Abstract
Background
Cutaneous leishmaniasis (CL) is a vector-mediated skin disease, characterized by chronic wounds on the skin and caused by macrophages in protozoan parasites. It is an endemic disease in the southern and southeastern Anatolia region and is still an important public health problem in Turkey. Because of the civil war in Syria, immigrants to this region in the last 3 years have begun to more frequently present with this disease. The aim of this study was to draw attention to the dramatic increase in new cases with CL after the beginning of the civil war in Syria.
Material/Methods
In this retrospective study, we evaluated demographic, epidemiological, and clinical features of 110 patients diagnosed with cutaneous leishmaniasis who were admitted to the Department of Dermatology at Kahramanmaras Sutcu Imam University Faculty of Medicine between January 2011 and June 2014.
Results
A total of 110 patients included in the study; 50 (45%) were males, and 60 (55%) were females. The age range of the study group was 1–78 years, and the infection was more prevalent in the 0–20 year age group. Of these patients, 76 (69%) were Syrian refugees living in tent camps and 34 (31%) were Turkish citizens. The majority of the cases were diagnosed between October and December.
Conclusions
Immigrations to endemic regions of Turkey from neighbouring countries where CL incidence is higher may lead to large increases in case numbers. In order to decrease the risk of exposure, housing conditions of the refugees must be improved, routine health controls must be performed, effective measures must be set in place for vector control, and infected individuals must be diagnosed and treated to prevent spread of the infection.
Keywords: Epidemiology; Leishmaniasis, Cutaneous; Turkey
Background
Cutaneous leishmaniasis (CL) is a vector-transmitted skin disease caused by an obligate intra-macrophage protozoan parasite, and the infection causes the development of atrophic cicatrice and malformation [1,2]. This infection has been known in Turkey for centuries, and it is also locally called Urfa sore, Antep sore, Halep sore, or oriental sore. In Turkey, more than 98% of all cases of CL are reported from 7 cities located in the south and south-east regions: Şanlıurfa, Diyarbakır, Adana, Osmaniye, Kahramanmaraş, Hatay, and İçel [3]. According to recent data of the Ministry of Health of Turkey, there is a tendency towards an increase in the prevalence of CL [4], and the refugees fleeing from Syria due to civil war have been reported as the main cause of this increase [5,6].
The present study evaluated the current status of CL in our region (southeastern Anatolia, Turkey), the prevalence of which is on the rise in association with population movement in recent years. For this purpose, we reviewed the epidemiological and clinical features of 110 patients who were admitted to the Department of Dermatology at Kahramanmaras Sutcu Imam University Faculty of Medicine between January 2011 and June 2014 and who were subsequently diagnosed with CL. The aim of the study was to draw attention to the dramatic increase in the number of new cases of CL in our region after the beginning of the civil war in Syria.
Material and Methods
The present study retrospectively evaluated 110 patients who were admitted to the Department of Dermatology at Kahramanmaras Sutcu Imam University Faculty of Medicine between January 2011 and June 2014 and who were subsequently diagnosed with CL based on the clinical features, tissue smear, and histopathological examination, if necessary. The cases were evaluated in terms of age, sex, clinical features of the lesions, localization, presence of single or multiple lesions, seasonal distribution, and sites of initial presentation. The chi-square test was used in statistical analysis. A p value <0.05 was considered statistically significant.
Results
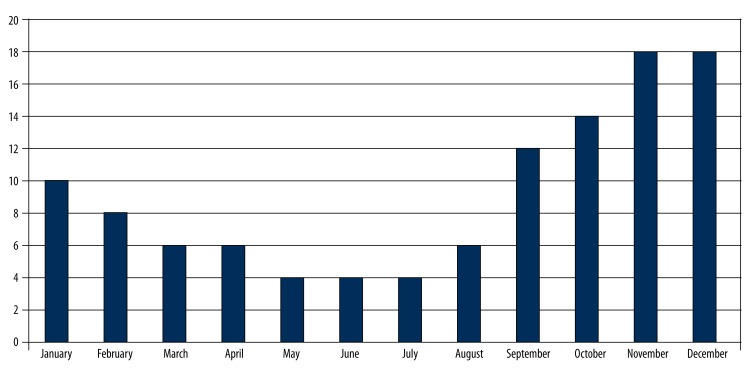
Of 110 patients included in the study, 50 (45%) were males, and 60 (55%) were females, and there was no significant difference between the two groups in terms of gender (p>0.05). The age range of the study group was 1–78 years, the infection was more prevalent in the 0–20 year age group (52.7%), and the prevalence rate was significantly higher compared to other age groups (p<0.05) (Table 1). The lesions were located on the face in 79 cases (72%), the hands and arms in 38 cases (35%), feet and legs in 13 cases (12%), and back and abdomen in 4 cases (4%). Of these cases, 77 (70%) had a single lesion and 33 patients (30%) had multiple lesions (Table 1). The number of lesions ranged between 1 and 12, and the mean number of lesions per patient was 2.14. The size of the lesions ranged from 0.5 cm to 8.5 cm, and the mean lesion size was 3.7±2.9 cm. The noduloulcerative lesions were the most common form of lesions, occurring in 59 cases (54%), whereas papulonodular lesion occurring in 47 cases (43%) and vegetative lesions occurring in 4 cases (4%) were less common lesions (Figures 1, 2). The duration of lesions was a minimum of 1 month and a maximum of 19 months as reported by the patients. When the annual distribution of the cases was evaluated, 9 cases occurred in 2011, 11 cases occurred in 2012, 58 cases occurred in 2013, and 32 cases were diagnosed in the first 6 months of 2014 (Table 2). Of these patients, 76 (69%) were Syrian refugees living in the tent camps in Turkish towns after fleeing from the civil war, and 34 (31%) were Turkish citizens living in Kahramanmaraş city center, villages close to the city center, and other districts located close to the Syrian border (Table 2). Cases were diagnosed most frequently between October and December (Figure 3).
Table 1.
The distribution of cutaneous leishmaniasis cases by age, sex and number of lesions.
| Age group (year) | Sex | Number of lesion | ||
|---|---|---|---|---|
| Female (%) | Male (%) | Single lesion (%) | Multiple lesions (%) | |
| 0–20 | 30 (27) | 28 (26) | 18 (16) | 40 (36) |
| 20–40 | 10 (9) | 6 (5) | 4 (4) | 12 (11) |
| ≥40 | 20 (19) | 16 (14) | 11 (10) | 25 (23) |
| Total | 60 (55) | 50 (45) | 33 (30) | 77 (70) |
Figure 1.

Multiple papulonodular lesions in the right cheek of a 11-year-old Syrian boy diagnosed with cutaneous leishmaniasis.
Figure 2.

(A) Multiple papulonodular lesions with sporotrikoid pattern extending from the right fifth finger to arm in a 48 -year-old Syrian woman diagnosed with cutaneous leishmaniasis. (B) Significant clinical healing was observed after a single dose injection of intralesional meglumine antimonate in the same patient.
Table 2.
The distribution of cutaneous leishmaniasis cases by year and ethnicity.
| Year | Domestic | Syrian refugees | Total |
|---|---|---|---|
| 2011 | 9 | 0 | 9 |
| 2012 | 10 | 1 | 11 |
| 2013 | 9 | 49 | 58 |
| 2014 (first six months) | 6 | 26 | 32 |
Figure 3.
The distribution of leishmaniasis cases in terms of months.
Discussion
Cutaneous leishmaniasis is an infectious disease caused by the leishmania parasite and occurring in mammalian hosts after the bite of an infected sand fly. The infection is transmitted by the bite of a female phlebotomine sand fly, which has more than 500 species identified to date. Dogs, coyotes, and foxes serve as reservoirs of infection. The causative parasite is found in amastigote form (without a flagellum) in humans and other mammalians and in promastigote form (with a flagellum) in the sand fly, which serve as the intermediate host of infection [1].
The initial lesions appear as erythematous papules on the exposed body sites such as face and extremities and become nodular crusted lesions. When the surface of the crusted lesion is removed, horny processes are observed projecting from the under-surface of a crust, and this is referred to as “tin-tack” sign (signe de clou) (Figure 4). The papules and nodules become ulcerated over time or heal leaving an atrophic scar without ulceration. The infection can cause subcutaneous nodules arranged in a linear pattern as a result of lymphatic dissemination of the parasite, which is a rare occurrence called a sporotrichoid pattern. Pentavalent antimony compounds such as meglumine antimoniate and sodium stibogluconate are first-line treatment options. The intralesional administration of pentavalent antimony compounds was used in our cases. Only 4 patients with multiple lesions were admitted to the hospital for intramuscular administration of the treatment.
Figure 4.

After removing of the crust of the leishmaniasis lesion, “tin-tack” sign was seen over the wound (sign de clou).
Cutaneous leishmaniasis can occur at all ages and in both sexes; however, the infection is more common in children and young adults [1,2]. In a study by Oliveria et al., conducted in 2 different locations in Mali, 75% of the cases were younger than 30 years of age [7]. In a large series of 1880 patients reported by Douba et al. from Aleppo, Syria, 80% of the patients newly diagnosed with CL were below 16 years of age [8]. In 2 epidemiological studies conducted in 2 different locations in Turkey that allowed migration of large number of people fleeing from civil war in Syria, 52% and 60% of the patients were under 20 years of age, respectively [5,6]. Consistent with the literature, 52.7% of the patients in the present study were under 20 years of age. This finding reflects insufficient hygiene practices in this age group and more frequent exposure to sand fly bites due to more frequent participation in outdoor and rural activities. The lower prevalence rate in older people may be due to acquired immunity from exposure to the vector at an early age.
Many studies did not report a significant difference in terms of sex distribution in CL [1,2,7,9], similar to our study; however, the present study reported a higher number of female than male patients. Most of the patients diagnosed with CL were Syrian refugees, and the majority of males in this particular population remained in their home country or died in the civil war, and the immigrants were mostly women. Although the infection can occur in all seasons, higher prevalence rates have been reported in the autumn months following the warm months of summer [9,10]. In a study by Uzun et al. that was conducted in the territory of Adana, the highest number of cases were reported in October, November, and December [11]. Consistent with the literature, most cases occurred in October, November, and December in the present study, possibly because of people sleeping outside of their houses during the warm season between May and September, unhygienic housing for Syrian refugees in tent camps, and the large sand fly population. Most cases are diagnosed after an incubation periods of 2–3 months after the high-transmission period of the summer months.
Similar to most studies that were conducted in Turkey, the face was the most common site of involvement. The rate of multiple lesions was 30%, which was similar to that in previous studies, and the face was the most common site of involvement in most of these studies [1,9,12].
According to 2008 data of the World Health Organization (WHO), CL is reported from 82 countries, and 1.5 million new cases occur each year. Afghanistan, Sudan, Iran, Iraq, Saudi Arabia, Algeria, and South America account for 90% of all cases occurring in the world [13]. The development of resistance to insecticides by sand flies, leaving patients untreated, travel to endemic areas, and migrations play a role in increased prevalence of CL cases [1,3]. A total of 46 003 new cases were diagnosed in Turkey between 1990 and 2010. Of these cases, 96% were reported from Şanlıurfa, Adana, Osmaniye, Hatay, Diyarbakır, İçel, and Kahramanmaraş. The cases reported within this period from our province account for 2% of all cases [4]. Since the civil war in Syria began in April 2011, 200 386 Syrian citizens were placed in 20 tent camps as of August 23, 2013. These tent camps were constructed by the Prime Ministry Disaster and Emergency Management Authority (AFAD) for Syrian refugees fleeing from Syria due to war. It is known that approximately 350 000 Syrian refugees are living outside the camps in Turkey. In Kahramanmaraş, approximately 15 000 refugees are accommodated, which accounts for 7.5% of all refugees in Turkey [10]. Therefore, a dramatic increase in the number of cases with CL in our region is obviously attributable to the increasing number of Syrian refugees fleeing from highly endemic areas. During a period of more than 3 years, 67 patients who were Syrian refugees were diagnosed with and treated for CL. The number of cases might be higher considering admission of the patients to other health care units in our province.
The present study has some limitations. Firstly, the study was conducted on a relatively small number of patients based on the data of a single tertiary health care facility. In addition, the prevalence rate reported in the present study may not reflect the actual disease prevalence in our region because most Syrian refugees living in tent camps and Turkish citizens living in the rural areas experience difficulties in accessing health care services.
Conclusions
In conclusion, population movement and migration from neighboring counties with a high incidence for CL to an already endemic area for CL unfavorably affects the prevalence of CL in our region and increases the risk of exposure to this infection. In addition, it is obvious that CL might become a serious dermatological health problem in the near future because Syrian refugees, who were initially settled in tent camps close to the Syrian border and less often in the city center, began migrating to western and northern Anatolian territories. To decrease the risk of exposure, we suggest that housing conditions of the refugees coming from highly endemic areas must be improved, routine health controls must be implemented, effective measures must be set in place for vector control, and infected individuals must be diagnosed and treated to prevent spread of the infection.
Footnotes
Source of support: Departmental sources
References
- 1.Den Boer M, Argaw D, Jannin J, Alvar J. Leishmaniasis impact and treatment access. Clin Microbiol Infect. 2011;17:1471–77. doi: 10.1111/j.1469-0691.2011.03635.x. [DOI] [PubMed] [Google Scholar]
- 2.Gürel MS, Yeşilova Y, Ölgen MK, Özbel Y. Cutaneous leishmaniasis in Turkey. Turkiye Parazitol Derg. 2012;36:121–29. doi: 10.5152/tpd.2012.29. [DOI] [PubMed] [Google Scholar]
- 3.Ok UZ, Balcioğlu IC, Taylan Ozkan A, et al. Leishmaniasis in Turkey. Acta Trop. 2002;84:43–48. doi: 10.1016/s0001-706x(02)00134-1. [DOI] [PubMed] [Google Scholar]
- 4.The Statistics Department of Ministery of Health of Turkey. http://www.saglik.gov.tr.
- 5.Salman IS, Vural A, Unver A, Saçar S. Cutaneous leishmaniasis cases in Nizip, Turkey after the Syrian civil war. Mikrobiyol Bul. 2014;48:106–13. [PubMed] [Google Scholar]
- 6.Turhanoglu M, Alp Erdal S, Bayindir Bilman F. A nine-year evaluation of cutaneous leishmaniasis patients in Diyarbakir Training and ResearchHospital, Turkey. Mikrobiyol Bul. 2014;48:335–40. doi: 10.5578/mb.7265. [DOI] [PubMed] [Google Scholar]
- 7.Oliveira F, Doumbia S, Anderson JM, et al. Discrepant prevalence and incidence of Leishmania infection between two neighboring villages in Central Mali based on Leishmanin skin test surveys. PLoS Negl Trop Dis. 2009;3:e565. doi: 10.1371/journal.pntd.0000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Douba MD, Abbas O, Wali A, et al. Chronic cutaneous leishmaniasis, a great mimicker with various clinical presentations: 12 years experience from Aleppo. J Eur Acad Dermatol Venereol. 2012;26:1224–29. doi: 10.1111/j.1468-3083.2011.04266.x. [DOI] [PubMed] [Google Scholar]
- 9.Köktürk A, Baz K, Aslan G, et al. İçel’ de kutanöz leishmaniasisin durumu. T Parazitol Derg. 2002;26:367–69. [in Turkey] [Google Scholar]
- 10.Baz K, Köktürk A, Türsen U, et al. Anamur’ da kutanöz leishmaniasis. Türkiye Klinikleri Dahili Tıp Bilimleri Dermatoloji Dergisi. 2002;12:5–10. [in Turkey] [Google Scholar]
- 11.Uzun S, Uslular C, Yücel A, et al. Cutaneous leishmaniasis: evaluation of 3074 cases in the Çukurova region of Turkey. Br J Dermatol. 1999;140:347–50. doi: 10.1046/j.1365-2133.1999.02673.x. [DOI] [PubMed] [Google Scholar]
- 12.Koçarslan S, Turan E, Ekinci T, et al. Clinical and histopathological characteristics of cutaneous leishmaniasis in Sanliurfa City of Turkey including Syrian refugees. Indian J Pathol Microbiol. 2013;56:211–15. doi: 10.4103/0377-4929.120367. [DOI] [PubMed] [Google Scholar]
- 13.WHO. Report of the consultative meeting on cutaneous leishmaniasis Geneva, WHO Headquarters; 30 April to 2 May 2007; WHO/HTM/NTD/IDM/2008.7 http://www.who.int/leishmaniasis/resources/Cutaneous_leish_cm_2008.pdf. [Google Scholar]