Abstract
Sub-optimal vaccination coverage and recent outbreaks of vaccine-preventable diseases serve as a reminder that vaccine hesitancy remains a concern. ImmunizeCA, a new smartphone app to help track immunizations, may address several reasons for not vaccinating. We conducted a study to describe demographic variables, attitudes, beliefs and information sources regarding pediatric vaccination in a sample of childbearing women who were willing to download an immunization app. We also sought to measure their current mobile usage behaviors and determine if there is an association between participant demographics, attitudes, beliefs and information sources regarding pediatric vaccination and mobile usage. We recruited participants using a combination of passive and active methods at a tertiary care hospital in Ottawa, Canada. We used surveys to collect demographic information, examine attitudes, behavior, and information sources regarding immunization and self-reported mobile phone usage. A total of 54 women participated. The majority had positive attitudes toward vaccination (96%) and intended to vaccinate their children (98%). Participants were interested in information on pediatric vaccination (94%), and found information from public health the most reliable and accessible (78%). Participants also trusted immunization information from their doctor or nurse and public health (83%) more than other sources. There was variability in participant use of mobile apps for other purposes. The median participant mobile readiness score was 3.2. We found no significant associations between participant age, behavior and attitudes regarding vaccination and mobile readiness scores. This is the first evaluation of mobile readiness for a smartphone app to track immunizations. Our findings suggest that there exists an opportunity to provide reliable information on vaccination through mobile devices to better inform the public, however predictors of individual engagement with these technologies merits further study.
Keywords: attitudes and behaviors, immunization, knowledge, mobile technology, pediatric vaccination, vaccine hesitancy
Introduction
Technology and technological applications are increasingly being utilized in health care settings. For immunization, recall/reminder text messages have been successful in increasing coverage in both pediatric and adult populations.1 In addition, they are preferred by users over traditional reminder methods such as mail or phone 2 and can be simple, short, and personalized.2-4 Recall/reminders are relatively passive, offer cost effective scalability, and ease of customization based on age group, gender and medical condition. However, text messaging has character restrictions (∼160) and requires accurate contact information which can be challenging over time.1 Using contemporary methods such as email and smartphone applications (apps) offer the advantages of text messaging (scalability, low cost and automatic customization) while mitigating some of the challenges (stable form of contact and character limits).5 However, they may require more active engagement in order to achieve change and there exists a paucity of literature examining the effectiveness and acceptability of email reminders and smartphone applications to increase vaccination coverage.6
ImmunizeCA is a free smartphone app that permits Canadian users to track immunizations.7 Current adult and pediatric schedules are embedded allowing users to enter immunizations and the app creates a virtual immunization card which resembles the official paper record for each profile entered in the app. The app also has a reminder system, which can sync to the device's calendar app and creates custom notifications for upcoming or overdue immunizations. The app has direct links to Immunization Fact Sheets and information on vaccine-preventable disease (VPD) outbreaks, and has the ability to notify parents if their child is at risk.
Particularly in vulnerable infants, on-time vaccination is critical in preventing morbidity and mortality from VPDs. In general, factors known to inhibit on-time vaccination include: concerns about vaccine safety, which are increasingly disseminated via the Internet, challenges understanding the vaccination schedule, logistical issues related to attending vaccination appointments, and finally, the belief that vaccination is unnecessary because VPDs are rare.8 ImmunizeCA has features which address each of these factors and thus has the potential to impact vaccine hesitancy and on-time vaccination coverage.
However, the readiness of individuals to utilize a mobile app for interacting with personal health information, specifically, for tracking immunizations and accessing vaccine information remains uncertain. We are conducting an ongoing, longitudinal study to evaluate the impact of a smartphone mediated application in maternal adherence to on-time pediatric vaccination. As a necessary first step, we measured baseline immunization attitudes, information sources and mobile usage behaviors of a sample of childbearing women who were willing to download the app. Specifically, the objective of this study was to describe participant baselines attitudes, beliefs and information sources for pediatric vaccination and current mobile usage behavior. We also sought to determine if there is an association between vaccination attitudes, beliefs and mobile usage behavior.
Results
Characteristics of participants
A total of 54 women consented to participate and all completed the survey. 20% of participants were recruited through passive methods, and 80% were through active methods.
We had one individual who was interested in participating who was deemed ineligible due to her device (Blackberry Q10). An additional 5 individuals contacted research staff to participate and then were nonresponsive; they did not provide consent or fill out the survey.
The mean age of the study population was 31.8 years (Table 1). Over half (63%) of the participants were first-time mothers and 96% indicated they were married or in a common law relationship. Nearly all (93%) had completed a post-secondary diploma or degree. When asked to identify all of the type(s) of health care provider(s) mothers expected to be involved in their child's future health care, the majority selected family doctor or pediatrician (79% and 37% respectively). Over a quarter mentioned a non-physician and 33% reported planning to seek healthcare for their child from more than one provider.
Table 1.
Demographics of study participants
| Measure | All Participants n = 54 |
|---|---|
| Mean Age (SD) | 31.8 (4.6) |
| First Time mother, n (%) | |
| Yes | 34 (63.0) |
| No | 20 (37.0) |
| Number of previous children, n (%): | |
| 0 | 34 (63) |
| 1 | 15 (27.8) |
| 2 | 3 (5.6) |
| 3 | 2 (3.7) |
| Relationship Status, n (%): | |
| Married or common-law | 52(96.3) |
| Dating | 0(0.0) |
| Divorced/Separated | 0(0.0) |
| Single | 1(1.9) |
| Unanswered | 1(1.9) |
| I will seek health care for my child(ren) from the following sources, n(%): * | 43(79.6) |
| Family Doctor | |
| Pediatrician | 20(37.0) |
| Nurse Practitioner | 9(16.7) |
| Complementary and Alternative Medicine Provider | 5(9.3) |
| Multiple sources | 18(33.3) |
| Highest education level attained, n(%): | |
| <High School | 0(0.0) |
| High School | 1(1.9) |
| Some post-secondary | 3(5.6) |
| Community college/ technical school diploma | 8(14.8) |
| Undergraduate Degree | 21(38.9) |
| Graduate Degree | 21(38.9) |
| Current occupation status, n(%): | |
| Not employed outside of the home | 6(11.1) |
| Student | 1(1.9) |
| employed part-time | 4(7.4) |
| Employed Full-time | 40(74.1) |
| Self employed | 2(3.7) |
| Maternity leave | 2(3.7) |
| Self employed | 2(3.7) |
** Selections are not mutually exclusive and thus, may add to more than 100%.
Attitudes, beliefs and behaviors regarding vaccination
The vast majority of participants agreed or strongly agreed that vaccines prevent serious infectious diseases (96%), most agreed or strongly agreed that on-time vaccination was important for their child (86%), and 89% believed that other people's children should be vaccinated (Table 2). Over a quarter of respondents agreed or strongly agreed that the risk of vaccination outweighed the benefits (26%). When asked if vaccines were given at too young an age, 70% of participants disagreed or strongly disagreed. Nearly all participants agreed or strongly agreed that they planned on vaccinating their child (98%) (Table 2). Overall, 22% of participants agreed and nearly 10% neither agreed nor disagreed that they may forget their child's vaccination appointments. A larger proportion of first-time mothers (27%) agreed that they may forget their child's vaccination appointments, as compared to mothers of more than one child (15%).
Table 2.
Attitudes and Behavior and Information sources regarding vaccination
| Responses | ||||||
|---|---|---|---|---|---|---|
| Total Participants, n = 54 | ||||||
| Survey Questions | Missing | Strongly Disagree | Disagree | Neither agreenor disagree | Agree | Strongly agree |
| The risk of vaccination outweighs the benefits, n(%) | 0 (0.0) | 20 (37) | 17(31.5) | 3(5.6) | 2(3.7) | 12(22.2) |
| Vaccines prevent serious infectious diseases, n(%) | 0(0.0) | 0(0.0) | 0(0.0) | 2(3.7) | 16(29.6) | 36(66.7) |
| Vaccines cause disease, n(%) | 1(1.9) | 31(58.5) | 17(32.1) | 3(5.7) | 1(1.9) | 1(1.9) |
| Vaccines are given at too young an age, n(%) | 0(0.0) | 20(37.0) | 17(31.5) | 9(16.7) | 4(7.4) | 4(7.4) |
| I believe vaccinating on-time is important for my child's health, n(%) | 0(0.0) | 2(3.7) | 2(3.7) | 3(5.6) | 12(22.2) | 35(64.8) |
| I believe that other people's children should be vaccinated, n(%) | 0(0.0) | 0(0.0) | 0(0.0) | 6(11.1) | 20(37.0) | 28(51.9) |
| I plan to have my own child vaccinated, n(%) | 0(0.0) | 1(1.9) | 0(0.0) | 0(0.0) | 14(25.9) | 39(72.2) |
| I may forget my child's vaccination appointments, n(%) | 0(0.0) | 21(38.9) | 16(29.6) | 5(9.3) | 12(22.2) | 0(0.0) |
| I plan to use Complementary and Alternative Medicine for my child, n(%) | 0(0.0) | 9(16.7) | 13(24.1) | 22(40.7) | 9(16.7) | 1(1.9) |
| Reliable vaccination information is generally available and accessible, n(%) | 0(0.0) | 0(0.0) | 10(18.5) | 8(14.8) | 26(48.1) | 10(18.5) |
| Reliable vaccination information is available and accessible from Public Health, n(%) | 0(0.0) | 0(0.0) | 3(5.6) | 10(18.5) | 25(46.3) | 16(29.6) |
| Reliable vaccination information is available and accessible from the Internet, n(%) | 0(0.0) | 1(1.9) | 12(22.2) | 14(25.9) | 22(40.7) | 5(9.35) |
| Reliable vaccination information is available and accessible from Mobile Devices, n(%) | 1(1.9) | 1(1.9) | 8(15.1) | 26(49.1) | 15(28.3) | 3(5.7) |
| Reliable vaccination information is available from Complementary and Alternative Medicine providers, n(%) | 1(1.9) | 4(7.5) | 8(15.1) | 36(67.9) | 5(9.4) | 0(0.0) |
| I am interested in information about pediatric vaccinations, n(%) | 1(1.9) | 0(0.0) | 1(1.9) | 2(3.8) | 30(56.6) | 20(37.7) |
| I trust information from the Internet about pediatric vaccinations, n(%) | 0(0.0) | 0(0.0) | 19(35.2) | 28(51.9) | 7(13.0) | 0(0.0) |
| I trust information from my doctor or nurse about pediatric vaccinations, n(%) | 2(3.7) | 0(0.0) | 5(9.6) | 4(7.7) | 17(32.7) | 26(50.0) |
| I trust information from my Complementary and Alternative Medicine provider about pediatric vaccinations, n(%) | 0(0.0) | 6(11.1) | 10(18.5) | 30(55.6) | 7(13.0) | 1(1.9) |
| I trust information from Public Health about pediatric vaccinations, n(%) | 0(0.0) | 1(1.9) | 2(3.7) | 4(7.4) | 29(53.7) | 18(33.3) |
Information sources
When asked about the reliability and accessibility of pediatric vaccine information from various sources and which sources were most trusted, the majority of participants (92%) were very interested in information about pediatric vaccination (Table 2) and 66% agreed or strongly agreed it was generally available and accessible. Participants identified public health as the most reliable (76%) and trusted source (87%). Half of participants (50%) agreed or strongly agreed information is reliable and accessible on the Internet, while only a third (33%) of participants agreed or strongly agreed that information is reliable and accessible through mobile devices, while nearly half (49%) responded that they neither agreed nor disagreed with this statement.
Mobile device usage, mobile readiness scores and association with vaccination attitudes and behaviors
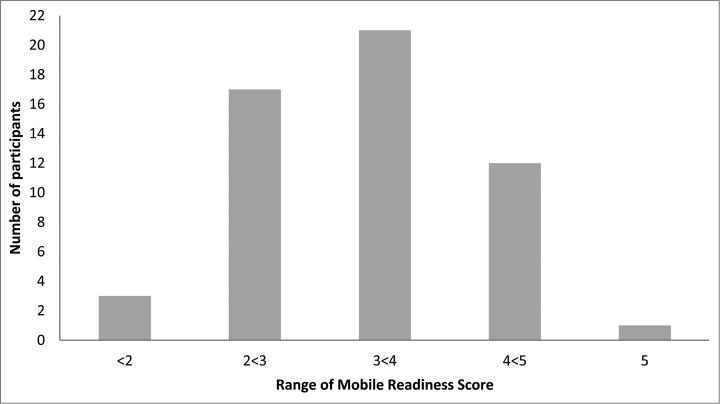
The vast majority (86%) of participants reported using apps on their smartphones regularly to obtain information (e.g. transit schedules, weather news) (Table 3). Organizational apps (such as scheduling, guides and planners) were also reported to be used by many participants (58% responded often or always). There was considerable variability in the responses about using smartphones to manage bank transactions (Table 3). Educational apps such as language learning programs were reportedly the least used, with just over a quarter of participants reporting using them often or always. Similarly, fitness and health apps were only reported to be used by 35% of participants. In total, we observed 21 different mobile readiness scores ranging from 1 to 5 (Fig. 1). The median was 3.2(IQR 1.2) with 21(38%) participants scoring between 3 and 4 on our scale.
Table 3.
Mobile Device Usage
| Responses | ||||||
|---|---|---|---|---|---|---|
| Total Participants, n = 54 | ||||||
| Missing | Never | Rarely | Often | Sometimes | Always | |
| Managing bank transactions, n(%) | 0(0.0) | 15(27.8) | 8(14.8) | 14(25.9) | 6(11.1) | 11(20.4) |
| Using information apps (train schedules, weather, news), n(%) | 0(0.0) | 1(1.9) | 1(1.9) | 20(37.0) | 7(13.0) | 25(46.3) |
| Using entertainment apps (gaming), n(%) | 1(1.9) | 9(17.0) | 12(22.6) | 12(22.6) | 10(18.9) | 10(18.9) |
| Using educational apps (language learning programs, reference works), n(%) | 0(0.0) | 14(25.9) | 13(24.1) | 11(20.4) | 13(24.1) | 3(5.6) |
| Using organizational apps (financial planning, voice recording, scheduling, nutritional guides), n(%) | 0(0.0) | 4(7.4) | 6(11.1) | 23(42.6) | 12(22.2) | 9(16.7) |
| Using fitness and/or health apps, n(%) | 0(0.0) | 10(18.5) | 14(25.9) | 15(27.8) | 11(20.4) | 4(7.4) |
Figure 1.
The distribution of participant mobile readiness scores (n = 54) calculated using the mean response to survey questions examining baseline mobile usage behavior outlined in Table 3.
In our posthoc analyses, we did not identify any significant associations between behaviors and attitudes about vaccination and the mobile readiness scores. There was no statistically significant linear correlation between participant age and mobile readiness score (p = 0.66). Mobile readiness scores were not significantly different between first-time mothers and mothers who had previous children (p = 0.37).
Discussion
Ensuring high on-time vaccination coverage is a priority for public health programs. This is particularly important with the re-emergence and transmission of VPDs such as measles and pertussis in developed countries and the continued transmission in developing countries. Vaccine hesitancy has been partly fuelled by anti-vaccinationists leveraging the Internet and social media to communicate their messages,9 individuals seeking information from sources such as the Internet and friends and family are predictive of intention to peruse an alternative immunization schedule.10 In addition, studies have shown that simply searching “vaccination” on the Internet yields up to 60% anti-vaccine content.11,12 In this study, although most of our study population viewed vaccination positively, was highly interested in information regarding pediatric vaccination, and used mobile devices regularly, more participants agreed that reliable vaccination information is available and accessible from the Internet than on mobile devices. We also found no evidence of association between attitudes or behavior toward vaccination and mobile device usage. We believe we have identified an opportunity to provide reliable and accessible immunization information through mobile devices. This may also present a novel mechanism for public health officials to circumvent the Internet and communicate directly with parents.13-15
While the opportunities posed by personal, mobile immunization records appear to be vast, they may only be realized if the public is receptive and the technology can achieve widespread adoption. In order to gauge readiness of individuals to utilize smartphones as a method of tracking immunizations, we reported on participant's current smartphone behaviors as a proxy for mobile readiness. The specific questions we used to assess mobile readiness reflected the 2 factors which were found to be highly predictive of technology readiness in the 2014 assessment of TRI construct validity: the number of online behaviors engaged in during the past year and the number of technology-oriented behaviors.16 These were reflected in the questions we asked participants regarding their mobile usage for other purposes (Table 3). These questions used to assess mobile readiness have not been used by others. The TRI, however, has been previously used in research by over 127 groups in 30 countries.16 In contrast to the homogeneity of vaccination attitudes, we observed a wide variety of mobile readiness scores (Fig. 1). This may be an important factor to consider, as individuals may not be equally likely to adopt an app, despite having uniform attitudes regarding vaccination. However, the predictive value of these questions will need to be further validated. TR may be an important predictor or technology-related behaviors, although data on its impact in the health care context is still scarce.17,18.
This study had several notable strengths. We captured participants during an important period to evaluate their attitudes toward vaccination, just prior or just after having a child. Another strength of this study was that all participants who consented to participate completed the survey. Our study is also, to the best of our knowledge, the largest sample of completed surveys related to a vaccination app, and the only evaluation of mobile readiness for a vaccine tracking app for smartphones.
Limitations of this study included the homogeneity in the responses related to vaccination attitudes, which suggests the sample is likely not representative of the general population. Our sample size also limited the power of the study to detect associations between mobile usage and vaccination attitudes although it is consistent with other studies conducted to evaluate the feasibility, acceptability or efficacy of smartphone mediated interventions for health.19-29 However, our ability to detect associations was more limited by the homogeneity of responses, i.e. the fact that so many of the attitudes were similar made it difficult to identify what factors influence the small variations we did observe. This is not surprising considering that the type of individuals who would be willing to participate in this study would be strongly supportive of vaccination. Participants were also highly educated, mostly married, employed and on average 2 years older than the average maternal age at childbirth in Ontario,30 which may be an indicator of attitudes toward immunization and openness to using a mobile app.31,32 The relationship between mobile readiness and vaccination attitudes would be better examined by a cross-sectional study design where individuals sampled were not restricted to those willing to download an immunization app.
With nearly all of participants reporting that they planned on vaccinating their child and believing that other people's children should be vaccinated, we were surprised to observe that over a quarter of participants agreed or strongly agreed that the risk of vaccination outweighed the benefits, although this could reflect a misinterpretation of the question. This particular question was flagged during pilot testing and subsequently revised to accommodate concerns. However, these revisions may not have been sufficient in resolving confusion. Further clarification of this question may have been warranted.
Another warranted avenue of investigation is that it is possible that support toward vaccination in first time mothers during pregnancy may deteriorate as they are exposed to misinformation regarding vaccination shortly after birth. This is particularly true if they are relying on the Internet for which it is recognized the accuracy of immunization information is poor.11,33,34 Direct communication by public health through user friendly mobile apps could provide a mechanism to mitigate against this. This is the first part of a longitudinal study which aims to determine the impact of a mobile application on maternal attitudes and beliefs regarding pediatric vaccination.
The receptiveness of the vaccine hesitant to an app and the impact of the app on attitudes toward vaccination merits further study. Given that mobile devices and applications have a higher barrier to entry for development and distribution as compared to tools traditionally leveraged by anti-vaccine communities such as Internet and social media,9,33,35,36 mobile apps may be less likely to deliver inaccurate information to users regarding immunization and over time may become a convenient, reliable and trusted source for those seeking information. Unlike websites, apps are subjected to approval by the app stores, in particular by Apple which is attentive to public reporting on inappropriate or inaccurate information contained within apps.
Conclusions
Despite the efficiency, cost-effectiveness and safety of immunization programs, vaccine hesitancy remains a concern and several regions of the world are witnessing the re-emergence of previously controlled VPDs. Mobile technologies provide public health officials with an opportunity to leverage technology and regain lost ground to anti-vaccine campaigners. Mobile technologies can also be used to communicate with the public in new ways as well empowering individuals to become participatory in their health. Our study found that there is potentially an unrealized opportunity to communicate immunization information via mobile applications. While being willing to download an app and interested in information on pediatric vaccination, only one third of participants reported that reliable and accessible on mobile devices. While text messaging and other recall interventions have been successful in increasing immunization uptake, the impact of mobile apps on vaccination attitudes and increasing immunization coverage remains unclear. Future studies should examine the impact of mobile apps on these metrics.
Methods
Study setting
The study was conducted at the Civic campus of The Ottawa Hospital, a large, teaching hospital in Ottawa, Ontario, Canada. Recruitment took place in parts of the Obstetrics/Gynecology Newborn Care and Women's Health Program, The Birthing Unit and Perinatal Care units which provides care to over 4200 women and their families every year.37 The study was approved by the Research Ethics Board at The Ottawa Hospital. Participants were recruited over a 9 month period between November 2013 and July 2014.
Study population
Our study population included women aged 18 years and older who were in their third trimester of pregnancy or who had given birth within the previous 3 months. Participants who spoke English, owned a smartphone and consented to participate were eligible for the study. Women were recruited through a combination of active and passive recruitment. Passive methods used included displaying posters describing the study in the hospital's obstetrical units, ultrasound waiting rooms and obstetrician offices. In parallel, supplementary active methods of recruitment such as short presentations at prenatal information sessions held at the Civic campus, snowball sampling and study handouts given by physicians and clinical managers at their discretion.
Data collection tools
A baseline survey of 32 questions (7 demographic, 25 other) was developed and pilot-tested on 5 mothers. Minor changes were made to the survey as a result, and those results were not included in the sample (n = 54). Pilot testing was conducted to ensure that participants understood the survey questions and instructions.
Survey questions
Participant demographic information at baseline was collected. Variables collected include age, relationship status, employment status, education level, type of health care provider, and pregnancy history. The survey itself included questions on a 5-point Likert scale to collect participants’ baseline attitudes and behaviors related to childhood vaccinations, as well as information about smartphone and mobile app usage.
There is no established definition for “mobile readiness." However, “technology readiness” is defined as “peoples propensity to embrace and use new technologies for accomplishing goals in home life and at work”.38 For the purposes of this study, we have adapted this and have defined mobile readiness as “an individual's propensity to embrace and adopt a mobile device as a platform for accessing and interacting with personal health information." We believe that mobile readiness is critical to the topic we are examining because the effectiveness of applications to influence immunization attitudes will be dependent on their likelihood to use those applications. Obviously an application that appears to have the necessary features to influence vaccination attitudes will not be effective if the target population is not prepared to utilize it.
We have assumed that participation in the study suggested a willingness to use the app, as this was a requirement to participate in the study. What is less certain is whether the participants will actually utilize the app. In order to ascertain this, we measured participant use of app for other purposes, for example bank transactions or acquiring information such as news, weather or transit schedules. The concept of using number of technology oriented behaviors to predict an individual's propensity to adopt a novel technology is derived from content that was identified to be predictive of Technology readiness index scores,16 specifically the number of online behaviors engaged in during the past year (i.e., banking) and number of technology oriented behaviors (i.e. using cloud applications).
Descriptive analyses
Baseline demographic information is presented as means and standard deviations (SD). Responses to questions on the Likert scale and to categorical variables are presented as frequencies and percentages.
Statistical analysis
Using polytomous logistic regression, we conducted univariate analyses to assess the relationship between participants’ responses to survey questions related to mobile device usage and behaviors and attitudes about vaccination, as well as between demographic variables (participant age and parity) and mobile device usage. Responses were modeled as ordinal values from 1 to 5. We individually modeled the relationships between each survey question relating to mobile readiness and both demographic variables and behaviors / attitudes about vaccination. In the posthoc analysis, we created a mobile readiness score by taking the sum of the 6 mobile usage survey question responses for each participant, and modeled the relationships between this score and behaviors / attitudes about vaccination. We used a Spearman's rank correlation coefficient to verify whether there was a significant correlation between participant age and mobile readiness score. We used a Wilcoxon rank sum test to test for significant differences in the mobile readiness scores between first-time mothers and mothers who had previous children.
Acknowledgments
We would also like to thank the ImmunizeCA team; Developers Cameron Bell, Julien Guerinet and Yulric Sequeira, our partners at CPHA, Greg Penney, Chandni Sondagar and at ImmunizeCanada, a coalition of CPHA, Lucie Marisa Bucci.
Disclosure of Potential Conflicts of Interest
Both KW and KA are founders of Sigvaria Mobile Technologies Inc., the company responsible for developing the ImmunizeCA app for the Canadian Public Health Association (CPHA).
Funding
Thank you to our funders, the Pan Canadian Influenza Research Network (PCIRN), the Canadian Association for Immunization Research and Evaluation (CAIRE), and the Public Health Agency of Canada (PHAC).
References
- 1. Stockwell MS, Fiks AG. Utilizing health information technology to improve vaccine communication and coverage. Hum Vaccin Immunother 2013; 9:1802–11; PMID:23807361; http://dx.doi.org/ 10.4161/hv.25031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stockwell MS, Kharbanda EO, Martinez RA, Lara M, Vawdrey D, Natarajan K, Rickert VI. Text4Health: impact of text message reminder–recalls for pediatric and adolescent immunizations. Am J Public Health 2012; 102:e15-e21; PMID:22390457; http://dx.doi.org/ 10.2105/AJPH.2011.300331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ahlers-Schmidt CR, Hart T, Chesser A, Paschal A, Nguyen T, Wittler RR. Content of text messaging immunization reminders: what low-income parents want to know. Patient Educ Couns 2011; 85:119-21; PMID:20832970; http://dx.doi.org/ 10.1016/j.pec.2010.08.007 [DOI] [PubMed] [Google Scholar]
- 4. Stockwell MS, Westhoff C, Kharbanda EO, Vargas CY, Camargo S, Vawdrey DK, Castaño PM. Influenza Vaccine Text Message Reminders for Urban, Low-Income Pregnant Women: A Randomized Controlled Trial. Am J Public Health 2014; 104(S1):27-e12; PMID:24354839, http://dx.doi.org/ 10.2105/AJPH.2013.301620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Clark SJ, Butchart A, Kennedy A, Dombkowski KJ. Parents' experiences with and preferences for immunization reminder/recall technologies. Pediatrics 2011; 128:e1100-5; PMID:22007019; http://dx.doi.org/ 10.1542/peds.2011-0270 [DOI] [PubMed] [Google Scholar]
- 6. Odone A, Ferrari A, Spagnoli F, Visciarelli S, Shefer A, Pasquarella C, Signorelli C. Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage: A systematic review. Hum Vaccin Immunother 2014; 72-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ottawa Hospital Research Institute (2014). ImmunizeCA (Version 2.0.4) [Mobile Application Software]. Retrieved from http://www.immunize.ca/en/app.aspx [Google Scholar]
- 8. Mills E, Jadad AR, Ross C, Wilson K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J Clin Epidemiol 2005; 58:1081-8; PMID:16223649; http://dx.doi.org/ 10.1016/j.jclinepi.2005.09.002 [DOI] [PubMed] [Google Scholar]
- 9. Wilson K, Keelan J. Social media and the empowering of opponents of medical technologies: the case of anti-vaccinationism. J Med Int Res 2013; 15:e103; PMID:23715762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wheeler M, Buttenheim AM. Parental vaccine concerns, information source, and choice of alternative immunization schedules. Hum Vaccin Immunother 2013; 9:1782-9; PMID:23900266; http://dx.doi.org/ 10.4161/hv.25959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wolfe RM, Sharp LK. Vaccination or immunization? The impact of search terms on the internet. J Health Commun 2005; 10:537-51; PMID:16203632; http://dx.doi.org/ 10.1080/10810730500228847 [DOI] [PubMed] [Google Scholar]
- 12. Kata A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm – An overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 2012; 30:3778-89; PMID:22172504; http://dx.doi.org/ 10.1016/j.vaccine.2011.11.112 [DOI] [PubMed] [Google Scholar]
- 13. Wilson K, Atkinson K, Deeks S. Opportunities for utilizing new technologies to increase vaccine confidence. Exp Rev Vaccin 2014:1-9 [DOI] [PubMed] [Google Scholar]
- 14. Feemster KA. Overview: special focus vaccine acceptance. Hum Vaccin Immunother 2013; 9:1752-4; PMID:23974831; http://dx.doi.org/ 10.4161/hv.26217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gowda C, Dempsey AF. The rise (and fall?) of parental vaccine hesitancy. Hum Vaccin Immunother 2013; 9:1755-62; PMID:23744504; http://dx.doi.org/ 10.4161/hv.25085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Parasuraman A, Colby CL. An updated and streamlined technology readiness index TRI 2.0. J Serv Res 2014; 18:59-74; doi:1094670514539730 [Google Scholar]
- 17. Kuo K-M, Liu C-F, Ma C-C. An investigation of the effect of nurses' technology readiness on the acceptance of mobile electronic medical record systems. BMC Med Inform Decis Mak 2013; 13:88; PMID:23938040; http://dx.doi.org/ 10.1186/1472-6947-13-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Campbell JD, Harris KD, Hodge R. Introducing telemedicine technology to rural physicians and settings. J Family Pract 2001; 50:419-24; PMID:11350706 [PubMed] [Google Scholar]
- 19. Wharton CM, Johnston CS, Cunningham BK, Sterner D. Dietary self-monitoring, but not dietary quality, improves with use of smartphone app technology in an 8-week weight loss trial J Nutr Educ Behav. 2014; 46:440-4; PMID:25220777; http://dx.doi.org/ 10.1016/j.jneb.2014.04.291 [DOI] [PubMed] [Google Scholar]
- 20. Min YH, Lee JW, Shin YW, Jo MW, Sohn G, Lee JH, Lee G, Jung KH, Sung J, Ko BS, et al. . Daily collection of self-reporting sleep disturbance data via a smartphone app in breast cancer patients receiving chemotherapy: a feasibility study. J Med Internet Res 2014; 16:e135; PMID:24860070; http://dx.doi.org/ 10.2196/jmir.3421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Man C, Nguyen C, Lin S. Effectiveness of a smartphone app for guiding antidepressant drug selection. Fam Med 2014; 46:626-30; PMID:25163042 [PubMed] [Google Scholar]
- 22. Hong Y, Goldberg D, Dahlke DV, Ory MG, Cargill JS, Coughlin R, Hernandez E, Kellstedt DK, Peres SC. Testing usability and acceptability of a web application to promote physical activity (iCanFit) among older adults. JMIR Human Factors 2014; 1:e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dennis ML, Scott CK, Funk RR, Nicholson L. A pilot study to examine the feasibility and potential effectiveness of using smartphones to provide recovery support for adolescents. Subst Abus 2014; 13:0; PMID:22421189 2531005; http://dx.doi.org/ 10.1080/08897077.2014.970323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Irvine Michael JD. Outcome evaluation of a time management smartphone application: a pilot study" (2013). Doctor of Psychology (PsyD). Paper 118. http://digitalcommons.georgefox.edu/psyd/118. [Google Scholar]
- 25.Freshwater ES, Crouch R. Technology for trauma: testing the validity of a smartphone app for pre-hospital clinicians. Int Emer Nursbib 2015; 23:32-37; https://dx.doi.org/ 10.1016/j.ienj.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 26. Mellone S, Tacconi C, Chiari L. Validity of a Smartphone-based instrumented Timed Up and Go. Gait Posture 2012; 36:163-5; PMID:22421189; http://dx.doi.org/ 10.1016/j.gaitpost.2012.02.006 [DOI] [PubMed] [Google Scholar]
- 27. Lin C-Y, Peng K-L, Chen J, Tsai J-Y, Tseng Y-C, Yang J-R, Chen M-H. Improvements in dental care using a new mobile app with cloud services. J Formosn Med Assoc 2014; 113:742-9; PMID:24796822; http://dx.doi.org/ 10.1016/j.jfma.2014.02.009 [DOI] [PubMed] [Google Scholar]
- 28. Faurholt-Jepsen M, Frost M, Vinberg M, Christensen EM, Bardram JE, Kessing LV. Smartphone data as objective measures of bipolar disorder symptoms. Psychiatry Res 2014; 217:124-7; PMID:24679993; http://dx.doi.org/ 10.1016/j.psychres.2014.03.009 [DOI] [PubMed] [Google Scholar]
- 29. Jandee K, Lawpoolsri S, Taechaboonsermsak P, Khamsiriwatchara A, Wansatid P, Kaewkungwal J. Customized-language voice survey on mobile devices for text and image data collection among ethnic groups in Thailand: a proof-of-concept study. JMIR Mhealth Uhealth 2014; 2:e7; PMID:25098776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Employment and Social Development Canada. Family life - Age of mother at childbirth. In: Indicators of Well-Being in Canada (2011) Government of Canada. http://www4.hrsdc.gc.ca/.3ndic.1t.4r@-eng.jsp?iid=75 [Google Scholar]
- 31. Larson HJ, Jarrett C, Eckersberger E, Smith D, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014; 32:2150-9; PMID:24598724 [DOI] [PubMed] [Google Scholar]
- 32. Larson HJ, Smith DM, Paterson P, Cumming M, Eckersberger E, Freifeld CC, Ghinai I, Jarrett C, Paushter L, Brownstein JS, et al. . Measuring vaccine confidence: analysis of data obtained by a media surveillance system used to analyse public concerns about vaccines. Lancet Infect Dis 2013; 13:606-13; PMID:23676442; http://dx.doi.org/ 10.1016/S1473-3099(13)70108-7 [DOI] [PubMed] [Google Scholar]
- 33. Keelan J, Pavri-Garcia V, Tomlinson G, Wilson K. YouTube as a source of information on immunization: a content analysis. Jama 2007; 298:2482-4; PMID:18056901; http://dx.doi.org/ 10.1001/jama.298.21.2482 [DOI] [PubMed] [Google Scholar]
- 34. Poland GA, Jacobson RM. The age-old struggle against the antivaccinationists. N Engl J Med 2011; 364:97-9; PMID:21226573; http://dx.doi.org/ 10.1056/NEJMp1010594 [DOI] [PubMed] [Google Scholar]
- 35. Vance K, Howe W, Dellavalle RP. Social internet sites as a source of public health information. Dermatol Clin 2009; 27:133-6; PMID:19254656; http://dx.doi.org/ 10.1016/j.det.2008.11.010 [DOI] [PubMed] [Google Scholar]
- 36. Huesch M, Ver Steeg G, Galstyan A. Vaccination (Anti-) campaigns in social media. Workshops at the Twenty-Seventh AAAI Conference on Artificial Intelligence, 2013
- 37. The Ottawa Hospital, Our Model of Care. Birthing Unit, Civic Campus. Accessed July 17, 2014. Retrieved from https://www.ottawahospital.on.ca/wps/portal/Base/TheHospital/OurModelofCare/ProfessionalTeam/Nursing/NursingUnitProfiles/BirthingUnit [Google Scholar]
- 38. Parasuraman A. Technology Readiness Index (TRI) a multiple-item scale to measure readiness to embrace new technologies. J Ser Res 2000; 2:307-20; http://dx.doi.org/ 10.1177/109467050024001 [DOI] [Google Scholar]