Abstract
Cystinuria is a genetic cause of recurrent kidney stones which may be more recurrent and larger than more common non-cystine stones. They may have a greater impact on health-related quality of life (HRQoL). We measured this impact by surveying HRQoL in patients with stones, comparing non-cystine stone formers (NCSF) to cystine stone formers (CYSF) and both groups to normative values of the US population. We used SF-36v2 via an internet instrument. CYSF patients were recruited via cystinuria-related websites, two patient advocacy groups, and an active endourology practice. NCSF patients were recruited from the same practice and by email. Total n surveyed with scorable data: 214 CYSF and 81 NCSF. The participants included 128 men and 161 women. The group of CYSF were significantly younger (39 vs. 54 years) and suffered longer from kidney stones (255 vs. 136 months). CYSF patients had significantly more episodes of stones than NCSF patients in the last year (N = 108 CYSF, N = 20 NCSF). More frequent stones in the last year and mental comorbidities most often predicted worse scores in the individual HRQoL domains. However, cystine stone composition was a significant predictor of worse scores only for role emotional. Better scores in all SF-36 domains were associated with greater time since the last kidney stone event. Although kidney stones are often transient, kidney stone formers, regardless of stone composition, have a worse HRQoL than the standard US population, which has a normative score of 50, such as general health (41.2 ± 12.8), bodily pain (46.5 ± 11.8) and mental health (45.1 ± 12.6). CYSF are more frequent and severe stone formers compared with NCSF with a resulting greater, direct impact on the HRQoL of CYSF patients. Whether preventive strategies for cystinuria are being properly utilized by practitioners, and which strategies are most effective, should be established.
Keywords: Calcium, Calculi, Renal, Kidney stones, Cystinuria, Nephrolithiasis, Urolithiasis
Introduction
Kidney stones are painful, debilitating and recurrent, yet little is known about how they affect the long-term quality of life of individuals. Limited data suggest that health-related quality of life (HRQoL) and mental health are affected more adversely than some physicians might predict [1, 2]. Women appear to be more affected than men [3]. Although episodes of renal colic are often short-lived, leading to spontaneous stone passage in the majority of cases, as many as 20 % require urologic intervention, affect a relatively younger population than many other chronic diseases, lead to significant expenses, and can have an important impact on work attendance [4, 5]. In addition, stone prevention requires attention to regimens of frequent fluid ingestion with a resultant increase in urine volume and voiding frequency, changes in diet or use of prescription medications and may focus sizeable attention on asymptomatic stones in between episodes of colic [6].
Cystinuria, a genetic disorder of transepithelial cystine transport, is a particularly debilitating form of nephrolithiasis characterized by large, recurrent stones [7]. More than 80 % of patients will experience their first symptomatic stone in the first two decades of life and then often have recurrent stones every 3–5 years or more frequently [8]. While quality of life has been assessed in stone formers before, there is a dearth of data regarding the experiences of people with cystinuria. In this protocol we assessed the impact of cystinuria on HRQoL in patients with cystinuria and compared their responses with the more common condition of non-cystine-based stones. In addition, we compared our samples of cystine and non-cystine stone formers (CYSF and NCSF) with normative values for the control population of the United States. We demonstrate here, in the largest survey of people with cystinuria ever completed, that cystinuria results in worse quality of life than do non-cystine stones, and that both stone formers of either composition have worse HRQoL than the normative US population.
Methods
Using a multidisciplinary team including a nephrologist, urologist, epidemiologist and biostatistician, we developed a web-based survey that captured patient demographics, comorbidities, general health status, urologic-specific healthcare utilization and HRQoL information. A structured online questionnaire was used to capture relevant information.
Study design
This protocol was designed as an online survey only. Prior to data collection, the protocol was approved by the institutional review boards of both St. Vincents Hospital and Thomas Jefferson University. The survey was designed to capture information anonymously; no personal health-related identifiers were included. The internet protocol (IP) number was used to control for data accuracy. The survey generated a code number that allowed the tracking of non-responders. All data were stored on SurveyMonkey.com and were only accessible by key study personnel. The SF-36v2 was used to measure HRQoL. The instrument generates normative scores, standardized to the US population, which has mean values ± SD of 50 ± 10 for each domain. Scores above 50 represent better HRQoL and scores below 50, worse, than the US mean. Data were transferred into SPSS 18 for statistical analysis. Statistical analysis consisted of independent t tests and Fischer’s exact test. Multiple regression analyses included the following variables: stone event frequency, time of last stone event, and whether the event required treatment. Age, gender, grouped comorbidities and type of stone were also included. The grouped comorbidities (and specific symptoms surveyed) were:
Mental (anxiety, depression).
Musculoskeletal (arthritis, back, shoulder, or knee problem).
Respiratory (asthma, chronic bronchitis).
Metabolic (diabetes mellitus, high blood pressure, high cholesterol, obesity).
Sample selection and inclusion criteria
Patients were identified from several sources. First, a link to the survey was posted on the website of the International Cystinuria Foundation (ICF, www.cystinuria. org). Emails were sent periodically to the Cystinuria Support Network (CSN, www.cystinuria.com), an email list with more than 250 subscribers. Patients in the Kidney Stone Prevention Program at St. Vincent’s Hospital in New York were given an introductory letter with a link to the survey. In compliance with IRB procedures, study candidates were required to complete an online informed consent form in order to be included in the analysis. This consent form was administered electronically and not collected by the investigators. Study inclusion criteria required that patients were 18 years or older, could communicate in English, could give consent to participate, and had internet access with either an email address or a valid postal address in the United States. We required that NCSF had had their last episode of a symptomatic kidney stone or a urological stone intervention within the last year. Proof of stone composition was not elicited.
Sample size calculation
Our hypothesis was that we would detect at least a 2-point difference in lower SF-36 Physical and Mental Component Scores (PCS and MCS) between the CYSF compared with the NCSF groups. In order to detect such a difference with a sensitivity of 80 %, we would need a minimum of 119 NCSF participants and 166 CYSF participants. We therefore aimed to recruit at least 250–300 NCSF individuals and 250–300 CYSF, recognizing that a number of study candidates would be ineligible or would choose not to participate.
Results
Sample demographics
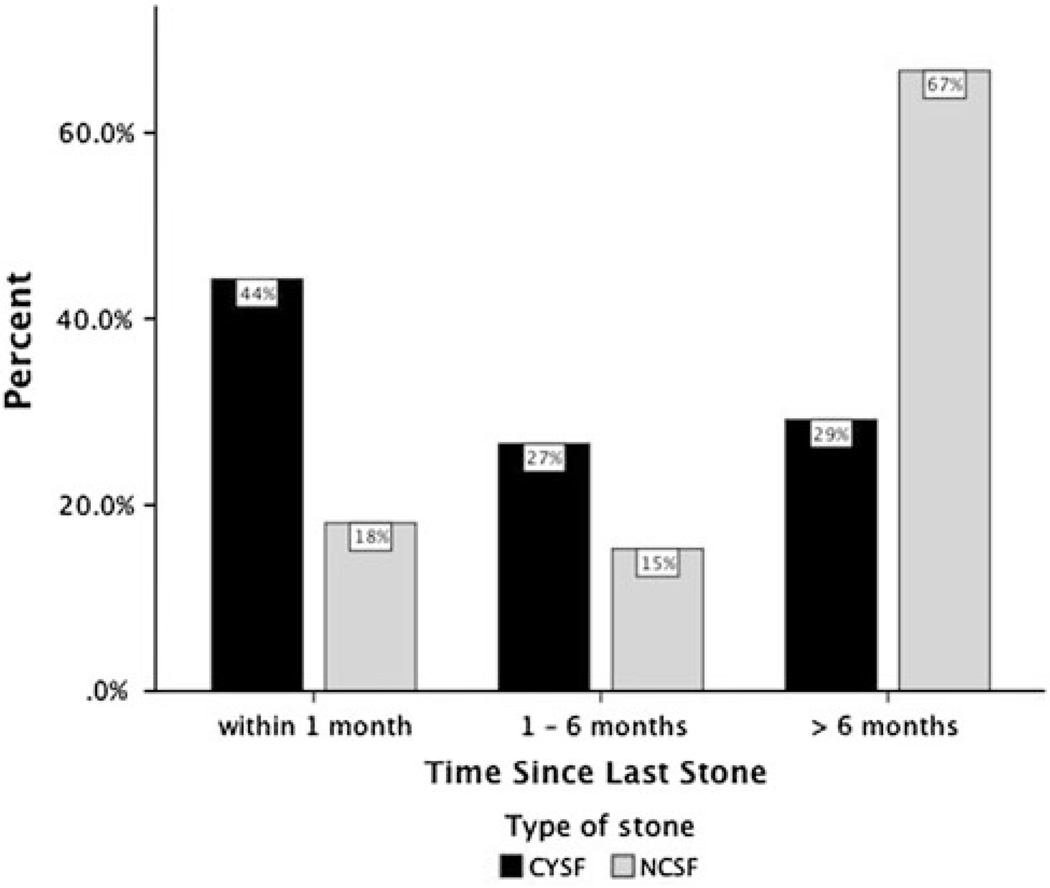
In total, we included 295 kidney stone patients into the data analysis, including 214 CYSF and 81 NCSF. The NCSF reported having 54 calcium stones, 11 uric acid stones, and 16 said they did not know their stone composition. The participants included 161 women and 128 men. There were more women in the CYSF group, and more men in the NCSF group. A detailed distribution is shown in Table 1. The mean age of CYSF in our sample was 15 years less than that of the NCSF. The majority of participants in the total sample were white (≥90 %). Access to health insurance coverage was similar in both groups (92 vs. 84 %, p >0.05). The major type of insurance was preferred provider organization (PPO) in both groups. Half of the CYSF reported a stone treatment in the past year, while only 25 % of the NCSF, all of whom were supposed to have had a symptomatic stone in the last year, reported a stone-related treatment. Almost a third of CYSF were hospitalized because of a kidney stone-related event within the last 12 months time period. The CYSF in our sample experienced kidney stones for a longer period (255 vs. 136 months) and reported more stone episodes (mean 5.13 vs. 2.41, p <0.001) during the past 12 months, shown in Table 2. One-third of the patients with cystinuria in the sample experienced a kidney stone episode within the prior month (Fig. 1). Table 2 also shows the types of urologic interventions that the 2 groups experienced. Urological stone treatment was significantly higher for CYSF; 30 % of our CYSF sample underwent a kidney stone removal procedure during the past year, compared with 7 % of NCSF. The application of shockwave lithotripsy was 16 % in both groups, while ureteroscopy and nephrostolithotomy treatments were significantly higher in the CYSF group. Nephrectomy occurred in 1 % of CYSF and 2 % of NCSF.
Table 1.
Age, gender and race distribution
| CYSF | NCSF | Total | |
|---|---|---|---|
| Participants in survey | 214 | 81 | 295 |
| Age, years (SD)** | 39 (13) | 54 (14) | 53 (15) |
| Male (SD)** | 43 (15) | 55 (14) | 47 (15) |
| Female (SD)** | 37 (13) | 51 (14) | 40 (14) |
| Gender | |||
| Male (%)* | 82 (39) | 46 (61) | 128 (44) |
| Female (%)* | 129 (61) | 32 (39) | 161 (56) |
| Race | |||
| Caucasian (%) | 192 (94) | 68 (90) | 260 (93) |
| African American (%) | 2 (1) | 1 (1) | 3 (1) |
| Hispanic (%) | 4 (2) | 2 (3) | 6 (2) |
| Asian/Pacific Islander (%) | 4 (2) | 4 (5) | 8 (3) |
| Prefer not to answer (%) | 3 (1) | 1 (1) | 4 (1) |
| Currently employed (%) | 137 (64) | 48 (57) | 183 (62) |
| Hospital stay for kidney stones (%)* | 68 (32) | 8 (10) | 76 (26) |
p < 0.05 by Fishers exact test
p < 0.05 by independent t test
Table 2.
Stone treatments: non-surgical, surgical interventions and hospitalizations (%)
| CYSF (N = 214) |
NCSF (N = 81) |
Total (N = 295) |
|
|---|---|---|---|
| Suffers from kidney stones (months)** | 255 | 136 | |
| Special diet | 85 (40) | 32 (40) | 117 (40) |
| Stone treatment past year* | 108 (50) | 20 (25) | 128 (43) |
| Hospitalized because of kidney stone* | 61 (28) | 8 (10) | 69 (23) |
| Stone removal* | 65 (30) | 6 (7) | 71 (24) |
| Shockwave lithotripsy | 34 (16) | 13 (16) | 47 (16) |
| Ureteroscopy* | 65 (30) | 6 (7) | 71 (24) |
| Nephrostolithotomy* | 28 (13) | 2 (2) | 30 (10) |
| Nephrectomy | 3 (1) | 2 (2) | 5 (2) |
p < 0.05 by Fishers exact test
p < 0.05 by independent t test
Fig. 1.
Distribution of time since last stone episode in cystine stone formers (CYSF) and non-cystine stone formers (NCSF), within 1 months: N = 85 CYSF/13NCSF, 1–6 months: N = 51 CYSF/11 NCSF, >6 months: N = 56 CYSF/48 NCSF
The prevalence of comorbidities among study participants is shown in Table 3. NCSF showed a significantly higher prevalence of cancer, heartburn, high cholesterol and underactive thyroid, while a significantly higher prevalence of arthritis, chronic pain and headaches was seen in CYSF. The higher prevalence of comorbidities within the NCSF group might be attributable to the higher age of this group.
Table 3.
Co-morbidities (% of each stone type)
| CYSF | NCSF | Total | |
|---|---|---|---|
| Anemia | 21 (10) | 4 (5) | 25 |
| Anxiety | 30 (14) | 8 (10) | 38 |
| Arthritis* | 18 (18) | 14 (14) | 32 |
| Asthma | 19 (9) | 3 (4) | 22 |
| Back, shoulder, or knee problems | 33 (15) | 15 (19) | 48 |
| Cancer* | 2 (1) | 6 (7) | 8 |
| Chronic bronchitis | 3 (1) | 2 (3) | 5 |
| Chronic pain* | 36 (17) | 6 (7) | 42 |
| Depression | 35 (16) | 10 (12) | 45 |
| DM | 9 (4) | 9 (11) | 18 |
| Epilepsy | 0 (0) | 1 (1) | 1 |
| Family history of kidney stones | 52 (24) | 19 (24) | 71 |
| Headaches* | 31 (15) | 2 (3) | 33 |
| Heartburn* | 5 (2) | 7 (9) | 12 |
| Hepatitis | 3 (1) | 1 (1) | 4 |
| High blood pressure | 53 (25) | 25 (31) | 78 |
| High cholesterol* | 35 (16) | 25 (31) | 60 |
| Infertility | 5 (2) | 2 (3) | 7 |
| Nasal allergies | 19 (9) | 7 (9) | 26 |
| Obesity | 32 (15) | 9 (11) | 41 |
| Overactive thyroid | 2 (1) | 2 (3) | 4 |
| Underactive thyroid* | 4 (2) | 6 (7) | 10 |
CYSF cystine stone formers, NCSF non-cystine stone formers
p < 0.05 by Fishers exact test
Comparison of quality of life components
When comparing the total sample of CYSF and NCSF combined, men reported a better HRQoL than women in all domains except one of the physical component domains, physical functioning. All other domains were better in men than in women: role-physical (p = 0.031), bodily pain (p = 0.009), general health (p = 0.04), vitality (p = 0.0001), social functioning (p = 0.001), role emotional (p = 0.008), mental health (p = 0.037), PCS (p = 0.027) and MCS (p = 0.003). There were also differences in the effect of gender on 2 HRQoL MCS domains between CYSF and NCSF. Specifically, scores were worse for women than men CYSF for vitality (p = 0.005), social functioning (p = 0.037) and the MCS (p = 0.029). Among NCSF, a significantly lower score for females could be found only in social functioning (p = 0.013) and role emotional (p = 0.026) as compared with men.
Regression results for PCS and MCS are presented in Table 4. The following variables were used: type of stone; respiratory, musculoskeletal, metabolic and mental comorbidities; gender; kidney stone treatment in the last year; frequency of stone events; age; and last stone event. All variables were entered together in a simultaneous regression. All partial regression coefficients are reported as raw (B) coefficients.
Table 4.
Regression model for summary scores
| PCS | MCS | |||
|---|---|---|---|---|
| B | p | B | p | |
| # of kidney stone episodes in last year | −0.630 | 0.0001 | −0.457 | 0.050 |
| Time since last kidney stone episode | 0.730 | 0.0001 | 0.482 | 0.066 |
| Treatment required for stones in last year | 0.032 | 0.978 | 2.498 | 0.112 |
| Age | −0.027 | 0.517 | 0.072 | 0.201 |
| Gender | −1.981 | 0.063 | −2.616 | 0.071 |
| Co-morbid conditions | ||||
| Mental | −0.672 | 0.444 | −9.410 | 0.000 |
| Musculoskeletal | −5.191 | 0.0001 | 0.396 | 0.755 |
| Respiratory | −6.620 | 0.0001 | 2.369 | 0.304 |
| Metabolic | −1.545 | 0.009 | −.626 | 0.436 |
| Type of stone | 1.720 | 0.205 | −3.023 | 0.102 |
| Adjusted R2 | 0.404 | 0.350 | ||
| F | 18.551 | 14.944 | ||
| Significance of F | 0.0001 | 0.0001 | ||
| N | 260 | 260 | ||
B coefficient in regression equation for predicting the dependent variable, p significance level of coefficient
The results of the regression indicated that the predictors explained 42.7 % of the variance in PCS (R2 = 0.42, F(10, 249) = 18.551, p <0.001). Worse PCS scores were predicted by greater frequency of stone events in the last year (B = −0.63, p <0.001), shorter time since the last stone event (B = 0.73, p <0.001), and more musculoskeletal (B = −5.191, p <0.001), respiratory (B = −6.62, p <0.001) and metabolic comorbidities (B = −1.545, p <0.009). The regression for the MCS showed that the predictors explained 37.5 % of the variance (R2 = 0.375, F(10, 249) = 14.94, p <0.001). Only the variable mental comorbidities (B = −9.410, p <0.001) had a significant effect to predict the MCS.
On the domain level, the regression indicated that the predictors explained 34.8 % of the variance in physical functioning (R2 = 0.34, F(10, 254) = 13.58, p <0.001). Worse physical functioning scores were predicted by greater frequency of stone events in the last year (B = −0.423, p <0.015), and more of all the grouped comorbidities: mental (B = −4.137, p <0.001), musculoskeletal (B = −4.119, p <0.001), respiratory (B = −5.574, p <0.002) and metabolic (B = −1.562, p <0.01).
For the eight individual HRQoL domains, Table 5 indicates the proportion explained by all of the variables in the regression model, and the p values for the contribution of the individual variables, including the four grouped comorbidities. All eight domains had significant proportions explained by different combinations of variables. More frequent stones in the last year and mental comorbidities most often predicted worse scores in the individual domains. Cystine stone formation as compared with noncystine stone formation was a significant predictor of worse scores only for role emotional.
Table 5.
Contributions of study variables to specific domains of the SF-36 HRQoL instrument, based on multiple regression
| Domain | % of variance predicted by variables |
More stones in last year |
Shorter time since last stone event |
Female gender |
Required urologic intervention for stone event |
Mental comorbidities |
Musculoskeletal comorbidities |
Respiratory comorbidities |
Metabolic comorbidities |
CYSF |
|---|---|---|---|---|---|---|---|---|---|---|
| Physical functioning | 34.8 p < 0.001 |
−0.42 p < 0.015 |
−4.14 p < 0.001 |
−4.12 p < 0.001 |
−5.374 p < 0.002 |
−1.56 p < 0.01 |
||||
| Role-physical | 37.7 p < 0.001 |
−0.78 p < 0.001 |
0.74 p < 0.001 |
−3.12 p = 0.003 |
−3.67 p < 0.001 |
|||||
| Bodily pain | 44.4 p < 0.001 |
−0.64 p < 0.001 |
1.18 p < 0.001 |
−2.4 p = 0.04 |
−3.90 p < 0.001 |
|||||
| General health | 32.4 p < 0.001 |
−0.77 p < 0.001 |
−2.834 p = 0.04 |
−2.62 p = 0.023 |
−3.24 p = 0.009 |
−8.80 p < 0.001 |
−1.94 p = 0.013 |
|||
| Vitality | 34.3 p < 0.001 |
0.81 p < 0.001 |
3.68 p = 0.016 |
−6.07 p < 0.001 |
−3.35 p = 0.007 |
|||||
| Social functioning | 39.6 p < 0.001 |
0.81 p < 0.001 |
−3.63 p = 0.008 |
3.40 p = 0.21 |
−6.32 p < 0.001 |
−3.16 p = 0.008 |
||||
| Role emotional | 34.2 p < 0.001 |
−0.581 p = 0.015 |
−8.85 p < 0.001 |
−3.98 p < 0.032 |
||||||
| Mental health | 33.7 p < 0.001 |
1.74 p = 0.032 |
−8.02 p < 0.001 |
The first column indicates the proportion of variance with associated p value in the eight HRQoL domains explained by the individual variables including 4 grouped comorbidities. Each cell contains B, the unstandardized beta, indicating the extent to which each study variable contributed to the HRQoL score
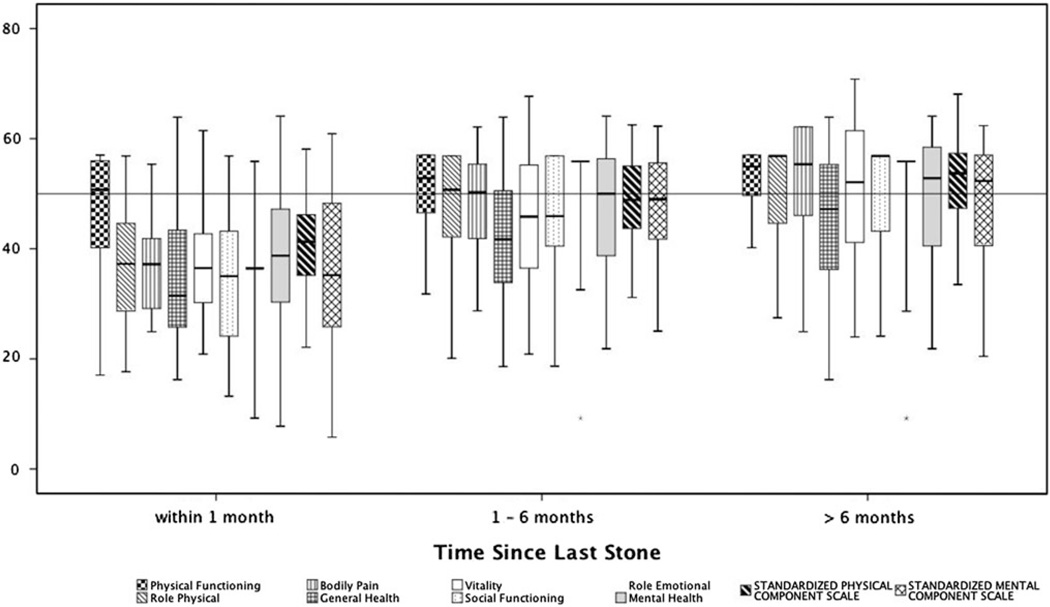
We divided our total sample, both CYSF and NCSF, into three subgroups based on the last reported kidney stone event (within 30 days, >1–6 months, 6 months–1 year). Our results showed better scores in all SF-36 domains with greater time since the last kidney stone event. We demonstrated a significant difference between all three time groups (Fig. 2).
Fig. 2.
Health-related quality of life (HRQoL) scores in eight domains and composite physical and mental component scales at varying intervals since last stone for both CYSF and NCSF. The line across at 50 represents the normative US mean. Scores above 50 represent better HRQoL and scores below 50, worse, than the US mean. Within 1 month: N = 85 CYSF/13NCSF, 1–6 months: N = 51 CYSF/11 NCSF, >6 months: N = 56 CYSF/48 NCSF
Discussion
In this online survey, we compared two groups of kidney stone formers to US norms. As previous studies demonstrated, our results indicate that kidney stone formers have a lower quality of life than the standard, normative US population [1, 3]. Our study fills a critical knowledge gap about quality of life in CYSF since it is the first to specifically study this population. In our sample, CYSF report a lower quality of life than NCSF. This appears clearly related to the fact that in our sample, the CYSF had more stones, and more recent stones, than the NCSF. The majority of CYSF in our sample had a stone event within 1 month prior to the HRQOL assessment. CYSF are also more likely to undergo surgical interventions. More recent stone events were strongly correlated with all HRQoL indices, most likely because 22 questions in the SF-36 focus on the preceding 30-day interval. Therefore, the high likelihood of recent stone events in our CYSF translated into overall lower HRQoL domain scores in this group. For both groups, these results are similar to those reported in other chronic conditions like diabetes and inflammatory bowel disease [9]. Consistent with the idea that more frequent stones was the cause of worse HRQoL in cystine stone formers, the regression model revealed only one domain, role emotional, for which CYSF was a significant predictor of worse scores as compared with NCSF (Table 5).
Studies of HRQoL in stone formers in general have also demonstrated reduced scores in various domains. In 189 patients, whose stone composition was not specified and therefore can be presumed to be mostly calcium or NCSF, stone formers had lower scores than the normative US population for general health and bodily pain but not for other domains [3]. That result differed from our NCSF group, which had lower scores than the normative US data in all domains except physical functioning, bodily pain and the PCS. The difference may be attributable to our selection of a more acute sample in that we required that NCSF had had their last episode of a symptomatic kidney stone or a stone treatment within the last year. Both groups were similar in age, with Penniston’s sample 50.9 years and our NCSF group 53 years old. In the study of Penniston, HRQoL impairment was accentuated among those who were overweight and obese, and among those with depression, diabetes mellitus, hypertension and musculoskeletal complaints. Other comorbidities did not appear to affect HRQoL scores. Similarly, in our study, worse HRQoL was associated with the grouped mental, musculoskeletal, respiratory and metabolic comorbidities. However, in Penniston’s study, neither the number of stone surgeries nor shock wave lithotripsies were associated with differences in HRQoL, while in our study, participants who required urologic intervention for stone events had worse scores for vitality and mental health (Table 5). Other studies have shown varying results. In Saudi Arabia, with a mean of 7.2 months following lithotripsy, 110 patients had worse HRQoL for bodily pain and social functioning than 220 volunteers [10]. In another study of 155 stone formers, their HRQoL was diminished in 5 of 8 domains and for the PCS [10]. Multivariate regression modeling showed that increasing body mass index and age were the strongest predictors of decreased physical well-being. In the only longitudinal study of HRQoL in stone formers, 96 patients completed two surveys, with a median interval of 18 months [11]. No statistically significant differences in any of the SF-36 domains or the PCS or MCS from one survey to the next were noted. The authors suggested that the SF-36 may not be an adequate tool to monitor quality of life over time in stone patients because 18 patients with a stone event within the month preceding completion of the initial questionnaire had no clinically or statistically significant changes in any of the SF-36 domains between the first and follow-up questionnaire. They suggested that a validated, disease-specific questionnaire was needed to facilitate comparison of treatment strategies for stone disease. We plan to obtain longitudinal data regarding HRQoL in a larger group of patients with genetic kidney stone disease.
Mental health conditions should not be underestimated in the treatment of CYSF. Mental health comorbidities in CYSF were higher and had a strong association in the mental summary score. Chung et al. [12] demonstrated a risk of subsequent depressive disorders following a diagnosis of urinary calculi in Taiwan. Angell et al. [2] also showed strong associations of depression with stone episodes within the last year. These psychological effects are usually not fully recognized during the treatment and prevention of stone events.
There are potential limitations to our study. We anticipated a much higher number of patients with NCSF. Although we desired a sample size of 119 NCSF and fell short in enrolling only 81, we easily exceeded the number of CYSF needed, enrolling 214 when the desired sample size was 166. We were therefore able to demonstrate the 2-point difference in scores that we hypothesized existed between the two groups. However, the participation of the two groups was solicited in different ways, because the CYSF that responded are active monitors of the online activities of the CSN and ICF. It is possible that participants in these two patient advocacy groups are different with respect to their HRQoL or comorbidities than nonparticipants in these internet-based activities and may be a more active group with respect to stone formation as well. Because the design was an anonymous online survey, we do not have data regarding non-responders. We sought to enroll an active group of NCSF, by enrolling them from our active endourology practice and requiring that their most recent stone episode occurred in the last year. However, we are not aware of any active patient advocacy group for calcium stone formers (other than for those with primary hyperoxaluria) and therefore the characteristics of the NCSF and CYSF may of necessity be different. We have not demonstrated that our patients accurately classify themselves as CYSF or NCSF and have not verified the accuracy of self-reported medical histories. However, previous epidemiologic studies have concluded that patients’ self-reported data are appropriate [13].
As expected, we found in our sample of CYSF, a higher number of stone events associated with the time of the administration of the QOL measurement. While 93 CYSF reported a stone event within the last month, only 17 NCSF had a stone event in the same time period. The SF-36 used the QOL-instrument designed to capture a time period of 30 days prior to administration of the survey. All retrospective measures are subject to recall bias and therefore a definite timeframe should be established. We suggest that future studies measure HRQoL, at the time of the event, in a more standardized fashion, to decrease a potential error variance in the measurement and increase the statistical power.
We demonstrated that the use of a generic instrument to assess the burden of kidney stone in HRQoL is feasible. The application of a generic instrument for the assessment of HRQoL should include additional questions like comorbidities and other stone disease-related items. The time between the last stone event and HRQoL assessment needs to be recorded and accounted for in the analysis and interpretation of domain scores. Penniston et al. [14] have developed a 28-question, disease-specific instrument with questions pertinent to symptoms related to stones and treatment, emotions, daily routines and self-perception. This instrument has been tested in calcium oxalate stone formers and shows a promising internal consistency. As one would expect, the results showed differences between stone formers with and without stones; and, among those with stones, those whose stones were causing symptoms and those whose stones were not causing symptoms. Additional, detailed psychometric testing is being done before the use of that instrument is more widely promoted in a clinical setting. It would be desirable to test it as well among those affected by genetic etiologies of kidney stones.
Conclusions
HRQoL assessment can be implemented in the regular care of kidney stone patients. Domain results and summary scores could give physicians guidance in the treatment of stone disease. Treatment plans should include potential comorbidities, as they have an impact on HRQoL. The application of a generic instrument seems to be appropriate, and the development of a disease-specific HRQoL instrument for cystinuria should be considered. The time between stone event and application of the SF-36 needs to be accounted for to prevent an overestimation in domain scores and the interpretation for treatment.
Acknowledgments
We appreciate a thorough reading of the manuscript by John C. Lieske MD. This study was funded in part by the Susan Schott Research Fund. This work was also generously supported by the Rare Kidney Stone Consortium, a part of NIH Rare Diseases Clinical Research Network (RDCRN). Funding was provided by grant 1U54DK083908-01 from the NIDDK and the Office of Rare Diseases Research (ORDR), part of the National Center for Advancing Translational Sciences (NCATS). The views expressed in written materials or publications do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention by trade names, commercial practices, or organizations imply endorsement by the US Government.
M. Grasso is a consultant for Karl Storz Endoscopy; D.S. Goldfarb is a consultant for Takeda and Astra Zeneca, is owner of Ravine Group and received honoraria from Mission Pharmacal.
Footnotes
Presented in part on 11/06/08 at the annual meeting of the American Society of Nephrology, Philadelphia, PA, USA.
Conflict of interest F. Modersitzki has no conflict of interest; L. Pizzi has no conflict of interest;
Contributor Information
Frank Modersitzki, Kidney Stone Prevention Programs, Nephrology Section/111G, DVAMC, New York Harbor VA Medical Center and NYU School of Medicine, 423 E. 23 St., New York, NY 10010, USA.
Laura Pizzi, School of Health Policy, Jefferson Medical College, Philadelphia, PA, USA.
Michael Grasso, Endourology Section, Lenox Hill Hospital, New York, NY, USA.
David S. Goldfarb, Email: david.goldfarb@nyumc.org, Kidney Stone Prevention Programs, Nephrology Section/111G, DVAMC, New York Harbor VA Medical Center and NYU School of Medicine, 423 E. 23 St., New York, NY 10010, USA; Endourology Section, Lenox Hill Hospital, New York, NY, USA.
References
- 1.Bryant M, Angell J, Tu H, Goodman M, Pattaras J, Ogan K. Health related quality of life for stone formers. J Urol. 2012;188:436–440. doi: 10.1016/j.juro.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 2.Angell J, Bryant M, Tu H, Goodman M, Pattaras J, Ogan K. Association of depression and urolithiasis. Urology. 2012;79:518–525. doi: 10.1016/j.urology.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Penniston KL, Nakada SY. Health related quality of life differs between male and female stone formers. J Urol. 2007;178(6):2435–2440. doi: 10.1016/j.juro.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 4.Saigal CS, Joyce G, Timilsina AR. Direct and indirect costs of nephrolithiasis in an employed population: opportunity for disease management? Kidney Int. 2005;68:1808–1814. doi: 10.1111/j.1523-1755.2005.00599.x. [DOI] [PubMed] [Google Scholar]
- 5.Lotan Y. Economics and cost of care of stone disease. Adv Chronic Kidney Dis. 2009;16:5–10. doi: 10.1053/j.ackd.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Goldfarb DS. Reconsideration of the 1988 NIH consensus statement on prevention and treatment of kidney stones: are the recommendations out of date? Rev Urol. 2002;4:53–60. [PMC free article] [PubMed] [Google Scholar]
- 7.Mattoo A, Goldfarb DS. Cystinuria. Semin Nephrol. 2008;28:181–191. doi: 10.1016/j.semnephrol.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Dello Strologo L, Pras E, Pontesilli C, Beccia E, Ricci-Barbini V, de Sanctis L, Ponzone A, Gallucci M, Bisceglia L, Zelante L, Jimenez-Vidal M, Font M, Zorzano A, Rousaud F, Nunes V, Gasparini P, Palacin M, Rizzoni G. Comparison between SLC3A1 and SLC7A9 cystinuria patients and carriers: a need for a new classification. J Am Soc Nephrol. 2002;13:2547–2553. doi: 10.1097/01.asn.0000029586.17680.e5. [DOI] [PubMed] [Google Scholar]
- 9.Pizzi LT, Weston CM, Goldfarb NI, Moretti D, Cobb N, Howell JB, Infantolino A, Dimarino AJ, Cohen S. Impact of chronic conditions on quality of life in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2006;12:47–52. doi: 10.1097/01.mib.0000191670.04605.e7. [DOI] [PubMed] [Google Scholar]
- 10.Bensalah K, Tuncel A, Gupta A, Raman JD, Pearle MS, Lotan Y. Determinants of quality of life for patients with kidney stones. J Urol. 2008;179:2238–2243. doi: 10.1016/j.juro.2008.01.116. [DOI] [PubMed] [Google Scholar]
- 11.Donnally CJ, 3rd, Gupta A, Bensalah K, Tuncel A, Raman J, Pearle MS, Lotan Y. Longitudinal evaluation of the SF-36 quality of life questionnaire in patients with kidney stones. Urol Res. 2011;39:141–146. doi: 10.1007/s00240-010-0313-2. [DOI] [PubMed] [Google Scholar]
- 12.Chung SD, Keller JJ, Lin HC. Increased risk of depressive disorder within 1 year after diagnosis with urinary calculi in Taiwan. Psychiatry Res. 2012;198:332–333. doi: 10.1016/j.psychres.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 13.Curhan GC, Willett WC, Rimm EB, Stampfer MJ. A prospective study of dietary calcium and other nutrients and the risk of symptomatic kidney stones. N Engl J Med. 1993;328:833–838. doi: 10.1056/NEJM199303253281203. [DOI] [PubMed] [Google Scholar]
- 14.Penniston KL, Nakada SY. Development of an instrument to assess the health related quality of life of kidney stone formers. J Urol. 2013;189:921–930. doi: 10.1016/j.juro.2012.08.247. [DOI] [PubMed] [Google Scholar]