Abstract
Purpose
Prolonged sitting has emerged as a risk factor for early mortality, but the extent of benefit realized by replacing sitting time with exercise, or activities of everyday living (i.e. non-exercise activities), is not known.
Methods
We prospectively followed 154,614 older adults (59–82 years) in the NIH-AARP Diet and Health Study who reported no major chronic diseases at baseline and reported detailed information about sitting time, exercise, non-exercise activities. Proportional hazards models were used to estimate adjusted hazard ratios and 95% confidence intervals (HR [95%CI]) for mortality. An isotemporal modeling approach was used to estimate associations for replacing sitting time with specific types of physical activity, with separate models fit for less active and more active participants to account for non-linear associations.
Results
During 6.8 (SD=1.0) years of follow-up 12,201 deaths occurred. Greater sitting time (≥ 12 vs. < 5 hrs/d) was associated with increased risk for all-cause and cardiovascular mortality. In less active adults (< 2 hrs/d total activity), replacing one hour of sitting per day with an equal amount of activity was associated with lower all-cause mortality for both exercise (HR=0.58 [0.54,0.63]) and non-exercise activities (HR=0.70 [0.66,0.74]), including household chores, lawn and garden work, and daily walking. Among more active participants (2+ hrs/d total activity) replacement of sitting time with purposeful exercise was associated with lower mortality (HR=0.91 [0.88–0.94]), but not with non-exercise activity (HR=1.00 [0.98–1.02]). Similar results were noted for cardiovascular mortality.
Conclusions
Physical activity intervention strategies for older adults often focus on aerobic exercise, but our findings suggest that reducing sitting time and engaging in a variety of activities is also important, particularly for inactive adults.
Keywords: sedentary behavior, prevention, lifestyle activities, cancer
INTRODUCTION
In modern societies that have largely engineered obligatory physical activity out of daily life (22, 27), encouraging participation in moderate-vigorous aerobic exercise has been a key public health strategy for reducing the risk for non-communicable diseases and early mortality (26). However, recent studies have challenged the idea that a few hours per week of aerobic exercise is alone sufficient to fully mitigate mortality risks (16, 23, 25) associated with the many hours that adults spend in sedentary behavior (16). In part, this may reflect that elevated health risks associated with excessive sitting arise from the displacement of routine daily activities by sitting behaviors (8, 16). Activities typically displaced by prolonged sitting include daily activities like household chores (e.g., cooking, cleaning, shopping), as well as moderate-vigorous activities not typically classified as aerobic exercise (e.g. vacuuming, sweeping, mowing, gardening). We refer to such behaviors as non-exercise physical activities to distinguish them from exercise done for health and fitness (26), and from sedentary time. Implicit in the displacement hypothesis is that replacing sitting time with physically active behaviors will be associated with lower disease risk. However, few studies have estimated the mortality benefits associated with replacement of sitting time with an equal amount of time in either purposeful exercise or other non-exercise activities.
In this report we extend our earlier finding that excessive sedentary time was associated with greater mortality(16) and, using more detailed measurements of physical activity and sitting time, we estimate the mortality benefits associated with replacement of sitting time with different types of physical activity. To do so we are among the first to employ a novel isotemporal modeling approach that facilitates investigation of the mortality trade-offs between spending time in either sedentary behavior or physical activity (2, 19). Clarifying what types of physical activity are healthful alternatives to sitting is critical for the development of evidenced-based recommendations for reducing sedentary time and increasing physical activity, and since results from randomized trials of sedentary time and mortality are unavailable, prospective observational studies provide essential insights.
METHODS
The NIH-AARP Diet and Health Study was established in 1995–96 when 566,398 AARP members (50–71 years) in six states and two metropolitan areas responded to a questionnaire about their medical history, diet, and demographics(30). A Follow-up Questionnaire asking detailed questions about active and sedentary behaviors, medical history and risk factors was completed by 318,714 participants in 2004–2006. Those eligible for this analysis (N=154,614) personally responded to both questionnaires, were free of major diseases at the start of follow-up (2004–2006), and had sufficiently complete exposure data (see Document, Supplementary Digital Content (SDC) 1: Methods for Development of the Analytic Study Sample). Questionnaire completion was considered to imply informed consent. The US National Cancer Institute’s Special Studies Institutional Review Board approved the study.
Assessment of Physical Activity and Sedentary Behaviors
The physical activity questionnaire asked how much time per week was spent in 16 activities during the past 12 months. Activities were classified as exercise and sports (8 questions) and as non-exercise activity (8 questions), including household chores (5 questions), lawn and garden (2 questions), and daily walking activities (1 question). Activity duration (hrs/d) was calculated as the sum of all exercise, non-exercise, and all activities (i.e., Overall physical activity). For descriptive purposes, an energy cost of each activity was assigned using standard methods, and physical activity energy expenditure was calculated (MET-hrs/d). Three sitting questions asked about the number of hours spent “in a typical 24-hour period during the past 12 months”. See Document, SDC 2: Assessment of Physical Activity and Sedentary Behaviors, and Figure footnotes for details. The exercise items have been validated against physical activity diaries, r=0.62 and 0.65 (3, 34).
End Point Ascertainment and Covariate Assessment
Vital status was determined through linkage with the Social Security Administration Death Master File, and the National Death Index. The primary end points for our analysis were mortality from all-causes, cardiovascular disease, and cancer. A broad range of covariates were evaluated as potential confounders to the associations of interest (see Table 1).
Table 1.
Characteristics of participants, by overall physical activity and sitting time (hrs/d)
| Overall Physical Activity (hrs/d) | Overall Sitting Time (hrs/d) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | < 1.0 | 1.0 to 1.9 | 2.0 to 2.9 | 3.0 to 3.9 | ≥ 4.0 | < 5 | 5 to 6.9 | 7 to 8.9 | 9 to 11.9 | ≥12 |
| N | 26,065 | 43,541 | 36,216 | 22,517 | 26,275 | 13,634 | 38,368 | 42,520 | 28,174 | 31,918 |
| Age (yrs) | 70.2 | 69.9 | 69.9 | 69.7 | 69.4 | 69.8 | 69.8 | 70.2 | 69.9 | 69.4 |
| Men (%) | 60.9 | 57.0 | 51.2 | 47.0 | 44.8 | 52.9 | 54.0 | 54.0 | 52.6 | 49.7 |
| Body mass index (%) | ||||||||||
| Normal weight (< 25 kg/m2) | 26.1 | 32.3 | 35.4 | 37.5 | 38.7 | 28.6 | 39.3 | 35.6 | 32.0 | 28.7 |
| Overweight (25–29.9 kg/m2) | 35.0 | 36.9 | 36.3 | 35.7 | 35.5 | 25.8 | 35.7 | 37.9 | 38.3 | 36.3 |
| Obese (≥ 30 kg/m2) | 27.1 | 20.0 | 17.6 | 16.6 | 16.0 | 12.0 | 14.6 | 18.5 | 22.3 | 27.1 |
| College degree (%) | 44.9 | 48.2 | 47.2 | 45.3 | 41.8 | 48.4 | 48.5 | 46.2 | 44.6 | 42.2 |
| Working/not retired (%) | 23.1 | 22.2 | 19.7 | 18.9 | 20.0 | 15.9 | 21.4 | 17.5 | 20.5 | 27.2 |
| Smoking history (%) | ||||||||||
| Never | 38.6 | 40.0 | 41.4 | 42.1 | 43.7 | 43.4 | 42.9 | 41.0 | 39.8 | 38.9 |
| Former | 44.2 | 45.9 | 45.6 | 45.3 | 42.9 | 39.9 | 44.2 | 46.0 | 46.4 | 45.3 |
| Current | 6.0 | 5.1 | 4.8 | 4.8 | 5.2 | 4.3 | 4.2 | 4.9 | 5.5 | 6.6 |
| Health status at follow-up | ||||||||||
| High blood pressure (%) | 53.9 | 50.0 | 48.4 | 46.3 | 44.7 | 43.3 | 45.6 | 49.2 | 51.1 | 52.8 |
| High cholesterol (%) | 50.7 | 50.6 | 50.2 | 48.8 | 48.0 | 45.3 | 47.5 | 50.6 | 51.9 | 51.7 |
| Diabetes (%) | 17.6 | 12.5 | 10.8 | 9.8 | 9.7 | 10.2 | 10.0 | 11.5 | 13.1 | 15.4 |
| Depression (%) | 13.9 | 11.5 | 10.9 | 10.5 | 10.4 | 9.5 | 10.0 | 10.6 | 12.3 | 14.3 |
| General health (%) | ||||||||||
| Excellent | 11.1 | 15.6 | 18.1 | 19.3 | 21.8 | 16.5 | 20.3 | 16.8 | 15.5 | 14.9 |
| Very Good | 32.8 | 39.4 | 40.9 | 42.5 | 42.2 | 30.5 | 41.6 | 41.8 | 40.3 | 37.3 |
| Good | 34.8 | 30.4 | 27.9 | 26.2 | 25.3 | 21.3 | 26.1 | 30.0 | 31.3 | 32.8 |
| Fair | 11.3 | 6.3 | 5.0 | 4.5 | 3.8 | 4.2 | 4.5 | 5.5 | 7.3 | 8.8 |
| Poor | 1.7 | 0.5 | 0.3 | 0.3 | 0.2 | 0.4 | 0.3 | 0.4 | 0.6 | 1.1 |
| Sleep (hrs/d) | 6.8 | 6.9 | 7.0 | 7.0 | 6.9 | 6.8 | 6.9 | 7.0 | 7.0 | 6.9 |
Statistical analysis
Our first objectives were to determine the marginal effects of hours of sedentary behavior, exercise, and non-exercise activity on overall mortality. We therefore modeled each effect in a separate Cox Proportional Hazards Model and report estimated hazard ratios (HR) and 95% confidence intervals. Follow-up time was calculated from the scan date of the Follow-up Questionnaire until death from any cause or the end of the follow-up (December 31, 2011). Tests for trend were performed by entering the median values of each category in the models. Spearman correlations were used to describe the relation between exposures. Covariates that changed the magnitude of the sedentary behavior associations by at least 10% were retained in covariate adjusted models. To evaluate dose-response relationships and to determine whether associations were linear, restricted cubic splines were used. To fit the splines, 4 to 6 knots were distributed evenly across the range of the exposure (at 0.5 to 1 hr intervals) and splines were trimmed at ~95th percentile of each exposure distribution. We also tested for interactions between sex and physical activity and sitting time on mortality by entering the cross-products of sex (0,1) and the continuous versions of each behavioral exposure.
Our next objective was to determine the substitution effect of replacing sedentary behavior with each type of physical activity using the approach described by Mekary and colleagues (19). Therefore, we included exercise, non-exercise activity, and total reported time in a single cox model, where total time is the sum of all activities and siting time. In this model the variable for sitting time is not included (i.e., it is “dropped”), and resultant hazard ratios estimate associations for replacing one hour of sitting per day with an equal amount of time in a given type of activity. Because of the nonlinearity of the association between physical activity and mortality (p < 0.01), we fit separate models for less active (< 2 hrs/d of overall activity) and more active participants (≥ 2 hrs/d) in order to obtain summary estimates for an average effect within each group. These categories were determined post-hoc by evaluating overall physical activity and all-cause mortality using restricted cubic splines, where a plateau in risk reduction was noted at roughly 2 hrs/day of overall activity (see Figure, SDC 3: Supplemental Figure 1. Association between all-cause mortality and overall physical activity).
Sensitivity analyses examined our primary results for reverse causality by excluding participants that accumulated less than two years of follow-up. SAS 9.1 (SAS Institute Inc., Cary, NC) was used; statistical tests were two-sided.
RESULTS
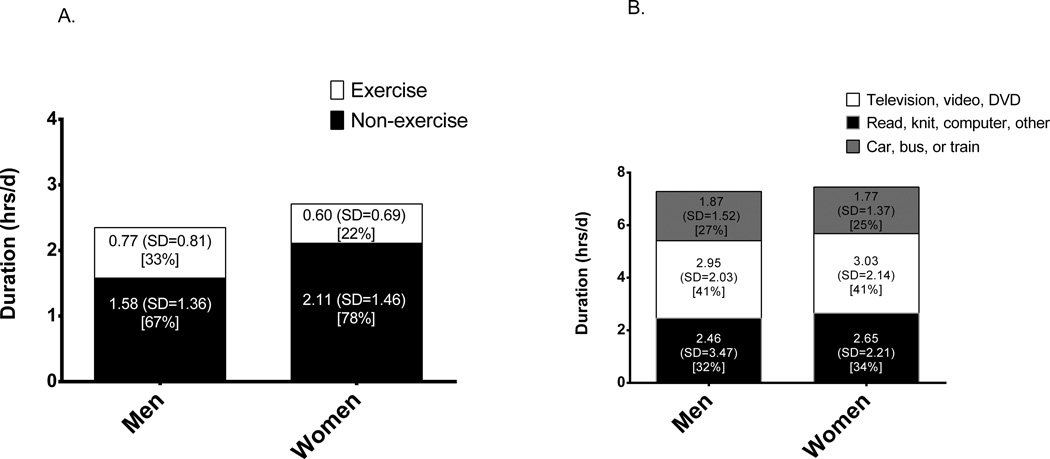
During 6.8 (SD=1.0) years of follow-up, 7,218 deaths in men and 4,983 deaths in women occurred. Sedentary behavior and physical activity were associated with age, education, obesity, smoking, co-morbid health conditions, and general health status (Table 1). Women reported more time in overall (2.70 vs. 2.35 hrs/d) and non-exercise activity than men, but less time in exercise (Figure 1, Panel A). Non-exercise activity was mostly derived from household chores (43%), followed by lawn and garden (15%) and daily walking (14%) in men and women combined. Less active participants (< 2 hrs/d of total activity, n=69,606) reported 1.15 (SD=0.50) hrs/d of activity and 4.5 (SD=2.2) MET-hrs/d of energy expenditure, while more active participants (n=85,008) reported 3.64 (SD=1.50) hrs/d of activity and 14.0 (SD=6.4) MET-hrs/d of expenditure (See also Figure, SDC 4: Supplemental Figure 2. Physical activity energy expenditure (MET-hrs/d) in less and more active participants, by sex). The proportion of total activity derived from exercise and non-exercise activity was similar in less and more active participants. Time spent sitting overall was similar for men (7.3 [SD=3.4] hrs/d) and women (7.5 [SD=3.5] hrs/d) (Figure 1, Panel B). Correlations between exercise and non-exercise physical activity were weakly positive in men (r= 0.10, p < 0.01) and women (0.18, p < 0.01). Correlations between overall sitting and both exercise and non-exercise activity were weakly negative (r= −0.03 to −0.10, all p < 0.01).
Figure 1.
Duration (hrs/d) of overall physical activity (Panel A) and sitting time (Panel B), by type of behavior and sex, the NIH-AARP Diet and Health Study
Values are mean and SD, and % total activity reported
More sitting time was associated with a graded increase in risk for all-cause mortality (Table 2). Compared to men reporting < 5 hrs/d of sitting, adjusted hazard ratios (95% CI) for all-cause mortality in men reporting 5–6.9, 7–8.9, 9–11.9 and ≥ 12 hrs/d of sitting were 1.05 (0.98, 1.11), 1.10 (1.03,1.18), 1.19 (1.09, 1.29), and 1.21 (1.11, 1.31), respectively. For women, the hazard ratios (95% CI) for overall sitting were 1.10 (1.01, 1.19), 1.09 (1.00, 1.19), 1.25 (1.14, 1.38), and 1.40 (1.27, 1.54). There was no statistical interaction between sitting time and sex on mortality (P interaction = 0.59).
Table 2.
Association between overall sitting time (hrs/d) and cause-specific mortality, by sex, the NIH-AARP Diet and Health Study
| MEN | WOMEN | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||||
| Deaths (n) | HR | (95% CI) | HR | (95% CI) | Deaths (n) | HR | (95% CI) | HR | (95% CI) | |
| All-causes | ||||||||||
| < 5 | 1,756 | 1.00 | - | 1.00 | - | 1,081 | 1.00 | - | 1.00 | - |
| 5 to 6.9 | 2,191 | 1.05 | (0.98, 1.11) | 1.05 | (0.98, 1.11) | 1,423 | 1.11 | (1.02, 1.20) | 1.10 | (1.01, 1.19) |
| 7 to 8.9 | 1,532 | 1.11 | (1.03, 1.19) | 1.10 | (1.03, 1.18) | 1,010 | 1.11 | (1.02, 1.21) | 1.09 | (1.00, 1.19) |
| 9 to 11.9 | 896 | 1.21 | (1.11, 1.31) | 1.19 | (1.09, 1.29) | 701 | 1.29 | (1.17, 1.42) | 1.25 | (1.14, 1.38) |
| ≥ 12 | 843 | 1.23 | (1.13, 1.33) | 1.21 | (1.11, 1.31) | 768 | 1.43 | (1.30, 1.57) | 1.40 | (1.27, 1.54) |
| Ptrend | < 0.01 | < 0.01 | < 0.01 | < 0.01 | ||||||
| Cardiovascular | ||||||||||
| < 5 | 457 | 1.00 | - | 1.00 | - | 269 | 1.00 | - | 1.00 | - |
| 5 to 6.9 | 623 | 1.13 | (1.00, 1.28) | 1.13 | (1.00, 1.27) | 367 | 1.12 | (0.96, 1.32) | 1.13 | (0.97, 1.33) |
| 7 to 8.9 | 430 | 1.18 | (1.03, 1.35) | 1.17 | (1.02, 1.34) | 246 | 1.06 | (0.89, 1.26) | 1.05 | (0.88, 1.25) |
| 9 to 11.9 | 267 | 1.36 | (1.16, 1.58) | 1.32 | (1.14, 1.54) | 202 | 1.44 | (1.19, 1.73) | 1.40 | (1.17, 1.69) |
| ≥ 12 | 257 | 1.42 | (1.21, 1.66) | 1.40 | (1.20, 1.63) | 221 | 1.59 | (1.33, 1.91) | 1.55 | (1.29, 1.86) |
| Ptrend | < 0.01 | < 0.01 | < 0.01 | < 0.01 | ||||||
| Cancer | ||||||||||
| < 5 | 691 | 1.00 | - | 1.00 | - | 448 | 1.00 | - | 1.00 | - |
| 5 to 6.9 | 833 | 1.01 | (0.92, 1.12) | 1.01 | (0.92, 1.12) | 549 | 1.05 | (0.93, 1.19) | 1.03 | (0.91, 1.17) |
| 7 to 8.9 | 554 | 1.03 | (0.92, 1.16) | 1.03 | (0.92, 1.15) | 371 | 1.01 | (0.88, 1.17) | 1.00 | (0.87, 1.14) |
| 9 to 11.9 | 332 | 1.16 | (1.02, 1.33) | 1.15 | (1.01, 1.32) | 230 | 1.06 | (0.90, 1.25) | 1.04 | (0.88, 1.22) |
| ≥ 12 | 270 | 1.03 | (0.89, 1.19) | 1.02 | (0.88, 1.17) | 229 | 1.08 | (0.91, 1.27) | 1.06 | (0.90, 1.25) |
| Ptrend | 0.24 | 0.32 | 0.42 | 0.57 | ||||||
| Other causes | ||||||||||
| < 5 | 608 | 1.00 | - | 1.00 | - | 364 | 1.00 | - | 1.00 | - |
| 5 to 6.9 | 735 | 1.01 | (0.91, 1.13) | 1.02 | (0.92, 1.14) | 507 | 1.17 | (1.02, 1.34) | 1.16 | (1.01, 1.33) |
| 7 to 8.9 | 548 | 1.14 | (1.01, 1.28) | 1.14 | (1.01, 1.28) | 393 | 1.28 | (1.11, 1.48) | 1.25 | (1.08, 1.44) |
| 9 to 11.9 | 297 | 1.14 | (1.00, 1.32) | 1.12 | (0.97, 1.29) | 269 | 1.46 | (1.24, 1.71) | 1.41 | (1.20, 1.65) |
| ≥ 12 | 316 | 1.31 | (1.14, 1.50) | 1.27 | (1.11, 1.46) | 318 | 1.74 | (1.49, 2.03) | 1.70 | (1.45, 1.99) |
| Ptrend | < 0.01 | < 0.01 | < 0.01 | < 0.01 | ||||||
Model 1: adjusted for Age (years), Education (< 12 yrs, high school graduate, some college, college graduate, unknown), Smoking history (never, stopped 10+, 5–9, 1–4 years ago, stopped < 1 year, current smoker, unknown), Sleep duration (< 4, 4, 5.9, 6, 7.9, 8, 9.9, 10+ hours/day, unknown), Overall health (excellent, very good, good, fair, poor, unknown), and Body Mass Index (< 25, 25, 29.9, 30+ kg/m2, unknown)
Model 2: additionally adjusted for Overall physical activity (< 1, 1–1.9, 2–2.9, 3–3.9, 4+ hrs/d)
Associations for sitting were stronger for cardiovascular mortality, and other causes, but results were null for cancer mortality.
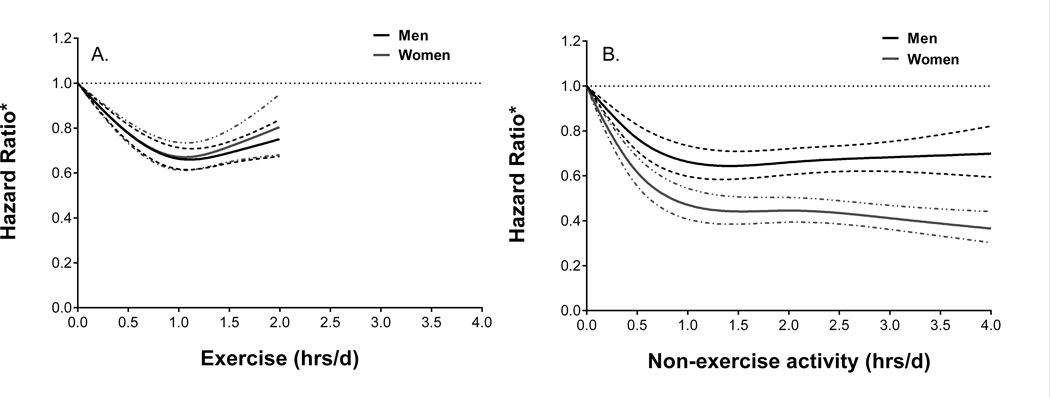
Greater amounts of both exercise and non-exercise activity were independently associated with lower all-cause mortality after adjusting for covariates, sitting time, and the other type of activity (Figure 2).
Figure 2.
Association* between all-cause mortality and exercise and non-exercise activity estimated by restricted cubic splines, by sex, the NIH-AARP Diet and Health Study
*Values are Hazard Ratios and 95% Confidence Intervals adjusted for Age (years), Education (< 12 yrs, high school graduate, some college, college graduate, unknown), Smoking history (never, stopped 10+, stopped 5–9, stopped 1–4 years, stopped < 1 year, current smoker, unknown), Sleep duration (< 4, 4–5.9, 6–7.9, 8–9.9, 10+ hours/day, unknown), Overall health (excellent, very good, good, fair, poor, unknown), and Body Mass Index (< 25, 25–29.9, 30+ kg/m2, unknown), Overall sitting (hrs/d), and the other type of physical activity. To fit the splines knots were placed at intervals of 0.5 to 1 hrs/d increments over the range of each exposure and data were trimmed at approximately the 95th percentile of each exposure distribution.
Exercise activities include: walking for exercise; jogging or running; racquet sports; playing golf; swimming laps; bicycling or stationary bike; other aerobic exercise; weight training or lifting
Non-exercise activities include: light household chores; moderate-vigorous indoor household chores; moderate outdoor chores; vigorous outdoor chores; home repairs; caring for children, caring for adults, walking for daily activities
Mortality was 20 to 30% lower for men and women reporting 1 to 2 hours/day of exercise (Figure 2, Panel A). One to 2 hours/day of non-exercise activity was associated with 30% reduction in mortality in men, and 50–60% reduction in women (Figure 2, Panel B). The statistical interaction between physical activity and sex on mortality was non-significant for exercise (P interaction = 0.90), but was significant for non-exercise activities (P interaction < 0.0001).
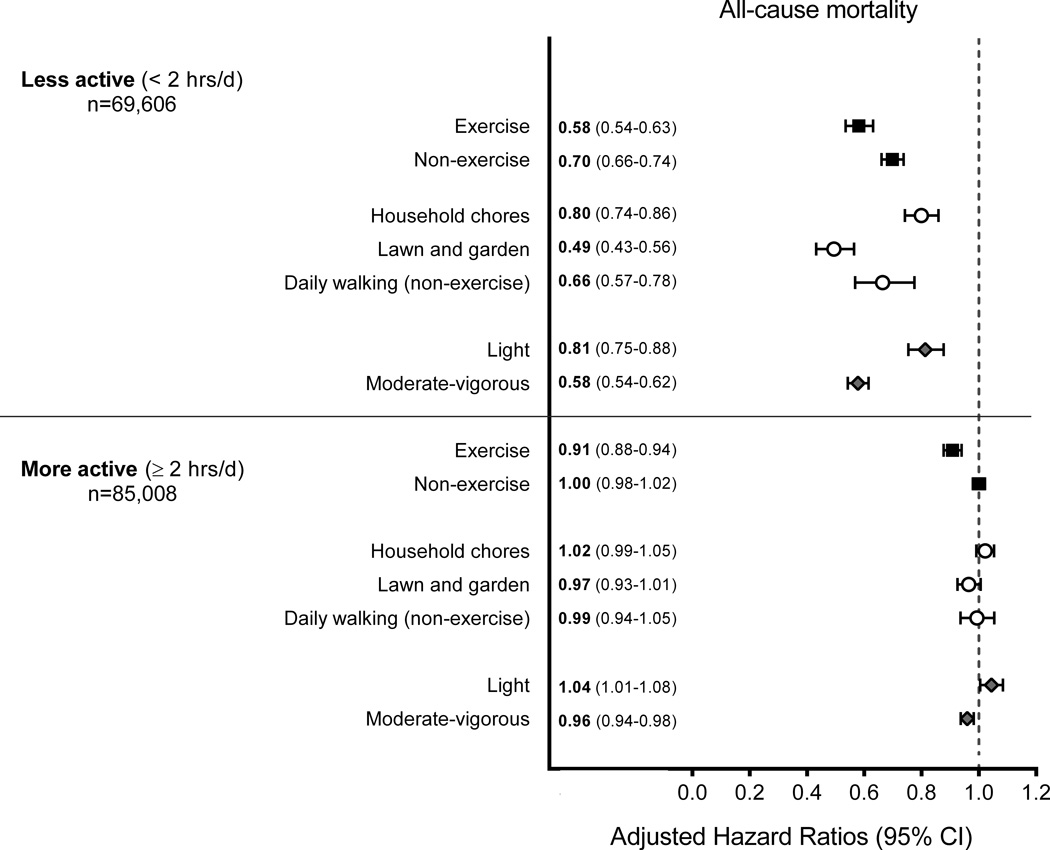
Next, we fit isotemporal models to estimate the mortality benefits associated with replacing sitting time with an equal amount of different types of physical activity, in less active (<2 hrs/d overall activity) and more active participants (≥ 2 hrs/d). For less active participants, replacing one hour of sitting with an equal amount of time in physical activity was associated with lower all-cause mortality for both exercise (HR=0.58 [0.54,0.63]) and non-exercise activities (HR=0.70 [0.66,0.74]) (Figure 3). Significant protective replacement associations were also noted for specific non-exercise activities (i.e., household chores, lawn and garden, daily walking), as well as both light and moderate-vigorous intensity activities. Stronger associations were observed for replacement of sitting time with higher intensity activities (e.g., Exercise HR=0.58 [0.54–0.63] vs. Household chores HR=0.80 [0.74–0.86]). In contrast, among more active participants replacement of sitting time with purposeful exercise was associated with lower mortality (HR=0.91 [0.88–0.94]), but replacement of sitting with non-exercise activity was not (HR=1.00 [0.98–1.02]). Results for cardiovascular mortality were broadly consistent with those for all-cause mortality (see Figure, SDC 5: Supplemental Figure 3. Estimated risk for cardiovascular mortality associated with replacement of one hour of overall sitting with an equal amount of time in specific types and intensities of physical activity).
Figure 3.
Estimated risk* for all-cause mortality associated with replacement of one hour of overall sitting with an equal amount of time in specific types and intensities of physical activity, in less and more active participants, the NIH-AARP Diet and Health Study.
*Values are Hazard Ratios and 95% Confidence Intervals adjusted for Age (years), Education (< 12 yrs, high school graduate, some college, college graduate, unknown), Smoking history (never, stopped 10+, stopped 5–9, stopped 1–4 years, stopped < 1 year, current smoker, unknown), Sleep duration (< 4, 4–5.9, 6–7.9, 8–9.9, 10+ hours/day, unknown), Overall health (excellent, very good, good, fair, poor, unknown), and Body Mass Index (< 25, 25–29.9, 30+ kg/m2, unknown), and Overall sitting (hrs/d) each type of Physical Activity (hrs/d), and the sum of Overall Sitting and Physical Activity time (hrs/d)
Exercise activities include: walking for exercise; jogging or running; racquet sports; playing golf; swimming laps; bicycling or stationary bike; other aerobic exercise; weight training or lifting
Non-exercise activities include: light household chores; moderate-vigorous indoor household chores; moderate outdoor chores; vigorous outdoor chores; home repairs; caring for children, caring for adults, walking for daily activities
Household chores include: light household chores; moderate-vigorous indoor household chores; home repairs; caring for children, caring for adults
Lawn and garden activities include: moderate outdoor chores; vigorous outdoor chores
Daily walking (non-exercise) includes: walking for daily activities
Light activities include: light household chores; walking for daily activities
Moderate-vigorous activities include: walking for exercise; jogging or running; racquet sports; playing golf; swimming laps; bicycling or stationary bike; other aerobic exercise; weight training or lifting; moderate-vigorous indoor household chores; moderate outdoor chores; vigorous outdoor chores; home repairs; caring for children, caring for adults
In detailed analysis by sex, the replacement benefits for exercise and non-exercise activities were consistently observed in less active men and women. In more active men and women, lower mortality was only observed when exercise replaced sitting time (see tables, SDC 6: Supplemental Table 1A. Partition and isotemporal substitution models for all-cause mortality in less active participants; Supplemental Table 1B. Partition and isotemporal substitution models for all-cause mortality in more active participants). However, there was some variation by sex in results for the individual non-exercise activities. The replacement associations for cardiovascular mortality were weaker and non-significant among less active men for household chores, daily walking, and light intensity activity compared to women (see Table, SDC 7 Supplemental Table 2A. Partition and isotemporal substitution models for cardiovascular mortality in less active participants). We also found an unexpected increase in risk associated with replacing sitting time with household and light intensity activity in more active men (e.g., SDC 7 Supplemental Table 2B. Partition and isotemporal substitution models for cardiovascular mortality in more active participants). In contrast, there was a significant inverse association for replacing sitting time with lawn and garden activities in more active men, but not among women (SDC 7 Supplemental Table 2B. Partition and isotemporal substitution models for cardiovascular mortality in more active participants).
Sensitivity analyses excluding participants with fewer than two years of follow-up did not materially alter our primary results (see Tables, SDC 8 Supplemental Table 3. Cause-specific mortality and sedentary behavior after excluding short follow-up; Table 4. Partition and isotemporal substitution models for mortality in less and more active participants, excluding those with < 2 years of follow-up).
DISCUSSION
In this prospective study of older adults free of major medical conditions, greater overall sitting time (≥ 12 vs. < 5 hrs/d) was associated with a graded increase in risk of 20–40% for death from all-causes and 40–55% greater risk for cardiovascular mortality. Among less active adults, replacement of one hour per day of sitting with an equal amount of either exercise or non-exercise activity was associated with lower mortality. Inactive adults may get substantial mortality benefits from reducing couch-time by an hour each day in favor of engaging in purposeful exercise, or a broad range of activities of everyday living, such as lawn and garden activities, daily walking apart from exercise, and household chores. In contrast, for adults who accumulate more overall physical activity—two-thirds of which was derived from non-exercise sources in this study—our results indicate that replacing sitting time with more non-exercise activity does not confer additional protection. Purposeful exercise is needed to reduce risk for mortality further in more active adults. This investigation again highlights the mortality risks associated with prolonged sitting and for the first time identifies specific types of physical activity as healthful alternatives to sitting. Collectively, our study provides strong support for the public health recommendation to “avoid inactivity” in favor of more physical activity(26). Future studies are needed to confirm our findings and to refine our understanding of the most healthful balance between spending time in sedentary and physically active pursuits.
Only about 30% of older adults (65+ years) in the United States report engaging in enough aerobic activity to meet the 2008 Physical Activity Guidelines(21), and many spend 9–10 hours/d or more in sedentary behavior(15). For these individuals, reducing sitting by one hour is about a 10% reduction in total sitting time. Time-use studies of older adults suggest that most sedentary behaviors are potentially modifiable leisure-time pursuits (e.g., television, socializing, relaxing, reading, hobbies)(12), and mortality has been noted to be elevated by 10 to 50% for those reporting the most overall sitting(16, 31) and by 40–60% among those watching the most television(6, 16, 33). Therefore, intervention strategies that target reductions in time spent in leisure-time sedentary behavior could improve health and longevity if these deleterious behaviors were replaced with physical activity. However, it has not been clear whether reducing sitting time is associated with lower mortality, and aside from purposeful exercise (26), what other types of activity could be recommended as a healthful alternative to sitting. The isotemporal modeling approach can provide insight and recent studies have reported replacement of television viewing with brisk walking to be associated with reduced risk of depression (18), and replacement of accelerometer measured sedentary time with light intensity or moderate-vigorous intensity activity to be favorably associated with cardiometabolic biomarkers (2). Our findings complement and extend these reports by estimating for the first time the mortality benefits associated with replacing sitting time with specific types of physical activity.
Our findings for physical activity are consistent with research demonstrating the mortality benefits associated with exercise and/or leisure-time activity (e.g.,(9, 14, 20)), non-exercise activities overall(17, 32), and individual non-exercise pursuits, such walking(7), housework(1, 17), and do-it-yourself activities(29), but these studies did not consider the inter-play between sedentary time and physical activity. A key finding in our study was that, in more active adults, replacement of sitting time with purposeful exercise conferred additional mortality protection, whereas replacing sitting with non-exercise activities did not. This result is consistent with the hypothesis that decreasing sitting time in more active and fit individuals will be associated with smaller reductions in risk(8, 27) and indicates that at some amount of overall physical activity the risks associated with too much sitting can be eliminated. Cognizant that our results are specific to our study population and the physical activity questionnaire employed, we urge caution when translating our definition of “less” and “more active” adults to other studies. The actual threshold remains unknown but identifying the amount, types, and patterns of physical activity required to minimize risk associated with prolonged sitting should be a research priority.
The limitations of our study should be considered carefully. We relied on self-reported information and measurement error undoubtedly introduced misclassification and probably attenuated of the strength of associations. The few studies that have employed objective measures report stronger associations for these exposures (11, 13). It should be noted that results from this study are applicable to older adults in good health entering their seventh decade, and our findings could differ for younger and less healthy older adults. Future research should evaluate the possible mortality benefits associated with replacing sedentary time for physical activity in adults with pre-existing conditions, such as heart disease or a previous cancer diagnosis. More frequent bouts of activity that break up sedentary time have been associated with better metabolic health(5) and a recent study has suggested that reducing sitting time may enhance the beneficial metabolic effects of exercise (10). It is possible that the somewhat stronger associations we observed in women may be associated with both the greater amount of non-exercise they accumulated, as well as the manner in which they accumulated the activity. Higher levels of non-exercise activity also may be linked to a greater frequency of activity participation (days/week) and more frequent movement throughout the day. However, our assessment of physical activity did not assess activity frequency, it only assessed a small number of light intensity activities, and we did not have a measure of cardiorespiratory fitness in the study. These factors limited our ability to investigate the impact of activity frequency (e.g., time/week, bouts/day), many lower intensity non-exercise activities, or effects associated with the relative intensity of activity. Future prospective studies of mortality or incident disease end-points that utilize better and more comprehensive measures of the overall amount, specific types, and patterns of behavior in older adults are needed to elucidate these etiologic questions (4).
The isotemporal modeling approach we employed also merits comment. First, the mortality associations reported herein only reflect substitution effects between sitting and activity derived from the statistical models rather than the association for actual changes in these behaviors. Second, because the number of hours in a day is finite, any model evaluating the relation between sleep, sitting, and activity is a defacto substitution model. Any time component not explicitly included in the model can add a substitution effect to the exposure of interest. We chose to treat sleep time as a confounding factor in our models and evaluated the isotemporal associations only for the universe of sitting and activity behaviors measured in this study. However, we have recently noted that the associations between time spent sleeping, sitting, and in moderate-vigorous activity and mortality appear to be independent from one another (35). Future research should consider incorporating sleep time into the mix when investigating the health effects of time-use trade-offs (e.g., (2)). Third, risk estimates derived from the models are isotemporal, but not isocaloric. The stronger associations we observed for replacing sitting time with higher intensity activities may be due to the larger energy expenditure (per hour) for more intense activities, rather than an intensity-specific effect per se. Fourth, implementation of these models required that we select an increment of time for which the substitution associations could be estimated. We chose a one hr/d increment as a pragmatic yet plausible choice for a target reduction in daily sedentary time (equivalent to a 10% reduction for someone who sits for 10 hrs/d). This amount of change in sedentary time is consistent with reductions observed in recent intervention trials (28). Other isotemporal substitution studies have used a 30 min/d time increment (2, 18, 19). Our choice of time increment in no way affects the statistical significance of our results, but the strength of the associations will be affected. The strength of the mortality benefits we report for a one hr/d reduction in sitting time would be about half as strong if we used a 30 min/d increment and about twice as strong if we used a 2 hr/d time increment. It’s possible that replacing one hour of sitting with an hour of exercise is not always possible, but taken together our results implicitly suggest that replacing an hour of sitting with any of the activities we evaluated, individually or in combination, could provide mortality benefit for inactive adults. There is a great need to develop interventions that effectively reduce sitting time and increase physical activity (24, 28) and future behavioral studies should seek to identify the optimal activity preferences for those interested in reducing sitting time.
Time spent in sedentary behavior has increased by 43% in the last 40 years in this country (22) and older adults routinely spend the majority of their day in sedentary pursuits, mostly in leisure-time. These changes have undoubtedly had a profound effect on the amount of physical activity that adults accumulate each day. To date, public health strategies for physical activity have not explicitly targeted a reduction in sedentary behaviors in the effort to increase overall amounts of physical activity in the population, in part because it was unclear if reducing sitting time would confer benefit and—apart from purposeful exercise—what activities could be recommended as healthful alternatives to sitting. Our results add to the increasingly strong and consistent evidence demonstrating the deleterious influence of sedentary behavior on mortality and indicate that replacing sitting time by one hour per day with either purposeful exercise or a broad range of activities of everyday living is associated with greater longevity, particularly among less active adults.
Supplementary Material
Acknowledgments
The publication of this study in no way constitutes an endorsement of the results by the American College of Sports Medicine.
Funding. This research was supported in part by the Intramural Research Program of the United States National Institutes of Health, National Cancer Institute.
Footnotes
Conflict of Interest/Financial Disclosure: None reported
Scientific Contributions: Dr. Matthews had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Matthews, Moore. Acquisition of data: Hollenbeck, Park. Analysis and interpretation of data: Matthews, Moore, Xiao, Blair, Keadle, Sampson. Drafting of the manuscript: Matthews, Moore, Xiao, Blair, Keadle, Park, Sampson. Critical revision of the manuscript for important intellectual content: Matthews, Moore, Sampson, Blair, Xiao, Keadle, Hollenbeck, Park. Statistical analysis: Matthews, Sampson, Moore. Obtained funding: Matthews. Administrative, technical, and material support: Park, Hollenbeck, and Matthews. Study supervision: Park, Matthews.
Additional Contributions: We are indebted to the participants in the NIH-AARP Diet and Health Study for their outstanding cooperation.
Supplementary Digital Content (SDC) Listing
SDC 1: Methods for Development of the Analytic Study Sample
SDC 2: Assessment of Physical Activity and Sedentary Behaviors
SDC 3 Supplemental Figure 1. Association between all-cause mortality and overall physical activity (sum of exercise and non-exercise activity) estimated by restricted cubic splines, by sex, the NIH-AARP Diet and Health Study
SDC 4 Supplemental Figure 2. Physical activity energy expenditure (MET-hrs/d) in less and more active participants, by sex, the NIH-AARP Diet and Health Study
SDC 5 Supplemental Figure 3. Estimated risk for cardiovascular mortality associated with replacement of one hour of overall sitting with an equal amount of time in specific types and intensities of physical activity, in less and more active participants, the NIH-AARP Diet and Health Study.
SDC 6 Supplemental Table 1A. Partition and isotemporal substitution models for all-cause mortality in less active participants, overall and by sex - the NIH-AARP Diet & Health Study; Supplemental Table 1B. Partition and isotemporal substitution models for all-cause mortality in more active participants, overall and by sex - the NIH-AARP Diet & Health Study
SDC 7 Supplemental Table 2A. Partition and isotemporal substitution models for cardiovascular mortality in less active participants, overall and by sex - the NIH-AARP Diet & Health Study; Supplemental Table 2B. Partition and isotemporal substitution models for cardiovascular mortality in more active participants, overall and by sex - the NIH-AARP Diet & Health Study
SDC 8 Supplemental Table 3. Cause-specific mortality and sedentary behavior after excluding short follow-up (< 2 person-yrs), by sex - the NIH Diet & Health Study Table 4. Partition and isotemporal substitution models for mortality in less and more active participants, excluding those with < 2 years of follow-up - the NIH-AARP Diet & Health Study
References
- 1.Besson H, Ekelund U, Brage S, et al. Relationship between subdomains of total physical activity and mortality. Medicine and Science in Sports and Exercise. 2008;40(11):1909–1915. doi: 10.1249/MSS.0b013e318180bcad. [DOI] [PubMed] [Google Scholar]
- 2.Buman MP, Winkler EAH, Kurka JM, et al. Reallocating Time to Sleep, Sedentary Behaviors, or Active Behaviors: Associations With Cardiovascular Disease Risk Biomarkers, NHANES 2005–2006. American Journal of Epidemiology. 2013;179(3):323–334. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- 3.Chasan-Taber S, Rimm EB, Stampfer MJ, et al. Reproducibility and Validity of a Self-Administered Physical Activity Questionnaire for Male Health Professionals. Epidemiology. 1996;7(1):81–86. doi: 10.1097/00001648-199601000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Colbert LH, Matthews CE, Havighurst TC, et al. Comparative validity of physical activity measures in older adults. Med Sci Sports Exerc. 2011;43(5):867–876. doi: 10.1249/MSS.0b013e3181fc7162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunstan DW, Kingwell BA, Larsen R, et al. Breaking Up Prolonged Sitting Reduces Postprandial Glucose and Insulin Responses. Diabetes Care. 2012;35(5):976–983. doi: 10.2337/dc11-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunstan DW, Salmon J, Healy GN, et al. Association of Television Viewing With Fasting and 2-h Postchallenge Plasma Glucose Levels in Adults Without Diagnosed Diabetes. Diabetes Care. 2007;30(3):516–522. doi: 10.2337/dc06-1996. [DOI] [PubMed] [Google Scholar]
- 7.Hamer M, Chida Y. Walking and primary prevention: a meta-analysis of prospective cohort studies. British Journal of Sports Medicine. 2008;42(4):238–243. doi: 10.1136/bjsm.2007.039974. [DOI] [PubMed] [Google Scholar]
- 8.Hamilton MT, Hamilton DG, Zderic TW, et al. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. [Review] [88 refs] Diabetes. 2007;56(11):2655–2667. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- 9.Hu FB, Willett WC, Li T, et al. Adiposity as compared with physical activity in predicting mortality among women. New England Journal of Medicine. 2004;351(26):2694–2703. doi: 10.1056/NEJMoa042135. [DOI] [PubMed] [Google Scholar]
- 10.Keadle S, Lyden K, Staudenmayer J, et al. The independent and combined effects of exercise training and reducing sedentary behavior on cardiometabolic risk factors. Applied Physiology, Nutrition, and Metabolism. 2014;39(7):770–780. doi: 10.1139/apnm-2013-0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koster A, Caserotti P, Patel KV, et al. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS One. 2012;7(6):e37696. doi: 10.1371/journal.pone.0037696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krantz-Kent R, Stewart J. How do older Americans spend their time? Monthly Labor Review. 2007;130(5):8–26. [Google Scholar]
- 13.Manini TM, Everhart JE, Patel KV, et al. Daily Activity Energy Expenditure and Mortality Among Older Adults. JAMA: The Journal of the American Medical Association. 2006;296(2):171–179. doi: 10.1001/jama.296.2.171. [DOI] [PubMed] [Google Scholar]
- 14.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. New England Journal of Medicine. 2002;347(10):716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 15.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95(2):437–445. doi: 10.3945/ajcn.111.019620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matthews CE, Jurj AL, Shu XO, et al. Influence of exercise, walking, cycling, and overall nonexercise physical activity on mortality in Chinese women. Am J Epidemiol. 2007;165(12):1343–1350. doi: 10.1093/aje/kwm088. [DOI] [PubMed] [Google Scholar]
- 18.Mekary RA, Lucas M, Pan A, et al. Isotemporal Substitution Analysis for Physical Activity, Television Watching, and Risk of Depression. American Journal of Epidemiology. 2013;178(3):474–483. doi: 10.1093/aje/kws590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mekary RA, Willett WC, Hu FB, et al. Isotemporal Substitution Paradigm for Physical Activity Epidemiology and Weight Change. American Journal of Epidemiology. 2009;170(4):519–527. doi: 10.1093/aje/kwp163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore SC, Patel AV, Matthews CE, et al. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med. 2012;9(11):e1001335. doi: 10.1371/journal.pmed.1001335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Center for Health Statistics. Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD: 2013. [PubMed] [Google Scholar]
- 22.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obesity Reviews. 2012;13(8):659–680. doi: 10.1111/j.1467-789X.2011.00982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Owen N, Sparling PB, Healy GN, et al. Sedentary behavior: emerging evidence for a new health risk. Mayo Clinic proceedings Mayo Clinic. 2010;85(12):1138–1141. doi: 10.4065/mcp.2010.0444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Owen N, Sugiyama T, Eakin EE, et al. Adults' Sedentary Behavior: Determinants and Interventions. American Journal of Preventive Medicine. 2011;41(2):189–196. doi: 10.1016/j.amepre.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 25.Patel AV, Bernstein L, Deka A, et al. Leisure Time Spent Sitting in Relation to Total Mortality in a Prospective Cohort of US Adults. American Journal of Epidemiology. 2010;172(4):419–429. doi: 10.1093/aje/kwq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report. Washington, DC: US Department of Health and Human Services; 2008. pp. A1–A10. [DOI] [PubMed] [Google Scholar]
- 27.Powell KE, Paluch AE, Blair SN. Physical Activity for Health: What Kind? How Much? How Intense? On Top of What? Annual Review of Public Health. 2011;32(1):349–365. doi: 10.1146/annurev-publhealth-031210-101151. [DOI] [PubMed] [Google Scholar]
- 28.Prince SA, Saunders TJ, Gresty K, et al. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta-analysis of controlled trials. Obesity Reviews. 2014;15(11):905–919. doi: 10.1111/obr.12215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sabia S, Dugravot A, Kivimaki M, et al. Effect of Intensity and Type of Physical Activity on Mortality: Results From the Whitehall II Cohort Study. American Journal of Public Health. 2011;102(4):698–704. doi: 10.2105/AJPH.2011.300257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schatzkin A, Subar AF, Thompson FE, et al. Design and Serendipity in Establishing a Large Cohort with Wide Dietary Intake Distributions : The National Institutes of Health-American Association of Retired Persons Diet and Health Study. American Journal of Epidemiology. 2001;154(12):1119–1125. doi: 10.1093/aje/154.12.1119. [DOI] [PubMed] [Google Scholar]
- 31.van der Ploeg HP, Chey T, Korda RJ, et al. Sitting time and all-cause mortality risk in 222,497 australian adults. Archives of Internal Medicine. 2012;172(6):494–500. doi: 10.1001/archinternmed.2011.2174. [DOI] [PubMed] [Google Scholar]
- 32.Weller I, Corey P. The impact of excluding non-leisure energy expenditure on the relation between physical activity and mortality in women. Epidemiology. 1998;9(6):632–635. [PubMed] [Google Scholar]
- 33.Wijndaele K, Brage S, Besson H, et al. Television viewing time independently predicts all-cause and cardiovascular mortality: the EPIC Norfolk Study. International Journal of Epidemiology. 2010;40(1):150–159. doi: 10.1093/ije/dyq105. [DOI] [PubMed] [Google Scholar]
- 34.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. International Journal of Epidemiology. 1994;23(5):991–999. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 35.Xiao Q, Keadle SK, Hollenbeck AR, et al. Sleep Duration and Total and Cause-Specific Mortality in a Large US Cohort: Interrelationships With Physical Activity, Sedentary Behavior, and Body Mass Index. American Journal of Epidemiology. 2014;180(10):997–1006. doi: 10.1093/aje/kwu222. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.