Abstract
Objective
Alcohol-impaired driving persists as a major cause of traffic fatalities and injuries among young drivers. This meta-analysis examined whether brief alcohol interventions were effective in reducing driving after drinking among adolescents and young adults.
Method
Our systematic search identified 12 experimental/quasi-experimental evaluations (16 intervention groups) that measured driving while intoxicated and related consequences and provided data for effect size calculation (N = 5,664; M age =17 years; 57% male). The studies were published between 1991 and 2011. Three-level random-effects meta-analyses using a structural equation modeling approach were used to summarize the effects of the interventions.
Results
Compared with controls, participants in brief alcohol interventions reported reduced drinking and driving and related consequences (ḡ = 0.15, 95% CI [0.08, 0.21]). Supplemental analyses indicated that reductions in driving while intoxicated were positively associated with the reduced post-intervention heavy use of alcohol. These findings were not attenuated by study design or implementation factors.
Conclusions
Brief alcohol interventions under 5 hours of contact may constitute a promising preventive approach targeting drinking and driving among adolescents and young adults. Reducing heavy episodic alcohol consumption appeared to be a major factor in reducing drunk-driving instances. Interpretation of the findings must be made with caution, however, given the possibility of publication bias and the small observed effect size. Future research should focus on the exact mechanisms of behavior change leading to beneficial outcomes of brief alcohol interventions and the potential effectiveness of combined brief interventions and other preventive approaches.
Keywords: Adolescents, Brief alcohol intervention, Driving after drinking/DWI, Heavy episodic drinking, Meta-analysis, Underage drinkers, Young adults
Introduction
Alcohol-impaired driving remains a serious public health problem despite extensive prevention and intervention efforts aiming to reduce drunk driving. Young drivers are of particular concern given their high crash risk, susceptibility to alcohol’s impairing effects, driving inexperience, greater sensation seeking and impulsivity, and limited planning capacities [1–4]. Unfortunately, drinking and driving continues to be wide spread among high school and college-aged youth [5,6]. National estimates, for instance, indicate that U.S. high school students drive after drinking about 2.4 million times a month; with nearly one in ten having done so at least once in the prior month [5].
Driving while intoxicated (DWI) is a major cause of U.S. traffic fatalities and injuries [7]. Those who drive after drinking tend to be involved in more serious crashes and sustain greater injury severities than those who drive sober [3]. For example, drivers under 21 years old are 17 times more likely to die in a crash when they have a blood alcohol concentration of 0.08% or higher than when they have not been drinking [5]. Furthermore, motor vehicle crashes are the leading cause of mortality for U.S. adolescents [8] and over 20% of drivers aged 15 to 20 involved in fatal motor vehicle crashes in 2010 were drinking prior to the crash [9].
Most drinking drivers are not diagnosed with an alcohol use disorder, but rather are simply engaging in periodic alcohol consumption, sometimes at excessive levels [1,10]. Heavy episodic drinking (defined here as consuming four or more alcoholic drinks on one or more occasions for women and five or more drinks on one or more occasions for men) is one risk factor for motor vehicle crashes and other related negative consequences [1]. Heavy episodic drinking is common among adolescents [5,11], and most (81%) teen drivers involved in lethal road traffic crashes have blood alcohol concentrations (BACs) at high levels indicative of heavy episodic drinking [5].
Prevention and Intervention
Prevention and intervention strategies used to address drinking and driving vary by punitive level and the drivers they target [1]. Universal DWI prevention approaches target the general population prior to the occurrence of a DWI event. These might include, for example, alternate transportation and designated driver programs, educational training for servers of alcoholic beverages, BAC level laws, or other laws targeting young drivers and their access to alcohol [1,12]. Selective and indicated DWI prevention approaches target drivers deemed at high risk for drunk driving and may involve license revocation or suspension, fines, probation, vehicle immobilization or tagging, or alcohol screening and brief intervention programs [1,13].
Brief alcohol interventions (BAIs) may be particularly well suited for DWI prevention among young drivers, who can be easily identified and recruited via school and university settings. Brief interventions refer to a broad family of interventions that can vary in length, structure, delivery personnel, underpinning theory, and philosophy [14]. The defining feature is the short duration of the intervention, which typically entails between one and five sessions with only a few hours in total duration. The therapeutic components in a BAI also vary, but typically include one or more of the following: assessment and feedback related to alcohol consumption; comparison of drinking habits with relevant norms (e.g., same gender, same age peers); goal-setting and contracting exercises; decisional balance exercises highlighting the pros and cons of drinking; discussion of drinking moderation strategies; and provision of information (e.g., how to calculate BAC or money spent on alcohol). These therapeutic components are often based on the principles of cognitive behavioral therapy, motivational enhancement therapy [15], and the trans-theoretical model of behavior change [16], which emphasize the importance of stimulating participants’ abilities, capacities, and motivations to self-evaluate and self-regulate behaviors. For instance, the intervention might highlight the perceived costs and benefits of alcohol consumption, provide opportunities to discuss options for moderating alcohol consumption, and provide personalized BAC charts based on participants’ height and weight.
Research on the effectiveness of selective and indicated DWI programs has largely focused on programs for convicted offenders and recidivists or interventions for those injured in road traffic crashes and treated in emergency rooms and trauma settings [13,17–19]. One meta-analysis that investigated the effects of remediation programs for DWI offenders on their subsequent recidivism, for instance, suggested that education and combined education/psychotherapy programs were associated with the largest beneficial effects, especially for the lowest risk group of offenders [20]. Another review of the research indicated that legal sanctions were effective in reducing DWI recidivism [13]. Other reviews have indicated that remedial or rehabilitation programs combined with licensing sanctions resulted in the greatest reduction in alcohol-related driving incidents [21]. A more recent review [22], however, found no evidence that punitive approaches to drinking and driving, such as suspension or revocation of a driver’s license, conviction or probation, were effective in reducing DWI recidivism. Although these prior literature reviews provide evidence that certain prevention efforts may reduce DWI, to date we are unaware of any prior reviews or meta-analyses that have focused specifically on BAIs as a selective intervention approach to reduce driving after drinking for adolescents and young adults.
Given the public safety and health risks, potentially lethal consequences of alcohol-impaired driving, and costs of prevention and treatment efforts, an important question is whether BAIs are effective in reducing DWI among adolescents and young adults. Research to date suggests that brief interventions are effective in reducing alcohol use among this population [23–26]. Thus, the objective of the current study is to examine whether BAIs targeting adolescents and young adults are also effective in reducing drinking and driving occurrences. We use meta-analytic methods to synthesize findings from primary studies identified in a systematic review of the literature and estimate the average effect of BAIs on DWI outcomes. We also explore whether effects on DWI outcomes are robust after controlling for study quality characteristics and examine whether post-intervention changes in heavy episodic drinking explain any effects on DWI outcomes.
Method
Study inclusion
This meta-analysis synthesizes findings from a subset of studies included in a larger systematic review on the effectiveness of BAIs for adolescents and young adults [26]. Studies eligible for the larger parent review met the following eligibility criteria: (1) evaluate a brief alcohol intervention designed to have beneficial effects on participants’ alcohol use or alcohol-related consequences; (2) have no more than five hours of total contact time and no more than four weeks in duration between the first and last session; (3) use a randomized or quasi-experimental research design that included a comparison condition of no treatment, wait-list control, or some form of treatment as usual; (4) focus on adolescents and young adults age 11–25, or on samples of undergraduate college students; (5) assess the effects on at least one alcohol use or alcohol-related problem outcome; (6) provide enough information to calculate post-intervention effect sizes indexing differences between groups on relevant outcomes; (7) be conducted in 1980 or later. There were no geographic or language restrictions on eligibility. To be eligible for inclusion in the current meta-analysis, studies had to additionally report a DWI-related outcome.
Literature search and coding procedures
We used a comprehensive search strategy to identify all published and unpublished studies that met the aforementioned inclusion criteria. The following electronic bibliographic databases were searched through December 31, 2012: CINAHL, Clinical Trials Register, Dissertation Abstracts International, ERIC, International Bibliography of the Social Sciences, NIH RePORTER, PsycARTICLES, PsycINFO, PubMed, Social Services Abstracts, Sociological Abstracts, and WorldWideScience.org. The full search strategy used in ProQuest is listed in the Appendix. We also conducted extensive grey literature searching, including websites, conference proceedings, hand searching of journals, and harvesting of references from bibliographies [26].
Under the supervision of the project’s principal investigator (this study’s second author), a team of six masters’s level research assistants first screened all abstracts/titles to eliminate clearly irrelevant reports. All six researchers initially screened 500 randomly selected abstracts/titles and discussed disagreements until 100% consensus was reached. The remaining abstracts/titles were screened by one researcher, with the principal investigator reviewing all their screening decisions as a second screener. Any disagreements were discussed until consensus was reached. If there was any ambiguity at the abstract/title phase, we retrieved the full text report for further review. Full text was retrieved for all reports that were not judged explicitly ineligible in the initial screening. The same team then used the same procedure to screen full text reports and make final eligibility decisions, with the principal investigator again reviewing all eligibility decisions and consensus used to resolve any disagreements [26].
Eligible studies were then coded on a range of variables related to study methods, intervention details, participant characteristics, statistical findings, and general study characteristics. Data extraction followed a standardized coding protocol, with data entered directly into a FileMaker Pro database. Coding was conducted by the same research team after several weeks of training led by the principal investigator. During training, five studies were coded by all coders, who then convened to resolve coding discrepancies until 100% consensus was attained on all coded variables. After the training period, coding questions were addressed in weekly meetings and decided via consensus with the group. In addition, the principal investigator reviewed all coding and resolved any further discrepancies via consensus with the initial coder.
The study participant characteristics of interest that were coded included age, percent in college, percent male, racial/ethnic composition of groups, and baseline alcohol consumption level. Intervention characteristics included: focal modality (cognitive behavioral skills training, cognitive behavioral + motivational enhancement, expectancy challenge, family focused therapy, feedback/information only, motivational interview, psycho-education, or other), format (self-administered, individual, group, or family), dosage (total duration, number of sessions, and number of days between first and last session), and DWI focus (1=intervention included DWI-related components). The following methodological characteristics were also extracted: study design (randomized controlled trial, controlled quasi-experiment), attrition (% from pretest to first follow-up), intention to treat (ITT) vs. treatment on the treated (TOT) analysis, inclusion of a CONSORT-style participant flow diagram, and timing of post-intervention follow-up.
Effect size calculation
The outcomes of interest in the meta-analysis were measured with standardized mean difference effect sizes, coded so that positive effect sizes represent better outcomes (e.g., lower frequency of DWI). Standardized mean difference effect sizes (d) were calculated as the difference in group means for the intervention and comparison groups after the end of the intervention divided by the pooled standard deviation for those groups. All standardized mean difference effect sizes were adjusted with the small-sample correction factor to provide unbiased estimates of effect size (g) [27]. For binary outcomes, the Cox transformation was used to convert log odds ratio effect sizes into standardized mean difference effect sizes [28]. We also inflated the standard errors of effect size estimates that originated from cluster-randomized trials when the authors did not properly account for the cluster design in their own analyses. Namely, we multiplied the standard error of the effect size by the square root of the design effect [29]. When cluster-randomized trials did not report the intraclass correlation coefficient (ICC), we used an ICC value of .13, which was the estimated average ICC for all alcohol consumption outcomes across all studies in the parent meta-analysis [26].
Data analysis
Analytic strategies
A number of studies included in the analyses reported multiple measures of DWI outcomes (e.g., frequency of driving after drinking, car accidents related to alcohol use, driving after 5 or more drinks), measured DWI outcomes at multiple follow-up points, or compared results of multiple brief intervention groups to a shared control group. As a result, the effect sizes available for synthesis were not statistically independent. To account for the within-study dependencies in the effect sizes, we used three-level meta-analyses using a structural equation modeling approach in all analyses where primary study participants (Level 1) provide multiple effect size estimates (Level 2), which were nested within studies (Level 3) [30–32]. This analytic approach permitted inclusion of statistically dependent effect sizes within any given meta-analysis without restrictions on the number of included studies or number of effect sizes per study [30,33]. All mean effect size and meta-regression models were run using the three-level meta-analyses and performed with the metaSEM package in the R statistical environment.
Sensitivity analysis and publication bias
Although our original intent was to examine whether any of the contextual variables moderated intervention effects, the homogeneity in effects ultimately precluded any complex moderator analyses. Therefore, we instead conducted a series of post-hoc sensitivity analyses to explore whether the overall mean effect size for DWI outcomes was robust after controlling for other potential confounding characteristics, such as intervention focus and implementation issues; outcome assessment timing; study design and quality indicators. Finally, we inspected contour-enhanced funnel plots [34,35] and conducted regression tests for funnel plot asymmetry to assess the possibility of publication bias [36].
Missing data
When primary studies failed to include enough statistical information needed to estimate effect sizes, we contacted primary study authors for that information. Most authors were responsive to our request and provided the needed information. For those studies where we were unable to obtain the requested data, we did not impute missing effect sizes. There was a small amount of missing data for participant demographic information (see Table 2) but we did not impute missing data for any of the variables.
Table 2.
Descriptive statistics for characteristics of studies included in the meta-analysis.
| %/M | k = 12/g= 16/n=30 | Range | |
|---|---|---|---|
| Report characteristics a | |||
| Publication year (Mdn) | 2008 | 12 | 1991 – 2011 |
| Journal article publication; % (n) | 83 | 12 | 0 – 1 |
| Country; % (n) | |||
| Australia | 8 | 12 | 0 – 1 |
| Brazil | 17 | 12 | 0 – 1 |
| United States | 75 | 12 | 0 – 1 |
| Research design and implementation | |||
| Randomized controlled trial; % (n)a | 83 | 12 | 0 – 1 |
| Attrition; % (n)b | 23 | 16 | 4 – 60 |
| Unit of assignment - individual; % (n)b | 81 | 16 | 0 – 1 |
| ITT analysis; % (n) a | 33 | 12 | 0 – 1 |
| CONSORT chart included; % (n) a | 42 | 12 | 0 – 1 |
| Post-intervention follow-up, in weeks; M (SD)c | 25 (17) | 30 | 4 – 52 |
| Sample characteristics (intervention groups) b | |||
| Average age; M (SD) | 17 | 13 | 13.5 – 20.5 |
| College students; % (n) | 59 | 16 | 0 – 1 |
| Male; % (n) | 57 | 15 | 41– 100 |
| White; % (n) | 70 | 11 | 62 – 80 |
| Black; % (n) | 8 | 11 | 2 – 15 |
| Hispanic; % (n) | 12 | 10 | 4 – 19 |
| Level of alcohol severity; % (n) | |||
| Abstainers | 13 | 16 | 0 – 1 |
| Low - experimenters | 13 | 16 | 0 – 1 |
| Medium - regular users | 38 | 16 | 0 – 1 |
| Hazardous users | 38 | 16 | 0 – 1 |
| Intervention characteristics b | |||
| DWI information included; % (n) | 63 | 16 | 0 – 1 |
| Intervention modality; % (n) | |||
| Cognitive behavioral therapy (CBT) | 13 | 16 | 0 – 1 |
| Motivational enhancement therapy (MET) | 44 | 16 | 0 – 1 |
| CBT + MET | 25 | 16 | 0 – 1 |
| Psycho - educational therapy | 13 | 16 | 0 – 1 |
| Feedback/information only | 6 | 16 | 0 – 1 |
| Intervention modal format; % (n) | |||
| Self-administered | 25 | 16 | 0 – 1 |
| Individual with provider | 44 | 16 | 0 – 1 |
| Group with provider | 31 | 16 | 0 – 1 |
| Intervention length; M (SD) | |||
| Duration (minutes) | 70 (73) | 16 | 2.5 – 240 |
| Days between first and last session | 6 (9) | 16 | 1 – 30 |
| Total number of sessions | 1.5 (.8) | 16 | 1 – 4 |
Notes. Means and standard deviations shown for continuous measures; percentages and counts shown for dichotomous measures. Percentages may not sum to 100 due to rounding error.
k: number of studies; g: number of intervention groups; n: number of effect sizes.
Estimates calculated at study level,
Estimates calculated at intervention group level,
Estimates calculated at effect size level
Results
Literature search
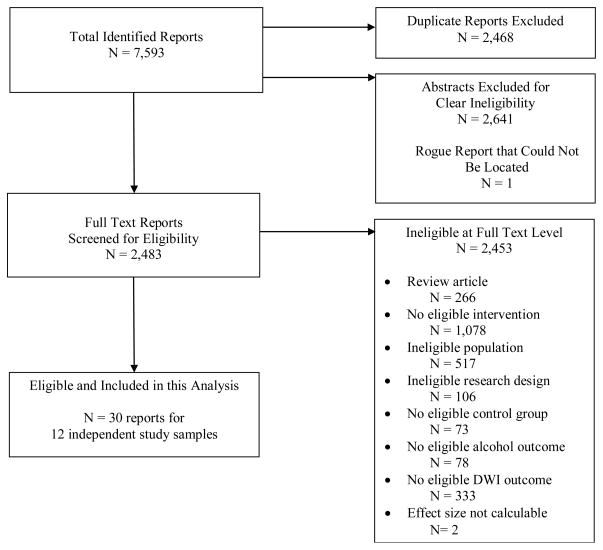
In the larger parent systematic review, 7,593 reports were identified in the literature search, of which 2,468 were duplicates and dropped from consideration, 2,641 were screened as ineligible at the abstract phase, and one report could not be located [26]. Of the 2,483 articles retrieved in full text format, 2,452 were deemed ineligible for the meta-analysis because they did not involve an eligible intervention or population, did not use a group comparison research design, did not have an appropriate control group, or did not report results for an eligible outcome (see Figure 1). One study [37,38] was excluded from the meta-analysis because we were unable to estimate an effect size based on the information included in study reports. 1 Thus, our review included 12 studies reported in 30 documents providing treatment effect information on some measure of drinking and driving.
Figure 1.
Study identification flow diagram.
Description of included studies
Research study, intervention, and participant characteristics are shown in Tables 1 and 2 for all studies contributing to the meta-analysis. Most studies (75%) were conducted in the United States, with the publication date ranging from 1991 through 2011. The majority of the studies (83%) used randomized designs. Only one-third of the studies (33%) employed an intention-to-treat analysis and fewer than one-half (42%) provided a CONSORT-style chart outlining participant recruitment and retention. The average overall attrition rate across groups was moderate, at 23%. In all studies, outcome data were self-reported by youth. Operationalization of the drinking and driving outcomes varied across studies. Most studies (75%) reported frequency of drinking and driving over a specific period of time. Only a few studies used items from validated scales such as the Rutgers Alcohol Problem Index [39,40], Drug Use Screening Inventory [41], or Drinker Inventory of Consequences-2L [42]. Most outcomes were reported prior to or at the six month interval, with only five studies providing data for 12 month results.
Table 1.
Characteristics of included studies.
| Study | Country | RCT | Intervention Program | TX N (Total N) |
TX % Male |
TX % White |
TX Age Range (M) |
TX % in College |
Focal Modality |
TX Format | TX Duration (minutes) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bingham, 2011 [52–54] | USA | Y | M-PASS | 398 (742) | 41 | 80 | 18–20 (18.1) | 100 | MET/MI | Self-adm. | 60 |
| D’Amico, 2002 [55–57] | USA | Y | DARE - Abbreviated | 63* (188)* | 41 | 63 | 14–19 (16) | 0 | Feedback | Group | 50 |
| Risk Skills Training | 63* (188)* | 41 | 63 | 14–19 (16) | 0 | CBT+MET | Group | 50 | |||
| De Micheli, 2004 [41] | Brazil | Y | Brief Intervention (“FRAMES”) | 28 (59) | 60 | NR | 13–18 (15) | 0 | MET/MI | Individual | 20 |
| Preventive Orientation (Leaflet) | 20 (40) | 50 | NR | 10–18 (13.5) | 0 | PET | Individual | 2.5 | |||
| Dearing, 2008 [58] | USA | N | Alcohol Curriculum Infusion | 91 (158) | NR | NR | NR | 100 | CBT | Group | 50 |
| Fromme, 2004 [43,59,60] | USA | Y | Professional-Led LMC | 159 (323) | 62 | 62 | NR (19) | 100 | CBT+MET | Group | 240 |
| Peer-Led LMC | 193 (357) | 62 | 62 | NR (19) | 100 | CBT+MET | Group | 240 | |||
| Howat, 1991 [45] | Australia | Y | Driving Simulator | 24 (48) | NR | NR | 18–35 (NR) | 100 | CBT | Self-adm. | 43 |
| Maio, 2005 [61,62] | USA | Y | Virtual Interactive Party | 135 (266) | 67 | 71 | 14–18 (16) | 0 | CBT+MET | Self-adm. | 25 |
| Paschall, 2011 [39,40] | USA | Y | AlcoholEdu | 1102 (2400) | 44 | 76 | 18- NR (18.8) | 100 | PET | Self-adm. | 150 |
| Schaus, 2009 [42] | USA | Y | Brief Motivational Interview | 128* (275)* | 48 | 78 | 18- NR (20.5) | 100 | MET/MI | Individual | 40 |
| Simão, 2005 [63] | Brazil | N | BASICS | 291 (382)* | 60 | NR | 18- NR (NR) | 100 | MET/MI | Individual | 50 |
| Spirito, 2004 [64–71] | USA | Y | Brief Motivational Interview | 64 (124) | 67 | 72 | 13–17 (16) | 0 | MET/MI | Individual | 37.5 |
| Brief Motivational Interview | 46 (83) | 65 | 79 | 18–19 (18.4) | 46 | MET/MI | Individual | 37.5 | |||
| Werch, 2010 [72,73] | USA | Y | Behavior-Image Model (BIM) | 140 (283) | 44 | 70 | 18–21 (19) | 100 | MET/MI | Individual | 25 |
Notes. RCT: Randomized Controlled Trial; NR: Not reported by study authors; M-PASS: Michigan Prevention and Alcohol Safety for Students, DARE: Drug Abuse Resistance Education, FRAMES: Feedback, Responsibility, Advice, Menu of Options, Empathy, Self-efficacy; LMC: Lifestyle Management Class, CBT: Cognitive Behavioral Therapy, BASICS: Brief Alcohol Screening and Intervention for College Students, MET: Motivational Enhancement Therapy, MI: Motivational Interviewing, PET: Psycho-educational Therapy, Self-adm.: Self-administered
Analytic samples varied across the effect sizes.
The meta-analysis synthesized data from 5,664 students from 12 independent study samples (2,945 in intervention and 2,719 in control conditions). Two studies provided effect sizes comparing two unique intervention groups with two unique control groups, and two studies compared two unique intervention groups with shared control groups; consequently, there were 16 intervention conditions represented in the meta-analysis. Participants were on average 17 years old (range was 13.5 to 20.5 years). On average, participant samples were more than one-half (57%) male and 70% White. 2 Nine interventions targeted college students, six focused on high school students, and one targeted both high school and college youth. Most participant samples (76%) could be classified as regular or potentially hazardous alcohol users based on frequent heavy episodic drinking reported at baseline assessments.
Motivational interviewing/motivational enhancement (MET) was the most frequently applied intervention modality (44%), followed by the combination of cognitive behavioral (CBT) and MET (25%). Nearly one-half of the interventions were delivered individually (44%), one-third were provided in a group format, and the remainder were self-administered via computer or driving simulator. On average, interventions lasted 70 minutes (range from 2.5–240 minutes), with the majority delivered in 1–2 sessions. Most of the interventions (63%) involved some discussion of drinking and driving. For example, the Lifestyle Management Class (LMC) [43] incorporated a discussion about legal considerations around drinking and driving. Another study used a brief motivational interview that included an information sheet about the effects of alcohol on driving [44]. One study examined the effects of a driving simulator intervention that focused specifically on demonstrating how alcohol detrimentally affects driving performance [45]. Finally, three studies involved discussion of harm-reduction approaches, such as planning for safe transportation [39,40,42,43].
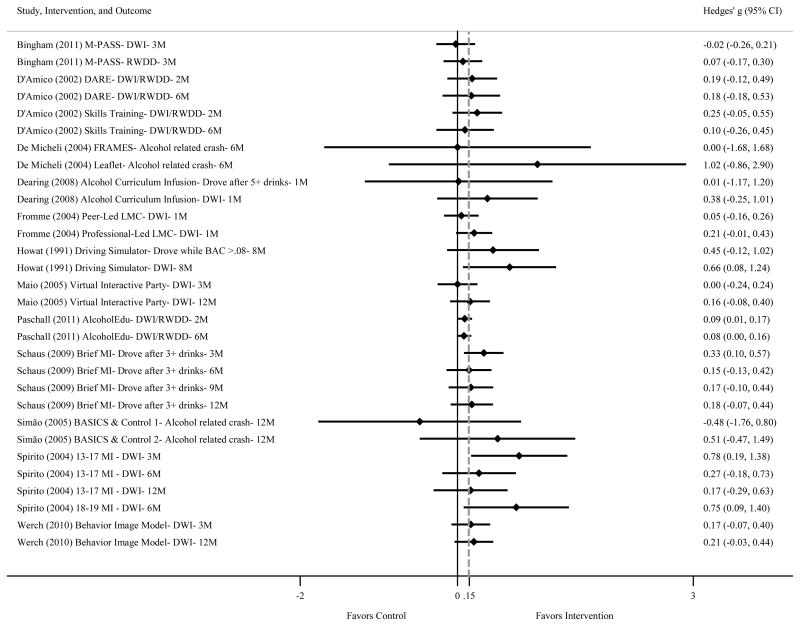
Main intervention effect
Figure 2 shows results from the meta-analysis synthesizing 30 effect sizes from 12 studies (16 intervention groups) on the DWI outcomes. Effect sizes ranged from −0.48 to 1.02 and although most were positive (i.e., favoring the intervention conditions) only five of the 30 effect sizes were significantly different from zero. Nonetheless, the overall results from the meta-analysis indicated that BAIs were associated with statistically significant improvements (i.e., reductions) in DWI, relative to control conditions (ḡ = 0.15, 95% CI [0.08, 0.21], Q = 26.62, p = .59, τ2L3= 0.00, I2L3 =1.00%). 3 Thus, on average, BAIs were associated with a 0.15 standard deviation improvement in DWI outcomes, relative to outcomes for youth in the comparison conditions.
Figure 2.
Forest plot of brief alcohol intervention effects on drinking and driving outcomes (relative to control).
Notes. The left-hand column lists, in alphabetical order, the study authors and publication year, intervention name, outcome type, and timing of follow-up. The estimated effect sizes and their respective confidence intervals are shown in the right column. The vertical line denotes no intervention effect, with effects to the right of the line indicating a positive intervention effect. BAIs were associated with statistically significant improvements in drinking and driving outcomes, relative to control conditions (ḡ= 0.15, 95% CI [0.08, 0.21], Q = 26.62, within-study estimated heterogeneity τ2L2 = 0, between-study τ2L3= 0, proportion of total variation of the effect size due to within-study heterogeneity I2L2= 0, between-study I2L3= 1%).
DWI: Driving While Intoxicated; RWDD: Rode with a Drunk Driver; M: Month follow-up; BAC: Blood Alcohol Concentration; MI: Motivational Interviewing
The reductions in DWI outcomes were larger when we additionally controlled for corresponding intervention effect sizes on heavy episodic drinking outcomes. Results from a bivariate three-level meta-regression model indicated that BAIs that yielded larger reductions in heavy episodic alcohol consumption among under age youth were also likely to yield larger subsequent effects on DWI outcomes (b = 0.37, 95% CI [+0.00, 0.75]). Statistically controlling for effects on heavy episodic drinking outcomes also slightly attenuated the overall mean effect size (ḡ= 0.11, 95% CI [0.04, 0.18]). This finding has important implications for future research and practice, which we address in the discussion section.
Although the primary objective of this study was to examine whether BAIs were associated with reductions in DWI outcomes among participants, it is worth noting that on average, these interventions were also effective in reducing alcohol consumption, which was the primary target of the interventions (ḡ = 0.11, 95% CI [0.03, 0.20]). Thus, there was evidence that BAIs were not only effective in reducing alcohol consumption among adolescents and young adults, but also led to significant reductions in DWI outcomes.
Sensitivity analyses
Results from the meta-analysis for DWI outcomes indicated homogeneity in effects, as evidenced by small τ2 and I2 values (τ2L2 = 0.00, τ2L3= 0.00, I2L2= 0.00, I2L3= 1.00%), and a non-significant heterogeneity statistic (Q = 26.62, p = .59). Table 3 presents the results of these sensitivity analyses, estimated using three-level meta-regression models that additionally controlled for the following study characteristics: whether the brief intervention included DWI information components (e.g., information about the effects of alcohol on driving); whether the study authors reported clear implementation problems with the intervention (versus not); posttest timing of DWI outcomes (in weeks); quasi-experimental research design (versus randomized controlled trial); whether the authors conducted a TOT analysis (versus ITT analysis); and overall study attrition. Model 1 shows results from six separate bivariate meta-regression analyses examining each covariate, in turn. Because we did not have sufficient degrees of freedom to include all covariates in a single multivariable meta-regression model, we then estimated a meta-regression model that included the three statistically significant covariates from the bivariate analyses (Model 2).
Table 3.
Sensitivity analyses examining robustness of effects after controlling for study characteristics (k = 12).
| Model 1a | Model 2 | |||||
|---|---|---|---|---|---|---|
| Characteristics | b | 95% CI | b | 95% CI | ||
| DWI focus (y = 1) | 0.00 | [−0.14, 0.14] | ||||
| Implementation problems (y = 1) | −0.08 | † | [−0.16, 0.00] | −0.11 | [−0.35,0.12] | |
| Posttest timing (weeks) | 0.00 | [0.00, 0.00] | ||||
| QED (y = 1) | 0.10 | [−0.35, 0.56] | ||||
| TOT analysis (y = 1) | 0.04 | * | [0.00, 0.07] | −0.08 | [−0.26, 0.10] | |
| Average attrition | −0.26 | * | [−0.49, −0.03] | −0.11 | [−0.51, 0.28] | |
| Constant | n/a | 0.26 | *** | [0.13, 0.40] | ||
Notes. k: number of studies; b: unstandardized coefficient from meta-regression model; CI: Confidence Interval; QED: Quasi-Experimental Design; TOT: Treatment on the Treated.
Model 1 shows coefficients from six separate bivariate meta-regression models.
p< .10.
p< .05.
p< .01.
p< .001
As shown in Model 1 (Table 3), three covariates had significant or marginally significant bivariate associations with the magnitude of the DWI effect sizes. Namely, intervention effects on DWI were larger for interventions without implementation problems (b = −0.08, 95% CI [−0.16, 0.00]), those using TOT analysis (b = 0.04, 95% CI [0.00, 0.07]), and those with lower attrition rates (b = −0.26, 95% CI [−0.49, −0.03]). Notably, BAIs were effective in reducing DWI, regardless of whether the intervention explicitly provided information related to DWI, outcome measurement timing, and research design.
As shown in Model 2, the multivariable meta-regression model yielded a similar pattern of results as those seen with bivariate models. Again, results indicated that improvements in DWI outcomes were larger for interventions without implementation problems (b = −0.11, 95% CI [−0.35, 0.12]) and those with lower attrition rates (b = −0.11, 95% CI [−0.51, 0.28]); but neither of these effects were statistically significant. After controlling for the other study quality measures, the TOT variable was no longer positively associated with the DWI outcomes. Controlling for the three study characteristics attenuated their associations with intervention effects. In addition, it increased the overall mean effect size (ḡ = 0.26, 95% CI [0.13, 0.40]) indicating that the weaknesses in study design and implementation might have led to overly conservative estimates of the main intervention effects.
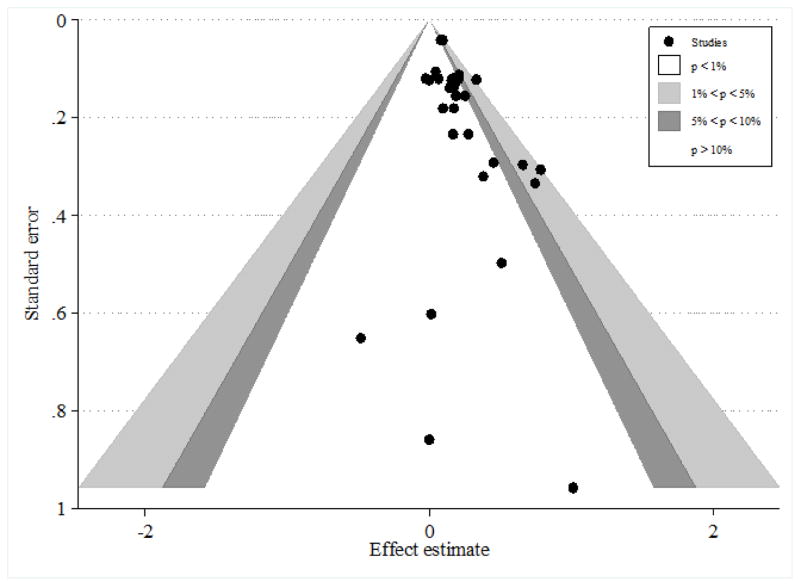
Publication bias
To assess the risk of publication bias we visually inspected a contour-enhanced funnel plot for the DWI effect sizes included in the meta-analysis (see Figure 3). Examination of the funnel plot indicated asymmetry and a general lack of studies in the literature with null or negative effects (regardless of sample size). We used the three-level meta-analytic framework to regress the DWI effect sizes on their standard errors, and found evidence that effect sizes were positively and significantly associated with their standard errors (b=0.83, p = .01).
Figure 3.
Contour-enhanced funnel plot for assessing small-study reporting bias.
Notes. Contours illustrate the statistical significance of the study-effect estimates
Discussion
We used three-level meta-analytic models to synthesize findings from 12 studies examining the effects of BAIs on DWI outcomes among 16 different intervention groups composed of adolescents and young adults. The results indicated that BAIs were associated with modest but statistically significant reductions in drinking and driving, relative to controls. Adolescents and young adults who participated in BAIs reported decreased driving after drinking and related consequences compared to those who did not participate in such interventions. The reductions in drinking and driving were statistically significant, but somewhat modest in clinical terms - many individual studies failed to report statistically significant results on their own, but pooling across studies indicated that BAIs yielded a 0.15 standard deviation improvement in drinking and driving outcomes. Similarly, these interventions had a modest but statistically significant positive effect on overall alcohol consumption among adolescents and young adults. Whether these effects are clinically meaningful will of course depend on client populations, client preferences, and practice settings.
Results from our study were consistent with prior research indicative of relative responsivity of young participants to brief interventions [25,26,47]. For example, results from a meta-analysis of eight BAIs supported their beneficial effects for adolescent substance users [25], and another meta-analysis of 43 computer-delivered BAIs [23] also pointed to reduced post-intervention alcohol use and related problems among college students. Results from the current study therefore support the finding that brief interventions offer promise as one way of addressing not only alcohol consumption among adolescents and young adults, but also drunk driving and related consequences.
The current study indicated that BAIs were associated with modest reductions in drinking and driving and that these results were stable after controlling for study methods, implementation, and outcome measurement characteristics. However, the exact mechanisms of this behavior change are not clear. Scholars have recently called attention to the limited research on brief intervention mechanisms leading to beneficial outcomes, especially among brief motivational interventions, which constituted the largest group of interventions included in the current meta-analysis [48,49]. Some scholars have questioned the adequacy of the process measures typically used to verify the link between key components and the effects of the brief motivational interventions [49]. Indeed, many studies of intervention processes rely on participant self-reports, rather than intervention content analysis [48]. A recent re-analysis of three randomized controlled trials assessed the effect of various characteristics of brief motivational interventions on unhealthy alcohol use but found no robust and consistent predictors of outcomes across different populations and settings [48].
Although homogeneity of effects in this meta-analysis prevented us from conducting complex moderator analysis that could disentangle potential intervention process mechanisms, our results highlighted one potential effective mechanism: improvements in DWI outcomes were larger for interventions that also reduced participants’ excessive episodic alcohol consumption. Preventive efforts aimed at DWI reduction might therefore be more effective in reducing drinking and driving if they target heavy episodic use of alcohol that is commonly reported in this age group. Furthermore, inclusion of DWI information in the BAI was not related to drinking and driving reductions. Although some forms of DWI discussion or information might yield larger effects than others, we could not fully explore these nuances given the limited variability in the studies included in the meta-analysis.
It is important to note the limitations of the current meta-analysis related to the primary studies that were synthesized. First, all measures of substance use and DWI were self-reported. Although official reports of alcohol-impaired driving (i.e., documented DWI related crashes or arrest BAC) are more objective indicators than self-reports, laws guiding the incidence reporting and collection of these statistics vary by geographical location, and many DWI events are undetected by law enforcement [13,22]. Thus, despite the possibility of reporting bias, self-reported data might still provide reasonably accurate estimates of youth’s frequency of drinking and driving.
The results of sensitivity analyses also indicated the possibility of publication bias. It does not appear that the bias is due to small study bias per se, given that null/negative effect sizes are missing from the literature regardless of the sample sizes of those studies. Of course, one must interpret these results cautiously given that the lack of null/negative findings could be due to publication bias resulting from underreporting of null/negative effects, or could be due to other factors such as the strong efficacy of these interventions for reducing DWI (i.e., if these interventions are indeed consistently effective, then primary studies will rarely report null/negative effects). Furthermore, although it is conceivable that the effects of BAIs on DWI outcomes among adolescents and young adults are universally positive, it is also possible that some primary study authors may fail to report non-significant or negative findings. Some authors may believe that null or unfavorable results are more difficult to publish, or may refrain from publishing results they view as unhelpful [50]. Such reporting biases hinder the advancement of science and evidence based decision-making, however, and thus it is critical that primary study authors report all results from studies regardless of their magnitude or direction.
Future research should address effective mechanisms of behavior change in BAIs intended to reduce DWI among underage youth. The parent meta-analysis on which the current sample was based found a number of BAI therapeutic components associated with increased efficacy, including decisional balance or goal-setting exercises, personalized feedback reports, and norm referencing components [26]. Future research should, therefore explore whether certain therapeutic components such as these play different roles in increasing the effectiveness of BAIs on DWI outcomes, or if there are divergent mechanisms underlying observed effects for alcohol consumption versus DWI outcomes.
The current meta-analysis focused exclusively on BAIs in isolation from other types of interventions, thus future research is also needed to examine if BAIs are most effective as stand-alone interventions or in combination with other types of selective approaches. For example, one study suggested that brief parent interventions may reduce high-risk teen driving [51]. Such interventions are not administered directly to the underage drivers but rather influence parental regulation of teen driving and could be a potentially promising addition to BAIs directly targeting younger drivers. Consequently, an important future research direction would be to investigate the effectiveness of combination of brief interventions with other selective measures among underage drinkers.
In conclusion, BAIs are associated with modest positive reductions in driving after drinking and related consequences among adolescents and young adults. These interventions may therefore constitute a cost effective preventive approach to address drinking and driving widespread in this age group. More research is needed to examine if other low-cost interventions can yield similar or larger effects. More methodologically rigorous research on this topic could provide further confidence in the effect estimates derived in this research synthesis. The relatively modest observed effects might be due to the poor methodological practices that are common in this literature (e.g., lack of intention-to-treat analyses, reliance on self-reported outcomes). Although additional research is required to investigate the mechanisms underlying these observed behavior changes, results to date indicate that reducing heavy episodic alcohol consumption may be one way in which BAIs can reduce drunk-driving instances among youth.
Acknowledgments
This work was partially supported by Award Number R01AA020286 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIAAA or the National Institutes of Health.
Appendix
Full Electronic Search Strategy for ERIC, IBSS, PsycARTICLES, PsycINFO, Social Services Abstracts, and Sociological Abstracts Databases within ProQuest
Search Terms used: ((KW=((BASICS) or (Alcohol NEAR intervention) or (Brief NEAR alcohol) or (Brief NEAR intervention) or (Brief NEAR psychotherapeutic) or (Brief NEAR motivation*) or (Brief NEAR therapy) or (Brief NEAR counseling) or (Brief NEAR physician advice) or (Brief NEAR alcohol intervention*) or (Motivational enhancement) or (Motivational NEAR interview*) or (Motivational NEAR intervention) or (University assistance program) or (Student assistance program) or (Alcohol screening) or (Personalized feedback) or (personalised feedback) or (mailed feedback)))) and (KW=((Effective*) or (Efficac*) or (randomized control*) or (randomised control*) or (random*) or (comparison) or (quasi-exper*) or (control group) or (control condition) or (group comparison) or (evaluat*))) and (KW=((Alcohol) or (Drink*) or (Substance) or (Drug) or (Marijuana) or (cannabis) or (cocaine) or (amphetamine) or (heroin))).
Footnotes
The authors of this study reported non-significant differences in drinking and driving rates between the brief alcohol intervention and control groups at multiple follow-ups.
Note that race/ethnicity information was not reported in studies conducted outside of the United States.
References
References marked with an asterisk (*) indicate studies included in the meta-analysis.
- 1.Brown TG, Bhatti J, Leo ID. Driving while impaired (treatments) In: Miller PM, editor. Interventions for Addiction Comprehensive Addictive Behaviors and Disorders. Vol. 3. San Diego, CA: Academic Press; 2013. pp. 207–217. [Google Scholar]
- 2.Li K, Simons-Morton BG, Hingson R. Impaired-driving prevalence among US high school students: Associations with substance use and risky driving behaviors. Am J Public Health. 2013;103:e71–77. doi: 10.2105/AJPH.2013.301296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Voas RB, Lacey JC. Alcohol and highway safety: A review of the state of knowledge. U.S. Department of Transportation, National Highway Traffic Safety Administration; 2011. DOT HS-811 374. [Google Scholar]
- 4.Voas RB, Torres P, Romano E, Lacey JH. Alcohol-related risk of driver fatalities: An update using 2007 data. J Stud Alcohol Drugs. 2012;73:341–350. doi: 10.15288/jsad.2012.73.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Teen drinking and driving: A dangerous mix 2012 [Google Scholar]
- 6.Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among US college students ages 18–24, 1998–2005. J Stud Alcohol Drugs Suppl. 2009;16:12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Highway Traffic Safety Administration (NHTSA) State alcohol-impaired driving estimates. Traffic safety facts 2011 data. Washington (DC): NHTSA, Department of Transportation; 2013. DOT HS, 811 776. [Google Scholar]
- 8.Centers for Disease Control and Prevention. Teen drivers: get the facts. Injury prevention & control: Motor vehicle safety 2012 [Google Scholar]
- 9.National Highway Traffic Safety Administration (NHTSA) Young drivers. Traffic safety facts 2010 data. Washington (DC): NHTSA, Department of Transportation; 2012. DOT HS, 811 622. [Google Scholar]
- 10.Kanny D, Liu Y, Brewer R, Hua L. Binge drinking - United States, 2011. Centers for disease control morbidity and mortality weekly report. 2013;62:77–80. [Google Scholar]
- 11.Patrick ME, Schulenberg JE, Martz ME, Maggs JL, O’Malley PM, et al. Extreme binge drinking among 12th-grade students in the United States: prevalence and predictors. JAMA Pediatr. 2013;167:1019–1025. doi: 10.1001/jamapediatrics.2013.2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shults RA, Elder RW, Sleet DA, Nichols JL, Alao MO, et al. Reviews of evidence regarding interventions to reduce alcohol-impaired driving. Am J Prev Med. 2001;21:66–88. doi: 10.1016/s0749-3797(01)00381-6. [DOI] [PubMed] [Google Scholar]
- 13.Nochajski TH, Stasiewicz PR. Relapse to driving under the influence (DUI): a review. Clin Psychol Rev. 2006;26:179–195. doi: 10.1016/j.cpr.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Heather N. Interpreting the evidence on brief interventions for excessive drinkers: the need for caution. Alcohol Alcohol. 1995;30:287–296. [PubMed] [Google Scholar]
- 15.Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York, NY: Guilford Press; 1991. [Google Scholar]
- 16.Prochaska J, DiClemente C. The transtheoretical approach: Crossing traditional boundaries of therapy. Homewood, IL: Dow Jones-Irwin; 1984. [Google Scholar]
- 17.Brown TG, Dongier M, Ouimet MC, Tremblay J, Chanut F, et al. Brief motivational interviewing for DWI recidivists who abuse alcohol and are not participating in DWI intervention: a randomized controlled trial. Alcohol Clin Exp Res. 2010;34:292–301. doi: 10.1111/j.1530-0277.2009.01092.x. [DOI] [PubMed] [Google Scholar]
- 18.Schermer CR, Moyers TB, Miller WR, Bloomfield LA. Trauma center brief interventions for alcohol disorders decrease subsequent driving under the influence arrests. J Trauma. 2006;60:29–34. doi: 10.1097/01.ta.0000199420.12322.5d. [DOI] [PubMed] [Google Scholar]
- 19.Wells-Parker E, Williams M. Enhancing the effectiveness of traditional interventions with drinking drivers by adding brief individual intervention components. J Stud Alcohol Drugs. 2002;63:655–664. doi: 10.15288/jsa.2002.63.655. [DOI] [PubMed] [Google Scholar]
- 20.Wells Parker E, Bangert Drowns R, McMillen R, Williams M. Final results from a meta analysis of remedial interventions with drink/drive offenders. Addiction. 1995;90:907–926. doi: 10.1046/j.1360-0443.1995.9079074.x. [DOI] [PubMed] [Google Scholar]
- 21.McKnight AJ, Voas RB. The effect of license suspension upon DWI recidivism. Alcohol Drugs Driving. 1991;7:43–54. [Google Scholar]
- 22.Ahlin EM, Zador PL, Rauch WJ, Howard JM, Duncan GD. First-time DWI offenders are at risk of recidivating regardless of sanctions imposed. J Crim Justice. 2011;39:137–142. doi: 10.1016/j.jcrimjus.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carey KB, Scott-Sheldon LA, Elliott JC, Bolles JR, Carey MP. Computer-delivered interventions to reduce college student drinking: a meta-analysis. Addiction. 2009;104:1807–1819. doi: 10.1111/j.1360-0443.2009.02691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins-Biddle J, Dilonardo J. Alcohol and highway safety: Screening and brief intervention for alcohol problems as a community approach to improving traffic safety. Washington, DC: National Highway Traffic Safety Administration; 2013. DOT HS 811 836. [Google Scholar]
- 25.Tait RJ, Hulse GK. A systematic review of the effectiveness of brief interventions with substance using adolescents by type of drug. Drug Alcohol Rev. 2003;22:337–346. doi: 10.1080/0959523031000154481. [DOI] [PubMed] [Google Scholar]
- 26.Tanner-Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. J Subst Abuse Treat. 2014 doi: 10.1016/j.jsat.2014.09.001. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. J Educ Stat. 1981;6:107–128. [Google Scholar]
- 28.Sánchez-Meca J, Marín-Martínez F, Chacón-Moscoso S. Effect-size indices for dichotomized outcomes in meta-analysis. Psychol Methods. 2003;8:448–467. doi: 10.1037/1082-989X.8.4.448. [DOI] [PubMed] [Google Scholar]
- 29.Higgins JP, Deeks JJ, Altman DG. In: Cochrane handbook for systematic reviews of interventions Chichester, Special topics in statistics. Higgins JPT, Green S, editors. UK: John Wiley & Sons; 2008. pp. 481–529. [Google Scholar]
- 30.Cheung MW. Modeling dependent effect sizes with three level meta-analyses: a structural equation modeling approach. Psychol Methods. 2013;19:211–229. doi: 10.1037/a0032968. [DOI] [PubMed] [Google Scholar]
- 31.Konstantopoulos S. Fixed effects and variance components estimation in three-level meta-analysis. Res Synthesis Methods. 2011;2:61–76. doi: 10.1002/jrsm.35. [DOI] [PubMed] [Google Scholar]
- 32.Van den Noortgate W, López-López JA, Marín-Martínez F, Sánchez-Meca J. Three-level meta-analysis of dependent effect sizes. Behav Res Methods. 2013;45:576–594. doi: 10.3758/s13428-012-0261-6. [DOI] [PubMed] [Google Scholar]
- 33.Cheung MW. Fixed-and random-effects meta-analytic structural equation modeling: Examples and analyses in R. Behav Res Methods. 2014;46:29–40. doi: 10.3758/s13428-013-0361-y. [DOI] [PubMed] [Google Scholar]
- 34.Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295:676–680. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- 35.Palmer TM, Peters JL, Sutton AJ, Moreno SG. Contour enhanced funnel plots for meta-analysis. Stata J. 2008;8:242–254. [Google Scholar]
- 36.Rothstein HR, Sutton AJ, Borenstein M. Publication bias in meta-analysis: Prevention, assessment and adjustments. West Sussex, England: John Wiley & Sons; 2005. [Google Scholar]
- 37.LaChance H. Group motivational intervention for underage college student drinkers in mandated university-based programming. Diss Abstr Int. 2004;80 (UMI No. 3136631) [Google Scholar]
- 38.LaChance H, Ewing SWF, Bryan AD, Hutchison KE. What makes group MET work? A randomized controlled trial of college student drinkers in mandated alcohol diversion. Psychol Addict Behav. 2009;23:598–612. doi: 10.1037/a0016633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39*.Paschall MJ, Antin T, Ringwalt CL, Saltz RF. Effects of AlcoholEdu for college on alcohol-related problems among freshmen: A randomized multicampus trial. J Stud Alcohol Drugs. 2011;72:642–650. doi: 10.15288/jsad.2011.72.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40*.Paschall MJ, Antin T, Ringwalt CL, Saltz RF. Evaluation of an Internet-based alcohol misuse prevention course for college freshmen: Findings of a randomized multi-campus trial. Am J Prev Med. 2011;41:300–308. doi: 10.1016/j.amepre.2011.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41*.De Micheli D, Fisberg M, Formigoni ML. Study on the effectiveness of brief intervention for alcohol and other drug use directed to adolescents in a primary health care unit. Rev Assoc Med Bras. 2004;50:305–313. doi: 10.1590/s0104-42302004000300040. [DOI] [PubMed] [Google Scholar]
- 42*.Schaus JF, Sole ML, McCoy TP, Mullett N, O’Brien MC. Alcohol screening and brief intervention in a college student health center: A randomized controlled trial. J Stud Alcohol Drugs Suppl. 2009:131–141. doi: 10.15288/jsads.2009.s16.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43*.Fromme K, Corbin W. Prevention of heavy drinking and associated negative consequences among mandated and voluntary college students. J Consult Clin Psychol. 2004;72:1038–1049. doi: 10.1037/0022-006X.72.6.1038. [DOI] [PubMed] [Google Scholar]
- 44*.Spirito A, Monti PM, Barnett NP, Colby SM, Sindelar H, et al. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. J Pediatr. 2004;145:396–402. doi: 10.1016/j.jpeds.2004.04.057. [DOI] [PubMed] [Google Scholar]
- 45*.Howat P, Robinson S, Binns C, Palmer S, Landauer A. Educational biofeedback driving simulator as a drink-driving prevention strategy. J Alcohol Drug Educ. 1991;37:7–14. [Google Scholar]
- 46*.Bingham CR, Barretto AI, Walton MA, Bryant CM, Shope JT, et al. Efficacy of a web-based, tailored, alcohol prevention/intervention program for college students: Three-month follow-up. J Drug Educ. 2011;41:405–430. doi: 10.2190/DE.41.4.e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brown TG, Dongier M, Ouimet MC, Tremblay J, Chanut F, et al. The role of demographic characteristics and readiness to change in 12-month outcome from two distinct brief interventions for impaired drivers. J Subst Abuse Treat. 2012;42:383–391. doi: 10.1016/j.jsat.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 48.Bertholet N, Palfai T, Gaume J, Daeppen JB, Saitz R. Do brief alcohol motivational interventions work like we think they do? Alcohol Clin Exp Res. 2014;38:853–859. doi: 10.1111/acer.12274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heather N. Toward an understanding of the effective mechanisms of alcohol brief interventions. Alcohol Clin Exp Res. 2014;38:626–628. doi: 10.1111/acer.12336. [DOI] [PubMed] [Google Scholar]
- 50.McCambridge J. A case study of publication bias in an influential series of reviews of drug education. Drug Alcohol Rev. 2007;26:463–468. doi: 10.1080/09595230701494366. [DOI] [PubMed] [Google Scholar]
- 51.Simons-Morton BG, Hartos JL, Beck KH. Increased parent limits on teen driving: positive effects from a brief intervention administered at the Motor Vehicle Administration. Prev Sci. 2004;5:101–111. doi: 10.1023/b:prev.0000023080.76550.ab. [DOI] [PubMed] [Google Scholar]
- 52*.Barretto AI, Bingham CR, Goh KN, Shope JT. Developing a web-based health promotion intervention: A case study from a brief motivational alcohol program. Health Promot Pract. 2011;12:193–201. doi: 10.1177/1524839909353740. [DOI] [PubMed] [Google Scholar]
- 53*.Bingham CR, Barretto AI, Shope JT. Web-based alcohol brief intervention for first-year university students: Recruitment participation and retention. Alcohol Clin Exp Res. 2008;32:253A. [Google Scholar]
- 54*.Bingham CR, Barretto AI, Walton MA, Bryant CM, Shope JT, et al. Efficacy of a web-based, tailored, alcohol prevention/intervention program for college students: Initial findings. J Am Coll Health. 2010;58:349–356. doi: 10.1080/07448480903501178. [DOI] [PubMed] [Google Scholar]
- 55*.D’Amico EJ. Adolescent risk-taking and prevention: Development of a new risk skills training program. Diss Abstr Int. 1999;188 (UMI No. 9947209) [Google Scholar]
- 56*.D’Amico EJ, Fromme K. Implementation of the risk skills training program: A brief intervention targeting adolescent participation in risk behaviors. Cognitive Behav Pract. 2000;7:101–117. [Google Scholar]
- 57*.D’Amico EJ, Fromme K. Brief prevention for adolescent risk-taking behavior. Addiction. 2002;97:563–574. doi: 10.1046/j.1360-0443.2002.00115.x. [DOI] [PubMed] [Google Scholar]
- 58*.Dearing J. Reducing alcohol-related harm through utilizing a harm prevention curriculum at the University of Central Oklahoma. Diss Abstr Int 2008 [Google Scholar]
- 59*.Barnett NP, Tevyaw TOL, Fromme K, Borsari B, Carey KB, et al. Brief alcohol interventions with mandated or adjudicated college students. Alcohol Clin Exp Res. 2004;28:966–975. doi: 10.1097/01.alc.0000128231.97817.c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60*.Fromme K, Orrick D. The lifestyle management class: A harm reduction approach to college drinking. Addict Res Theory. 2004;12:335–351. [Google Scholar]
- 61*.Maio RF, Shope JT, Blow FC, Gregor MA, Zakrajsek JS, et al. Randomized controlled trial of an emergency department-based interactive computer program to prevent alcohol misuse among injured adolescents. Acad Emerg Med. 2003;10:514–515. doi: 10.1016/j.annemergmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 62*.Maio RF, Shope JT, Blow FC, Gregor MA, Zakrajsek JS, et al. A randomized controlled trial of an emergency department-based interactive computer program to prevent alcohol misuse among injured adolescents. Ann Emerg Med. 2005;45:420–429. doi: 10.1016/j.annemergmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 63*.Simão MO. Doctoral dissertation. Universidade de São Paulo; RiberãoPreto, Brazil: 2005. Avaliação da eficácia da intervenção breve para redução de danosemestudantesuniversitários da UNESP quefazemusoexcessivo de bebidasalcoólicas [Evaluating the effectiveness of brief intervention for harm reduction in university UNESP students who overuse alcohol/Assessment of the effectiveness of brief intervention to reduce harm in university students who use alcohol of unesp excessively] [Google Scholar]
- 64*.Barnett NP, Lebeau-Craven R, O’Leary TA, Colby SM, Woolard R, et al. Predictors of motivation to change after medical treatment for drinking-related events in adolescents. Psychol Addict Behav. 2002;16:106–112. [PubMed] [Google Scholar]
- 65*.Barnett NP, Monti PM, Wood MD. Motivational interviewing for alcohol-involved adolescents in the emergency room. In: Wagner EF, Waldron H, editors. Innovations in adolescent substance abuse interventions. New York: Bergman Press; 2001. pp. 143–168. [Google Scholar]
- 66*.Becker SJ, Spirito A, Hernandez L, Barnett NP, Eaton CA, et al. Trajectories of adolescent alcohol use after brief treatment in an emergency department. Drug Alcohol Depend. 2012;125:103–109. doi: 10.1016/j.drugalcdep.2012.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67*.Monti PM, Barnett N, O’Leary T, Colby SM. Adolescents, alcohol, and substance abuse: reaching teens through brief interventions. In: Monti PM, Colby SM, O’Leary T, editors. Motivational enhancement for alcohol-involved adolescents. New York: Guilford; 2001. pp. 145–182. [Google Scholar]
- 68*.Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- 69*.National Addiction Centre. Brief intervention leaves teenage drinkers less likely to revisit accident and emergency. Drug Alcohol Findings. 2000;3:13. [Google Scholar]
- 70*.Neighbors CJ, Barnett NP, Rohsenow DJ, Colby SM, Monti PM. Cost-effectiveness of a motivational intervention for alcohol-involved youth in a hospital emergency department. J Stud Alcohol Drugs. 2010;71:384–394. doi: 10.15288/jsad.2010.71.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71*.Tapert SF, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, et al. Depressed mood, gender, and problem drinking in youth. J Child Adolesc Subst Abuse. 2003;12:55–68. [Google Scholar]
- 72*.Werch CE, Moore MJ, Bian H, DiClemente CC, Ames SC, et al. Efficacy of a brief image-based multiple-behavior intervention for college students. Ann Behav Med. 2008;36:149–157. doi: 10.1007/s12160-008-9055-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73*.Werch CE, Moore MJ, Bian H, DiClemente CC, Huang IC, et al. Are effects from a brief multiple behavior intervention for college students sustained over time? Prev Med. 2010;50:30. doi: 10.1016/j.ypmed.2009.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]