research has found an association between media exposure and vaccination coverage. A study of parents of children with asthma found that an increase in influenza vaccination coincided with an increase in media coverage.20 A study of younger children 6 to 59 months of age, found that influenza-related media coverage explained 85% of the variation in influenza vaccinations when compared to the same time the previous year.21 Another study found a significant association between parents vaccinating their children against the 2009 H1N1 influenza pandemic and watching national television news.13 Research on another adolescent recommended vaccine, the human papillomavirus (HPV) vaccine, also supports the hypothesis that media exposure influences vaccination. In-depth interviews with mothers revealed that exposure to media and marketing about HPV vaccination played a crucial role in their decision to vaccinate their daughters by raising awareness about the vaccine, providing facts about the vaccine and its benefits, prompting discussions with their daughters, and encouraging them to seek more information.22 A content analysis of HPV stories from major newspapers, the AP wire, and television news networks found that exposure to health-related media content was significantly associated with knowledge about HPV.23
In light of the previous work that has identified important drivers of adolescent influenza vaccination, the objectives of this paper are to (1) describe parents' sources of information about influenza vaccine, (2) determine whether the number of reported sources of information is associated with having their adolescent receive influenza vaccine, and (3) determine if parental attitudes toward vaccines act as a mediator in the relationship between sources of information and receipt of influenza vaccine among a racially/ethnically and socio-demographically diverse sample.
Results
Description of participants
The majority of adolescents were female (54.2%), African-American (74.2%), and in 6th to 8th grade (59.2%); 61.9% of parents reported that their adolescent had received influenza vaccine the prior fall/winter (Table 1). The respondents were evenly distributed among the intervention arms (Table 1). The majority of respondents were the mother of the adolescent (83.9%), with the smallest proportion (7.5%) being ‘other’ which included grandmother, grandfather, aunt, and guardians (Table 1).
Table 1.
Demographics characteristics of study population
| Characteristics | No. (%) |
|---|---|
| Total | 360 (100) |
| Adolescent Characteristics | |
| Gender | |
| Male | 165 (45.8) |
| Female | 195 (54.2) |
| Race/Ethnicity | |
| White | 59 (16.4) |
| African-American | 267 (74.2) |
| Hispanic | 6 (1.7) |
| Other | 28 (7.8) |
| Grade | |
| 6–8th | 213 (59.2) |
| 9–12th | 147 (40.8) |
| Received influenza vaccine prior fall/winter | |
| Yes | 223 (61.9) |
| No | 137 (39.1) |
| Parent Characteristic | |
| Relation to adolescent | |
| Mother | 302 (83.9) |
| Father | 31 (8.6) |
| Other | 27 (7.5) |
| Study Characteristics | |
| Intervention arm | |
| Arm 1 | 114 (31.7) |
| Arm 2 | 130 (36.1) |
| Arm 3 | 116 (32.2) |
Reported sources of information on influenza vaccine
A majority of respondents reported that they had heard about influenza vaccine from their physician or medical professional (95.0%), followed by family or friends (80.6%), and television (77.2%). The least frequently reported source of information on influenza vaccine was radio (47.8%) (Table 2). A majority reported a mostly positive (50.4%) or neutral (43.2%) portrayal of influenza vaccine in the media (data not shown).
Table 2.
Reported sources of information
| Source of information | No. (%) |
|---|---|
| Physician or Medical Professional | 342 (95.0) |
| Family or Friends | 290 (80.6) |
| Television | 278 (77.2) |
| Advertisement from drug company | 207 (57.5) |
| Internet | 183 (50.8) |
| Newspaper or magazine article | 179 (49.7) |
| Radio | 172 (47.8) |
Association of number of sources of information and receipt of influenza vaccine
In the crude analysis, gender, grade, race, parental attitudes regarding influenza vaccine, media prompted parent to speak with doctor, and the number of sources of information on influenza vaccine were significantly associated with the adolescent having received influenza vaccine the prior fall/winter (Table 3). After adjusting, adolescents in grades 6–8 were 1.4 times as likely to have received influenza vaccine the prior fall/winter compared to adolescents in grades 9–12 (adjusted odds ratio (aOR) 1.4; 95% confidence intervals (CI) 1.1–2.8; p = 0.02). Parent who reported that hearing about influenza vaccine in the media prompted them to talk to their adolescent's doctor about influenza vaccine were almost twice as likely to report that their adolescent received an influenza vaccine the prior fall/winter (aOR 1.8; 95% CI 1.1–3.0; p = 0.02). Parents who scored high (7–10) on the attitudes scale were 5 times more likely to report their adolescent having received the influenza vaccine the prior fall/winter compared to parents who scored lower (0–6) (aOR 5.1; 95% CI 3.1–8.4; P < 0.01) (Table 3).
Table 3.
Association between selected demographics and number of reported sources of information with having received influenza vaccine the prior fall/winter
| Variable | Crude Odds Ratio (95% CI) | P-value | Adjusted Odds Ratio* (95% CI) | P-value |
|---|---|---|---|---|
| Adolescent Characteristics | ||||
| Gender | ||||
| Male | REF | REF | ||
| Female | 1.5 (1.0–2.4) | 0.04 | 1.3 (0.8–2.2) | 0.29 |
| Race/Ethnicity | ||||
| White | REF | REF | ||
| African-American | 1.0 (0.6–1.8) | 0.97 | 1.1 (0.5–2.1) | 0.85 |
| Hispanic | 3.4 (0.4–31.2) | 0.27 | 2.6 (0.2–30.0) | 0.43 |
| Other | 4.1 (1.3–13.4) | 0.02 | 3.6 (1.0–12.9) | 0.05 |
| Grade | ||||
| 6–8th | 1.6 (1.1–2.5) | .03 | 1.4 (1.1–2.8) | 0.02 |
| 9–12th | REF | REF | ||
| Parental Characteristics | ||||
| Relation to adolescent | ||||
| Mother | 1.6 (0.7–3.6) | 0.23 | 1.4 (0.6–3.5) | 0.47 |
| Father | 1.1 (0.4–3.2) | 0.82 | 1.3 (0.4–4.3) | 0.68 |
| Other | REF | REF | ||
| Parental attitudes | ||||
| 0–6 | REF | REF | ||
| 7–10 | 5.8 (3.6–9.3) | <0.01 | 5.1 (3.1–8.4) | <0.01 |
| Prompt to speak to doctor | ||||
| No | REF | REF | ||
| Yes | 2.0 (1.3–3.0) | 0.002 | 1.8 (1.1–3.0) | 0.02 |
| Intervention arm | ||||
| Arm 1 | REF | REF | ||
| Arm 2 | 0.5 (0.3–0.9) | 0.03 | 0.7 (0.4–1.2) | 0.20 |
| Arm 3 | 0.6 (0.4–1.1) | 0.12 | 0.6 (0.3–1.2) | 0.13 |
| Number of sources of information | ||||
| 0–2 | REF | REF | ||
| 3–7 | 2.3 (1.4–3.1) | 0.03 | 1.3 (0.8–2.8) | 0.12 |
Adjusted for adolescent gender, race, grade, respondent's relationship to adolescent, parental attitudes, prompt to speak to doctor, intervention arm, and number of information sources
Mediation analysis
Since after adjustment the number of sources of information on influenza vaccine was no longer associated with the adolescent having received the influenza vaccine the prior fall/winter, we tested whether parental attitudes acted as a mediator for the relationship between number of information sources and the adolescent having ever received influenza vaccine. Controlling for intervention arm (Fig. 1), participants who reported more sources of information were more likely to have more positive attitudes than those with fewer reported sources of information (a = 0.7134, p = 0.0122). Participants who had more positive attitudes were more likely to have an adolescent who had received influenza vaccine the prior fall/winter (b = 0.5011, P < 0.0001). A bias-corrected bootstrap confidence interval for the indirect effect (ab = 0.3575) based on 1,000 bootstrap samples was entirely above zero (0.0731 to 0.7055). There was no evidence that sources of information influenced receipt of influenza vaccine independent of its effect on parental attitudes (c′ = 0.5175, p = 0.1148).
Figure 1.
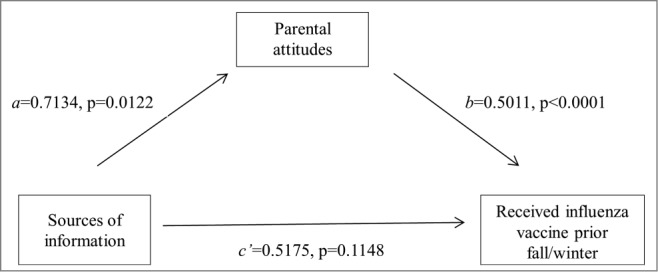
Simple mediation model for presumed influence of parental attitudes on the association between sources of information and receiving an influenza vaccine the prior fall/winter.
Discussion
To our knowledge, this is the first study that conducted a mediation analysis to examine information source exposure and influenza vaccine attitudes. The results from this analysis demonstrate that the significant association between total number of sources of information about influenza vaccine and receipt of influenza vaccine could be explained by more favorable influenza vaccine attitude scores. This finding could mean that simply being exposed to information is not sufficient to influence parental decisions about influenza vaccination. It is likely that the content of messages and/or appraisal of the value of a source influence attitudes in meaningful ways that can ultimately affect likelihood of vaccination.
Parents in 2 of the 3 study arms had received educational materials on adolescent immunization, including influenza vaccine. Intervention arm was controlled for in the analysis and was shown to have no association with vaccine receipt. In addition, the intervention brochure was not an option as an information source in the survey. Nevertheless, there remains a possibility that the information they received for the intervention may have influenced the types of information sources they reported and/or their perceptions from which media sources they received information on influenza vaccine. The impact of the brochure and adolescent intervention on vaccination uptake is currently under analysis.
The most common source of information about influenza vaccine reported by parents was physician or medical professional. It has been shown that physician recommendation for vaccination is associated with uptake,16-19 and we found that over 90% of parents report hearing about influenza vaccine from a physician or medical professional, which is encouraging. One study of 2009 H1N1 pandemic influenza vaccine uptake found that mass media exposure but not consultation with a medical professional was significantly associated with vaccine uptake.13 In addition, we found that hearing about influenza vaccine in the media prompted parents to talk to their adolescent's doctor about influenza was associated with receiving the influenza vaccine the previous fall/winter. The recommendation of one's own physician has been shown to be a key factor in a parents' decision to accept vaccination for their child,16-19 and how this interacts with messages from the media deserves further study. Taken together, these observations may indicate that parents' influenza vaccine-related behavior may be influenced on several different fronts, highlighting the importance of population-based health communication in addition to parent-physician communication.
The results of this study illustrate several interesting points in explaining how the vaccination behaviors of parents may be influenced by health communication. First, after physician or medical professional, family or friends was the next frequently reported source of information on influenza vaccine. This finding may provide support for the importance of social norms in encouraging vaccination among parents as other studies have demonstrated.23-30 Second, we can say that media exposure may contribute to a positive attitude of parents which was associated with their adolescent receiving an influenza vaccine. A previous study found a relationship between media exposure and knowledge about vaccines,13,23 but none have examined the relationship between sources of information about influenza vaccine and parental attitudes and how this may impact influenza vaccination uptake.
While this study focused only on the parent's attitudes and how that relates to sources of information and influenza vaccine receipt for their adolescent, it should not be forgotten that the adolescent themselves probably play an active role in health-related decisions. Previous work from our group showed that adolescents who participated in a school-based influenza vaccination clinic were more likely to have initiated a conversation with their parents about being vaccinated than non-vaccinated students.31 Future research should also examine the role of adolescent attitudes and their sources of information and decision-making dynamics between parents and adolescents. Additional detail and information should also be collected to determine how the information and knowledge has been applied by the parent in the decision-making process. For example, questions can address if parents understand or learned the concept of ‘herd immunity’ with questions like, “vaccinating our adolescent protects our household, other school children, and the community in general.”
Given the fact that nearly all parents characterized what they heard about influenza vaccine in the media as mostly positive or neutral, it is encouraging that these broadcast sources were found to be positively associated with vaccine uptake. One possible explanation for the use of media stories as a source of information is that the stories can be used by parents as a decision aid.28 In this case, someone might consider news stories in deciding whether or not to vaccinate their adolescent. If media content is going to be used in the context of decision-making, then stories need to include accurate and balanced information regarding risks and benefits. While these data cannot establish causality for the associations, the information provides evidence supporting the importance of improving vaccine information content available in the media. Moreover, the association between parental attitudes and media as an information source can be bidirectional. The information from the media may influence parental attitudes and behaviors toward vaccines. What remains to be explored is whether parents who are more accepting or not accepting of vaccination may be more likely to pay attention to media messages about vaccines.
Limitations
This study population is from one county in Georgia that was participating in an adolescent vaccination intervention; therefore the results may not be generalizable to other populations. Further, the rate of return of consent forms was low, reducing the power of our analysis and the precision of our effect estimates. However, low response rates are a constant challenge in school-based studies, and our response rate is comparable to that of other studies that mailed surveys.29,32-35 The low response rate raises concerns about generalizability and possible bias as parents who participated in the survey may differ in important ways from the majority of parents who opted not to take the survey. Those parents who feel more positive about vaccines may be more likely to respond compared to those who feel more negative or neutral about vaccines, leading to an overestimation of vaccination uptake and attitudes toward vaccines. Since we did not collect information on parents who did not complete the survey, comparisons to test for bias are not possible. However, recent research suggests that low recruitment may not bias observed results as much as previously thought.36-38 In order to increase response rate, future studies should try recruiting parents at school events, like open house, or researchers should consider sending mailings containing information fliers, newsletters with updates on the project, or holiday cards to maintain more consistency of communications throughout the project. Further research on a larger population will be needed to confirm this study's findings as well as examine this relationship more closely, in particular, the interplay between mass media and social norms and if the frequencies of exposure or specific type of media are influential. Parent report of vaccination was not confirmed by review of medical records so there may be recall bias. Finally, we did not collect information on the content or quality of information or on the number of times information was received from the different sources.
Conclusions
In order to improve influenza vaccination rates for seasonal and pandemic influenza, we need to expand our understanding of the role of health communication in vaccination. Health decision-making processes, such as a decision to receive a vaccine, do not occur in a vacuum but are influenced by health communication messaging, either from other people or mass media. This study shows the important role of multiple sources of information in influencing parental decision-making about influenza vaccine for adolescents. The role of physicians and other medical professionals influencing health decision-making, such as vaccination, is well documented. Harnessing the power of mass media as well as family members and friends as health advocates for influenza vaccination could potentially help increase vaccination rates among adolescents.
Methods
Study population
Participants in this analysis were a part of a larger intervention trial assessing strategies for increasing adolescent vaccination coverage for all 4 adolescent recommended vaccines, influenza, tetanus-diphtheria-pertussis, meningococcal, and human papillomavirus vaccines. The intervention has been described elsewhere.39 Briefly, the study was a multi-component, 3-arm controlled trial, which included 2 intervention arms and a control group. Six middle- and 5 high-schools, all located in one county in Georgia, participated. The intervention arms were (1) a parent-only intervention consisting of an educational brochure about adolescent immunizations guided by theoretical constructs (Health Belief Model (HBM) and Theory of Reasoned Action (TRA)), and (2) a parent and adolescent intervention, consisting of a teacher-delivered presentation including hands-on activities and problem-based learning exercises in addition to the materials from the parent-only arm. Survey eligibility criteria included (i) residing in Richmond County, Georgia, (ii) having adolescent(s) enrolled in a participating middle- or high-school, and (iii) providing consent to participate. Study protocols were reviewed and approved by the Emory Institutional Review Board (IRB) and the IRBs of collaborating institutions.
Data collection
Data collection methods are described elsewhere.17 Briefly, packets of study materials were mailed to a random sample of parents (or primary caretakers) of adolescents enrolled in either the middle- or high-schools in each study arm. The packets included an invitation letter briefly describing the survey, options to participate in the survey (via telephone or via an online survey), telephone numbers to call with questions or to complete the survey, and website address to complete the survey online. Data on sources of information were only collected during the third and final year of follow-up surveys which began in April 2013 and continued through July 2013 (Fig. S1). Reminder phone calls were made 2-weeks after the initial mailing and reminder postcards were mailed in May 2013. Each survey took approximately 25 minutes to administer, and parents received a $20 gift card as compensation for their time upon completion of the survey. Of the 4,876 invited to participate in the final year, 360 (7.4%) completed the survey.
Measures
Demographic information
Participants reported their child's gender, race, and school grade.
Attitudes and beliefs toward vaccination
Questions specific to: perceived susceptibility and perceived severity of influenza for adolescents; perceived barriers and perceived benefits of influenza vaccination for adolescents; and perceived social norms about getting adolescents vaccinated were asked. An influenza vaccine attitude score was computed for the 10 influenza vaccine attitude items. Each “true” item contributed one point to the overall influenza vaccine attitude score. Possible total scores range from 0–10, with higher scores indicating more positive attitudes toward influenza vaccination. Responses were added and dichotomized, according to the median score, into those who scored 0–6 (less positive) and 7–10 (more positive). Table 4 displays how key constructs from the HBM and TRA map onto questions on the parent survey.
Table 4.
Application of Health Belief Model (HBM) and Theory of Reasoned Action (TRA) constructs to inform the parent survey
| Theoretical Constructs | Items per Construct |
|---|---|
| Perceived Susceptibility (HBM) | - My child is not very likely to get the flu- A healthy 40-year-old is more likely to get the flu than my child- Compared to other children your child's age, your child is more likely to get the flu |
| Perceived Severity (HBM) | - Flu is a serious illness |
| Perceived Barriers (HBM) | - Your child could get sick from the flu vaccine itself |
| Perceived Benefits (HBM) | - Giving the flu vaccine to children will decrease their parents' time lost from work- Giving the flu vaccine to children decreases their time out of school- Children should be vaccinated against the flu |
| Social Norms (TRA) | - Most parents I know take their children for the flu vaccine- Most people important to me think I would give my child the flu vaccine |
Sources of information
Several questions were asked to examine exposure and relative value of information sources as correlates of influenza vaccine uptake. Parents were asked to indicate whether or not they had heard of influenza vaccine from each of the following 7 sources: physician/medical professional, family or friends, drug advertisement, internet (non-drug advertisement, such as a webpage or blog), TV (non-drug advertisement, such as the news), radio (non-drug advertisement), or newspaper/magazine article. Parents were asked to select all responses that applied; it was possible to report exposure to up to 7 sources. Responses were added and dichotomized, according to the median score, into those who reported 0–2 sources (low) and 3–7 sources (high).
Participants were also asked about their perception of media sources through the question, “Has what you have heard about influenza in the media, say in the newspaper or on TV, been mostly positive, mostly negative, or would you say it's been neutral?” Parents were also asked if hearing about the influenza vaccine from a previously mentioned media source prompted them to speak to their child's doctor about the influenza vaccine (yes/no).
Main outcome
The main outcome was parent report of their adolescent having received an influenza vaccine the prior fall or winter.
Data analysis
Since the current analysis is not designed to detect differences by study arm, the sample was treated as a single cross-section. Descriptive statistics were conducted on socio-demographic characteristics, information sources, attitudes toward influenza vaccination, and the outcome measure. Bivariate and multivariable logistic regressions were conducted to assess correlates of having received influenza vaccine the prior fall/winter, controlling for all other variables in the model.
A simple mediation analysis was performed using ordinary least squares path analysis of the PROCESS SAS macro to test a second hypothesis, that parental attitudes explain the association between information sources and influenza vaccine uptake.40 All analyses were conducted using SAS9.2 (Cary, NC) and evaluated at the P ≤ 0.05 significance level.
Acknowledgments
The authors wish to thank Dianne Miller at Emory University, Dr. Ketty M Gonzalez, former District Health Director for the East Central Health District, Dr. Tara Vogt, Project Officer, and the school district administrators, principals, teachers, and staff of participating schools. We would also like to thank our survey participants.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Funding
This project is funded by the Centers for Disease Control and Prevention cooperative agreement 5UO1IP000413. Dr. Sales was supported by grant K01 MH085506 from the National Institute of Mental Health, NIH.
Supplemental Material
Supplemental data for this article can be accessed on the publisher's website.
References
- 1.Smith NM, Bresee JS, Shay DK, Uyeki TM, Cox NJ, Strikas RA. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2006; 55:1-42; PMID:16874296 [PubMed] [Google Scholar]
- 2.Davis MM, King JC Jr., Moag L, Cummings G, Magder LS. Countywide school-based influenza immunization: direct and indirect impact on student absenteeism. Pediatrics 2008; 122:e260-5; PMID:18595972; http://dx.doi.org/ 10.1542/peds.2007-2963 [DOI] [PubMed] [Google Scholar]
- 3.King JC Jr., Cummings GE, Stoddard J, Readmond BX, Magder LS, Stong M, Hoffmaster M, Rubin J, Tsai T, Ruff E. A pilot study of the effectiveness of a school-based influenza vaccination program. Pediatrics 2005; 116:e868-73; PMID:16322144; http://dx.doi.org/ 10.1542/peds.2005-1301 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention CDC's advisory committee recommends influenza vaccination for Children 6 months through 18 years of age. 2008 [Google Scholar]
- 5.Centers for Disease Control and Prevention Flu vaccination coverage, United States, 2011–12 influenza season. 2013 [Google Scholar]
- 6.Healthy People 2020 Topics and objectives: immunization and infectious diseases. 2014 [Google Scholar]
- 7.Bryant WK, Ompad DC, Sisco S, Blaney S, Glidden K, Phillips E, Vlahov D, Galea S. Determinants of influenza vaccination in hard-to-reach urban populations. Prev Med 2006; 43:60-70; PMID:16684559; http://dx.doi.org/ 10.1016/j.ypmed.2006.03.018 [DOI] [PubMed] [Google Scholar]
- 8.Galarce EM, Minsky S, Viswanath K. Socioeconomic status, demographics, beliefs and A(H1N1) vaccine uptake in the United States. Vaccine 2011; 29:5284-9; PMID:21621577; http://dx.doi.org/ 10.1016/j.vaccine.2011.05.014 [DOI] [PubMed] [Google Scholar]
- 9.Ostbye T, Taylor DH, Lee AM, Greenberg G, van Scoyoc L. Racial differences in influenza vaccination among older Americans 1996–2000: longitudinal analysis of the Health and Retirement Study (HRS) and the Asset and Health Dynamics Among the Oldest Old (AHEAD) survey. BMC Public Health 2003; 3:41; PMID:14678561; http://dx.doi.org/ 10.1186/1471-2458-3-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galarce EM, Ramanadhan S, Viswanath K. Health information seeking In: Thompson TL, Roxanne P, Nussbaum JF, eds. The Routledge Handbook of Health Communication. New York, NY: Routledge, 2011 [Google Scholar]
- 11.Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med 2007; 45:107-14; PMID:17628649; http://dx.doi.org/ 10.1016/j.ypmed.2007.05.013 [DOI] [PubMed] [Google Scholar]
- 12.Fu LY, Bonhomme LA, Cooper SC, Joseph JG, Zimet GD. Educational interventions to increase HPV vaccination acceptance: a systematic review. Vaccine 2014; 32:1901-20; PMID:24530401; http://dx.doi.org/ 10.1016/j.vaccine.2014.01.091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jung M, Lin L, Viswanath K. Associations between health communication behaviors, neighborhood social capital, vaccine knowledge, and parents' H1N1 vaccination of their children. Vaccine 2013; 31:4860-6; PMID:23954379; http://dx.doi.org/ 10.1016/j.vaccine.2013.07.068 [DOI] [PubMed] [Google Scholar]
- 14.Small SL, Sampselle CM, Martyn KK, Dempsey AF. Modifiable influences on female HPV vaccine uptake at the clinic encounter level: a literature review. J Am Assoc Nurse Pract 2013; 26:519-25; PMID:24170346 [DOI] [PubMed] [Google Scholar]
- 15.Viswanath K, Nagler RH, Bigman-Galimore CA, McCauley MP, Jung M, Ramanadhan S. The communications revolution and health inequalities in the 21st century: implications for cancer control. Cancer Epidemiol Biomarkers Prev 2012; 21:1701-8; PMID:23045545; http://dx.doi.org/ 10.1158/1055-9965.EPI-12-0852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brewer NT, Gottlieb SL, Reiter PL, McRee AL, Liddon N, Markowitz L, Smith JS. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis 2011; 38:197-204; PMID:20838362; http://dx.doi.org/ 10.1097/OLQ.0b013e3181f12dbf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gargano LM, Herbert NL, Painter JE, Sales JM, Morfaw C, Rask K, Murray D, DiClemente RJ, Hughes JM. Impact of a physician recommendation and parental immunization attitudes on receipt or intention to receive adolescent vaccines. Hum Vaccin Immunother 2013; 9:2627-33; PMID:23883781; http://dx.doi.org/ 10.4161/hv.25823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guerry SL, De Rosa CJ, Markowitz LE, Walker S, Liddon N, Kerndt PR, Gottlieb SL. Human papillomavirus vaccine initiation among adolescent girls in high-risk communities. Vaccine 2011; 29:2235-41; PMID:21288799; http://dx.doi.org/ 10.1016/j.vaccine.2011.01.052 [DOI] [PubMed] [Google Scholar]
- 19.Winston CA, Wortley PM, Lees KA. Factors associated with vaccination of medicare beneficiaries in five U.S. communities: Results from the racial and ethnic adult disparities in immunization initiative survey, 2003. J Am Geriatr Soc 2006; 54:303-10; PMID:16460383; http://dx.doi.org/ 10.1111/j.1532-5415.2005.00585.x [DOI] [PubMed] [Google Scholar]
- 20.Gnanasekaran SK, Finkelstein JA, Hohman K, O'Brien M, Kruskal B, Lieu T. Parental perspectives on influenza vaccination among children with asthma. Public Health Rep 2006; 121:181-8; PMID:16528952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma KK, Schaffner W, Colmenares C, Howser J, Jones J, Poehling KA. Influenza vaccinations of young children increased with media coverage in 2003. Pediatrics 2006; 117:e157-63; PMID:16452325; http://dx.doi.org/ 10.1542/peds.2005-1079 [DOI] [PubMed] [Google Scholar]
- 22.Griffioen AM, Glynn S, Mullins TK, Zimet GD, Rosenthal SL, Fortenberry JD, Kahn JA. Perspectives on decision making about human papillomavirus vaccination among 11- to 12-year-old girls and their mothers. Clin Pediatr (Phila) 2012; 51:560-8; PMID:22589477; http://dx.doi.org/ 10.1177/0009922812443732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelly BJ, Leader AE, Mittermaier DJ, Hornik RC, Cappella JN. The HPV vaccine and the media: how has the topic been covered and what are the effects on knowledge about the virus and cervical cancer? Patient Educ Couns 2009; 77:308-13; PMID:19395221; http://dx.doi.org/ 10.1016/j.pec.2009.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daley MF, Crane LA, Chandramouli V, Beaty BL, Barrow J, Allred N, Berman S, Kempe A. Influenza among healthy young children: changes in parental attitudes and predictors of immunization during the 2003 to 2004 influenza season. Pediatrics 2006; 117:e268-77; PMID:16452334; http://dx.doi.org/ 10.1542/peds.2005-1752 [DOI] [PubMed] [Google Scholar]
- 25.Daley MF, Crane LA, Chandramouli V, Beaty BL, Barrow J, Allred N, Berman S, Kempe A. Misperceptions about influenza vaccination among parents of healthy young children. Clin Pediatr (Phila) 2007; 46:408-17; PMID:17556737; http://dx.doi.org/ 10.1177/0009922806298647 [DOI] [PubMed] [Google Scholar]
- 26.Hilyard KM, Quinn SC, Kim KH, Musa D, Freimuth VS. Determinants of parental acceptance of the H1N1 vaccine. Health Educ Behav 2013; 41:307-14; PMID:24369176; http://dx.doi.org/ 10.1177/1090198113515244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mok E, Yeung SH, Chan MF. Prevalence of influenza vaccination and correlates of intention to be vaccinated among Hong Kong Chinese. Public Health Nurs 2006; 23:506-15; PMID:17096775; http://dx.doi.org/ 10.1111/j.1525-1446.2006.00590.x [DOI] [PubMed] [Google Scholar]
- 28.O'Connor AM, Stacey D, Entwistle V, Llewellyn-Thomas H, Rovner D, Holmes-Rovner M, Tait V, Tetroe J, Fiset V, Barry M, et al.. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2003:CD001431. [DOI] [PubMed] [Google Scholar]
- 29.`Sales JM, Painter JE, Pazol K, Gargano LM, Orenstein W, Hughes JM, DiClemente RJ. Rural parents' vaccination-related attitudes and intention to vaccinate middle and high school children against influenza following educational influenza vaccination intervention. Hum Vaccin 2011; 7:1146-52; PMID:22048112; http://dx.doi.org/ 10.4161/hv.7.11.17891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sturm LA, Mays RM, Zimet GD. Parental beliefs and decision making about child and adolescent immunization: from polio to sexually transmitted infections. J Dev Behav Pediatr 2005; 26:441-52; PMID:16344662; http://dx.doi.org/ 10.1097/00004703-200512000-00009 [DOI] [PubMed] [Google Scholar]
- 31.Herbert NL, Gargano LM, Painter JE, Sales JM, Morfaw C, Murray D, Diclemente RJ, Hughes JM. Understanding reasons for participating in a school-based influenza vaccination program and decision-making dynamics among adolescents and parents. Health Educ Res 2013; 28:663-72; PMID:23727620; http://dx.doi.org/ 10.1093/her/cyt060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Claudio L, Stingone JA. Improving sampling and response rates in children's health research through participatory methods. J Sch Health 2008; 78:445-51; PMID:18651932; http://dx.doi.org/ 10.1111/j.1746-1561.2008.00328.x [DOI] [PubMed] [Google Scholar]
- 33.Ji PY, Pokorny SB, Jason LA. Factors influencing middle and high schools' active parental consent return rates. Eval Rev 2004; 28:578-91; PMID:15486162; http://dx.doi.org/ 10.1177/0193841X04263917 [DOI] [PubMed] [Google Scholar]
- 34.McMorris BJ, Clements J, Evans-Whipp T, Gangnes D, Bond L, Toumbourou JW, Catalano RF. A comparison of methods to obtain active parental consent for an international student survey. Eval Rev 2004; 28:64-83; PMID:14750292; http://dx.doi.org/ 10.1177/0193841X03257532 [DOI] [PubMed] [Google Scholar]
- 35.Shih TH, Fan X. Comparing response rates from web and mail surveys: a meta-analysis. Field Methods 2008; 20:249-71; http://dx.doi.org/ 10.1177/1525822X08317085 [DOI] [Google Scholar]
- 36.Abraham KG, Maitland A, Bianchi SM. Nonresponse in the American time use survey: who is missing and how much does it matter. Public Opin Q 2006; 70:676-703; http://dx.doi.org/ 10.1093/poq/nfl037 [DOI] [Google Scholar]
- 37.Keeter S, Kennedy C, Dimock M, Best J, Craighill P. Gauging the impact of growing nonresponse on estimates from a National RDD Telephone Survey. Public Opin Q 2006; 70:759-79; http://dx.doi.org/ 10.1093/poq/nfl035 [DOI] [Google Scholar]
- 38.Choung RS, Locke GR, Schleck CD, Ziegenfuss JY, Beebe TJ, Zinsmeister AR, Talley NJ. A low response rate does not necessarily indicate non-response bias in gastroenterology survey research: a population-based study. J Public Health 2013; 21:87-95; http://dx.doi.org/ 10.1007/s10389-012-0513-z [DOI] [Google Scholar]
- 39.Gargano LM, Herbert NL, Painter JE, Sales JM, Vogt TM, Morfaw C, Jones LM, Murray D, DiClemente RJ, Hughes JM. Development, theoretical framework, and evaluation of a parent and teacher-delivered intervention on adolescent vaccination. Health Promot Pract 2014; 15:556-67; PMID:24440920; http://dx.doi.org/ 10.1177/1524839913518222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis. New York, NY: The Guilford Press, 2013 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


