Abstract
A cross-sectional study was performed to assess current public awareness of herpes zoster (HZ) and its vaccine, determine the factors that influence people's intention regarding HZ vaccination, and investigate the barriers for vaccination by changing decisions with sequential questions regarding knowledge, cost, and physician's recommendation in the Department of Infectious Diseases, Korea University Guro Hospital, in South Korea, between August 23 and September 15 of 2013. Among 603 subjects who completed the survey, 85.7% and 43.6% subjects were aware of HZ and HZ vaccination, respectively. Women, younger age group, those with higher income or higher education levels were more likely to be aware of HZ. Overall, 85.8% of subjects aware of HZ were willing to be vaccinated or vaccinate their parents. The main obstacles for the increased acceptance toward vaccination were the high cost and low perceived risk, which decreased acceptance to 60.2%. However, physician's recommendation reversed 69.5% of the refusal to accept HZ vaccine. These results indicate that expanding public education and physician's recommendations are important factors aimed at increasing HZ vaccine coverage rate.
Keywords: awareness, health surveys, health behavior, herpes zoster, vaccination
Abbreviations
- HZ
herpes zoster
- VZV
varicella zoster virus
- PHN
postherpetic neuralgia
- KUGH
Korea University Guro Hospital
- OR
odds ratio
- CI
confidence interval
- GEE
generalized estimating equation
Introduction
Herpes zoster (HZ) is a viral disease caused by the reactivation of latent varicella zoster virus (VZV) in the dorsal root ganglia, and is characterized by dermatomal vesicular rash and severe pain.1 Both the acute pain and its common complication, postherpetic neuralgia (PHN), significantly impair normal social functioning and reduce health-related quality of life.2-5 PHN when defined as pain that lasts more than 3 months after rash onset is estimated to occur in approximately 30% of subjects aged ≥70 y.6 Moreover, the incidence and severity of PHN increase with age.6,7
As HZ treatments, including oral antiviral agents, antidepressants/analgesics, anticonvulsants and corticosteroids, have not achieved satisfactory results, vaccination against HZ may be a good measure. Several large studies suggested that live-attenuated HZ vaccine could decrease the incidence of HZ and PHN by over 50% in adults aged >60 y.8,9 Besides, considering the high seroprevalence of VZV in the Korean population, more than 90% of subjects aged >11 y are at risk of developing HZ.10 Therefore, HZ vaccine is expected to decrease disease burden significantly regarding potential risk population in Korea and its high effectiveness.
Age-standardized incidence rates increase over time because HZ is closely associated with decreased cellular immunity.11-14 In 2040, the proportion of people aged ≥65 y is expected to reach 32.3%, which is about 3 times higher than the current proportion in South Korea and this trend has been observed in other countries too.15-17 Accordingly, HZ vaccination may play an important role in promoting healthy aging. In 2009, the Korean Ministry of Food and Drug Safety approved the live-attenuated HZ vaccine for people aged ≥60 y, and extended the age range to people aged ≥50 y in 2011; however, actual vaccine uptake by the population began in 2012.
The recommended immunizations for adult Koreans are provided by the Korea Centers for Disease Control and Prevention and the Korean Society of Infectious Diseases and include 5 vaccines for the general adult population: influenza vaccine, tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) or tetanus toxoid and reduced diphtheria toxoid vaccine (Td), pneumococcal vaccine, herpes zoster vaccine, and hepatitis A vaccine.18 Vaccine coverage rates are vary as follows: influenza, 33.5% (adults aged ≥19 y) and 77.4% (elderly aged ≥65 y) in the 2013–2014 season; and pneumococcus, 46.7% (elderly aged ≥65 y).19 Pneumococcal vaccines for the elderly aged ≥65 y and influenza vaccines for priority groups are administered without charge in 255 nationwide public health centers under the committed funding by central and local governments. All the other vaccines for adults are available in clinics and hospitals and paid out-of-pocket by the vaccinees. The current vaccination cost of HZ vaccine in Korea, including both the cost of the vaccine and its administration fee, is US $180–200 (US $1 = KR ₩1,000), which is approximately 0.7–0.8% of the average annual income of South Korean people (South Korean Gross domestic product per capita in 2014, US $24,328).20
Previous studies which were performed in other countries have indicated that the factors that influence awareness of HZ include the education level, race, history of HZ, or having witnessed someone with HZ.21-23 In one US study, the individual decision to be vaccinated was associated with awareness of the disease, personal risk assessment, and the physician's recommendation.24
The present study aimed to assess the current awareness of HZ and HZ vaccination as a function of age, gender, history of HZ, having witnessed someone with HZ, and socioeconomic status in Korea. Furthermore, we evaluated the factors that influence attitudes toward HZ vaccination, and investigated the barriers for vaccination by changing decisions with sequential conditions, knowledge, cost, and physician's recommendation.
Results
Study population. Among the 656 subjects invited to participate in the survey, 603 (91.9%) subjects responded. The most common reason for not participating was the lack of time to complete the survey. Among the respondents, 359 were aged ≥50 y and 244 were aged <50 y, comprising 271 men (44.9%) and 332 women (55.1%). The slightly higher predominance of women was the same in both age groups (Table 1). The respondents who completed the entire questionnaire totaled 472 (78.3%). The age distribution of respondents was as follows: 19–29 y (7.3%), 30–39 y (16.7%), 40–49 y (16.4%), 50–59 y (24.4%), 60–69 y (18.4%), and ≥70 y (16.8%).
Table 1.
Demographic characteristics of the subjects interviewed (N = 603)
| Aged ≥50 y | Aged 19–49 y | |||
|---|---|---|---|---|
| Total | (N = 359) | (N = 244) | p-value | |
| Gender | ||||
| Male | 271 (44.9%) | 158 (44.0%) | 113 (46.3%) | 0.577 |
| Female | 332 (55.1%) | 201 (56.0%) | 131 (53.7%) | |
| Mean number of y of education | ||||
| (mean ± SD) | 12.1 ± 4.0 | 10.4 ± 4.1 | 14.6 ± 2.2 | <0.001 |
| Mean level of income ($)* | 2934 ± 1750 | 2441 ± 1675 | 3640 ± 1608 | <0.001 |
| Presence of comorbidities | N/A | 160 (44.6%) | N/A | N/A |
| History of vaccination since adulthood | N/A | 246 (68.5%) | N/A | N/A |
* US $1 = KR ₩1,000.
N/A, not applicable; SD, standard deviation.
The average duration of education reported was 12.1 y, and the older group had a lower education level when compared with the younger group (10.4 ± 4.1 y vs. 14.6 ± 2.2 y, respectively, p <0.001). Most subjects aged ≥50 y (75.5%) had been educated beyond middle school and most subjects aged < 50 y (97.1%) had been educated beyond high school. In the latter, more than 50% reported having graduated from college (56.6%). Moreover, the mean monthly household income was lower in the older group when compared with the younger group (US $2,441 ± 1,675 vs. US $3,640 ± 1,608, respectively, p <0.001; Table 1). Approximately 50% of the older group reported having a monthly income of <US $2,000 (50.6%, 172/340) and 29.5% (72/244) of the younger group's monthly income exceeded US $5,000. More than 50% of the subjects aged ≥50 y had no comorbidities (56.9%, 199/350), and the most common comorbidity was diabetes (32.7%, 65/199). Regarding the vaccination history of subjects aged ≥50 y, 68.5% (246/359) respondents stated having received adulthood vaccines: seasonal influenza vaccine in the last influenza season (62.4%, 224/359), pneumococcal vaccine (19.8%, 71/359), and HZ vaccine (3.1%, 11/359).
Awareness of HZ and HZ vaccination. Overall, 85.7% (517/603) reported they had heard of HZ and 43.6% (225/516) were aware of HZ vaccination. Subjects aware of HZ were more likely to be women and younger, except for the group aged 20–29 y The frequency of subjects aware of HZ varied according to their education level: those who did not complete elementary school education (68.6%), those who completed elementary school (72.2%), those who completed middle school (85.1%), those who completed college (92.1%), and those who pursued university education (95.5%; p < 0.001). Subjects who reached higher education levels were more likely to be aware of HZ (p < 0.001, linear by linear test). Likewise, subjects with higher monthly income were generally more likely to be aware of HZ: monthly income of < US $2,000 (76.7%), US $2,000–2,999 (90.0%), US $3,000–3,999 (94.0%), US $4,000–4,999 (90.8%), and ≥US $5,000 (91.5%).
Most subjects who had heard of HZ were relatively well informed about HZ. For example, most of the subjects who stated they are aware of HZ knew that it accompanies pain (94.7%, 480/507) and that risk of HZ increases with age (77.5%, 385/497). The most common misunderstanding was that related to the belief that when HZ is treated, PHN can be prevented, of which the correct rate was 59.3% (293/494). When we scored each of the 5 questions, personal history of HZ or having witnessed someone with HZ was associated with increased awareness of HZ (3.84 vs. 3.57, n = 479, p = 0.02).
Most respondents aged ≥50 y who stated they were aware of HZ (80.1%, 237/296) believed they were unlikely or very unlikely to develop HZ in the future, and this belief was similar for men and women (p = 0.059). The perceived likelihood of being infected with HZ (likely or very likely) increased with age: 50–59 y, 17.3%; 60–69 y, 20.2%; and ≥70 y, 24.6%. The majority of respondents aged less than 50 y stated their parents were very unlikely or unlikely to develop HZ (77.9%, 169/217).
The self-reported prevalence of HZ was 19.6% (100/511) and increased with age. Subjects who had witnessed someone with HZ amounted to 67.8% (350/516). Less than 50% of the subjects (43.6%, 225/516) were aware of HZ vaccination and 40.1% of them (89/222) knew that the vaccine had been licensed for individuals aged ≥50 y (Table 2). Among subjects aged ≥50 y, 22.0% (33/150) stated that they had previously received a physician's recommendation of vaccination: subjects aged 50–59 y (15.2%, 10/66), 60–69 y (32.7%, 18/55) and ≥70 y (17.2% , 5/29)(p = 0.491).
Table 3.
Acceptance of HZ vaccination after specific conditions, stratified by epidemiologic characteristics
| Would you be vaccinated against HZ? (yes)† | After reading offered information, would you be vaccinated? (yes)† | Would you be vaccinated considering the present cost? (yes)† | Would you be vaccinated if your doctor recommended it? (yes)† | |
|---|---|---|---|---|
| Total§ | 440/513 (85.8%) | 471/512 (92.0%) | 306/513 (59.6%) | 443/510 (86.9%) |
| Age | ||||
| <50 y | 198 (90.4%)* | 211 (96.3%)* | 180 (82.2%)* | 210 (95.9%)* |
| 50–69 y | 190 (85.2%)* | 204 (91.5%)* | 108 (48.4%)* | 184 (83.3%)* |
| ≥70 y | 52 (73.2%)* | 56 (80.0%)* | 18 (25.4%)* | 49 (70.0%)* |
| Gender | ||||
| Male | 189 (87.5%) | 202 (92.7%) | 138 (63.0%) | 189 (87.1%) |
| Female | 251 (84.5%) | 269 (91.5%) | 168 (57.1%) | 254 (86.7%) |
| Education | ||||
| Incomplete high school education | 104 (78.2%)* | 112 (85.5%)* | 48 (36.6%)* | 97 (74.0%)* |
| College education | 333 (88.6%)* | 355 (94.2%)* | 254 (67.2%)* | 342 (91.2%)* |
| Monthly household income | ||||
| <US $5,000 | 325 (84.2%) | 352 (91.4%) | 212 (54.9%)* | 330 (85.9%) |
| ≥US $5,000 | 96 (90.6%) | 102 (95.3%) | 82 (76.6%)* | 98 (91.6%) |
| GEE (OR) [95% CI] | N/A | 2.08 [1.53–2.84] * | 0.10 [0.07–0.14] * | 5.91 [4.44–7.77] * |
* p < 0.05.
§Ninety subjects were excluded in this table due to missing values and the numbers are not consistent between questions as some interviewees did not complete the entire questionnaire.
GEE, generalized estimating equation; OR, odds ratio; CI, confidence interval; N/A, not applicable.
†For subjects aged <50 y, the questions were modified as “Would you allow HZ vaccination to your parents following condition?”
Table 2.
Self-reported history of HZ, having witnessed others with HZ, awareness of HZ, and awareness of HZ vaccination, according to age group
| Total | Aged ≥50 y | Aged 19–49 y | ||
|---|---|---|---|---|
| N (%) | n (%) | n (%) | p-value | |
| History of HZ | 100/511 (19.6%) | 72/293 (24.6%) | 28/218 (12.8%) | 0.001 |
| Had witnessed someone with HZ | 350/516 (67.8%) | 218/297 (73.4%) | 132/219 (60.3%) | 0.025 |
| Was aware of the HZ vaccine | 225/516 (43.6%) | 152/297 (51.2%) | 73/219 (33.3%) | 0.034 |
| Was aware that the HZ vaccine had been licensed for individuals aged ≥50 y* | 89/222 (40.1%) | 69/150 (46.0%) | 20/72 (27.8%) | 0.010 |
The total numbers are not consistent between questions as some interviewees did not complete the entire questionnaire.
* Subjects among those who were aware of HZ vaccine answered this question.
HZ, herpes zoster.
The source of information about HZ and its vaccine was different between the 2 age groups (p = 0.028). Older subjects aged ≥50 y reported having received information about HZ from relatives and friends (44.1%, 67/152) and mass media (42.8%, 65/152). By contrast, younger subjects reported that mass media was the main source of information about HZ (68.5%, 50/73). Only 17.8% (40/225) subjects reported they received information on HZ vaccination from physicians.
Attitude toward being vaccinated or vaccinating parents against HZ. In analysis of the attitude toward being vaccinated or vaccinating parents against HZ, subjects who had received HZ vaccination were excluded. Overall, 85.6% (507/592) subjects aware of HZ were willing to be vaccinated or vaccinate their parents against HZ. Among 284 subjects aged ≥50 y who were aware of HZ, personal history of HZ was not associated with a higher rate of willingness to be vaccinated (Odds Ratio [OR]: 0.737, 95% Confidence Interval [CI]: 0.397–1.371, p = 0.334). Likewise, having witnessed someone with HZ was not associated with a higher rate of willingness to be vaccinated (OR: 0.888, 95% CI: 0.461–1.711, p = 0.723). Subjects' willingness to be vaccinated showed no trend toward a higher self-reported rate of receiving the annual seasonal influenza vaccine (OR: 1.053, 95% CI: 0.553–2.004, p = 0.875).
The main reasons for not being vaccinated were associated with the low perceived risk of developing HZ (34.2%, 25/73), followed by concerns about the adverse effects following immunization (21.9%, 16/73), concerns about the vaccination cost (17.8%, 13/73), misconceptions about the belief that after being infected once, no further vaccination is required (15.1%, 11/73), fear of needles (8.2%, 6/73), lack of physician's recommendation of HZ vaccination (6.8%, 5/73), and uncertainty about the vaccine effectiveness (5.5%, 4/73). Some of those willing to be vaccinated or to allow vaccination of their parents responded the question about the reasons for refusal, which was 34 subjects aged ≥50 y and 11 subjects aged <50 y The main concern for subjects aged ≥50 y was the cost of vaccine (58.8%, 20/34) and that for subjects aged <50 y was lack of physician's recommendation (36.4%, 4/11) and adverse events following immunization (36.4%, 4/11).
Willingness to be vaccinated or to accept parents' vaccination against HZ was evaluated by dividing the subjects into 4 groups according to age group and awareness of HZ (Figs. 1 and 2). At each stage of sequential questions, willingness to accept vaccination according to the conditions, which are knowledge, cost and physician's recommendation, and how prior responses affected the next questions ware analyzed.
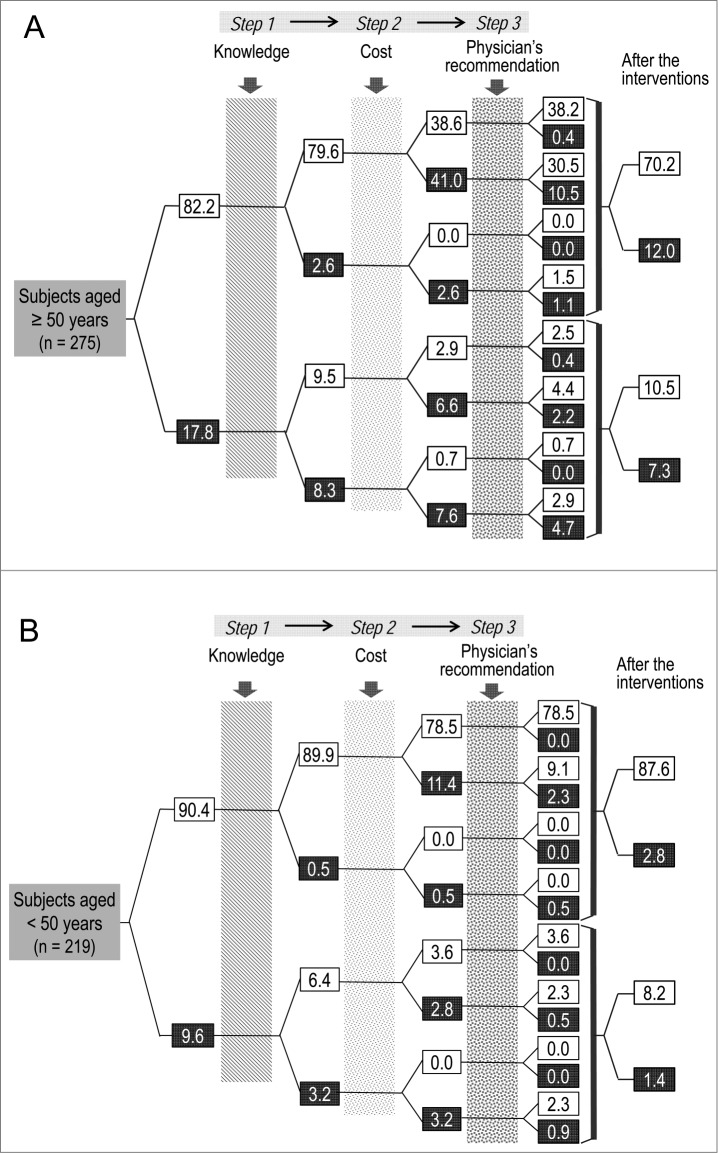
Figure 1.
Impact of knowledge, cost, and physician's recommendation on the intention to be vaccinated (A), or allowing parents to be vaccinated (B) against HZ among subjects who had heard of HZ (1A, subjects aged ≥50 y; 1B, subjects aged 19–49 y). Numbers in white boxes indicate the percentage of subjects who mentioned that they would be vaccinated or allow their parents to be vaccinated against HZ and those in black boxes indicate the percentage of subjects who mentioned that they would not be vaccinated or not allow their parents to be vaccinated against HZ. HZ, herpes zoster.
Among subjects aged ≥50 y who were aware of HZ (n = 275), 82.2% stated they were willing to be vaccinated against HZ initially (Fig. 1A). Increased knowledge about HZ and its vaccination reversed 53.4% (9.5%/17.8%) of initial refusal to be vaccinated. However, 53.4% (47.6%/89.1%) of the subjects who had intention to be vaccinated after having knowledge about HZ vaccination refused to be vaccinated when informed about the cost of the HZ vaccine. Meanwhile, among those not willing to be vaccinated following increased knowledge about HZ and information of cost, 68.0% (39.3%/57.8%) of the subjects stated that they would accept vaccination after the physician's recommendation.
Among subjects aged <50 y who have heard of HZ (n = 219), 90.4% stated they were willing to allow vaccination of their parents (Fig. 1B). Knowledge about HZ and its vaccine reversed 66.7% (6.4%/9.6%) of refusal to give vaccination to their parents. Those who refused vaccination because of the cost amounted to 14.2% (11.4% + 2.8%). Physicians' recommendation reversed 76.5% (13.7%/17.9%) of total refusal after receiving knowledge and information about cost.
Overall, the high cost decreased the acceptance of vaccination; however, physician's recommendation restored this acceptance. Among subjects aged <50 y, with adequate knowledge of the HZ and its vaccine, cost, and physician's recommendation, the acceptance proportion increased from 90.4% to 95.8% though cost dropped it significantly. This is comparable with decrease from 82.2% to 80.7% among subjects aged ≥50 y who were aware of HZ were willing to be vaccinated.
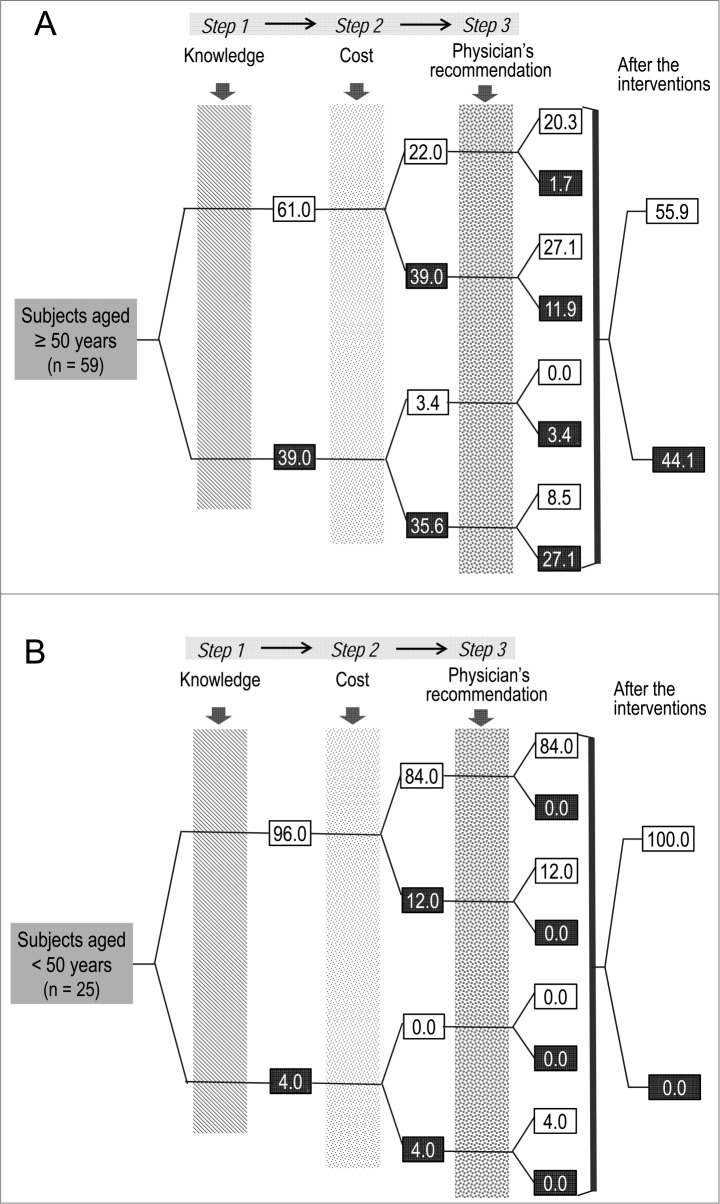
Those who had never heard about HZ initially were 59 subjects aged ≥50 y and 25 subjects aged <50 y (Fig. 2A and 2B). When given knowledge, 61.0% and 96.0% stated they would accept HZ vaccine respectively and following information about cost, total acceptance decreased to 25.4% and 84.0%. Among subjects aged ≥50 y and <50 y who initially accepted HZ vaccine after receiving knowledge, 63.9% (39.0%/61.0%) and 12.5% (12.0%/96.0%) turned their intention not to be vaccinated respectively; following physicians' recommendation, 47.7% and 100% of the refusal respectively.
Figure 2.
Impact of knowledge, cost, and physician's recommendation on the intention to be vaccinated (A), or allowing parents to be vaccinated (B) against HZ among subjects who had never heard of HZ (2A, subjects aged ≥50 y; 2B, subjects aged 19–49 y). Numbers in white boxes indicate the percentage of subjects who mentioned that they would be vaccinated or allow their parents to be vaccinated against HZ and those in black boxes indicate the percentage of subjects who mentioned that they would not be vaccinated or not allow their parents to be vaccinated against HZ. HZ, herpes zoster.
For the model analysis with Generalized Estimating Equation (GEE) to evaluate the factors that influence intention, only the respondents who answered all the 4 questions (initial willingness, awareness of HZ, cost, and physicians' recommendation) without history of HZ vaccination were included. After correction for gender, age, education level, and monthly household income, the perceived risk of HZ and benefit of HZ vaccination had a positive effect on willingness (OR: 2.08, 95% CI: 1.53–2.84, p <0.001). Awareness of the vaccination cost had a negative effect on willingness (OR: 0.10, 95% CI: 0.07–0.14, p <0.001), and the physician's recommendation increased willingness significantly (OR: 5.91, 95% CI: 4.44–7.77, p < 0.001).
In the final question, "Would you seek more information about a new vaccine that could prevent HZ if one were available?,” 54.2% subjects answered this question affirmatively and younger subjects were more likely to do so (those aged ≥50 y: 41.2% [148/359] and those aged <50 y: 73.4% [179/244], p <0.001).
Discussion
This study indicates the current public awareness of HZ and HZ vaccine, attitudes toward vaccination, and obstacles for increasing HZ vaccine uptake. The awareness of HZ among subjects varied markedly according to the country (17%–100%), and a global survey performed in 2006 indicated that 51% of Korean participants were aware of HZ.23 In the present study, most subjects were aware of HZ and were relatively well informed about the disease, especially women, younger adults, subjects with higher educational level and higher monthly household income. Furthermore, our study highlights that, notwithstanding the efficacy and effectiveness of HZ vaccine confirmed in several large clinical studies, awareness of HZ vaccination is not sufficient.
We could estimate the impacts of several factors that contribute to the intention to be vaccinated or vaccinate parents against HZ using sequential questions. Overall, 82.2% subjects aged ≥50 y who have heard of HZ were initially willing to be vaccinated; however, after getting knowledge about HZ and its vaccination and being aware of the cost, this percentage decreased to 42.2% and the cost of vaccination was an influential factor to drop the intention. However, physician's recommendation restored this percentage to 80.7%. For subjects aged <50 y, 90.4% initially accepted the vaccination of their parents; however, after getting information about HZ and being aware of the cost, this percentage decreased to 82.1%. These results demonstrate high demand of HZ vaccination in Korean people and underscore the negative effect of the cost and the significant positive effect of the physician's recommendation on subjects' willingness to be vaccinated.
Low vaccination rates may be the result of the lack of patient education and physician's recommendation. In one US study, 95% healthcare providers strongly recommended influenza and pneumococcal vaccines to eligible subjects; however, 88% recommended HZ vaccination, and only 41% strongly recommended it.25 In addition, the perceived risk of HZ, benefits of HZ vaccination, and physician's recommendation positively affected the vaccination rate.24 In the present study, physician's recommendation reversed the unwillingness to be vaccinated in 68.0% among subjects aged ≥50 y and 76.5% among subjects aged <50 y respectively, suggesting that the physician's recommendation may overcome the burden of vaccination cost.
HZ vaccine is one of the most expensive vaccines recommended for adults. Although the incidence and severity of HZ increase with age, the awareness of HZ and willingness to be vaccinated was lower among elderly population and the cost negatively influenced their willingness to be vaccinated. At present, HZ vaccine is not included in the national immunization program in Korea. Considering that financial factors were the most common barriers for HZ vaccination among older people, the inclusion of the vaccine into the program and a cost subsidy may help increase the vaccine coverage rate effectively, which has been observed during the pneumococcal vaccine implementation as part of the elderly immunization program against invasive pneumococcal diseases in Korea, 2013.
After people learnt about HZ and its vaccine, most of them were willing to be or to allow their parents vaccinated regardless of present status of awareness. Considering that mass media was the main source of information, they should convey accurate information about HZ and its vaccination to the public. Public awareness may be most efficiently promoted with education through media to increase HZ vaccination rates, particularly among older people and those with a low education level and low income.
We acknowledge that several limitations exist. First, the conditions that influenced the willingness to be vaccinated comprised sequential questions, which prevented the evaluation of the impact of each intervention separately. Second, this survey was performed in one hospital so it might not represent general Korean people. However, considering that behavioral patterns choosing hospital are not determined by region or economic status and accordingly, various groups of people visit tertiary teaching hospitals in Korea, the awareness and willingness presented in this study were assumed to be the same with the general Korean people. Lastly, this study design was simulation consisted of sequential questions according to our purpose and design and it might be different from the actual public behavior.
The HZ vaccine is a relatively new vaccine worldwide. At the early phase of introduction of a new vaccine, people are likely less aware of the vaccine and its cost may be high in most countries; thus people's acceptance of the vaccine is hindered.24,26 The recently developed vaccines, including human papillomavirus vaccines, have encountered similar public barriers.26 Accordingly, our study results would be useful as bases for developing strategies for introduction of new vaccines.
Considering the rapidly expanding elderly population, HZ will become increasingly important because of its prevalence in this population group. The major obstacles to increase HZ vaccination involve the cost, low perceived risk, and lack of knowledge of HZ and its vaccine. The promotion of both public education and the physicians' recommendation of vaccination may overcome these barriers considerably.
Patients and Methods
Study design. This cross-sectional study involved adults visited to the outpatient Department of Infectious Diseases in Korea University Guro Hospital (KUGH), South Korea, between August 23 and September 15 of 2013. KUGH is a tertiary teaching hospital that assists mainly the urban population. The research team members collected data from patients and their companions who visited the department. To avoid response bias, the members who conducted and assisted the survey were apart from relationship of doctor-patient or doctor-nurse and each participants received, read, and responded the questionnaires by themselves. Subjects eligible to participate in the study included those aged ≥50 y, or whose parents were aged ≥50 y and could be vaccinated. The groups were divided into 2 groups by age of 50 y, because the HZ vaccine has been approved for subjects aged ≥50 y in Korea. Two types of questionnaires were used: one was developed for subjects aged ≥50 y (Type A) and the other for subjects aged <50 y (Type B) (Appendix).
The current HZ vaccine is not indicated to adults aged <50 y; hence, they could not be surveyed for their willingness to be vaccinated, and their acceptance of their parents' HZ vaccination was surveyed instead. In accordance with the Confucian moral principles, Korean adults have a strong filial responsibility toward their parents. Accordingly, we assumed that their intention to accept vaccination for their parents is not just a recommendation but reflects their willingness to be vaccinated in the future. Therefore, our study results may not be exclusively confined to Korea in regards to the cultural phenomenon in which the unique parent-offspring interrelationship described earlier is evident.
The questionnaires were developed by the investigators on the basis of findings from previous studies (Appendix).21-25,27 The questionnaire referred to: (i) awareness of HZ, (ii) awareness of HZ vaccination, and (iii) behavioral factors that influence people's decisions to be vaccinated. We evaluated the change in willingness to be vaccinated using the following behavioral factors: awareness of the potential severity of HZ and efficacy of HZ vaccination, awareness of the cost of vaccination, and physician's recommendation of vaccination.
Basically, we designed the questionnaires in a way of that results could be utilized and interpreted in terms of public health intervention such as education on public and physicians. In addition, general process of accepting adult vaccination especially herpes zoster vaccination was in consideration. When someone gets aware of HZ through witnessing HZ patients or media, they may have interest and may search for the information about HZ and preventive measures. With relatively lower frequency, the physicians may have recommended HZ vaccination as it was recently licensed for use in Korea. We intended to measure the impact of knowledge and cost as well as physicians' recommendation at each moment which were the most important determinant factors in previous studies.24,25,27,28
With regards to the term, there is only one language used in Korea (Korean) and only one word indicating HZ (Dae-Sang-Po-Gin) that there was no miscommunication associated with terminology.23
Also, before the initiation of survey, a number of people with several different age group and educational level was asked to read and assess the questionnaires if there is anything difficult to understand.
Statistical analyses. The continuous variables were reported as mean ± standard deviation and analyzed using the unpaired 2-tailed t-test, and a value of p < 0.05 was considered significant. The self-reported prevalence of HZ, witnessing others with HZ, awareness of HZ, and awareness of HZ vaccination were reported as a function of age and socioeconomic status. The difference in the awareness of HZ according to demographic data was examined with the χ2-test. The factors that affected vaccination compliance—awareness of HZ, cost of its vaccination, and physician's recommendation—were examined by model analysis using the GEE method. All analyses were conducted using SAS software version 9.3 (SAS Institute, Cary, NC, USA).
Ethics statement. This study was approved by the Korea University's Institutional Review Board (Approval number: KUGH13104–001). A written informed consent form was signed by all participants.
Acknowledgments
The authors are grateful to Serl Hee Jang, Geum Mi Park, and Mi Young Kwon, who facilitated the performance of this study in the outpatient department.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Funding
This work was supported by a Korea University Guro Hospital grant (No. KUGH13104–001), underwritten by Merck Sharp & Dohme Corp. The organization funding this study had no role in the design and performance of the study; the collection, analysis, and interpretation of the data; or the preparation, review, and acceptance of the manuscript.
Appendix
Two types of questionnaires for survey on public awareness, attitudes and barriers for herpes zoster vaccination were used. One was developed for subjects aged 50 y (Type A) and the other for subjects aged <50 y (Type B).
References
- 1. Mandell GL, Bennett JE, Dolin R. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 7th ed Philadelphia: Churchill Livingstone/Elsevier; 2009. [Google Scholar]
- 2. Katz J, Cooper EM, Walther RR, Sweeney EW, Dworkin RH. Acute pain in herpes zoster and its impact on health-related quality of life. Clin Infect Dis 2004; 39:342-8; PMID:15307000; http://dx.doi.org/ 10.1086/421942 [DOI] [PubMed] [Google Scholar]
- 3. Chidiac C, Bruxelle J, Daures JP, Hoang-Xuan T, Morel P, Leplege A, El Hasnaoui A, de Labareyre C. Characteristics of patients with herpes zoster on presentation to practitioners in France. Clin Infect Dis 2001; 33:62-9; PMID:11389496; http://dx.doi.org/ 10.1086/320884 [DOI] [PubMed] [Google Scholar]
- 4. Oster G, Harding G, Dukes E, Edelsberg J, Cleary PD. Pain, medication use, and health-related quality of life in older persons with postherpetic neuralgia: results from a population-based survey. J Pain 2005; 6:356-63; PMID:15943957; http://dx.doi.org/ 10.1016/j.jpain.2005.01.359 [DOI] [PubMed] [Google Scholar]
- 5. Song H, Lee J, Lee M, Choi WS, Choi JH, Lee MS, Hashemi M, Rampakakis E, Kawai K, White R, et al. . Burden of illness, quality of life, and healthcare utilization among patients with herpes zoster in South Korea: a prospective clinical-epidemiological study. Int J Infect Dis 2014; 20:23-30; PMID:24412314; http://dx.doi.org/ 10.1016/j.ijid.2013.11.018 [DOI] [PubMed] [Google Scholar]
- 6. Helgason S, Petursson G, Gudmundsson S, Sigurdsson JA. Prevalence of postherpetic neuralgia after a first episode of herpes zoster: prospective study with long term follow up. BMJ 2000; 321:794-6; PMID:11009518; http://dx.doi.org/ 10.1136/bmj.321.7264.794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Choo PW, Galil K, Donahue JG, Walker AM, Spiegelman D, Platt R. Risk factors for postherpetic neuralgia. Arch Inter Med 1997; 157:1217-24; http://dx.doi.org/ 10.1001/archinte.1997.00440320117011 [DOI] [PubMed] [Google Scholar]
- 8. Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD, Arbeit RD, Simberkoff MS, Gershon AA, Davis LE, et al. . A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med 2005; 352:2271-84; PMID:15930418; http://dx.doi.org/ 10.1056/NEJMoa051016 [DOI] [PubMed] [Google Scholar]
- 9. Langan SM, Smeeth L, Margolis DJ, Thomas SL. Herpes zoster vaccine effectiveness against incident herpes zoster and post-herpetic neuralgia in an older US population: a cohort study. PLoS Med 2013; 10:e1001420; PMID:23585738; http://dx.doi.org/ 10.1371/journal.pmed.1001420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Choi WS, Noh JY, Huh JY, Jo YM, Lee J, Song JY, Kim WJ, Cheong HJ. Seroprevalence of varicella-zoster virus in Korea. J Med Virol 2010; 82:2123-6; PMID:20981803; http://dx.doi.org/ 10.1002/jmv.21917 [DOI] [PubMed] [Google Scholar]
- 11. Yih WK, Brooks DR, Lett SM, Jumaan AO, Zhang Z, Clements KM, Seward JF. The incidence of varicella and herpes zoster in Massachusetts as measured by the Behavioral Risk Factor Surveillance System (BRFSS) during a period of increasing varicella vaccine coverage, 1998-2003. BMC public Health 2005; 5:68; PMID:15960856; http://dx.doi.org/ 10.1186/1471-2458-5-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mullooly JP, Riedlinger K, Chun C, Weinmann S, Houston H. Incidence of herpes zoster, 1997-2002. Epidemiol Infect 2005; 133:245-53; PMID:15816149; http://dx.doi.org/ 10.1017/S095026880400281X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Choi WS, Noh JY, Huh JY, Jo YM, Lee J, Song JY, Kim WJ, Cheong HJ. Disease burden of herpes zoster in Korea. J Clin Virol 2010; 47:325-9; PMID:20181512; http://dx.doi.org/ 10.1016/j.jcv.2010.01.003 [DOI] [PubMed] [Google Scholar]
- 14. Arvin A. Aging, immunity, and the varicella-zoster virus. N Engl J Med 2005; 352:2266-7; PMID:15930416; http://dx.doi.org/ 10.1056/NEJMp058091. [DOI] [PubMed] [Google Scholar]
- 15. Statistics Korea Population Projections for Korea: 2010-2060. Deajeon: Statistics Korea; 2011 [Google Scholar]
- 16. Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States: Population Estimates and Projections. Washington: US. Census Bureau; 2014. Twenty-eight p. Report No.:P25-1140. [Google Scholar]
- 17. United Nations, Department of Economics and Social Affairs, Population Division World Population Ageing 2013. New York: United Nations; 2013. Report No.: ST/ESA/SER.A/348. [Google Scholar]
- 18. Korea Centers for Disease Control and Prevention Guidelines of Vaccination for Adult [Korean]. Cheongju: Korea Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 19. Korea Centers for Disease Control and Prevention Korea Health Statistics 2012: Korea National Health and Nutrition Examination Survey (KNHANES V-3) [Korean]. Cheongju: Korea Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 20. World Economic and Financial Surveys, World Economic Outlook Database [Internet] International Monetary Fund; October 2014 [cited 2014 Nov 24]. Available from: http://www.imf.org/external/pubs/ft/weo/2014/02/weodata/index.aspx. [Google Scholar]
- 21. Joon Lee T, Hayes S, Cummings DM, Cao Q, Carpenter K, Heim L, Edwards H. Herpes zoster knowledge, prevalence, and vaccination rate by race. J Am Board Fam Med 2013; 26:45-51; PMID:23288280; http://dx.doi.org/ 10.3122/jabfm.2013.01.120154 [DOI] [PubMed] [Google Scholar]
- 22. Javed S, Javed F, Mays RM, Tyring SK. Herpes zoster vaccine awareness among people >/= 50 years of age and its implications on immunization. Dermatol Online J 2012; 18:2; PMID:22948052 [PubMed] [Google Scholar]
- 23. Paek E, Johnson R. Public awareness and knowledge of herpes zoster: results of a global survey. Gerontology 2010; 56:20-31; PMID:19776543; http://dx.doi.org/ 10.1159/000240046 [DOI] [PubMed] [Google Scholar]
- 24. Lu PJ, Euler GL, Jumaan AO, Harpaz R. Herpes zoster vaccination among adults aged 60 years or older in the United States, 2007: uptake of the first new vaccine to target seniors. Vaccine 2009; 27:882-7; PMID:19071175; http://dx.doi.org/ 10.1016/j.vaccine.2008.11.077 [DOI] [PubMed] [Google Scholar]
- 25. Hurley LP, Lindley MC, Harpaz R, Stokley S, Daley MF, Crane LA, Dong F, Beaty BL, Tan L, Babbel C, et al. . Barriers to the use of herpes zoster vaccine. Ann Intern Med 2010; 152:555-60; PMID:20439573; http://dx.doi.org/ 10.7326/0003-4819-152-9-201005040-00005 [DOI] [PubMed] [Google Scholar]
- 26. Chow SN, Soon R, Park JS, Pancharoen C, Qiao YL, Basu P, Ngan HY. Knowledge, attitudes, and communication around human papillomavirus (HPV) vaccination amongst urban Asian mothers and physicians. Vaccine 2010; 28:3809-17; PMID:20347631; http://dx.doi.org/ 10.1016/j.vaccine.2010.03.027 [DOI] [PubMed] [Google Scholar]
- 27. Funovits AL, Wagamon KL, Mostow EN, Brodell RT. Refusal of shingles vaccine: implications for public health. J Am Acad Dermatol 2012; 66:1011-2; PMID:22583716; http://dx.doi.org/ 10.1016/j.jaad.2011.11.931 [DOI] [PubMed] [Google Scholar]
- 28. Opstelten W, van Essen GA, Hak E. Determinants of non-compliance with herpes zoster vaccination in the community-dwelling elderly. Vaccine 2009; 27:192-6; PMID:18996427; http://dx.doi.org/ 10.1016/j.vaccine.2008.10.047 [DOI] [PubMed] [Google Scholar]