Abstract
In 2012, the Centers for Disease Control and Prevention launched a national tobacco education campaign, Tips From Former Smokers, that consisted of graphic, emotionally evocative, testimonial-style advertisements. This longitudinal study examines changes in beliefs, tobacco-related cognitions and intentions to quit smoking among U.S. adult smokers after a 12-week airing of the campaign (n=4040 adult smokers pre- and post-campaign). Exposure to the campaign was associated with greater odds of intending to quit within the next 30 days [odds ratio (OR)=1.28, P < 0.01] and within the next 6 months (OR=1.12, P < 0.05), and quit intentions were stronger among respondents with greater campaign exposure (OR=1.12, P < 0.01). Campaign exposure was also associated with significant changes in beliefs about smoking-related risks (ORs=1.15–2.40) and increased worries about health (b=0.30, P < 0.001). Based on study change rates applied to U.S. census data, an estimated 566 000 additional U.S. smokers reported their intention to quit smoking within the next 6 months as a result of viewing campaign advertisements. Campaign effects were consistent with the theory of reasoned action and an expanding body of research demonstrating that graphic, emotional advertisements are highly effective for prompting positive cessation-related cognitions and behavioral intentions.
Introduction
Current cigarette smoking among U.S. adults has declined steadily from 22.5% in 2002 to 18.0% in 2012, but progress has slowed in recent years [1–3]. To reduce adult smoking rates and prevent some of the 480 000 tobacco-related deaths each year [2, 4], the Centers for Disease Control and Prevention (CDC) recommends implementing antismoking mass media campaigns along with other effective interventions for promoting smoking cessation [2, 5]. Evidence from campaign evaluations and controlled field experiments indicates that cessation media campaigns can be used to promote quitting, particularly when they are evidence-based and well-funded [6–12]. For example, evaluations of media campaigns featuring the serious harms of smoking in Australia and New York State found that respondent exposure was associated with increased quit attempts [12, 13]. In the United States, individuals who self-reported exposure to the national `EX' campaign reported increased quit attempts over the campaign period relative to those with no exposure [10], and effects were found for smokers of varying education levels and races/ethnicities [11]. Studies further suggest that media campaigns are more effective when they occur within the context of other tobacco control efforts, such as increased access to cessation aids and services, smoke-free laws, tax increases and school and community programs [6–9, 14–16].
Through funding from the U.S. Patient Protection and Affordable Care Act (2010), CDC launched a national tobacco education campaign, Tips From Former Smokers (Tips), in 2012. The campaign combines the message frame—`the serious health consequences of tobacco use'—with advertisement characteristics that have been linked with improved rates of recall and greater perceived effectiveness [17–19]. These advertisement characteristics include graphic, emotionally evocative, testimonial-style messages in which former smokers describe how tobacco-related illness has reduced their quality of life. Tips advertisements targeted all U.S. adult smokers and promoted evidence-based cessation services accessible by phone (1-800-QUIT-NOW) and Web (Smokefree.gov).
Two studies document the effects of the 2012 Tips campaign. A CDC study found that calls to 1-800-QUIT-NOW increased by 132% and visits to Smokefree.gov increased by 428% during the Tips campaign period [20]. McAfee and colleagues found that Tips was associated with substantial increases in quit attempts among U.S. smokers in 2012; an estimated 1.6 million smokers were motivated by the campaign to make a quit attempt, and 220 000 remained smoke-free at 3-month follow-up [21].
Even as evidence of campaign effectiveness emerges, it is important to understand the mechanism by which campaign advertising influences cessation behavior. In particular, understanding the extent to which campaign-targeted beliefs and cognitions change as a function of campaign exposure may inform the future selection of key messages for adult smoking cessation advertisements. These data may also inform the broader community of practitioners that use Tips media campaign materials for their own state tobacco control programs.
CDC's Best Practices for Comprehensive Tobacco Control Programs and a National Cancer Institute review indicate that beliefs and other tobacco-related cognitions may be the first measurable indicators of antismoking media campaign effectiveness [6, 22], and studies indicate that campaigns have successfully altered these behavioral precursors [10, 11, 23–26]. Behavior change theories suggest that population-level change in behavioral outcomes is preceded by a series of changes in individual-level cognitions and other influences, including beliefs, attitudes, social norms, risk perceptions, intentions and environmental-level influences [27–30]. The theory of reasoned action (TRA) predicts that attitudes and perceptions of social norms, which are a function of beliefs, drive intention to perform specific behaviors and that intention is an antecedent of actual behavior [31]. Consistent with TRA, empirical evidence indicates that beliefs and attitudes, including the perceived health risks of smoking, concerns about the health consequences of smoking, and motivation to quit, predict cessation-related quit intentions and behavioral outcomes, including quit attempts among adult smokers [32–36].
This study used data from a longitudinal cohort of adult smokers to examine early indicators of Tips campaign effectiveness. Three research questions were addressed: (i) Did the campaign change beliefs related to smoking-related illnesses highlighted in Tips advertisements?, (ii) Did the campaign increase cessation-related health worries and motivation to quit smoking? and (iii) Did the campaign increase immediate and longer-term intentions to quit smoking?
Materials and methods
Tips advertisements
Advertisements were developed through a rigorous multistage formative testing and evaluation process described elsewhere [21]. The first set of Tips advertisements aired on national cable television from 19 March 19 to 10 June 2012, in all U.S. media markets with additional advertising buys in select local media markets with known high smoking prevalence. The television campaign was augmented by radio, print, billboard, transit and digital/Web. Additionally, the campaign included Spanish-language advertisement placements (see Appendix A). Advertisements included information on telephone cessation services, which linked callers to their state quitline via the national 1-800-QUIT-NOW telephone portal and an online cessation Website from the National Cancer Institute (www.smokefree.gov). The campaign delivered substantial doses, with an average of 1023 television target rating points (TRPs) per market over 12 weeks, meeting CDC guidelines for effective levels of media campaign delivery [22].
Study design
Data are from a longitudinal online survey of adult smokers. Smokers were recruited from (i) GfK KnowledgePanel (KP) and (ii) the Survey Sampling International (SSI) online panel. All KP smokers were invited to participate via e-mail. KP is statistically representative of the U.S. population and is comparable to national random-digit-dial telephone surveys in terms of demographics and accuracy of self-reported data [37, 38]. KP employs address-based sampling for recruitment and maintenance, and all panelists are sampled with a known probability of selection [37]. To augment statistical power in the KP smoker sample, a sample of pre-identified SSI smokers was also invited via e-mail to participate. The SSI panel is a standard online panel of U.S. adults aged 18+ consisting of volunteer participants. Adults who smoked 100+ lifetime cigarettes and reported now smoking either every day or some days were defined as adult current smokers. The sample was powered to generate national estimates of the study outcomes.
Survey data on smokers from the KP and SSI samples were combined via a calibration weighting procedure to approximate the weighted profile of the KP-only sample. The combined smoker sample yields survey estimates on all study outcomes that are not statistically different from those that would be obtained from the nationally representative KP-only sample. Previous research suggests that this calibration method can improve sample efficiency by increasing statistical power without introducing significant bias [39, 40]. The evaluation protocol was approved by RTI International's institutional review board, and the survey was administered by GfK.
Smokers were surveyed before and after the campaign to assess the relationship between campaign exposure and changes in cessation-related knowledge, beliefs and intentions. At follow-up, all cessation-related outcomes were measured prior to the assessment of campaign exposure. A pre-post longitudinal study design was implemented because Tips advertisements aired nationally, and there was no unex-posed comparison group. The pre-campaign baseline survey was conducted from 21 February to 18 March 2012, with post-campaign follow-up from 11 June to 5 July 2012. A total of 4108 of 5903 KP-recruited smokers and 8049 SSI smokers completed the baseline survey. A larger SSI baseline sample was necessary due to anticipated lower longitudinal retention and survey response among volunteer panels. In total, 5241 smokers completed the follow-up survey [3051 KP smokers (75.5% retention rate) and 2190 SSI-recruited smokers (27.2% retention rate)].
Survey measures
Tips advertisement exposure index
To assess awareness of Tips television advertisements, respondents viewed each advertisement via video streams in the online survey to prompt recall. After viewing each advertisement, participants immediately completed a battery of questions assessing their frequency of exposure to the advertisement in the past 3 months. This process was repeated for seven randomly ordered Tips advertisements (described in Appendix A). A cumulative index of exposure frequency across all advertisements was created to measure total exposure advertisements, defined as the sum of recall frequency (0 = never saw advertisement, 4 = saw advertisement very often) across all seven Tips advertisements. Respondents who saw no advertisements received a value of 0, whereas respondents who saw all seven advertisements `very often' received a value of 28 for frequency of exposure (total range from 0 to 28). All respondents were assigned a frequency of exposure = 0 at pre-campaign because exposure was measured only post-campaign.
Beliefs about smoking-related health conditions and risk perceptions
Smokers' beliefs about the health effects of cigarette smoking highlighted in Tips advertisements were assessed. Respondents were asked `Do you believe cigarette smoking is related to …' heart disease, stroke, tracheotomy, Buerger's disease or amputations of limbs and asthma (yes/no). Smokers were also asked to indicate their agreement (dichotomized for `agree'/`strongly agree' versus `neither'/`disagree'/`strongly disagree') with the statement corresponding to a key Tips message, `Smoking can cause immediate damage to your body'.
Worries about health and motivation to quit
Two previously validated scales [40] were used to assess worries about health and motivation to quit. The worries about health scale assessed smokers' worries about the damage that smoking may do to their health and feelings of worry or disappointment when thinking about their own smoking. The scale included five items with 4-point Likert response scales: (i) How worried are you that smoking will damage your health in the future?; (ii) I get upset when I think about my smoking; (iii) I am disappointed in myself because I smoke; (iv) I get upset when I hear or read about illnesses caused by smoking and (v) warnings about the health risks of smoking upset me. Response options were from `not at all worried' to `very worried' for the first item and from `strongly disagree' to `strongly agree' for the remaining items. The motivation to quit scale measured smokers' overall desire and eagerness to quit smoking and included three items with 4-point response scales: (i) How much do you want to quit smoking? (`not at all' to `a lot'); (ii) I am eager for a life without smoking (`strongly disagree' to `strongly agree') and (iii) How would you rate quitting as a priority in your life? (`lowest priority' to `highest priority'). Each scale was created as the linear sum of each constituent item divided by the number of items. Factor analysis conducted for each scale showed strong one-factor solutions and significant factor loadings for each item in the scales. Cronbach's alpha coefficients were 0.87 for the worries about health scale and 0.87 for the motivation to quit scale.
Intentions to quit smoking
Two intermediate-term cognitive predictors of cessation were examined. Intention to quit in the next 30 days was defined as a dichotomous indicator variable for responding either `In the next 7 days' or `In the next 30 days' to the question `Do you plan to quit smoking for good …?' Intention to quit in the next 6 months was measured with the same question, using an indicator variable for answering in the next 7 days, next 30 days, or next 6 months.
Potential confounders
Our analysis included a range of covariates similar to those used in other studies of the impact of media campaigns on smoking-related outcomes [12, 24]. Baseline individual characteristics included age (continuous measure); an indicator for female (male excluded as the reference); indicators for African American, Hispanic and other race (white excluded as the reference); indicators for yearly household income of $20 000–$50 000, $50 000–$100 000 and $100 000 or more (<$20 000 excluded as the reference); experience taking tobacco-related surveys; sample source (KP or SSI); cigarette addiction (measured as total minutes until first cigarette after waking); presence of household smokers; daily television hours to account for media use habits (continuous measure); presence of children in household; self-reported chronic medical condition and self-reported mental health condition. State and media market-level covariates include 2010 state per capita tobacco program funding (in 100s of dollars), 2012 state cigarette excise taxes (in dollars), media market population size, media market median income (in tens of thousands of dollars) and proportion of media market with educational attainment of bachelor's degree or higher.
Statistical analyses
Relationship between cognitive precursors and behavioral change
The intermediate cognitive outcomes described in this study were hypothesized by campaign planners a priori as behavioral antecedents potentially affected by the Tips campaign, consistent with TRA predictions [41]. To confirm the predictive qualities of these outcomes, multivariate regression models were used to estimate the odds of making at least one quit attempt at follow-up as a function of the cognitive outcomes at baseline. Each model included a control variable for baseline quit attempts plus covariates for the confounders described above.
Impact of Tips campaign on cognitive precursors
Using the pooled baseline and follow-up data, regression models (logistic regressions for dichotomous outcomes and ordinary least squares regressions for continuous outcomes) were estimated to predict pre- to post-campaign population changes in each cognitive outcome. Each outcome was regressed on a dichotomous indicator for the post-campaign period, advertisement exposure index, interaction between post-campaign period and the advertisement exposure index, and covariates for all confounders described earlier (see Appendix B for full study models with covariates). The post-campaign indicator variable indicates the extent of pre-post change in each outcome over the 3-month campaign and absent other significant competing national interventions [21]. The interaction term indicates dose-response effects, whether the pre-post shift in each outcome was significantly greater among individuals with more frequent exposure to the campaign. The frequency of exposure index is centered with values expressed as the difference from their mean.
Each model contains two observations per participant (pre- and post- campaign); thus, the data are structured as a longitudinal panel clustered on unique individuals and ordered on time. To account for this correlation structure, models were estimated using Stata's `xtlogit' (for dichotomous outcomes) or `xtreg' (for continuous outcomes) commands to fit population-average logistic and least squares regressions. Although our study was not powered to detect effects among subgroups, exploratory analyses of interaction effects and stratified models assessed the moderation of campaign effects on 30-day quit intentions by age, ethnic origin, education and cigarette consumption. Because less than 1.7% of the analytic sample had missing observations on any outcomes, we excluded participants with missing data rather than imputing missing data values. Diagnostic analyses indicated that the models fit the data adequately with minimal evidence of variance inflation or multicollinearity. All models were weighted to reflect U.S. demographics and to account for attrition from baseline.
To yield U.S. population estimates, we applied the rates of change in the KP and SSI sample with and without the Tips campaign and national smoker prevalence data from the 2012 National Health Interview Survey [42] to U.S. Census data [43] to derive the total estimated number of national smokers intending to quit in the next 6 months as a result of Tips.
Results
Sample characteristics
The longitudinal sample consisted of 5241 smokers who completed each survey wave. The unweighted sample contained slightly fewer young smokers aged 18–24 and slightly more older smokers aged 55 or older at follow-up compared with baseline (Table I). In addition, more smokers with very low levels of cigarette addiction and more smokers with a mental health condition completed baseline compared with follow-up (Table I).
Table I.
Demographic and smoking-related characteristics of study sample of smokers
| Unweighted % |
Weighted % |
|||
|---|---|---|---|---|
| Characteristic | Pre-campaign baseline | Post-campaign follow-up | Pre-campaign baseline | Post-campaign follow-up |
| Age (%) | ||||
| 18–24 | 9.0 | 6.9 *** | 11.9 | 11.5 |
| 25–34 | 18.1 | 14.4 *** | 22.5 | 22.9 |
| 35–54 | 39.9 | 41.8 ** | 38.8 | 39.7 |
| 55+ | 33.1 | 36.9 *** | 26.8 | 25.9 |
| Gender (%) | ||||
| Male | 40.1 | 42.2 | 50.0 | 52.0 |
| Female | 59.9 | 57.8 | 50.0 | 48.0 |
| Race/ethnicity (%) | ||||
| White | 77.4 | 77.9 | 67.1 | 65.0 |
| Black | 7.9 | 7.7 | 12.7 | 13.9 |
| Hispanic | 7.9 | 7.8 | 12.0 | 12.4 |
| Asian | 1.8 | 1.9 | 2.5 | 2.7 |
| Other | 5.1 | 4.8 | 5.7 | 5.9 |
| Educational attainment (%) | ||||
| Less than high school | 6.6 | 6.4 | 17.6 | 19.8 |
| High school graduate | 24.8 | 24.0 | 38.9 | 38.8 |
| Some college | 47.8 | 46.1 | 31.6 | 30.1 |
| College graduate+ | 20.9 | 23.5 | 11.8 | 11.4 |
| Household income (%) | ||||
| <$20 000 | 26.2 | 24.9 | 37.6 | 35.3 |
| $20 000–$49 999 000 | 36.1 | 36.6 | 36.3 | 36.7 |
| $50 000–$99 999 000 | 24.3 | 24.7 | 18.4 | 19.1 |
| $100 000+ | 13.4 | 13.8 | 7.8 | 9.0 |
| Self-reported number tobacco surveys in past year | ||||
| Baseline mean number tobacco surveys | 0.61 | 0.85 *** | 0.72 | 1.02 *** |
| Time to first cigarette after waking (%) | ||||
| Within 5 min | 25.6 | 24.3 | 26.2 | 26.3 |
| 6–30 min | 43.0 | 42.6 | 41.3 | 39.8 |
| More than 30 min to 1 h | 15.7 | 14.9 | 15.4 | 14.8 |
| After more than 1 h | 15.8 | 18.2 *** | 17.1 | 19.2 *** |
| Tv hours per day (%) | ||||
| 1 or more hours | 93.0 | 92.8 | 92.5 | 92.0 |
| Children in the household (%) | ||||
| 1 or more | 35.2 | 32.3 | 38.9 | 38.2 |
| Has a mental health condition (%) | ||||
| Yes | 34.2 | 29.7 *** | 33.4 | 29.6 *** |
| Another smoker in the household (%) | ||||
| Yes | 46.2 | 41.0 *** | 48.8 | 43.3 *** |
Note:
P<0.05,
P<0.01,
P<0.001 for statistically significant difference between follow-up and baseline. Pre-campaign baseline survey conducted 21 February to 18 March 2012. Post-campaign follow-up conducted from 11 June to 5 July 2012. A total of 12 157 smokers completed the baseline survey and 5241 smokers completed the follow-up survey. Unweighted statistics represent raw proportions of each characteristic in the sample. Weighted statistics represented adjusted proportions that have been weighted to reflect national Census benchmarks in the population.
Campaign awareness and frequency of exposure
Overall, 78.5% of smokers recalled seeing at least one Tips advertisement on television. On average, smokers reported seeing 2.5 of the 7 television advertisements that aired, and 40.3% reported seeing at least one Tips advertisement `often' or `very often'. The mean score for the frequency of exposure index used in multivariate analysis was 5.9.
Baseline cognitive precursors and quit attempts
Results from logistic regression models indicated that the odds of a quit attempt at follow-up was a function of 8 of the 10 cognitive precursors examined in this study. As measured at baseline, three of the five items assessing smokers' knowledge of specific smoking-related health conditions (heart disease, tracheotomy, Buerger's/amputations) predicted quit attempts at follow-up (ORs 1.39–1.48, P < 0.05). The belief that smoking causes immediate damage to the body was also predictive of quit attempts [odds ratio (OR) = 1.64, P < 0.001], as were worries about health (b = 0.09, P < 0.001) and motivation to quit (b = 0.11, P < 0.01). Quit intentions at baseline (30-day OR = 2.58, P < 0.001; 6-month OR = 2.94, P < 0.001) were predictive of quit attempts at follow-up.
Smokers' beliefs about smoking-related health conditions and risk perceptions
The proportion of smokers that believe smoking is associated with the smoking-related health conditions highlighted by Tips advertisements increased significantly at follow-up (P < 0.05). Knowledge of health conditions that are novel or less commonly associated with smoking increased more between baseline and follow-up than those more commonly associated with smoking. For example, from baseline to follow-up, knowledge of risks from Buerger's disease or amputations increased from 27.4% to 47.1%, knowledge of stroke increased from 66.1% to 75.6%, and knowledge of tracheotomy increased from 76.9% to 84.6%. Pre-post changes observed for diseases more commonly associated with smoking were smaller (heart disease: 82.9–84.8%; asthma: 77.6–80.3%). Smokers' belief that smoking can cause immediate damage to the body also increased significantly between baseline (23.1%) and follow-up (26.8%; P < 0.05).
Logistic regression models show significant pre-post increases in the odds of each belief about specific health conditions at follow-up (ORs = 1.15–2.40) and the belief that smoking causes immediate damage to the body (OR = 1.21, P < 0.01; Table II). In addition, a significant interaction between frequency of exposure and the post-campaign period was observed for knowledge of Buerger's disease or amputations (OR = 1.22, P < 0.001), indicating a dose-response relationship between Tips exposure and this belief (Table II).
Table II.
Multivariate logistic regressions for Tips exposure and smoking-related beliefs
| Cigarette smoking is related to
… |
||||||
|---|---|---|---|---|---|---|
| Heart disease OR (95% CI) | Stroke OR (95% CI) | Tracheotomy OR (95% CI) | Buerger's/amputation OR (95% CI) | Asthma OR (95% CI) | Smoking causes immediate damage OR (95% CI) | |
| Main effect model independent variable | ||||||
| Post-campaign period | 1.14 (0.99, 1.31) | 1.58 (1.41, 1.78)*** | 1.64 (1.44, 1.87)*** | 2.38 (2.13, 2.65)*** | 1.13 (0.99, 1.29) | 1.19 (1.05, 1.34)** |
| Interaction model independent variable | ||||||
| Post-campaign period | 1.16 (1.01, 1.33)* | 1.60 (1.41, 1.80)*** | 1.66 (1.45, 1.90)*** | 2.40 (2.15, 2.68)*** | 1.15 (1.01, 1.31)* | 1.21 (1.07, 1.36)** |
| Frequency of exposure | 1.05 (0.96, 1.15) | 1.18 (1.09, 1.27)*** | 1.12 (1.03, 1.21)** | 1.13 (1.05, 1.22)*** | 1.07 (0.99, 1.16)+ | 1.10 (1.02, 1.19)** |
| Time × frequency of exposure | 1.04 (0.94, 1.15) | 1.08 (0.98, 1.19) | 1.05 (0.95, 1.16) | 1.22 (1.13, 1.32)*** | 1.06 (0.97, 1.16) | 1.03 (0.95, 1.12) |
Note: All models include the individual-level covariates age, gender, race/ethnicity, household income, experience taking tobacco-related surveys, sample source (KP or SSI), cigarette addiction, presence of household smokers, daily television hours, presence of children in household, self-reported chronic medical condition and self-reported mental health condition. All models also include the state and media market-level covariates 2010 state per capita tobacco program funding, 2012 state cigarette excise taxes, media market population size, media market median income and proportion of media market with educational attainment of bachelor's degree or higher.
P<0.05,
P<0.01,
P<0.001
Smokers' worries about health and motivation to quit
Smokers' mean scores for the worries about health scale increased significantly between baseline (2.6) and follow-up (2.7) (P < 0.05), while motivation to quit did not. Results from multivariate analysis were consistent with these descriptive patterns as pre-post time was associated with a statistically significant increase in worries about health (b = 0.06, P < 0.001); the interaction coefficient suggests this increase was more substantial among smokers with more frequent exposure to campaign advertisements (b = 0.02, P < 0.05) (Table III). Although pre-post time was not associated with motivation to quit among the general population of smokers, the interaction between time and self-reported exposure frequency suggests that change was greater among smokers who saw Tips advertisements more often (b = 0.03, P < 0.01; see Table III).
Table III.
Multivariate linear and logistic regressions for Tips exposure and quit motivation, worries about health, and intentions
| Motivation to quit |
Worries about health |
Quit in next 30 days |
Quit in next 6 months |
|
|---|---|---|---|---|
| Coefficient (95% CI) | Coefficient (95% CI) | OR (95% CI) | OR (95% CI) | |
| Main effect model independent variable | ||||
| Post-campaign period | 0.01 (−0.02, 0.04) | 0.06 (0.04, 0.09) *** | 1.28 (1.11, 1.49) *** | 1.13 (1.03, 1.25) * |
| Interaction model independent variable | ||||
| Post-campaign period | 0.01 (−0.02, 0.03) | 0.06 (0.03, 0.09) *** | 1.28 (1.10, 1.49) ** | 1.12 (1.01, 1.24) * |
| Frequency of exposure | 0.05 (0.03, 0.07)*** | 0.04 (0.02, 0.06)*** | 1.08 (0.99, 1.17) | 1.10 (1.03, 1.17)** |
| Time × frequency of exposure | 0.03 (0.01, 0.05)** | 0.02 (0.00, 0.04)* | 1.09 (0.99, 1.20) | 1.12 (1.05, 1.20)** |
Note: All models include the individual-level covariates age, gender, race/ethnicity, household income, experience taking tobaccorelated surveys, sample source (KP or SSI), cigarette addiction, presence of household smokers, daily television hours, presence of children in household, self-reported chronic medical condition and self-reported mental health condition. All models also include the state and media market-level covariates 2010 state per capita tobacco program funding, 2012 state cigarette excise taxes, media market population size, media market median income and proportion of media market with educational attainment of bachelor's degree or higher.
P<0.05,
P<0.01,
P<0.001
Smokers' intentions to quit
Intentions to quit in the next 30 days increased significantly from baseline (15.4%) to follow-up (18.9%; P < 0.05), as did intentions to quit in the next 6 months (36.9–40.1%; P < 0.05). Figure 1 displays mean intentions to quit at baseline and follow-up as a function of exposure to Tips. Pre-post changes in quit intentions were greater with increasing frequency of recall of exposure. Importantly, results from multivariate analysis were consistent with these observed changes (see Table III). Post-campaign period was associated with increased odds of intending to quit in the next 30 days (OR = 1.28, P < 0.01). Pre-post changes in 30-day quit intentions were greater with increasing frequency of advertisement exposure (OR = 1.09, P = 0.05). Post-campaign period was also associated with increased intentions to quit in the next 6 months (OR = 1.12, P < 0.05), and the change was greater among smokers who saw Tips advertisements more often (OR = 1.12, P < 0.0015; see Table III). Based on study change rates applied to U.S. census data, an estimated 566 000 additional U.S. smokers reported intentions to quit smoking within the next 6 months.
Fig. 1.
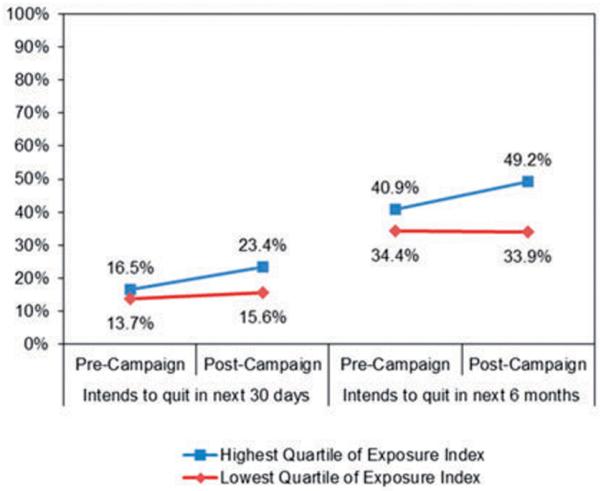
Percentage of smokers with 30-day and 6-month quit intentions by frequency of exposure to Tips, pre- and post-campaign.
Discussion
Three months after campaign launch in March 2012, smokers' exposure to Tips advertising was associated with greater odds of intending to quit within the next 30 days and within 6 months. An interaction effect indicates that the relationship between campaign exposure and intention to quit within 6 months was greater among smokers with higher levels of campaign exposure recall. An estimated 566 000 additional U.S. smokers reported intentions to quit smoking within the next 6 months as a result of viewing campaign advertisements.
Campaign exposure was also associated with significant changes in beliefs about smoking-related risks and increased worries about health. For example, exposure to Tips advertising was associated with a nearly 20% point increase in the proportion of adult smokers who correctly reported that smoking is associated with Buerger's disease or amputation. Knowledge of other negative health outcomes associated with smoking—including stroke, tracheotomy, heart disease and asthma—also increased significantly among those exposed to campaign advertising, although increases were smaller in part because of higher baseline levels of knowledge. Corroborating this evidence of a campaign effect on smoking-related cognitions, a five-item scale indicated that exposure was associated with increased worries about health.
This study adds to the growing body of evidence about the effectiveness of hard-hitting, emotionally evocative media campaigns [9, 12, 13, 32, 44] and supports and expands on previous research about the effectiveness of the Tips campaign [21]. These findings provide insight into the potential pathways through which Tips motivated smokers to attempt to quit [21]. The campaign successfully targeted specific cognitive factors (e.g., increasing smokers' concern for their health) that were theorized to affect cessation behavior and highlighted these factors in its messages. These results indicate that not only was the Tips campaign associated with changes in these cognitive precursors, but that these precursors were predictive of quit attempts in longitudinal analysis. Consistent with theories of behavior change, shifts in smoking and cessation-related cognition precursors as a result of Tips may positively impact future cessation behaviors. This study, combined with recent research showing that a substantial increase in quit attempts among U.S. smokers was associated with the campaign [20], suggests the Tips campaign successfully implemented a message strategy grounded in TRA and theories of behavior change, producing effects consistent with their predictions. This study suggests that the long-term impact of Tips on U.S. smoking behaviors may be larger than the effects described in earlier evaluation studies [20].
A major strength of this study is our use of longitudinal data to confirm that smokers' tobacco-related cognitions predict a range of cessation-related outcomes. In light of the national context within which the Tips campaign was implemented and evaluated, this cohort study provides evidence that observed campaign effects are likely causal. Specifically, the observed changes in outcomes occurred during a relatively short time frame in the absence of any other known large-scale interventions at the national level that could have produced similar effects [21]. Evidence of dose-response effects on smokers' intentions to quit, over and above the average population-level shifts, provides further support for causality.
This study has several limitations. First, the results may not be fully representative of U.S. smokers given the use of mixed sample sources. However, comparisons of demographic benchmarks based on the U.S. Census suggest that the calibrated KP and SSI combined sample is not significantly different from the weighted KP-only sample. Furthermore, multivariate analyses using the KP-only smoker sample yielded qualitatively similar results in direction and magnitude (e.g., 11 of the 14 statistically significant effects shown in Tables II and III remained significant), indicating that the additional SSI sample does not introduce significant bias in the study results. Second, although follow-up data are weighted to account for its effects, sample attrition limits these data. Studies show that online surveys suffer from greater respondent attrition than other types of studies [45, 46] but that attrition does not necessarily indicate bias [47]. Third, observed dose-response effects are based on self-reported measure of exposure, which can be subject to selective attention biases. Although an exogenous market-level measure of campaign delivery such as TRPs would have been preferable for establishing dose-response, the broad national coverage of the Tips campaign precluded any substantial variation in geographic-based measures of campaign delivery. Fourth, broad campaign coverage precluded the use of a non-exposed control study; thus, causal effects of the campaign must assume no other temporal differences between baseline and follow-up surveys. Evidence indicates no other large-scale media campaigns, interventions or policy changes occurred before or during the study period [21], and control variables for state-level cigarette taxes and tobacco prevention funding were included to account for known influences. The dose-response findings in this paper further support causal attribution of effects to the campaign.
In summary, this study provides important evidence that the Tips campaign influenced smoking-related cognitions, increased worries about health, and led to greater cessation intentions among U.S. smokers. The campaign highlighted specific health effects messages that were predicted to influence behavior change. Study results indicate that the campaign impacted these important cognitive precursors that are predictive of changes in cessation behavior. Findings are consistent with an expanding body of research demonstrating that hard-hitting, graphic, and emotional advertisements are effective at changing cessation-related outcomes. A major strength of this study is our use of longitudinal data to show that smokers' cognitions may be antecedent to a range of relevant cessation-related outcomes. Furthermore, evidence of population-level shifts in behavioral intentions along with dose-response effects as campaign exposure increases is encouraging. Given evidence that the withdrawal of media campaigns has been associated with a decline in beneficial effects [12], airing smoking cessation mass media campaigns with greater frequency and consistency across the United States would be expected to have even greater impact. Continuous airing of effective cessation campaigns could help to decrease the prevalence of smoking and reduce the burden of smoking-attributable mortality in the United States [2, 48].
Acknowledgements
This article is dedicated to Terrie Hall of Lexington, North Carolina, who passed away on Monday, 16 September 2013, and to Nathan Moose, of the Oglala Sioux tribe, who passed away 17 October 2013. Terrie and Nathan appeared in the Tips campaign and were instrumental in encouraging smokers to try to quit. Their willingness to show how smoking and secondhand smoke affected their lives in order to save others from such hardship revealed their courage, strength, and compassion. They were a source of inspiration to those who knew them and to those who viewed their advertisements. Special thanks to the following CDC staff who contributed to the Tips From Former Smokers campaign: For campaign oversight: Tim McAfee and Jane Mitchko. For scientific, programmatic, and technical support: Rebecca Bunnell; Terry Pechacek; William Marx; Gabbi Promoff; Karen Debrot and Renita Macaluso. For mobilizing CDC support and providing scientific support: Ursula Bauer and Thomas Frieden. For overall support: CDC's Office on Smoking and Health. Thanks also to Paul Shafer, MA, of RTI International for data analysis and technical support as well as the PlowShare Group for executing the media campaign.
Funding This work was supported by the Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, contract no. 200-2007-20016.
Appendix A.
| Advertisement name/mean exposured | Description/available at |
|---|---|
| Anthem Advertisement: mean exposure=1.1 | Three people with stomas provide tips on how to live with the consequences of their smoking. Tips include `When you have a hole in your neck, don't face the showerhead', `Suction out your tube before you eat,' `Crouch, don't bend over. You don't want to lose the food in your stomach' and `CPR is not mouth to mouth; it's mouth to stoma'. Then text on the screen reads, `Smoking causes immediate damage to your body', http://www.youtube.com/watch?v=GEWky9PEroU&list=PL184B81EA3136E9FE&index=15 |
| Terrie's Advertisement: mean exposure=1.4 | `Terrie's Advertisement' profiles a woman named Terrie who had throat cancer due to smoking, treatment of which caused her to lose her teeth and hair and to have her larynx (voice box) removed. With the aid of an electrolarynx, she talks the viewer through how she gets ready for the day by inserting her hands-free device, putting in her teeth, and putting on a wig. Text then reads, `Smoking causes immediate damage to your body'. http://www.youtube.com/watch?v=5zWB4dLYChM&list=PL184B81EA3136E9FE&index=16 |
| Suzy's Advertisement: mean exposure=1.0 | In `Suzy's Advertisement', a woman named Suzy, who has suffered from a stroke caused by smoking, talks about losing her independence as her son helps wash her. She describes how she needs help with feeding, dressing, bathing, and even going to the bathroom. Her tip to smokers is `Enjoy your independence now'. Text then reads, `Smoking contributes to 1 in 5 strokes in the United States'. http://www.youtube.com/watch?v=ow5uw_iCm5A&list=PL184B81EA3136E9FE&index=17 |
| Roosevelt's Advertisement: mean exposure=0.8 | `Roosevelt's Advertisement' features a man named Roosevelt who had a heart attack at age 45 due to his smoking. He discusses the effect the heart attack has had on his life and how he did not know smoking could damage his heart. He shows a large scar on his chest from surgery and gives viewers this tip: `Do your heart a favor and quit now'. Text then reads, `Your heart attack risk drops as soon as you quit smoking'. http://www.youtube.com/watch?v=OdmI35elnCQ&list=PL184B81EA3136E9FE&index=18 |
| Buerger's Disease Advertisement: mean exposure=0.8 | The Buerger's disease advertisement profiles Brandon and Marie, two former smokers who are living with Buerger's disease as a result of their smoking. The disease can lead to amputations, which both of these individuals have experienced. Brandon, age 31, has lost both legs below the knee, while Marie, age 61, is missing fingers and parts of her feet. Marie tells viewers `Don't believe that this can't happen to you, because it can'. Then text on the screen reads, `Smoking causes immediate damage to your body', http://www.youtube.com/watch?v=-WrWwUsKKN8&list=PL184B81EA3136E9FE&index=22 |
| Jessica's Asthma Advertisementb,c: mean exposure=0.4 | This advertisement features a tip about secondhand smoke by Jessica and her son who suffers from asthma attacks due to secondhand smoke exposure. In her tip, she urges people `Don't be shy to tell people not to smoke around your kids'. Then text then reads, `Half of U.S. kids are exposed to secondhand smoke'. http://www.youtube.com/watch?v=3eUOjSTZMIE&list=PL184B81EA3136E9FE&index=19 |
| Cessation Tips Advertisementb: mean exposure=0.3 | The `Cessation Tips' advertisement features three people who successfully quit smoking after many years. They share practical tips, such as, `I threw away all my cigarettes, ashtrays, and lighters', `I started exercising instead of smoking', and `Letting my friends online know I was quitting kept me on track'. The advertisement ends with one of them saying `We did it; you can, too'. http://www.youtube.com/watch?v=d6iS44aHy4s&list=PL184B81EA3136E9FE&index=21 |
The advertisements shown above included 30-second advertisements made for television and may have also had print, out-of-home (billboard/bus shelter), radio and digital executions. In addition to the seven television advertisements listed, five other people appeared in/on print, digital radio and out-of-home advertisements only.
Jessica's English advertisement and the Cessation Tips advertisement were produced as public service announcements, complementing the paid media campaign.
All advertisements aired in English language; Jessica's Asthma advertisement also aired in Spanish language.
Mean exposure is the average self-reported frequency of exposure to each individual advertisement in the past 3 months as assessed at follow-up (0=never saw advertisement, 4=saw advertisement very often).
Appendix B Multivariate logistic regressions for Tips exposure and study outcomes
Table BI.
Multivariate logistic regression main effect models for Tips exposure and smoking-related beliefs
| Independent variable | Cigarette smoking is related to… | |||||
|---|---|---|---|---|---|---|
| Heart disease OR (95% CI) | Stroke OR (95% CI) | Tracheotomy OR (95% CI) | Buerger's/amputation OR (95% CI) | Asthma OR (95% CI) | Smoking causes immediate damage OR (95% CI) | |
| Post-campaign period | 1.14 (0.99, 1.31)+ | 1.58 (1.41, 1.78)*** | 1.64 (1.44, 1.87)*** | 2.38 (2.13, 2.65)*** | 1.13 (0.99, 1.29)+ | 1.19 (1.05, 1.34)** |
| Age | 1.00 (1.00, 1.01) | 1.00 (0.99, 1.01) | 0.98 (0.97, 0.99)*** | 1.00 (0.99, 1.00) | 0.98 (0.98, 0.99)*** | 0.99 (0.99, 1.00)* |
| High school graduate | 1.53 (1.08, 2.16)* | 1.47 (1.12, 1.95)** | 1.25 (0.89, 1.74) | 1.16 (0.88, 1.53) | 0.95 (0.69, 1.32) | 0.93 (0.69, 1.25) |
| Achieved some college | 1.72 (1.23, 2.40)** | 2.11 (1.61, 2.76)*** | 1.53 (1.11, 2.11)** | 1.05 (0.82, 1.36) | 1.08 (0.79, 1.48) | 0.77 (0.58, 1.01)+ |
| Earned college degree or more | 1.89 (1.30, 2.73)*** | 2.57 (1.90, 3.48)*** | 1.55 (1.09, 2.21)* | 1.39 (1.05, 1.85)* | 1.13 (0.80, 1.59) | 0.80 (0.59, 1.09) |
| Male | 0.99 (0.80, 1.24) | 0.89 (0.75, 1.06) | 0.93 (0.76, 1.12) | 0.84 (0.72, 0.99)* | 0.79 (0.66, 0.95)* | 0.76 (0.64, 0.91)** |
| White race | 0.98 (0.63, 1.55) | 1.33 (0.96, 1.84)+ | 0.97 (0.66, 1.44) | 1.20 (0.89, 1.63) | 1.19 (0.82, 1.72) | 0.71 (0.51, 0.98)* |
| African American race | 0.99 (0.57, 1.71) | 1.53 (1.01, 2.33)* | 1.07 (0.63, 1.82) | 1.56 (1.07, 2.29)* | 1.07 (0.66, 1.73) | 1.09 (0.72, 1.65) |
| Hispanic race | 1.10 (0.63, 1.93) | 0.88 (0.59, 1.31) | 1.17 (0.70, 1.94) | 1.60 (1.09, 2.37)* | 1.42 (0.88, 2.28) | 1.15 (0.76, 1.74) |
| Annual income ≥$20 000 and <$50 000 |
1.03 (0.72, 1.49) | 1.78 (1.34, 2.36)*** | 1.03 (0.75, 1.39) | 1.03 (0.79, 1.35) | 1.33 (0.97, 1.82)+ | 0.75 (0.55, 1.02)+ |
| Annual income ≥$50 000 and <$100 000 |
1.51 (1.00, 2.28)* | 1.78 (1.29, 2.45)*** | 0.98 (0.68, 1.42) | 0.82 (0.61, 1.10) | 1.10 (0.79, 1.54) | 0.84 (0.59, 1.18) |
| Annual income ≥$100 000 | 0.84 (0.49, 1.45) | 1.20 (0.79, 1.81) | 0.85 (0.54, 1.34) | 0.76 (0.52, 1.09) | 0.82 (0.54, 1.24) | 0.89 (0.55, 1.44) |
| Tobacco surveys taken past year | 1.01 (0.92, 1.10) | 1.08 (1.00, 1.16)* | 1.00 (0.92, 1.09) | 0.98 (0.92, 1.05) | 1.02 (0.94, 1.11) | 0.95 (0.89, 1.03) |
| Media market population size | 0.91 (0.45, 1.81) | 0.59 (0.36, 0.98)* | 0.83 (0.44, 1.56) | 1.05 (0.65, 1.68) | 0.84 (0.46, 1.55) | 0.92 (0.52, 1.64) |
| Median income in media market | 1.19 (0.98, 1.44)+ | 1.08 (0.94, 1.23) | 1.11 (0.94, 1.30) | 1.13 (0.99, 1.28)+ | 1.12 (0.97, 1.29) | 1.13 (0.98, 1.30)+ |
| Percentage of media market with college degree |
0.99 (0.95, 1.02) | 1.00 (0.98, 1.03) | 0.99 (0.96, 1.02) | 0.98 (0.96, 1.00) | 0.99 (0.96, 1.02) | 0.98 (0.95, 1.01) |
| State per capita tobacco control funding |
1.62 (0.75, 3.48) | 1.55 (0.88, 2.76) | 1.74 (0.91, 3.33)+ | 1.53 (0.91, 2.56) | 1.60 (0.91, 2.84) | 1.79 (0.98, 3.26)+ |
| State cigarette tax | 1.04 (0.93, 1.18) | 1.06 (0.97, 1.16) | 1.08 (0.98, 1.18) | 1.13 (1.05, 1.23)** | 1.01 (0.93, 1.11) | 1.03 (0.94, 1.13) |
| Time to first cigarette (in minutes) | 1.02 (0.91, 1.13) | 0.98 (0.90, 1.06) | 1.05 (0.96, 1.15) | 1.02 (0.95, 1.11) | 1.01 (0.93, 1.10) | 0.95 (0.87, 1.04) |
| Daily hours of television | 1.06 (0.98, 1.14) | 1.04 (0.98, 1.11) | 1.07 (1.00, 1.15)+ | 1.01 (0.96, 1.07) | 1.06 (0.99, 1.13)+ | 1.10 (1.03, 1.17)** |
| Other smoker in household | 0.92 (0.74, 1.14) | 0.91 (0.77, 1.07) | 1.04 (0.86, 1.26) | 1.05 (0.90, 1.23) | 1.06 (0.88, 1.27) | 0.87 (0.73, 1.04) |
| Children in household | 0.99 (0.78, 1.26) | 1.01 (0.83, 1.22) | 0.99 (0.79, 1.24) | 1.14 (0.96, 1.36) | 1.17 (0.96, 1.43) | 1.21 (1.00, 1.46)+ |
| Has a mental health condition | 1.54 (1.18, 2.01)** | 1.37 (1.11, 1.70)** | 1.30 (1.02, 1.64)* | 1.12 (0.91, 1.38) | 1.4 (1.13, 1.72)** | 1.01 (0.81, 1.27) |
| Has a non-mental chronic health condition |
1.68 (1.25, 2.25)*** | 1.29 (1.03, 1.62)* | 1.24 (0.95, 1.61) | 1.20 (0.97, 1.49) | 1.6 (1.23, 2.06)*** | 1.34 (1.07, 1.69)* |
| KP Panel | 1.05 (0.78, 1.41) | 0.73 (0.58, 0.91)** | 1.07 (0.84, 1.37) | 1.20 (0.96, 1.50) | 1.17 (0.89, 1.52) | 0.79 (0.62, 1.02)+ |
| Model N | 10 108 | 10 106 | 10 114 | 10 195 | 10 101 | 10 153 |
Note:
P<0.10,
P<0.05,
P<0.01,
P<0.001.
Reference categories for education, race, and income indicators are less than high school, other race, and income <$20 000, respectively.
Table BII.
Multivariate logistic regression interaction effect models for Tips exposure and smoking-related beliefs
| Cigarette smoking is related to
… |
||||||
|---|---|---|---|---|---|---|
| Independent variable | Heart disease OR (95% CI) | Stroke OR (95% CI) | Tracheotomy OR (95% CI) | Buerger's/amputation OR (95% CI) | Asthma OR (95% CI) | Smoking causes immediate damage OR (95% CI) |
| Post-campaign period | 1.16 (1.01, 1.33)* | 1.60 (1.41, 1.80)*** | 1.66 (1.45, 1.90)*** | 2.40 (2.15, 2.68)*** | 1.15 (1.01, 1.31)* | 1.21 (1.07, 1.36)** |
| Frequency of exposure | 1.05 (0.96, 1.15) | 1.18 (1.09, 1.27)*** | 1.12 (1.03, 1.21)** | 1.13 (1.05, 1.22)*** | 1.07 (0.99, 1.16)+ | 1.10 (1.02, 1.19)** |
| Time × frequency of exposure | 1.04 (0.94, 1.15) | 1.08 (0.98, 1.19) | 1.05 (0.95, 1.16) | 1.22 (1.13, 1.32)*** | 1.06 (0.97, 1.16) | 1.03 (0.95, 1.12) |
| Age | 1.00 (1.00, 1.01) | 1.00 (0.99, 1.00) | 0.98 (0.97, 0.99)*** | 1.00 (0.99, 1.00) | 0.98 (0.98, 0.99)*** | 0.99 (0.98, 1.00)* |
| High school graduate | 1.59 (1.12, 2.26)** | 1.54 (1.16, 2.03)** | 1.29 (0.93, 1.81) | 1.25 (0.95, 1.65) | 0.99 (0.71, 1.37) | 0.99 (0.73, 1.33) |
| Achieved some college | 1.77 (1.27, 2.47)*** | 2.21 (1.69, 2.89)*** | 1.58 (1.15, 2.19)** | 1.13 (0.87, 1.46) | 1.11 (0.81, 1.52) | 0.81 (0.61, 1.07) |
| Earned college degree or more | 1.96 (1.36, 2.84)*** | 2.76 (2.03, 3.75)*** | 1.63 (1.15, 2.33)** | 1.55 (1.17, 2.05)** | 1.18 (0.83, 1.66) | 0.86 (0.64, 1.17) |
| Male | 1.00 (0.80, 1.25) | 0.92 (0.78, 1.09) | 0.96 (0.79, 1.16) | 0.88 (0.75, 1.03) | 0.80 (0.67, 0.96)* | 0.79 (0.66, 0.94)** |
| White race | 1.00 (0.63, 1.57) | 1.38 (0.99, 1.91)+ | 1.00 (0.67, 1.47) | 1.29 (0.95, 1.75) | 1.22 (0.84, 1.76) | 0.74 (0.53, 1.03)+ |
| African American race | 0.98 (0.56, 1.71) | 1.54 (1.01, 2.34)* | 1.02 (0.60, 1.74) | 1.49 (1.01, 2.21)* | 1.07 (0.66, 1.74) | 1.07 (0.70, 1.64) |
| Hispanic race | 1.12 (0.64, 1.96) | 0.91 (0.61, 1.36) | 1.21 (0.73, 2.00) | 1.76 (1.18, 2.61)** | 1.45 (0.90, 2.34) | 1.25 (0.83, 1.90) |
| Annual income ≤ $20 000 and <$50 000 |
1.02 (0.71, 1.48) | 1.79 (1.35, 2.38)*** | 1.02 (0.75, 1.39) | 1.03 (0.79, 1.35) | 1.32 (0.96, 1.81)+ | 0.73 (0.54, 1.00)+ |
| Annual income ≤$50 000 and <$100 000 |
1.54 (1.01, 2.32)* | 1.87 (1.37, 2.57)*** | 1.00 (0.69, 1.44) | 0.87 (0.65, 1.17) | 1.12 (0.80, 1.57) | 0.86 (0.61, 1.22) |
| Annual income ≤$100 000 | 0.84 (0.49, 1.46) | 1.24 (0.82, 1.87) | 0.87 (0.55, 1.36) | 0.77 (0.53, 1.11) | 0.82 (0.54, 1.26) | 0.93 (0.58, 1.50) |
| Tobacco surveys taken past year | 1.00 (0.91, 1.10) | 1.09 (1.01, 1.17)* | 1.01 (0.92, 1.10) | 0.98 (0.92, 1.05) | 1.02 (0.93, 1.11) | 0.95 (0.88, 1.03) |
| Media market population size | 0.95 (0.48, 1.91) | 0.67 (0.40, 1.10) | 0.88 (0.47, 1.64) | 1.17 (0.72, 1.92) | 0.89 (0.48, 1.64) | 0.98 (0.55, 1.74) |
| Median income in media market | 1.18 (0.98, 1.43)+ | 1.08 (0.94, 1.23) | 1.11 (0.94, 1.31) | 1.13 (1.00, 1.29)+ | 1.12 (0.97, 1.29) | 1.13 (0.97, 1.30) |
| Percentage of media market with college degree |
0.99 (0.95, 1.02) | 1.00 (0.98, 1.03) | 0.99 (0.96, 1.02) | 0.98 (0.96, 1.00)+ | 0.99 (0.96, 1.02) | 0.98 (0.95, 1.01) |
| State per capita tobacco control funding |
1.60 (0.74, 3.47) | 1.50 (0.85, 2.64) | 1.75 (0.91, 3.35)+ | 1.57 (0.93, 2.66)+ | 1.62 (0.91, 2.88) | 1.82 (0.98, 3.35)+ |
| State cigarette tax | 1.04 (0.92, 1.17) | 1.07 (0.97, 1.17) | 1.08 (0.98, 1.19) | 1.13 (1.04, 1.23)** | 1.01 (0.93, 1.11) | 1.03 (0.94, 1.13) |
| Time to first cigarette (in minutes) |
1.01 (0.91, 1.12) | 0.97 (0.90, 1.06) | 1.05 (0.96, 1.15) | 1.01 (0.93, 1.10) | 1.00 (0.92, 1.09) | 0.93 (0.86, 1.01)+ |
| Daily hours of television | 1.04 (0.96, 1.13) | 1.02 (0.96, 1.08) | 1.05 (0.98, 1.13) | 0.98 (0.92, 1.04) | 1.04 (0.97, 1.11) | 1.09 (1.02, 1.16)* |
| Other smoker in household | 0.90 (0.73, 1.12) | 0.89 (0.75, 1.05) | 1.02 (0.85, 1.24) | 1.02 (0.87, 1.19) | 1.04 (0.86, 1.25) | 0.86 (0.72, 1.02)+ |
| Children in household | 0.98 (0.77, 1.25) | 0.96 (0.79, 1.16) | 0.96 (0.76, 1.20) | 1.10 (0.92, 1.31) | 1.15 (0.94, 1.41) | 1.18 (0.97, 1.43)+ |
| Has a mental health condition | 1.50 (1.15, 1.96)** | 1.36 (1.09, 1.68)** | 1.26 (0.99, 1.60)+ | 1.06 (0.86, 1.31) | 1.35 (1.10, 1.67)** | 1.00 (0.79, 1.26) |
| Has a non-mental chronic health condition |
1.67 (1.24, 2.25)*** | 1.29 (1.03, 1.62)* | 1.24 (0.95, 1.62) | 1.17 (0.94, 1.46) | 1.57 (1.21, 2.04)*** | 1.35 (1.07, 1.70)* |
| KP Panel | 1.05 (0.77, 1.41) | 0.69 (0.55, 0.87)** | 1.05 (0.82, 1.34) | 1.17 (0.94, 1.46) | 1.16 (0.88, 1.51) | 0.79 (0.62, 1.02)+ |
| Model N | 10 005 | 10 003 | 10 013 | 10 089 | 9998 | 10 047 |
Note:
P<0.10,
P<0.05,
P<0.01,
P<0.001.
Reference categories for education, race, and income indicators are less than high school, other race, and income <$20 000, respectively.
Table BIII.
Multivariate linear and logistic regression main effect models for Tips exposure and quit motivation, worries about health, and intentions
| Independent variable | Motivation to quit Coefficient (95% CI) | Worries about health Coefficient (95% CI) | Quit in next 30 days OR (95% CI) | Quit in next 6 months OR (95% CI) |
|---|---|---|---|---|
| Post-campaign period | 0.01 (−0.02, 0.04) | 0.06 (0.04, 0.09)*** | 1.28 (1.11, 1.49)*** | 1.13 (1.03, 1.25)* |
| Age | 0.00 (−0.00, 0.00) | 0.00 (−0.00, −0.00)* | 0.99 (0.98, 1.00)+ | 1.00 (1.00, 1.01) |
| High school graduate | 0.03 (−0.08, 0.15) | 0.05 (−0.05, 0.15) | 1.03 (0.73, 1.45) | 0.94 (0.72, 1.24) |
| Achieved some college | 0.03 (−0.08, 0.14) | 0.04 (−0.06, 0.13) | 1.01 (0.73, 1.39) | 0.99 (0.76, 1.28) |
| Earned college degree or more | 0.09 (−0.03, 0.21) | 0.13 (0.02, 0.24)* | 1.17 (0.83, 1.65) | 1.16 (0.87, 1.54) |
| Male | −0.05 (−0.11, 0.02) | −0.12 (−0.18, −0.07)*** | 0.96 (0.79, 1.15) | 0.93 (0.80, 1.08) |
| White race | −0.15 (−0.30, −0.00)* | −0.03 (−0.15, 0.10) | 0.90 (0.58, 1.41) | 0.71 (0.51, 1.01)+ |
| African American race | 0.13 (−0.05, 0.31) | 0.05 (−0.10, 0.21) | 1.31 (0.77, 2.23) | 1.08 (0.71, 1.65) |
| Hispanic race | 0.03 (−0.16, 0.21) | 0.12 (−0.05, 0.30) | 1.46 (0.88, 2.43) | 1.17 (0.77, 1.78) |
| Annual income ≥ $20 000 and <$50 000 | −0.03 (−0.14, 0.08) | −0.01 (−0.11, 0.08) | 0.87 (0.61, 1.25) | 0.94 (0.71, 1.23) |
| Annual income ≥$50 000 and <$100 000 | 0.01 (−0.12, 0.13) | −0.04 (−0.14, 0.06) | 0.97 (0.68, 1.39) | 1.02 (0.76, 1.36) |
| Annual income ≥$ 100 000 | −0.09 (−0.27, 0.09) | −0.08 (−0.23, 0.08) | 1.24 (0.82, 1.86) | 1.21 (0.86, 1.70) |
| Tobacco surveys taken past year | −0.06 (−0.09, −0.03)*** | -0.05 (−0.08, −0.03)*** | 0.96 (0.88, 1.05) | 0.89 (0.83, 0.96)** |
| Media market population size | −0.08 (−0.32, 0.15) | 0.02 (−0.19, 0.23) | 1.23 (0.62, 2.44) | 1.11 (0.66, 1.89) |
| Median income in media market | 0.05 (−0.00, 0.11)+ | 0.03 (−0.02, 0.08) | 1.20 (1.02, 1.41)* | 1.18 (1.03, 1.34)* |
| Percentage of media market with college degree | −0.01 (−0.02, −0.00)* | −0.01 (−0.02, −0.00)* | 0.96 (0.93, 0.99)** | 0.97 (0.94, 0.99)* |
| State per capita tobacco control funding | 0.18 (−0.05, 0.40) | 0.19 (−0.02, 0.41)+ | 0.92 (0.45, 1.89) | 1.10 (0.62, 1.96) |
| State cigarette tax | −0.02 (−0.06, 0.01) | 0.00 (−0.03, 0.03) | 1.02 (0.92, 1.13) | 0.96 (0.88, 1.04) |
| Time to first cigarette (in minutes) | 0.01 (−0.02, 0.04) | −0.02 (−0.05, 0.01) | 1.08 (0.97, 1.20) | 0.97 (0.90, 1.05) |
| Daily hours of television | 0.03 (0.01, 0.06)** | 0.04 (0.01, 0.06)** | 1.01 (0.94, 1.09) | 0.97 (0.92, 1.03) |
| Other smoker in household | −0.01 (−0.07, 0.05) | 0.01 (−0.05, 0.06) | 0.81 (0.66, 1.01)+ | 0.90 (0.77, 1.05) |
| Children in household | 0.20 (0.12, 0.27)*** | 0.17 (0.10, 0.23)*** | 1.42 (1.14, 1.75)** | 1.47 (1.24, 1.75)*** |
| Has a mental health condition | 0.17 (0.09, 0.26)*** | 0.13 (0.05, 0.20)*** | 1.37 (1.06, 1.77)* | 1.33 (1.09, 1.63)** |
| Has a non-mental chronic health condition | 0.25 (0.16, 0.34)*** | 0.23 (0.15, 0.31)*** | 1.48 (1.15, 1.90)** | 1.42 (1.16, 1.74)*** |
| KP Panel | 0.00 (−0.10, 0.10) | −0.02 (−0.10, 0.07) | 0.74 (0.56, 0.98)* | 0.63 (0.50, 0.79)*** |
| Model N | 10 095 | 10 195 | 10 156 | 10 156 |
Note:
P<0.10,
P<0.05,
P<0.01,
P<0.001.
Reference categories for education, race, and income indicators are less than high school, other race, and income <$20 000, respectively.
Table BIV.
Multivariate linear and logistic regression interaction models for Tips exposure and quit motivation, worries about health, and intentions
| Independent variable | Motivation to quit Coefficient (95% CI) | Worries about health Coefficient (95% CI) | Quit in next 30 days OR 95% CI) | Quit in next 6 months OR (95% CI) |
|---|---|---|---|---|
| Post-campaign period | 0.01 (−0.02, 0.03) | 0.06 (0.03, 0.09)*** | 1.28 (1.10, 1.49)** | 1.12 (1.01, 1.24)* |
| Frequency of exposure | 0.05 (0.03, 0.07)*** | 0.04 (0.02, 0.06)*** | 1.08 (0.99, 1.17)+ | 1.10 (1.03, 1.17)** |
| Time × frequency of exposure | 0.03 (0.01, 0.05)** | 0.02 (0.00, 0.04)* | 1.09 (0.99, 1.20)+ | 1.12 (1.05, 1.20)** |
| Age | 0.00 (−0.00, 0.00) | 0.00 (−0.01, −0.00)** | 0.99 (0.98, 1.00)* | 1.00 (1.00, 1.01) |
| High school graduate | 0.05 (−0.07, 0.17) | 0.05 (−0.05, 0.15) | 1.00 (0.71, 1.42) | 0.94 (0.71, 1.23) |
| Achieved some college | 0.04 (−0.08, 0.15) | 0.03 (−0.06, 0.13) | 1.00 (0.72, 1.38) | 0.98 (0.76, 1.28) |
| Earned college degree or more | 0.11 (−0.02, 0.23)+ | 0.13 (0.02, 0.23)* | 1.18 (0.83, 1.68) | 1.18 (0.88, 1.57) |
| Male | −0.04 (−0.10, 0.03) | −0.12 (−0.17, −0.06)*** | 0.96 (0.79, 1.16) | 0.94 (0.80, 1.09) |
| White race | −0.14 (−0.29, 0.01)+ | −0.04 (−0.17, 0.08) | 0.93 (0.59, 1.47) | 0.72 (0.51, 1.02)+ |
| African American race | 0.11 (−0.07, 0.29) | 0.00 (−0.14, 0.15) | 1.26 (0.73, 2.17) | 1.04 (0.67, 1.59) |
| Hispanic race | 0.04 (−0.15, 0.23) | 0.11 (−0.07, 0.28) | 1.46 (0.87, 2.45) | 1.18 (0.77, 1.82) |
| Annual income ≥$20 000 and <$50 000 | −0.03 (−0.14, 0.09) | 0.01 (−0.09, 0.10) | 0.90 (0.63, 1.29) | 0.95 (0.72, 1.24) |
| Annual income ≥$50 000 and <$100 000 | 0.02 (−0.10, 0.15) | −0.02 (−0.12, 0.08) | 1.01 (0.70, 1.44) | 1.04 (0.78, 1.40) |
| Annual income ≥$100 000 | −0.07 (−0.25, 0.11) | −0.06 (−0.22, 0.10) | 1.29 (0.86, 1.95) | 1.25 (0.89, 1.77) |
| Tobacco surveys taken past year | −0.06 (−0.09, −0.03)*** | −0.05 (−0.08, −0.03)*** | 0.97 (0.89, 1.06) | 0.90 (0.84, 0.97)** |
| Media market population size | −0.06 (−0.29, 0.18) | 0.03 (−0.18, 0.25) | 1.32 (0.66, 2.66) | 1.18 (0.70, 2.01) |
| Median income in media market | 0.05 (−0.00, 0.11)+ | 0.03 (−0.02, 0.08) | 1.20 (1.02, 1.41)* | 1.17 (1.03, 1.34)* |
| Percentage of media market with college degree | −0.01 (−0.02, −0.00)* | −0.01 (−0.02, 0.00)+ | 0.96 (0.93, 0.99)* | 0.97 (0.95, 0.99)* |
| State per capita tobacco control funding | 0.19 (−0.03, 0.42)+ | 0.22 (0.00, 0.43)* | 0.96 (0.47, 1.99) | 1.15 (0.65, 2.04) |
| State cigarette tax | −0.03 (−0.06, 0.01) | 0.00 (−0.03, 0.03) | 1.02 (0.92, 1.13) | 0.95 (0.88, 1.03) |
| Time to first cigarette (in minutes) | 0.01 (−0.02, 0.04) | −0.02 (−0.05, 0.01) | 1.08 (0.97, 1.20) | 0.97 (0.89, 1.05) |
| Daily hours of television | 0.02 (−0.00, 0.05)+ | 0.03 (0.01, 0.05)** | 1.00 (0.93, 1.08) | 0.95 (0.90, 1.00)+ |
| Other smoker in household | −0.02 (−0.08, 0.04) | 0.00 (−0.06, 0.05) | 0.79 (0.64, 0.98)* | 0.87 (0.74, 1.02)+ |
| Children in household | 0.18 (0.11, 0.25)*** | 0.14 (0.08, 0.21)*** | 1.35 (1.09, 1.68)** | 1.42 (1.19, 1.69)*** |
| Has a mental health condition | 0.16 (0.08, 0.25)*** | 0.11 (0.04, 0.19)** | 1.34 (1.04, 1.74)* | 1.31 (1.07, 1.60)** |
| Has a non-mental chronic health condition | 0.24 (0.15, 0.33)*** | 0.23 (0.15, 0.30)*** | 1.44 (1.11, 1.87)** | 1.38 (1.12, 1.70)** |
| KP Panel | −0.01 (−0.11, 0.09) | −0.04 (−0.12, 0.04) | 0.72 (0.55, 0.95)* | 0.61 (0.48, 0.76)*** |
| Model N | 9994 | 10 089 | 10 050 | 10 050 |
Note:
P<0.10,
P<0.05,
P<0.01,
P<0.001.
Reference categories for education, race and income indicators are less than high school, other race and income <$20 000, respectively.
Footnotes
Conflict of interest statement None declared.
Publisher's Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or RTI International.
References
- 1.Centers for Disease Control and Prevention Cigarette smoking among adults—United States, 2002. MMWR Morb Mortal Wkly Rep. 2004;53:427–31. [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services (USDHHS) The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2014. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention [Accessed: 29 April 2015];Figure 8.1. Prevalence of Current Smoking among Adults Aged 18 and over: United States, 1997–2012. http://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201306_08.pdf.
- 4.U.S. Department of Health and Human Services [Accessed: 29 April 2015]; HealthyPeople.gov. 2013 doi: 10.3109/15360288.2015.1037530. HealthyPeople.gov http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=41. [DOI] [PubMed]
- 5.Guide to Community Preventive Services [Accessed: 29 April 2015];Reducing Tobacco Use and Secondhand Smoke Exposure: Mass-Reach Health Communication Interventions. 2013 http://www.healthypeople.gov/2020/topics-objectives/topic/tobacco-use.
- 6.National Cancer Institute . Tobacco Control Monograph No. 19. U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; Bethesda, MD: 2008. The Role of the Media in Promoting and Reducing Tobacco Use. [Google Scholar]
- 7.Bala M, Strzeszynski L, Cahill K. Mass media interventions for smoking cessation in adults. Cochrane Database Syst Rev. 2008;1:CD004704. doi: 10.1002/14651858.CD004704.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Wilson LM, Avila Tang E, Chander G, et al. Impact of tobacco control interventions on smoking initiation, cessation, and prevalence: a systematic review. J Environ Public Health. 2012;2012:961724. doi: 10.1155/2012/961724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Durkin S, Brennan E, Wakefield M. Mass media campaigns to promote smoking cessation among adults: an integrative review. Tob Control. 2012;21:127–38. doi: 10.1136/tobaccocontrol-2011-050345. [DOI] [PubMed] [Google Scholar]
- 10.Vallone DM, Duke JC, Cullen J, et al. Evaluation of EX: a national mass media smoking cessation campaign. Am J Public Health. 2011;101:302–9. doi: 10.2105/AJPH.2009.190454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vallone DM, Niederdeppe J, Richardson AK, et al. A national mass media smoking cessation campaign: effects by race/ethnicity and education. Am J Health Promot. 2011;25:S38–50. doi: 10.4278/ajhp.100617-QUAN-201. [DOI] [PubMed] [Google Scholar]
- 12.Wakefield MA, Spittal MJ, Yong HH, et al. Effects of mass media campaign exposure intensity and durability on quit attempts in a population-based cohort study. Health Educ Res. 2011;26:988–97. doi: 10.1093/her/cyr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farrelly MC, Duke JC, Davis KC, et al. Promotion of smoking cessation with emotional and/or graphic antismoking advertising. Am J Prev Med. 2012;43:475–82. doi: 10.1016/j.amepre.2012.07.023. [DOI] [PubMed] [Google Scholar]
- 14.Wakefield MA, Durkin S, Spittal MJ, et al. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health. 2008;98:1443–50. doi: 10.2105/AJPH.2007.128991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McAlister A, Morrison TC, Hu S, et al. Media and community campaign effects on adult tobacco use in Texas. J Health Commun. 2004;9:95–109. doi: 10.1080/10810730490425231. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention Decline in smoking prevalence—New York City, 2002–2006. MMWR Morb Mortal Wkly Rep. 2007;56:604–8. [PubMed] [Google Scholar]
- 17.Terry-McElrath Y, Wakefield M, Ruel E, et al. The effect of antismoking advertisement executional characteristics on youth comprehension, appraisal, recall, and engagement. J Health Commun. 2005;10:127–43. doi: 10.1080/10810730590915100. [DOI] [PubMed] [Google Scholar]
- 18.Wakefield M, Durrant R, Terry-McElrath Y, et al. Appraisal of anti-smoking advertising by youth at risk for regular smoking: a comparative study in the United States, Australia, and Britain. Tob Control. 2003;12(Suppl 2):ii82–6. doi: 10.1136/tc.12.suppl_2.ii82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Biener L, McCallum-Keeler G, Nyman AL. Adults' response to Massachusetts anti-tobacco television advertisements: impact of viewer and advertisement characteristics. Tob Control. 2000;9:401–7. doi: 10.1136/tc.9.4.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Augustson E, Bright MA, Babb S, et al. Increases in quitline calls and smoking cessation Website visitors during a national tobacco education campaign—March 19-June 10, 2012. MMWR Morb Mortal Wkly Rep. 2012;61:667–70. [PubMed] [Google Scholar]
- 21.McAfee T, Davis KC, Alexander RL, Jr, et al. Effect of the first federally funded US antismoking national media campaign. Lancet. 2013;382:2003–11. doi: 10.1016/S0140-6736(13)61686-4. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention . Best Practices for Comprehensive Tobacco Control PRograms—2014. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2014. [Google Scholar]
- 23.Murray DM, Prokhorov AV, Harty KC. Effects of a statewide antismoking campaign on mass media messages and smoking beliefs. Prev Med. 1994;23:54–60. doi: 10.1006/pmed.1994.1008. [DOI] [PubMed] [Google Scholar]
- 24.Farrelly MC, Davis KC, Haviland ML, et al. Evidence of a dose-response relationship between “truth” antismoking ads and youth smoking prevalence. Am J Public Health. 2005;95:425–31. doi: 10.2105/AJPH.2004.049692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Price SM, Huhman M, Potter LD. Influencing the parents of children aged 9–13 years: findings from the VERB campaign. Am J Prev Med. 2008;34:S267–74. doi: 10.1016/j.amepre.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 26.Cowell AJ, Farrelly MC, Chou R, et al. Assessing the impact of the national `truth' antismoking campaign on beliefs, attitudes, and intent to smoke by race/ethnicity. Ethn Health. 2009;14:75–91. doi: 10.1080/13557850802257715. [DOI] [PubMed] [Google Scholar]
- 27.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Prentice Hall, Inc.; New Jersey: 1980. [Google Scholar]
- 28.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15:175–83. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 29.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Pearson; Prentice-Hall, Englewood Cliffs, NJ: 1986. [Google Scholar]
- 30.Hornik R. Public Health Communication: Evidence for Behavior Change. Lawrence Erlbaum Associates; London, NJ: 2002. [Google Scholar]
- 31.Fishbein M. A consideration of beliefs and their role in attitude measurement. In: Fishbein M, editor. Readings in Attitude Theory and Measurement. Wiley; New York, NY: 1967. pp. 257–66. [Google Scholar]
- 32.Duke JC, Nonnemaker J, Davis K, et al. The impact of cessation media messages on cessation-related outcomes: results from a national experiment of smokers. Am J Health Promot. 2014;28:242–50. doi: 10.4278/ajhp.120920-QUAN-452. [DOI] [PubMed] [Google Scholar]
- 33.Guoze F, Yuan J, Qiang L, et al. Individual-level factors associated with intentions to quit smoking among adult smokers in six cities of China: findings from the ITC China Survey. Tob Control. 2010;19:i6–11. doi: 10.1136/tc.2010.037093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou X, Nonnemaker J, Sherrill B, et al. Attempts to quit smoking and relapse: factors associated with success or failure from the ATTEMPT cohort study. Addict Behav. 2009;34:365–73. doi: 10.1016/j.addbeh.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 35.Hyland A, Wakefield M, Higbee C, et al. Anti-tobacco television advertising and indicators of smoking cessation in adults: a cohort study. Health Educ Res. 2006;21:348–54. doi: 10.1093/her/cyl048. [DOI] [PubMed] [Google Scholar]
- 36.Koblitz AR, Magnan RE, McCaul KD, et al. Smokers' thoughts and worries: a study using ecological momentary assessment. Health Psychol. 2009;28:484–92. doi: 10.1037/a0014779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yeager DS, Krosnick JA, Chang L, et al. Comparing the accuracy of RDD telephone surveys and Internet surveys conducted with probability and non-probability samples. Public Opin Q. 2011;75:709–47. [Google Scholar]
- 38.Chang L, Krosnick JA. National surveys via RDD telephone interviewing versus the Internet. Public Opin Q. 2009;73:641–78. [Google Scholar]
- 39.Disogra C, Cobb CL, Chan E, et al. Using probability-based online samples to calibrate non-probability opt-in samples. Presentation at the 67th Annual Conference of the American Association for Public Opinion Research (AAPOR), May 19; Orlando, FL. 2012. [Google Scholar]
- 40.Duke JC, Nonnemaker JM, Davis KC, et al. The impact of cessation media messages on cessation-related outcomes: results from a national experiment of smokers. Am J Health Promot. 2014;28:242–50. doi: 10.4278/ajhp.120920-QUAN-452. [DOI] [PubMed] [Google Scholar]
- 41.Ajzen I, Fishbein M. The influence of attitudes on behavior. In: Albarracin D, Johnson BT, Zanna MP, editors. The Handbook of Attitudes. Lawrence Erlbaum Associates; Mahwah, NJ: 2005. pp. 173–221. [Google Scholar]
- 42.Centers for Disease Control and Prevention [Accessed: 4 February 2013];Early Release of Selected Estimates Based on Data from the January–March 2012 National Health Interview Survey. 2012 http://www.cdc.gov/nchs/nhis/released201209.htm.
- 43.U.S. Census Bureau Population Division [Accessed: 6 August 2013];Table 2: Annual Estimates of the Resident Population for Selected Age Groups by Sex for the United States—April 1, 2010 to July 1, 2011 (NC-EST2011-02) 2012 http://www.census.gov/popest/data/national/asrh/2011/tables/NC-EST2011-02.xls.
- 44.Durkin SJ, Biener L, Wakefield MA. Effects of different types of antismoking ads on reducing disparities in smoking cessation among socioeconomic subgroups. Am J Public Health. 2009;99:2217–23. doi: 10.2105/AJPH.2009.161638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Khadjesari Z, Murray E, Kalaitzaki E, et al. Impact and costs of incentives to reduce attrition in online trials: two randomized controlled trials. J Med Internet Res. 2011;13:e26. doi: 10.2196/jmir.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Murray E, Khadjesari Z, White IR, et al. Methodological challenges in online trials. J Med Internet Res. 2009;11:e9. doi: 10.2196/jmir.1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McCoy TP, Ip EH, Blocker JN, et al. Attrition bias in a U.S. Internet survey of alcohol use among college freshmen. J Stud Alcohol Drugs. 2009;70:606–14. doi: 10.15288/jsad.2009.70.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.U.S. Department of Health and Human Services . Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2012. [Google Scholar]


