Abstract
The role of anxiety has been emphasized in etiological/maintenance models of anorexia nervosa. This study identified daily patterns of anxiety in anorexia nervosa and examined the likelihood of the occurrence of eating disorder behaviors in each trajectory, the daily temporal distribution of eating disorder behaviors in each trajectory, and the extent to which the tendency to exhibit particular anxiety trajectories was associated with baseline diagnostic and trait-level personality variables. Women with full or subthreshold anorexia nervosa (N = 118) completed a two-week ecological momentary assessment (EMA) protocol during which they reported on a variety of behavioral and affective variables, including anxiety and eating disorder behaviors. Using latent growth mixture modeling to classify EMA days (N = 1526) based on anxiety ratings, seven distinct daily anxiety trajectories were identified. Overall differences between trajectories were found for rates of binge eating, self-induced vomiting, body checking, skipping meals, and dietary restriction. Further, distinct daily temporal distributions of eating disorder behaviors were found across the trajectories, with peaks in the probability of behaviors frequently coinciding with high levels of anxiety. Finally, traits of personality pathology (affective lability, self-harm, social avoidance, and oppositionality) and the presence of a co-occurring mood disorder were both found to be associated with the tendency to experience particular daily anxiety trajectories (e.g., Stable High anxiety). Findings support the presence of within-person variability in daily anxiety patterns in anorexia nervosa and also provide evidence for an association between these anxiety patterns and eating disorder behaviors.
Keywords: eating disorder, anxiety, ecological momentary assessment, latent growth mixture modeling, personality
Daily Patterns of Anxiety in Anorexia Nervosa: Associations with Eating Disorder Behaviors in the Natural Environment
Anorexia nervosa (AN) is a serious psychiatric disorder characterized by symptoms including intense fear about weight gain, disturbances in body image, and maintenance of a less than minimally normal body weight (American Psychiatric Association, 1994). The disorder is further characterized by two subtypes: the restricting type (in which individuals’ low weight is maintained via fasting, limiting the amount and types of food eaten, and/or engaging in excessive exercise) and the binge-eating/purging type (in which individuals may exhibit restricting type behaviors in addition to regularly engaging in binge eating, purging, or both). AN is frequently accompanied by a number of medical problems including bradycardia and electrolyte imbalances (APA, 1994), and recent estimates suggest that individuals with AN are over five times more likely to die of any cause than age-matched controls, with one of five of these deaths resulting from suicide (Arcelus, Mitchell, Wales, & Nielsen, 2011). Further, the presence of co-occurring psychopathology in AN is common (Steinhausen, 2009) and has been found to be a poor prognostic factor (e.g., Papadopoulos, Ekbom, Brandt, & Ekselius, 2009). Among the DSM-IV (APA, 1994) Axis I disorders that most commonly co-occur with AN are mood and anxiety disorders (Halmi et al., 1991; Hudson, Hiripi, Pope, & Kessler, 2007). In particular, the co-occurrence of AN and anxiety disorders has been emphasized in research, with obsessive compulsive disorder (OCD), social phobia, and specific phobia identified as among those that are most common (Jordon et al., 2008; Kaye, Bulik, Thornton, Barbarich, & Masters, 2004). The DSM-IV Axis II personality disorders that are most frequently observed in AN are those from clusters B (e.g., borderline personality disorder) and C (e.g., obsessive compulsive personality disorder; Gaudio & Di Ciommo, 2011; Herzog, Keller, Lavori, Kenny, & Sacks, 1992).
Anorexia Nervosa Behaviors
In addition to the diagnostic symptoms of AN and the behaviors characterizing the two subtypes, individuals with AN frequently exhibit a variety of other maladaptive and ritualistic behaviors associated with the disorder (e.g., Shafran, Fairburn, Robinson, & Lask, 2004; Steinglass et al., 2011). Examples of such behaviors include body checking (i.e., repeated checking of shape and/or weight, such as pinching one’s flesh) and food- and eating-related rituals (e.g., eating meals alone, cutting food into small pieces). Although these behaviors are not included in the core diagnostic criteria, they are commonly addressed in cognitive behavioral models of AN and other eating disorders (e.g., Fairburn, Cooper, & Shafran, 2003; Fairburn, Shafran, & Cooper, 1999; Williamson, White, York-Crowe, & Stewart, 2004). For instance, body checking has been identified as a possible maintaining factor for dietary restriction in AN, and is a primary treatment target in Enhanced Cognitive Behavior Therapy for Eating Disorders (Fairburn, 2008; Fairburn et al., 1998). Further, rituals associated with food intake are conceptualized as driven or compulsive behaviors that are difficult to resist and may be associated with a subsequent, albeit temporary, sense of relief (Mazure, Halmi, Sunday, Romano, & Einhorn, 1994).
Emotion in Anorexia Nervosa
The importance of negative affective states in AN has recently been highlighted in the theoretical and empirical literature (e.g., Brockmeyer et al., 2012; Haynos & Fruzzetti, 2011; Schmidt & Treasure, 2006). For example, in their model of AN as a disorder of emotion dysregulation, Haynos and Fruzzetti (2011) posit the presence of an underlying emotional vulnerability that can result in heightened emotional arousal that may function as a trigger for various ED behaviors. Such conceptual accounts of the role of negative affective states in AN are supported by research findings indicating the presence of disturbances in emotional functioning in this population. For example, evidence suggests that individuals with AN exhibit a reduced ability to tolerate distress (Hambrook et al., 2011) and display heightened levels of emotional avoidance (Wildes, Ringham, & Marcus, 2010) and emotion dysregulation (Harrison, Sullivan, Tchanturia, & Treasure, 2010).
Additionally, several theoretical accounts have focused on anxiety, a specific facet of negative affect (NA), as being particularly relevant to the etiology, maintenance, and treatment of AN. For example, Strober (2004) has proposed that abnormal fear conditioning processes are a primary etiological factor in AN. Similarly, Steinglass and Walsh (2006) have proposed a model that emphasizes the fear of weight gain and the obsessional nature of associated cognitions in AN. Steinglass and colleagues (2011) further suggest that an intervention based on exposure and response prevention, a therapeutic approach widely used in the treatment of anxiety disorders (particularly OCD), may prove efficacious in the treatment of AN. These theoretical accounts highlighting the importance of anxiety in AN are consistent with empirical findings suggesting that (a) there are high rates of co-occurrence between AN and anxiety disorders (Halmi et al., 1991; Jordon et al., 2008; Kaye et al., 2004), (b) there are greater anxiety symptoms among those with AN compared to healthy controls (Frank et al., 2012), even after weight restoration (Wagner et al., 2007), and (c) anxiety symptoms may differentiate patients who do and do not experience remission from AN (Yackobovitch-Gavan et al., 2009). In sum, both conceptual accounts and empirical findings support the importance of anxiety in the etiology/maintenance and treatment AN.
Ecological Momentary Assessment
One methodology that is particularly well-suited for examining associations between behavioral and affective variables including anxiety is ecological momentary assessment (EMA), a technique that involves data collection in a participant’s natural environment in the moment when emotional experiences and behaviors occur (Smyth et al., 2001; Stone & Shiffman, 1994). The use of EMA provides several benefits over traditional self-report and laboratory-based designs, including greater ecological validity and generalizability, as well as reduced bias due to retrospective recall and the impact of state mood on memory of previous behaviors and affective experiences. Findings from previous EMA studies in samples of women with bulimia nervosa (BN) and binge eating disorder suggest that binge eating is associated with momentary NA (Haedt-Matt & Keel, 2011; Hilbert & Tuschen-Caffier, 2007; Smyth et al., 2007), as well as negative affect lability (Anestis et al., 2010). Further, a small EMA study of women with AN revealed substantial variability in mood within and across individuals, with affective lability found to be positively associated with restrictive and ritualistic behaviors (Engel et al., 2005). Other studies have sought to elaborate the nature of the variability of NA in eating disorders. For instance, Crosby and colleagues (2009) used a latent structure analysis to identify distinct daily trajectories of NA in a sample of women with BN. Results revealed that the likelihood of binge eating and purging differed across these daily trajectories, with a greater tendency for bulimic behaviors to occur on days characterized by high NA. Taken together, these findings provide further support for the importance of affective variables in relation to ED behaviors, highlighting the utility of examining these associations using momentary data.
Current Study
The overall goal of the current study was to examine the association between patterns of anxiety and ED behaviors in a sample of women with AN. There were four specific objectives: (a) to use a latent structure analysis (i.e., latent growth mixture modeling) to identify daily trajectories of anxiety in AN, (b) to examine differences in the occurrence of various ED behaviors across the identified trajectories, (c) to examine the temporal distribution of ED behaviors across the day in each identified pattern, and (d) to examine the extent to which baseline diagnostic and trait-level personality variables were associated with the propensity to exhibit particular daily anxiety trajectories. Broadly, this investigation sought to replicate the overall aim of the Crosby and colleagues’ (2009) study in BN by identifying daily mood trajectories and associations with ED behaviors in AN. However, in addition to conducting an EMA study with AN participants, which is unique, this study also extended the previous research by examining: (a) trajectories of anxiety, a facet of NA thought to be particularly relevant to AN; (b) a greater number of ED behaviors, including binge eating, self-induced vomiting, exercise, body checking, and various forms of restriction; and (c) person-level differences in baseline diagnostic and personality variables associated with the tendency to experience particular anxiety trajectories. Further, although prior studies have characterized within-diagnosis heterogeneity by identifying clinically relevant subtypes via empirical classification (e.g., latent profile analysis), such approaches do not address possible differences within individuals (e.g., the extent to which the experience of anxiety differs from day-to-day for a given person). In the present research, we hypothesized that ED behaviors would be more likely to occur on days characterized by higher and more variable anxiety (compared to days with stable low anxiety) and that the tendency to experience more days characterized by high levels of anxiety would be positively associated with the presence of co-occurring mood and anxiety disorders, as well as trait-level personality pathology.
Method
Participants
Participants were women (N = 118) meeting Diagnostic and Statistical Manual of Mental Disorders (4th Edition: DSM-IV; APA, 1994) criteria for full AN (n = 59) or subthreshold AN (n = 59). In the current study, subthreshold AN was defined as meeting all DSM-IV criteria for AN except: body mass index (BMI) of 17.6 to 18.5 kg/m2, or absence of amenorrhea or the cognitive symptoms of AN. As such, there were three possible symptom constellations: (a) amenorrhea, cognitive symptoms, and BMI of 17.6 to 18.5 kg/m2, (b) amenorrhea, no cognitive symptoms, and BMI < 17.5 kg/m2, and (c) no amenorrhea, cognitive symptoms, and BMI < 17.5 kg/m2 (see Le Grange et al., 2012 for further details). Seventy-three (61.9%) participants were diagnosed with AN restricting type and 45 (38.1%) were diagnosed with AN binge eating-purging type. A total of 601 individuals were phone screened for eligibility, of which 166 were further evaluated at three research facilities. Eligibility criteria included being female, at least 18 years of age, and satisfying criteria for full or subthreshold AN. In total, 121 individuals met criteria, agreed to participate, and were enrolled. Three participants with overall EMA compliance rates of < 50% were excluded from analyses, leaving a total of 118 participants. The final sample had a mean BMI of 17.2 kg/m2 (SD = 1.0; Range = 13.4–18.5) and a mean age of 25.3 years (SD = 8.4; Range = 18–58) at baseline. A total of 23.7% of the sample had a current mood disorder and 42.4% had a current anxiety disorder. Most participants were Caucasian (96.6%), single/never married (75.4%), and had completed at least some post-secondary education (90.7%).
Measures
Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-I/P)
The SCID-I/P (First et al., 1995) is a semi-structured interview used to assess Axis I psychiatric disorders. In the present study, the SCID-I/P was administered by trained assessors to assess for current AN and subthreshold AN, as well as current and lifetime criteria for other Axis I disorders. All SCID interviews were recorded and a second independent assessor rated current eating disorder diagnoses in a random sample of 25% (n = 30). Interrater reliability for current AN diagnosis based upon a kappa coefficient was .93.
One of the coauthors (CBP) provided SCID administration training consisting of an interactive didactic seminar and use of training tapes. Trainees (a) observed and scored interviews by advanced assessors, (b) administered the interview to staff in role plays, and (c) had their interviews reviewed by advanced assessors before independently administering the interview. To ensure consistency and prevent drift, assessors regularly communicated through teleconferencing/email and in-person meetings held at least yearly.
Dimensional Assessment of Personality Pathology-Basic Questionnaire (DAPP-BQ)
The DAPP-BQ (Livesley & Jackson, 2009) was administered in the current study as a measure of personality dysfunction. The DAPP-BQ is a 290-item self-report questionnaire that contains 18 scales that assess personality traits theorized to be associated with personality disorders. Items were rated on a 5-point scale ranging from (1) very unlike me to (5) very like me, and summed raw scores were converted to T-scores. In the current study, four scales were used: Self-Harm (i.e., suicidal/parasuicidal thoughts or behaviors; α = .96), Affective Lability (i.e., frequent, unpredictable shifts in mood; α = .92), Social Avoidance (i.e., avoidance of social relationships/contacts; α = .93), and Oppositionality (i.e., unreliable and passive-aggressive; α = 92). These particular scales were selected because they (a) assess personality traits theoretically relevant to socio-emotional functioning in AN and (b) have been found to be associated with measures of anxiety or the related construct of neuroticism (e.g., Livesley & Jackson, 2009).
EMA measures
Momentary anxiety was assessed using 8 items from the tension-anxiety scale of the Profile of Mood States (POMS; Lorr & McNair, 1971): on edge, restless, tense, anxious, uneasy, shaky, panicky, and relaxed (reverse coded). Participants rated their current mood on a 5-point scale ranging from (1) not at all to (5) extremely. The alpha coefficient for this measure in the current study was .92.
Participants also provided reports of eating episodes and various ED behaviors. Participants were asked to report all eating episodes, indicating whether the episode was a snack, a meal, or a binge. They also indicated whether they felt out of control or driven to eat. Participants were trained in standard definitions of eating events by clinical research staff during the EMA training session. The definition provided to participants for an unusually large amount of food was “an amount of food that most people would consider excessive,” and examples that were tailored to the participants’ eating habits were provided. Loss of control was defined as “the inability to stop eating,” and feeling driven to eat was defined as “the inability to prevent the eating episode.” Additionally, at the end of each day, participants indicated if they went at least 8 waking hours without eating and if they limited their food intake to less than 1200 kcal. Finally, participants were asked to report on specific ED behaviors, including self-induced vomiting, exercising, skipping a meal, and body checking (i.e., making sure thighs do not touch, checking joints and bones for fat).
Procedure
Participants were recruited at three sites in the Midwestern U.S. (Chicago, IL; Fargo, ND; Minneapolis, MN) from ED treatment facilities, mailings to ED treatment professionals, on-line postings, advertisements in community and campus newspapers, and flyers posted in clinical, community and campus settings. Study approval was obtained from the institutional review board at each site. Potential participants were first screened over the phone, and eligible individuals attended an informational meeting where they received further information regarding the study and provided written informed consent. Participants were then scheduled for two assessment visits during which a physical examination and laboratory tests were conducted to ensure medical stability, structured interviews were conducted, and self-report questionnaires were administered.
Participants were trained in the use of the palmtop computers (Handspring Visors) at the end of the first assessment. Research personnel met with participants to remind them of the study goals, what to expect during the data collection period, and how to address any questions that might arise during their participation. Participants were instructed not to complete entries at any times when they felt unable to reply (e.g., during class) or if safety was a concern (e.g., while driving), but instead to respond later. Participants carried the palmtop computer for 2 practice days, after which they returned and provided the data recorded during their practice period (these data were not used in analyses). This practice period was used both to ensure participants were familiar and comfortable with the EMA assessments and to minimize reactivity to the recording procedures (although research suggests that such monitoring is associated with minimal reactivity; e.g., Stein & Corte, 2003). These data were reviewed by research personnel and participants were given feedback regarding their compliance. Participants were then given the palmtop computer to complete EMA recordings over the subsequent 2 weeks. Attempts were made to schedule 2–3 visits for each participant during this 2-week interval to obtain recorded data to minimize any loss in the event of technical problems. Participants were given compliance feedback at each visit. Participants were compensated $100 per week for completing EMA assessments and were given a $50 bonus for a random signal compliance rate of at least 80%.
The EMA protocol in the current study implemented the three types of daily self-report methods described by Wheeler and Reis (1991): signal-contingent (i.e., providing a rating in response to a random prompt), event-contingent (i.e., providing a rating in response to an event or behavior, such as a binge eating episode), and interval-contingent, (i.e., providing a rating at a specified interval, such as at the end of the day). Each EMA report required approximately 2–3 minutes to complete. Participants provided signal-contingent data at six semi-random times throughout the day. Signal times were randomly distributed about the following six “anchor points” that subdivided the day into six roughly equivalent time blocks: 8:30AM, 11:10AM, 1:50PM, 4:30PM, 7:10PM, and 9:50PM. Signal times were normally distributed about these anchor points with standard deviations of 30 minutes that spread assessments evenly over typical waking hours. When signaled, participants were asked to rate their anxiety, to indicate whether they had engaged in body checking, and to report any other recent eating or ED behaviors not yet recorded. Participants were also asked to provide event-contingent data when any eating episodes (regular or binge) or AN behaviors (e.g., skipping meals, exercise, self-induced vomiting) occurred and interval-contingent data by completing EMA ratings of mood and dietary restriction (e.g., not eating for 8 hours, eating < 1200 kcal) at the end of each day.
Statistical Analyses
Model identification
To identify daily trajectories of anxiety, latent growth mixture modeling (LGMM; Muthén & Muthén, 2000) was used to analyze the ratings on the tension-anxiety subscale of the POMS. LGMM assumes that data are comprised of a mixture of groups, each with its own distinct trajectory. In addition to identifying trajectories that account for variability in the data, this analytical approach provides posterior probabilities of group membership so that observations in the sample can be assigned to the trajectory group that best represents their data. In the present study, days (rather than participants) were classified. With each participant providing several tension-anxiety ratings per day over multiple days, the number of different trajectories any single individual could experience was limited only by the number of trajectories identified in the LGMM analysis. As in Crosby and colleagues’ (2009) study, only signal-contingent tension-anxiety scale data were used in the LGMM analysis (although ratings were provided at other occasions) because the timing of the event-contingent and interval-contingent reports varied widely across participants. Thus, in this analysis, each day could have a maximum of six tension-anxiety ratings. Although the LGMM analysis allows for missing data, days that had fewer than four (≤ 50%) tension-anxiety ratings were excluded. This decision was made because we sought to model both linear and quadratic parameters in the LGMM analysis, in light of recommendations for at least four data points for the latter (Singer & Willet, 2003; p. 217), and because this approach is consistent with the precedent set in a previous EMA study in BN (Crosby et al., 2009), thus facilitating the comparison of findings across these studies. Of the 1768 days of ratings provided by the 118 participants, a total of 242 (13.7%) were excluded for having fewer than four completed random signal responses (many including partial days on the first and last day of recording), leaving a final total of 1526 participant days for the analyses.
The LGMM analyses were conducted using Mplus (Version 6.11; Muthén & Muthén, 1998–2010). Previous research suggested that characterizing the daily anxiety trajectories required the estimation of an intercept and linear and quadratic components in the models (Crosby et al., 2009). The models estimated mean growth curves (and within-class variation around the curves) for each class (Muthén & Muthén, 2000). Specifically, separate model parameters were estimated for each class and variation was allowed for the intercept, whereas the variances of the quadratic and linear components were fixed at zero to facilitate model convergence. Missing responses to random signals were estimated with full information maximum-likelihood estimation, and participant was included as a clustering variable to account for covariation within participant. To determine the best available model for the data, three fit indices and the entropy index were examined for each model. The fit indices included the Bayesian Information Criterion (BIC; Schwartz, 1978), sample-size adjusted BIC (aBIC; Sclove, 1987), and Consistent Akaike Information Criterion (cAIC; Bozdogan, 1987). Each fit index is calculated using the log likelihood, sample size, and number of parameters of the model. As a general rule, models with more trajectories (and thus more parameters) are penalized such that parsimony is encouraged in the selection process. The three fit indices differ with respect to how this penalty is calculated, with the BIC considered to be among the most conservative (Kadane & Lazar, 2004; Tofighi & Enders, 2008). The entropy index (Ramaswamy, DeSarbo, Reibstein, & Robinson, 1993) quantifies the accuracy of a model’s classification, having a minimum of 0 and a maximum of 1, with higher values indicating greater classification accuracy.
ED behaviors across trajectories
General estimating equations (GEE; Liang & Zeger, 1986) were used to evaluate differences in the daily occurrence of ED behaviors across the different anxiety trajectories. Overall comparisons between classes were based on the Wald Χ2 statistic and odds ratios with 99% confidence intervals were computed to compare the reference category (Stable Low anxiety) to the other classes. Post-hoc pairwise comparisons based on estimated marginal means were also conducted to examine each of the possible trajectory comparisons. Further, a second set of similar GEEs was conducted with the addition of a personality variable covariate (trait affective lability), which allowed for an examination of the unique associations between the anxiety trajectories and ED behaviors above and beyond a conceptually relevant baseline personality construct. A corrected alpha of .01 was selected to protect against Type I error in these analyses.
Temporal distribution of ED behaviors within trajectories
The temporal distribution of ED behaviors over the course of the day within each trajectory was examined via kernel density estimation (PROC KDE in SAS; SAS Institute Inc., 1999; Silverman, 1986). This procedure was used to estimate the probability that a given behavior occurred at each hour over 24 hours, with the cumulative daily probability summing to one. Specifically, the resulting functions represent the relationship between time of day and ED behaviors, depicting the variability in the likelihood of ED behaviors across the day. Separate functions were derived for the probability of four ED behaviors (binge eating, vomiting, skipping meals, and body checking) in each of the identified trajectories.
Associations between baseline characteristics and trajectories
An additional goal of the current study was to investigate individual differences by examining the extent to which baseline between-subjects variables were associated with the anxiety trajectories. A series of four GEEs were used to evaluate anxiety trajectory differences in diagnostic variables: full versus subthreshold AN, AN restricting type versus AN binge eating-purging type, presence versus absence of a current mood disorder, and presence versus absence of a current anxiety disorder. Further, the association between baseline personality variables (Affective Lability, Self-Harm, Social Avoidance, and Oppositionality) and propensity for displaying particular anxiety trajectories was examined. For each participant, the tendency to experience a given daily anxiety trajectory was represented as a proportion, calculated by dividing the number of days that were classified into that trajectory by the total number of days for that participant. For example, if a given participant had a total of 13 days of assessment with 6 of those days classified into Trajectory A, the proportion for Trajectory A would be .46 (6/13). Spearman Rho correlations were calculated to represent the associations between the baseline personality variables and the tendency to experience particular anxiety trajectories. A corrected alpha of .01 was selected to protect against Type I error.
Results
EMA Findings
Participants provided 14,945 separate EMA recordings (9085 responses to signals, 3383 eating episodes recordings, 999 ED behavior recordings, and 1478 end-of-day recordings) representing 1768 separate participant days. The number of days that participants provided EMA recordings ranged from 6 to 17, with a mean (SD) of 12.93 (2.09) and a median of 13. Compliance rates to the semi-random signals averaged 87% across participants (Range = 58–100%), and compliance with end-of-day ratings averaged 89% (Range = 24–100%). Additionally, results of a chi-square analysis revealed that the frequencies of the daily anxiety trajectories did not significantly differ across the first and second week of EMA (Χ2 = 10.42; df = 6; p = .108).
Model Identification
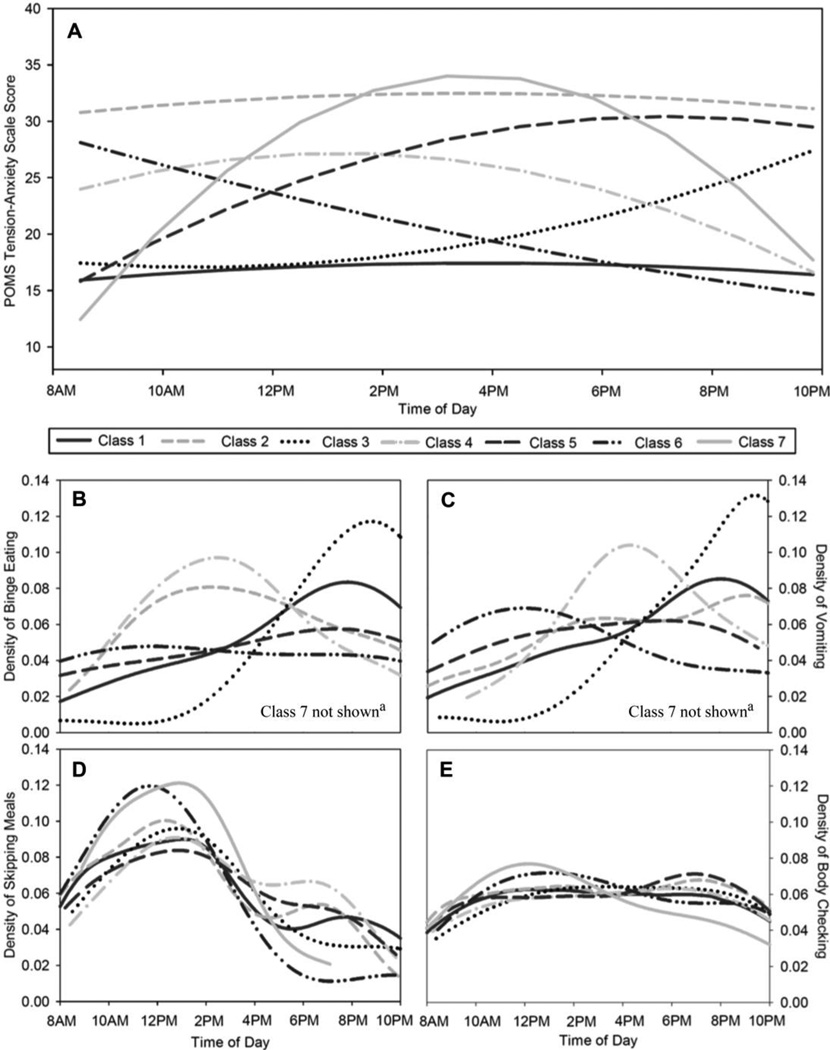
LGMM models comprised of 1 to 8 latent classes were evaluated (see Table 1). Two of the three fit indices (BIC and cAIC) reached a minimum for the 7-class model. Although the aBIC did not achieve a minimum, both the cAIC and BIC are known to be more conservative indices that favor more parsimonious models (Kadane & Lazar, 2004; Tofighi & Enders, 2008). Further, the BIC and cAIC are both consistent criteria and therefore tend to identify the correct model more frequently as sample size increases (Tofighi & Enders, 2008). In light of the agreement between the more conservative BIC and cAIC indices, and given that the 7-class model was characterized by the highest entropy value, this model for the anxiety trajectories was selected as the best fitting. The seven identified trajectories of anxiety are shown in Figure 1A, and the model parameters for each of the seven trajectories are presented in Table 2.
Table 1.
Results of Latent Growth Mixture Modeling for 1526 Ecological Momentary Assessment Days
| Number of Classes |
Number of Parameters |
LL | BIC | aBIC | cAIC | Entropy |
|---|---|---|---|---|---|---|
| 1 | 13 | −25304.2 | 50703.7 | 50662.4 | 50716.7 | - |
| 2 | 17 | −25184.5 | 50493.7 | 50439.7 | 50510.7 | 0.790 |
| 3 | 21 | −25083.9 | 50321.7 | 50255.0 | 50342.7 | 0.829 |
| 4 | 25 | −24987.0 | 50157.3 | 50077.9 | 50182.3 | 0.807 |
| 5 | 29 | −24925.6 | 50063.8 | 49971.7 | 50092.8 | 0.834 |
| 6 | 33 | −24885.6 | 50013.1 | 49908.2 | 50046.1 | 0.841 |
| 7 | 37 | −24868.6 | 50008.5 | 49891.0 | 50045.5 | 0.841 |
| 8 | 41 | −24855.2 | 50011.0 | 49880.7 | 50052.0 | 0.793 |
Note. LL = log likelihood; BIC = Bayesian information criterion; aBIC = sample size-adjusted Bayesian information criterion; cAIC = consistent Akaike information criterion.
Figure 1.
(A) Latent classes of daily anxiety trajectories; (B) Temporal distribution of binge eating across trajectories; (C) Temporal distribution of self-induced vomiting across trajectories; (D) Temporal distribution of skipping meals across trajectories; (E) Temporal distribution of body checking across trajectories. These figures display the distributions of behaviors across the day between 8AM and 10PM, but the functions computed for the distributions included all behaviors (including those that occurred outside this time window). a Density estimates for Class 7 are not displayed for binge eating or vomiting because only one episode of binge eating and no episodes of vomiting occurred in this class.
Table 2.
Proportions, Parameter Estimates, and Standard Errors for 7-Class Latent Growth Mixture Model
| Class | Anxiety Trajectory Description |
Number (Proportion)a of Days |
Intercept |
Linear |
Quadratic |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | p | Est. | SE | p | Est. | SE | p | |||
| 1 | Stable Low | 1089 (.714) | 15.92 | .63 | <.001 | 1.10 | .25 | <.001 | −.20 | .05 | <.001 |
| 2 | Stable High | 214 (.140) | 30.79 | 1.46 | <.001 | 1.29 | .45 | .004 | −.24 | .07 | .001 |
| 3 | Late Increasing | 74 (.049) | 17.44 | 1.00 | <.001 | −.95 | .61 | .119 | .59 | .14 | <.001 |
| 4 | Late Decreasing | 66 (.043) | 23.98 | 2.78 | <.001 | 3.60 | 1.81 | .047 | −1.02 | .28 | <.001 |
| 5 | Early Increasing | 38 (.025) | 15.82 | 1.79 | <.001 | 7.32 | 1.05 | <.001 | −.92 | .15 | <.001 |
| 6 | Early Decreasing | 34 (.022) | 28.11 | 2.77 | <.001 | −3.65 | 2.11 | .085 | .19 | .34 | .577 |
| 7 | Inverted U-Shape | 11 (.007) | 12.44 | 3.08 | <.001 | 16.21 | 5.01 | .001 | −3.03 | .86 | <.001 |
Note. Est. = Estimate; SE = Standard Error.
Proportions based upon most likely latent class membership
The two most frequent trajectories that were identified were characterized by stable anxiety across the day: Class 1, labeled “Stable Low,” accounted for 71.4% of all days and Class 2, labeled “Stable High,” accounted for 14.0%. Two trajectories were characterized by anxiety changes later in the day. Class 3, labeled “Late Increasing,” accounted for 4.9% of all days and was characterized by lower anxiety during the morning and mid-afternoon, with increasing anxiety through the late afternoon and evening. Class 4, labeled “Late Decreasing,” accounted for 4.3% of all days and was characterized by moderate levels of anxiety during the morning, rising slightly through the early afternoon and then decreasing to a low level by the end of the day. Two other trajectories were characterized by changes in anxiety that began early in the day. Class 5, labeled “Early Increasing,” accounted for 2.5% of all days and was characterized by a lower level of anxiety in the morning, followed by rising anxiety that peaks in early evening and then remains high. Class 6, labeled “Early Decreasing,” accounted for 2.2% of all days and was characterized by high levels of anxiety during the morning and a steady decrease to a low level by the end of the day. The final trajectory reflected a dramatic change in anxiety levels over the course of the day. Class 7, labeled “Inverted U-Shape,” accounted for 0.7% of all days and was characterized by the lowest levels anxiety during the morning, followed by a rapid increase until a peak during the mid- to late-afternoon and a rapid decrease to a low level during the evening. Given the low frequency of this trajectory and associated concerns regarding the validity of conducting analyses with such a small class, it was excluded from the subsequent trajectory comparison analyses, although it was retained in the descriptive data presented below, as well as in the examination of the within-trajectory temporal distribution of ED behaviors.
The primary purpose of this study was to classify days (rather than individuals) into clinically relevant anxiety trajectories (i.e., latent classes), given that individuals’ anxiety patterns might vary across days. Therefore, it was important to determine the extent to which individuals exhibited a variety of daily anxiety trajectories to ensure that classifying days was different than classifying people. The number of different daily trajectories for a single participant ranged from 1 to 7, with a mean (SD) of 2.42 (1.39). Approximately 30% (n = 35) of participants exhibited one type of trajectory, 32% (n = 38) had two, 19% (n = 22) had three, and 19% (n = 23) had four or more. Among the 35 participants who exhibited only one anxiety trajectory, approximately 89% (n = 31) had all Stable Low anxiety days and 11% (n = 4) had only Stable High anxiety days. Taken together, these findings provide support for the utility of classifying days to reflect variability in daily anxiety patterns within individuals.
ED Behaviors across Trajectories
Significant differences between the trajectories were found for the rates of binge eating (Wald Χ2 = 30.93; df = 5; p < .001), self-induced vomiting (Wald Χ2 = 12.94; df = 5; p = .024), and body checking (Wald Χ2 = 14.97; df = 5; p = .010). The percentage of days on which each behavior occurred in each trajectory is presented in Table 3. Rates of binge eating for the Stable High (Class 2; 24.3%), Late Increasing (Class 3; 27%), and Late Decreasing (Class 4; 22.7%) trajectories were significantly greater than in the Stable Low trajectory (Class 1; 9.7%), which served as the reference category. Additionally, rates of self-induced vomiting in the Stable High trajectory (Class 2; 34.6%) were significantly higher than rates in the Stable Low trajectory (Class 1; 14.4%), whereas body checking rates in the Late Increasing trajectory (Class 3; 71.6%) were significantly higher than rates in the Stable Low trajectory (Class 1; 47.3%). No significant differences between trajectories were found for exercise (Wald Χ2 = 7.27; df = 5; p = .201).
Table 3.
Binge Eating, Self-Induced Vomiting, and Body Checking across Daily Anxiety Trajectories
| Class | Anxiety Trajectory Description |
Binge Eating |
Self-Induced Vomiting |
Body Checking |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | OR | 99% CI | p | % | OR | 99% CI | p | % | OR | 99% CI | p | ||
| 1 | Stable Low |
9.7% | --- | --- | --- | 14.4% | --- | --- | --- | 47.3% | --- | --- | --- |
| 2 | Stable High |
24.3% | 2.98 | 1.05–8.42 | .007 | 34.6% | 3.14 | 1.11–8.87 | .005 | 52.8% | 1.25 | 0.43–3.58 | .590 |
| 3 | Late Increasing |
27.0% | 3.43 | 1.48–7.97 | <.001 | 25.7% | 2.05 | 0.84–5.01 | .038 | 71.6% | 2.81 | 1.28–6.16 | <.001 |
| 4 | Late Decreasing |
22.7% | 2.73 | 1.04–7.18 | .008 | 25.8% | 2.06 | 0.76–5.58 | .062 | 63.6% | 1.95 | 0.86–4.45 | .037 |
| 5 | Early Increasing |
23.7% | 2.88 | 0.98–8.41 | .011 | 18.4% | 1.34 | 0.34–5.31 | .583 | 65.8% | 2.14 | 0.71–6.51 | .077 |
| 6 | Early Decreasing |
23.5% | 2.85 | 0.88–9.27 | .022 | 23.5% | 1.83 | 0.51–6.54 | .224 | 58.8% | 1.59 | 0.63–4.01 | .195 |
Note. OR = odds ratio compared to Class 1; 99% CI = 99% confidence interval for odds ratio. Significance was evaluated with an alpha value of .01.
Significant differences between the trajectories also were found for the rates of the three dietary restriction variables: skipping meals (Wald Χ2 = 17.94; df = 5; p = .003), no eating for 8 waking hours (Wald Χ2 = 17.75; df = 5; p = .003), and eating less than 1200 kcal in a day (Wald Χ2 = 12.71; df = 5; p = .026). The percentage of days on which the three dietary restriction behaviors were reported across the seven trajectories is shown in Table 4. In comparison to the percentage of days on which meals were skipped in the Stable Low trajectory (Class 1; 29.2%), significantly higher rates were found for the Late Increasing (Class 3; 44.6%) and Late Decreasing (Class 4; 50.0%) trajectories. Further, rates of going 8 hours without eating in the Late Increasing trajectory (Class 3; 21.6%) were significantly higher than rates in the Stable Low trajectory (Class 1; 8.6%), whereas rates of eating less than 1200 kcal in the Late Decreasing trajectory (Class 4; 48.5%) were significantly higher than rates in the Stable Low trajectory (Class 1; 26.4%). Using post-hoc pairwise comparisons based on estimated marginal means, none of the trajectory differences (other than those differences from the Stable Low trajectory noted above) reached statistical significance (at an alpha of .01) for any of the ED behaviors.
Table 4.
Skipping Meals, No Eating for 8 Waking Hours, and Consuming Less Than 1200 kcal across Daily Anxiety Trajectories
| Class | Anxiety Trajectory Description |
Skipping Meals |
No Eating for 8 Waking Hours |
Consuming < 1200 kcal in a Day |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | OR | 99% CI | p | % | OR | 99% CI | p | % | OR | 99% CI | p | ||
| 1 | Stable Low |
29.2% | --- | --- | --- | 8.6% | --- | --- | --- | 26.4% | --- | --- | --- |
| 2 | Stable High |
37.9% | 1.48 | 0.64–3.42 | .232 | 15.0% | 1.86 | 0.64–5.38 | .132 | 26.6% | 1.01 | 0.34–2.99 | .982 |
| 3 | Late Increasing |
44.6% | 1.95 | 1.03–3.68 | .007 | 21.6% | 2.92 | 1.34–6.35 | <.001 | 36.5% | 1.60 | 0.74–3.45 | .116 |
| 4 | Late Decreasing |
50.0% | 2.42 | 1.11–5.32 | .004 | 19.7% | 2.60 | 0.80–8.41 | .037 | 48.5% | 2.62 | 1.07–6.40 | .006 |
| 5 | Early Increasing |
47.4% | 2.18 | 0.86–5.53 | .031 | 18.4% | 2.39 | 0.69–8.27 | .071 | 47.4% | 2.50 | 0.79–7.96 | .041 |
| 6 | Early Decreasing |
26.5% | 0.87 | 0.35–2.20 | .705 | 8.8% | 1.02 | 0.25–4.24 | .965 | 38.2% | 1.72 | 0.58–5.09 | .197 |
Note. OR = odds ratio compared to Class 1; 99% CI = 99% confidence interval for odds ratio. Significance was evaluated with an alpha value of .01.
A second set of analyses were conducted to examine differences among the anxiety trajectories in the occurrence of ED behaviors, controlling for trait affective lability (i.e., DAPP-BQ affective lability scale). Significant differences between the trajectories were found for the rates of binge eating (Wald Χ2 = 21.16; df = 5; p < .001), body checking (Wald Χ2 = 11.36; df = 5; p = .045), no eating for 8 waking hours (Wald Χ2 = 15.34; df = 5; p = .009), and eating less than 1200 kcal in a day (Wald Χ2 = 13.62; df = 5; p = .018). Specifically, the Late Increasing trajectory (Class 3) significantly differed from the Stable Low trajectory (Class 1) for binge eating (OR = 3.09, CI99% = 1.24–7.67, p = .001), body checking (OR = 2.64, CI99% = 1.17–5.93, p = .002), and no eating for 8 waking hours (OR = 2.84, CI99% =1.23–6.57, p = .001). The Late Decreasing trajectory (Class 4) significantly differed from the Stable Low trajectory (Class 1) for eating less than 1200 kcal in a day (OR = 2.63, CI99% = 1.12–6.18, p = .004). No significant differences between trajectories were found for self-induced vomiting (Wald Χ2 = 4.81; df = 5; p = .440), and although there was an overall effect for the anxiety trajectories for meal skipping (Wald Χ2 = 12.88; df = 5; p = .025), none of the trajectory comparisons were significant at the adjusted alpha of .01.
Temporal Distribution of ED Behaviors within Trajectories
Kernel density estimation was used to characterize the temporal distribution of binge eating, vomiting, skipping meals, and body checking across the day within each trajectory, estimating the probability that a given behavior occurred at each hour over 24 hours. Results of the density estimations revealed distinct patterns in the distribution of the various ED behaviors throughout the day across the trajectories (i.e., 8AM to 10PM; see Figure 1B-1E). Specifically, some probabilities peaked in the early to mid-afternoon, others peaked in the evening, and others exhibited no peaks, with approximately equal probabilities across the day.
Binge eating was most likely to occur in the evening on Stable Low anxiety days. Binge eating was also more likely in the evenings on Late Increasing anxiety days, although the peak in the probability was more dramatic. In contrast, on Stable High and Late Decreasing anxiety days, the highest likelihood of binge eating was during the afternoon. Finally, Early Increasing and Early Decreasing anxiety days were characterized by binge eating probabilities that were roughly equivalent throughout the course of the day.
Self-induced vomiting was most likely to occur in the evening on both Stable Low and Late Increasing anxiety days, although the peak in the probability of vomiting was more dramatic on Late Increasing anxiety days. In comparison, vomiting was most likely to occur in the late afternoon on Late Decreasing anxiety days and around noon on Early Decreasing anxiety days. Finally, on Stable High and Early Increasing anxiety days, the probability of vomiting gradually increased over the course of the day.
The temporal distribution of skipping meals was less variable than the distributions for binge eating and self-induced vomiting. In general, the probability of skipping meals was highest at around noon (i.e., lunch time) for all anxiety trajectories, although some were characterized by smaller, secondary peaks in the early evening (i.e., dinner time). Similarly, the distribution of body checking across the day did not dramatically vary across the anxiety trajectories. Slight peaks in the probability of body checking occurred in the early afternoon for some trajectories, and in the evening hours for others.
Association between Baseline Characteristics and Trajectories
Of the four analyses examining differences between the trajectories for the diagnostic variables of interest, only the presence of any current mood disorder was found to be associated with the anxiety trajectories (Wald Χ2 = 19.00; df = 5; p = .002). Specifically, the Stable High (Class 2; OR = 7.37, CI99% =2.08 −26.10, p < .001) and Early Increasing (Class 5; OR = 4.37, CI99% =1.12–17.06, p = .005) trajectories were more likely to occur among those with a current mood disorder. No significant differences between trajectories were found for full versus subthreshold AN (Wald Χ2 = 3.95; df = 5; p = .557) or AN restricting versus AN binge eating-purging type (Wald Χ2 = 8.94; df = 5; p = .112), and although there was an overall effect for the anxiety trajectories for the presence of any current anxiety disorder (Wald Χ2 = 13.89; df = 5; p = .016), none of the trajectory comparisons were significant at the adjusted alpha of .01.
Spearman Rho correlations were calculated to examine the association between proportions of anxiety trajectories and the baseline personality variables (see Table 5). The correlations revealed small positive associations (rs = .244 to .296, ps < .01) between the four DAPP-BQ scales and the Stable High trajectory proportion, as well as small to moderate negative associations (rs = −.278 to −.412, ps < .01) between the four personality variables and the Stable Low trajectory proportion. Additionally, a small positive association between the Late Decreasing trajectory proportion and DAPP-BQ Affective Lability was found. No other correlations were significant at the adjusted alpha of .01.
Table 5.
Spearman Rho Correlations between Anxiety Trajectory Proportions and Baseline Personality Variables
| DAPP-BQ Affective Lability |
DAPP-BQ Self-Harm |
DAPP-BQ Oppositionality |
DAPP-BQ Social Avoidance |
|
|---|---|---|---|---|
| Stable Low Proportion | −.412 | −.278 | −.302 | −.302 |
| Stable High Proportion | .285 | .296 | .269 | .244 |
| Late Increasing Proportion | .150 | .054 | .134 | .044 |
| Late Decreasing Proportion | .317 | .232 | .226 | .164 |
| Early Increasing Proportion | .159 | .236 | .179 | .200 |
| Early Decreasing Proportion | .104 | .132 | .037 | .071 |
Note. DAPP-BQ=Dimensional Assessment of Personality Pathology-Basic Questionnaire. Bolded values represent significant correlations evaluated with an alpha value of .01.
Discussion
Given that individuals may experience differing patterns of anxiety from day-to-day, there is utility in considering within-person variability in the tendency to experience particular patterns, as well as the way the varying patterns are associated with the occurrence of ED behaviors. Using an innovative approach that has been applied in only one previous study in the ED literature (Crosby et al., 2009), the current study classified days rather than individuals and identified seven daily anxiety trajectories in a sample of women with full or subthreshold AN: Stable Low, Stable High, Late Increasing, Late Decreasing, Early Increasing, Early Decreasing, and Inverted U-Shape. In examining the occurrence of ED behaviors in each trajectory compared to the Stable Low anxiety trajectory, binge eating was found to be more frequent on Stable High, Late Increasing, and Late Decreasing anxiety days, whereas self-induced vomiting was more likely only on Stable High days. Body checking and going 8 hours without eating was more likely to occur on Late Increasing anxiety days. Skipping meals was more common on Late Increasing and Late Decreasing anxiety days, whereas consuming less than 1200 kcal was more likely to occur only on Late Decreasing anxiety days. Additionally, an examination of the daily temporal distribution of ED behaviors within the trajectories revealed a number of distinct patterns. Of particular note, the Late Decreasing trajectory was associated with binge eating and vomiting earlier in the day compared to other trajectories, suggesting the possible impact of these behaviors on anxiety (e.g., behaviors reducing anxiety). In contrast, the Late Increasing trajectory was associated with binge eating and vomiting later in the day, perhaps reflecting the accumulating risk of increasing anxiety as an antecedent to these behaviors.
An additional goal of this study was to examine the extent to which baseline diagnostic and personality variables were associated with the anxiety trajectories. Anxiety trajectories were only found to be associated with the presence of a current mood disorder, with those individuals diagnosed with a mood disorder exhibiting a greater frequency of Stable High and Early Increasing anxiety days compared to Stable Low anxiety days. Further, baseline personality traits including affective lability, self-harm, oppositionality, and social avoidance were found to be positively associated with the proportion of Stable High anxiety days and negatively associated with the proportion of Stable Low anxiety days. These findings demonstrate that those who experience more days characterized by consistently high anxiety are more likely to be diagnosed with a current mood disorder and to display higher levels of personality pathology.
The results of the current study contribute to the growing literature suggesting the importance of emotion variables in AN, demonstrating the wide variability (both within- and between-persons) in the daily experience of anxiety, as well as the associated likelihood of ED behaviors. In particular, a substantial proportion of women in this study exhibited multiple anxiety trajectories during their participation, and findings of significant associations between trajectories and several ED behaviors, even when controlling for the conceptually relevant personality trait of affective lability, suggest a strong association between varying patterns of anxiety in the natural environment and the occurrence of ED behaviors. Further, the finding that the daily timing of certain ED behaviors (e.g., binge eating and self-induced vomiting) varies across the anxiety trajectories demonstrates further heterogeneity, perhaps reflecting a functional relationship between anxiety and these ED behaviors in AN, although the current study cannot address the casual nature of this association. Finally, these findings build upon those reported by Crosby et al. (2009) in their study of patterns of broad negative affect in women with BN. The trajectories identified in the current study are highly consistent with those from the Crosby and colleagues study, with the exception that the latter identified two additional trajectories (U-Shaped and Stable Moderate) not found in the current investigation. Of note, the Stable Low trajectory was the largest in both studies and the highly variable pattern (i.e., Inverted-U shape) identified in both studies was similarly infrequent. Additionally, the findings in the current study that binge eating was more common on Late Increasing and Stable High anxiety days, and that self-induced vomiting was more common on Stable High anxiety days, were consistent with the results from the BN study. Notable differences in the findings are the greater frequency of Stable High anxiety days in the current study compared to the corresponding Stable High NA trajectory identified by Crosby et al., as well as the finding in the BN study that the Early Increasing NA trajectory was associated with a greater likelihood of binge eating and purging.
The findings of the current study should be considered in light of certain limitations. First, participants may not have reported every instance of an ED behavior, although signal contingent responses offered the opportunity to report behaviors that had not previously been recorded in the preceding hours. Second, although the results highlight the heterogeneity in anxiety patterns and their associations with ED behaviors in women with AN, it should be noted that these behaviors did occur on some Stable Low anxiety days. However, this trajectory does not indicate the absence of anxiety, as evidenced by the fact that the level of anxiety reflected by the trajectory corresponds to an average response of approximately two (on a one to five scale) for each of the eight items of the POMS tension-anxiety scale. It is therefore likely that there are additional variables (other than anxiety) relevant to the occurrence of these behaviors that were not included in the current study. Third, the decision to use Stable Low anxiety days as the reference for the trajectory comparisons stemmed from the goal of facilitating comparisons with previous studies (i.e., Crosby et al., 2009), as well as the view that Stable Low anxiety days are conceptually distinct from days characterized by higher or fluctuating anxiety. However, differing likelihoods of ED behaviors across the other trajectories would also be of potential relevance. Unfortunately, the smaller size of the other trajectory classes likely limited our ability to reach statistical significance in the post-hoc pairwise comparisons between the various trajectories. A final potential limitation inherent in EMA methodology is reactivity. However, results from previous studies with ED samples have provided little evidence for reactivity (Crosby et al., 2009; Stein & Corte, 2003). Additionally, the frequency of daily anxiety trajectories did not significantly differ between the first and second week of EMA, providing further evidence that reactivity was likely minimal.
Clinical Implications
These results provide support for a link between patterns of anxiety and ED behaviors in AN. Although the nature of the analyses precludes determining the precise temporal order of this association, three possibilities exist. First, consistent with etiological/maintenance models of negative reinforcement that posit NA as an important antecedent of binge eating, high levels of anxiety may be a momentary risk factor that predisposes individuals to engage in certain ED behaviors, with anxiety levels subsequently decreasing. Second, individuals may exhibit an increase in anxiety after engaging in ED behaviors (e.g., anxiety subsequent to body checking due to the perception of having gained weight). Third, anxiety and the elevated likelihood of ED behaviors may not share a direct causal association and may instead result from some other variable (e.g., interpersonal difficulties, body dissatisfaction).
Although additional research is needed to fully elaborate on the nature of the anxiety–ED behavior associations identified in this study, the current findings may have implications for the treatment of people with AN. Specifically, it is likely that individuals with AN may vary in how their daily anxiety patterns and their ED behaviors are related, with some experiencing higher antecedent anxiety followed by lower anxiety levels subsequent to ED behaviors (e.g., negative reinforcement of binge eating or self-induced vomiting), and others exhibiting higher anxiety after certain ED behaviors (e.g., anxiety as a consequence of body checking). Further, these associations may vary across behaviors that are characterized by different functions in AN. Eliciting information about the temporal relationship of a patient’s daily anxiety patterns and ED behaviors may therefore aid in identifying emotional states and times of day associated with greater risk of ED behaviors.
Similarly, these findings suggest that the use of an ecological momentary intervention (EMI), a type of treatment involving clinical information or recommendations (e.g., skills for coping with NA) being delivered to individuals in the moment in their everyday lives, may have some utility in treating ED symptoms in this clinical population. EMIs may provide patients with recommendations at pre-established times (e.g., during the times when she most frequently reports struggling with anxiety), or they may utilize momentary assessment findings as indicators of the need for an intervention (e.g., when a patient reports high anxiety as part of therapeutic self-monitoring; see Heron & Smyth, 2010 for a review of EMIs). For instance, individuals with AN who engaged in ongoing, momentary self-monitoring on a mobile electronic device could be prompted with information on adaptive ways of coping with anxiety when a series of self-report ratings indicate a trajectory of anxiety that suggests an increased risk of an ED behavior (i.e., consistently increasing anxiety through the afternoon and evening). This focus on adaptive ways of responding to momentary risk factors (e.g., anxiety, NA, interpersonal stressors) is a hallmark of several ED treatments, particularly Dialectical Behavior Therapy (DBT; Safer, Telch, & Chen, 2009) and Integrative Cognitive Affective Therapy (ICAT; Wonderlich et al., 2008). For example, the distress tolerance module in DBT emphasizes momentary skills for coping during times of emotional turmoil. Similarly, ICAT focuses on addressing momentary self-discrepancy, which is viewed as a precursor to the negative affective experiences that ultimately trigger ED behaviors. However, as noted previously, the current findings do not address the causal nature of the association between anxiety patterns and ED behaviors in AN, thus additional research will be necessary to provide a stronger foundation for the potential utility of EMIs in the treatment of AN.
Conclusion
The present study identified daily trajectories of anxiety using data from a large sample of women with full or subthreshold AN who reported on their behaviors and anxiety in the natural environment. The use of EMA offered several advantages over retrospective assessment methods, which are subject to recall biases and other memory effects. This study also used an innovative statistical approach to examine the association between anxiety and ED behaviors in AN, as well as the link between state-based anxiety patterns and baseline diagnostic and trait personality variables. Seven distinct daily anxiety patterns were identified, with several exhibiting unique associations with ED behaviors, even when controlling for trait affective lability. These anxiety patterns are consistent with NA trajectories found in BN (Crosby et al., 2009), suggesting that these patterns are not unique to women with AN. Finally, evidence supporting an association between anxiety patterns in the natural environment and trait personality variables may help inform the development of more effective interventions.
Acknowledgments
This research was supported by R01 MH059674 and T32 MH082761 from NIMH, and P30 DK50456 from NIDDK.
Contributor Information
Jason M. Lavender, Neuropsychiatric Research Institute, Fargo, ND
Kyle P. De Young, Department of Psychology, University of North Dakota
Stephen A. Wonderlich, Neuropsychiatric Research Institute, Fargo, ND and University of North Dakota School of Medicine and Health Sciences
Ross D. Crosby, Neuropsychiatric Research Institute, Fargo, ND and University of North Dakota School of Medicine and Health Sciences
Scott G. Engel, Neuropsychiatric Research Institute, Fargo, ND and University of North Dakota School of Medicine and Health Sciences
James E. Mitchell, Neuropsychiatric Research Institute, Fargo, ND and University of North Dakota School of Medicine and Health Sciences
Scott J. Crow, University of Minnesota
Carol B. Peterson, University of Minnesota
Daniel Le Grange, The University of Chicago.
References
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: APA Press; 1994. [Google Scholar]
- Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Archives of General Psychiatry. 2011;68:724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Bozdogan H. Model selection and Akaike’s information criteria (AIC): The general theory and its analytic extensions. Psychometrika. 1987;52:345–370. [Google Scholar]
- Brockmeyer T, Holtforth MG, Bents H, Kämmerer A, Herzog W, Friederich HC. Starvation and emotion regulation in anorexia nervosa. Comprehensive Psychiatry. 2012;53:496–501. doi: 10.1016/j.comppsych.2011.09.003. [DOI] [PubMed] [Google Scholar]
- Crosby RD, Wonderlich SA, Engel SG, Simonich H, Smyth J, Mitchell JE. Daily mood patterns and bulimic behaviors in the natural environment. Behaviour Research and Therapy. 2009;47:181–188. doi: 10.1016/j.brat.2008.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG. Cognitive behavior therapy and eating disorders. New York: Guilford; 2008. [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour Research and Therapy. 2003;41:509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Shafran R, Cooper Z. A cognitive behavioural theory of anorexia nervosa. Behaviour Research and Therapy. 1999;37:1–13. doi: 10.1016/s0005-7967(98)00102-8. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM–IV Axis I Disorders: Patient Edition (SCIDI/P) New York: Biometrics; 1995. [Google Scholar]
- Frank GKW, Roblek T, Shott ME, Jappe LM, Rollin MD, Hagman JO, Pryor T. Heightened fear of uncertainty in anorexia and bulimia nervosa. International Journal of Eating Disorders. 2012;45:227–232. doi: 10.1002/eat.20929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaudio S, Di Ciommo V. Prevalence of personality disorders and their clinical correlates in outpatient adolescents with anorexia nervosa. Psychosomatic Medicine. 2011;73:769–774. doi: 10.1097/PSY.0b013e318235b9b5. [DOI] [PubMed] [Google Scholar]
- Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychological Bulletin. 2011;137:660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halmi KA, Eckert E, Marchi P, Sampugnaro V, Apple R, Cohen J. Comorbidity of psychiatric diagnoses in Anorexia Nervosa. Archives of General Psychiatry. 1991;48:712–718. doi: 10.1001/archpsyc.1991.01810320036006. [DOI] [PubMed] [Google Scholar]
- Hambrook D, Oldershaw A, Rimes K, Schmidt U, Tchanturia K, Treasure J, Chalder T. Emotional expression, self-silencing, and distress tolerance in anorexia nervosa and chronic fatigue syndrome. British Journal of Clinical Psychology. 2011;50:310–325. doi: 10.1348/014466510X519215. [DOI] [PubMed] [Google Scholar]
- Harrison A, Sullivan K, Tchanturia K, Treasure J. Emotional functioning in eating disorders: Attentional bias, emotion recognition and emotion regulation. Psychological Medicine. 2010;40:1887–1897. doi: 10.1017/S0033291710000036. [DOI] [PubMed] [Google Scholar]
- Haynos AF, Fruzzetti AE. Anorexia Nervosa as a disorder of emotion dysregulation: Evidence and treatment implications. Clinical Psychology: Science and Practice. 2011;18:183–202. [Google Scholar]
- Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. British Journal of Health Psychology. 2010;15:1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzog DB, Keller MB, Lavori PW, Kenny GM, Sacks NR. The prevalence of personality disorders in 210 women with eating disorders. Journal of Clinical Psychiatry. 1992;53:147–152. [PubMed] [Google Scholar]
- Hilbert A, Tuschen-Caffier B. Maintenance of binge eating through negative mood: A naturalistic comparison of binge eating disorder and bulimia nervosa. International Journal of Eating Disorders. 2007;40:521–530. doi: 10.1002/eat.20401. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan J, Joyce PR, Carter FA, Horn J, McIntosh VV, Luty SE, Bulik CM. Specific and nonspecific comorbidity in anorexia nervosa. International Journal of Eating Disorders. 2008;41:47–56. doi: 10.1002/eat.20463. [DOI] [PubMed] [Google Scholar]
- Kadane JB, Lazar NA. Methods and criteria for model selection. Journal of the American Statistical Association. 2004;99:279–290. [Google Scholar]
- Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. American Journal of Psychiatry. 2004;161:2215–2221. doi: 10.1176/appi.ajp.161.12.2215. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Crosby RD, Engel SG, Cao L, Ndungu A, Crow SJ, Wonderlich SA. DSM-IV-Defined Anorexia Nervosa versus Subthreshold Anorexia Nervosa (EDNOS-AN) European Eating Disorders Review. 2013;21:1–7. doi: 10.1002/erv.2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Livesley WJ, Jackson DN. Dimensional Assessment of Personality Pathology— Basic Questionnaire: Technical manual. Port Huron, MI: Sigma Assessment Systems; 2009. [Google Scholar]
- Lorr M, McNair DM. The Profile of Mood States manual. San Diego, CA: Educational and Industrial Testing Services; 1971. [Google Scholar]
- Mazure CM, Halmi KA, Sunday SR, Romano SJ, Einhorn AM. The Yale-Brown-Cornell Eating Disorder Scale: Development, use, reliability, and validity. Journal of Psychiatric Research. 1994;28:425–445. doi: 10.1016/0022-3956(94)90002-7. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK. Integrating person-centered and variable centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism, Clinical and Experimental Research. 2000;24:882–891. [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Sixth Edition. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- Papadopoulos FC, Ekbom A, Brandt L, Ekselius L. Excess mortality, causes of death and prognostic factors in anorexia nervosa. British Journal of Psychiatry. 2009;194:10–17. doi: 10.1192/bjp.bp.108.054742. [DOI] [PubMed] [Google Scholar]
- Ramaswamy V, DeSarbo W, Reibstein D, Robinson W. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Marketing Science. 1993;12:103–124. [Google Scholar]
- Safer D, Telch C, Chen E. Dialectical behavior therapy for binge eating and bulimia. New York, NY: Guilford Press; 2009. [Google Scholar]
- SAS Institute Inc. SAS/STAT® User’s Guide, Version 8. Cary, NC: SAS Institute Inc; 1999. [Google Scholar]
- Schmidt U, Treasure J. Anorexia nervosa: Valued and visible. A cognitive interpersonal maintenance model and its implications for research and practice. British Journal of Clinical Psychology. 2006;45:343–366. doi: 10.1348/014466505x53902. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Sclove LS. Application of model-section criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- Shafran R, Fairburn CG, Robinson P, Lask B. Body checking and its avoidance in eating disorders. International Journal of Eating Disorders. 2004;35:93–101. doi: 10.1002/eat.10228. [DOI] [PubMed] [Google Scholar]
- Silverman BW. Density Estimation for Statistics and Data Analysis. London: Chapman and Hall; 1986. [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Smyth J, Wonderlich S, Crosby R, Miltenberger R, Mitchell J, Rorty M. The use of ecological momentary assessment approaches in eating disorder research. International Journal of Eating Disorders. 2001;30:83–95. doi: 10.1002/eat.1057. [DOI] [PubMed] [Google Scholar]
- Smyth J, Wonderlich SA, Heron K, Sliwinski M, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress predict binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Stein KF, Corte CM. Ecological momentary assessment of eating-disordered behaviors. International Journal of Eating Disorders. 2003;34:349–360. doi: 10.1002/eat.10194. [DOI] [PubMed] [Google Scholar]
- Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT. Rationale for the application of exposure and response prevention to the treatment of anorexia nervosa. International Journal of Eating Disorders. 2011;44:134–141. doi: 10.1002/eat.20784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinglass JE, Walsh BT. Habit learning and anorexia nervosa: A cognitive neuroscience hypothesis. International Journal of Eating Disorders. 2006;39:267–275. doi: 10.1002/eat.20244. [DOI] [PubMed] [Google Scholar]
- Steinhausen HC. Outcome of eating disorders. Child and Adolescent Psychiatry Clinics of North America. 2009;18:225–242. doi: 10.1016/j.chc.2008.07.013. [DOI] [PubMed] [Google Scholar]
- Stice E, Agras WS. Subtyping bulimic women along dietary restraint and negative affect dimensions. Journal of Consulting and Clinical Psychology. 1999;67:460–469. doi: 10.1037//0022-006x.67.4.460. [DOI] [PubMed] [Google Scholar]
- Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavioral medicine. Annals of Behavioral Medicine. 1994;16:199–202. [Google Scholar]
- Strober M. Pathologic fear conditioning and anorexia nervosa: On the search for novel paradigms. International Journal of Eating Disorders. 2004;35:504–508. doi: 10.1002/eat.20029. [DOI] [PubMed] [Google Scholar]
- Sullivan PF. Mortality in anorexia nervosa. American Journal of Psychiatry. 1995;152:1073–1074. doi: 10.1176/ajp.152.7.1073. [DOI] [PubMed] [Google Scholar]
- Tofighi D, Enders CK. Identifying the correct number of classes in growth mixture models. In: Hancock GR, Samuelsen KM, editors. Advances in Latent Variable Mixture Models. Greenwich, CT: Information Age Publishing, Inc; 2008. pp. 317–341. [Google Scholar]
- Vermut JK, Magidson J. Latent GOLD 4.0 User’s Guide. Belmont, MA: Statistical Innovations, Inc; 2005. [Google Scholar]
- Wagner A, Aizenstein H, Venkatraman V, Fudge J, May J, Mazurkewicz L, Kaye W. Altered reward processing in women recovered from anorexia nervosa. American Journal of Psychiatry. 2007;164:1842–1849. doi: 10.1176/appi.ajp.2007.07040575. [DOI] [PubMed] [Google Scholar]
- Wheeler L, Reis HT. Self-recording of everyday life events: Origins, types, and uses. Journal of Personality. 1991;59:339–354. [Google Scholar]
- Wildes JE, Ringham RM, Marcus MD. Emotion avoidance in patients with anorexia nervosa: Initial test of a functional model. International Journal of Eating Disorders. 2010;43:398–404. doi: 10.1002/eat.20730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson DA, White MA, York-Crowe E, Stewart TM. Cognitive- behavioral theories of eating disorders. Behavior Modification. 2004;28:711–738. doi: 10.1177/0145445503259853. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Engel SG, Peterson CB, Robinson MD, Crosby RD, Mitchell JE, Simonich HK. Examining the conceptual model of Integrative Cognitive-Affective Therapy for BN: Two assessment studies. International Journal of Eating Disorders. 2008;41:748–754. doi: 10.1002/eat.20551. [DOI] [PubMed] [Google Scholar]
- Yackobovitch-Gavan M, Golan M, Valevski A, Kreitler S, Bachar E, Lieblich A, Stein D. An integrative quantitative model of factors influencing the course of anorexia nervosa over time. International Journal of Eating Disorders. 2009;42:306–317. doi: 10.1002/eat.20624. [DOI] [PubMed] [Google Scholar]