Abstract
Amebic liver abscess is a parasitic disease which is often encountered in tropical countries. A hepatogastric fistula secondary to an amebic liver abscess is a rare complication of this disease and there are only a handful of reported cases in literature. Here we present a case of an amebic liver abscess which was complicated with the development of a hepatogastric fistula. The patient presented with the Jaundice, pain and distension of abdomen. The Jaundice and pain improved partially after he had an episode of brownish black colored increase in frequency of stools for 5 to 6 d. Patient also had ascites and anemia. He was a chronic alcohol drinker. Esophagogastroduodenoscopy performed in view of the above findings. It showed a fistulous opening with bilious secretions along the lesser curvature of the stomach. On imaging multiple liver abscesses seen including one in sub capsular location. The patient was managed conservatively with antiamebic medications along with proton pump inhibitors. The pigtail drainage of the sub capsular abscess was done. The patient improved significantly. The repeat endoscopy performed after about two months showed reduction in fistula size. A review of the literature shows that hepatogastric fistulas can be managed conservatively with medications and drainage, endoscopically with biliary stenting or with surgical excision.
Keywords: Amebic liver abscess, Hepatogastric fistula, Esophagogastroduodenoscopy, Entaameba histolytica, Ultrasonography, Computed tomography
Core tip: Hepatogastric fistula is a rare complication of the amebic liver abscess. High index of suspicion is required for its diagnosis. The presenting complaints may be brownish black vomitus or stool. It can be managed conservatively, endoscopically or surgically depending on case. Hence in cases of amebic liver abscess developing brownish black stools or vomiting we should always rule out hepatogastric fistula formation especially when it is associated with improvement of symptoms.
INTRODUCTION
Amebic liver abscess is a parasitic disease which is commonly encountered in tropical countries[1]. A hepatogastric fistula secondary to an amebic liver abscess is a rare complication and only a handful of cases have been reported in literature[2,3]. A patient presenting with an anchovy sauce like vomitus or stool along with a simultaneous decrease in a preexisting pain in the abdomen should alert a clinician to the possibility of a hepatogastric fistula due to an abscess. There are a few other causes of this clinical entity. This condition can be managed conservatively with antibiotics and proton pump inhibitors, failing which surgery is the treatment of choice. Surgery involves excision of the fistulous tract with anastomosis. Here we report a case which presented with an anchovy sauce like stool and was successfully managed conservatively.
CASE REPORT
A 47-year-old male, with a history of regular alcohol intake presented with a history of pain and swelling in right upper abdomen which was mild to moderate in intensity, dull aching in character with occasional throbbing sensation with no radiation to any other site. The pain lasted a month and a half and was followed by generalized distension of the abdomen. This was accompanied with high color urine and jaundice. There was no fever. The patient then developed an increased frequency of stool which was liquid brownish-black and went on for 6 d. This was associated with a marked improvement in the abdominal pain and a decrease in the swelling over right upper abdomen. On examination there was tender hepatomegaly with ascites. The patient’s hemoglobin was 9.3 g/dL and leucocyte count was 16700/mcl. There was reversal of albumin and globulin ratio, increase in aspartate transaminase was more than alanine transaminase and increased total and direct bilirubin. Ascitic routine microscopy revealed a high serum ascites albumin gradient. Patient’s ultrasonography showed hepatomegaly with multiple heterogeneous solid cystic lesions with thickened walls, the largest measured 13.7 cm × 7.5 cm. In view of a history of daily alcohol intake with recent onset of black stool and a physical finding of ascites an esophagogastroduodenoscopy was performed. The study revealed a 2 cm × 2 cm deep ulcer with bilious discharge just above incisura on lesser curvature of the stomach (Figure 1). There were no varices. On further evaluation computed tomography (CT) suggested multiple large hepatic abscesses in both lobes of liver, the largest measuring 12.8 cm × 8.6 cm × 3.4 cm in the right lobe of liver. One of the abscesses in right lobe was sub capsular. The left lobe of liver had a hepatic abscess in segment 3 which had an exophytic extension and was indenting the lesser curvature of stomach. Air pockets were seen in the abscess cavity suggesting the probability of a fistulous opening within the stomach (Figure 2). His blood antibodies [enzyme linked immunosorbent assay (ELISA)] for entaamoeba histolytica came positive. An ultrasonography guided pigtail catheter was placed in right sub capsular abscess. The abscess content was anchovy sauce like. Pus culture was negative for bacteria. He was started on metronidazole and other supporting medications. He was also started on diloxanide furoate for luminal clearance of cysts. The patient improved clinically and at 4 wk a repeat endoscopy was performed. It showed a significant decrease in the size of the fistulous tract. A surgical option was explained to the patient and his relatives but they opted for medical line of management in view of risk associated Child Pugh C status. He was continued with close monitoring with proton pump inhibitors. The patient has been in regular follow up since the past 6 mo. The patient had American society of anesthesiologists’ classification of physical status of 4 on presentation, 3 at the time of discharge and 2 at 6 mo follow up.
Figure 1.

On retroflexon in stomach fistula with bile seen.
Figure 2.
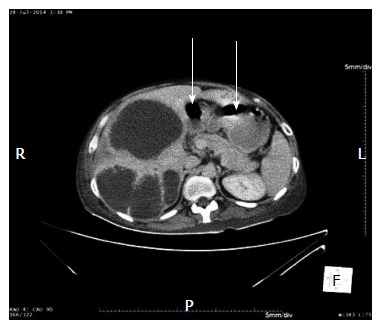
Multiple liver abscess with air pocket seen in the abscess in left lobe. (White arrows).
DISCUSSION
The prevalence of E. histolytica infections in India has been shown to range from 3.6% to 47.4% in different areas[1]. Amebic liver abscess occurs in less than 1% of entaameba histolytica infested patients[2]. Liver abscess rupturing into the pleural and peritoneal cavities is a relatively common phenomenon[3]. Only a handful of case reports of hepatogastric fistula have been published till now as it is a rare complication[3]. Hepatogastric fistulas have also been reported in cases of hepatocellular carcinoma intruding into stomach and presenting as an upper gastrointestinal bleed[4], post embolization for hepatocellular carcinoma leading to the formation of an abscess[5], as a complication of placing a pig tail in a liver abscess and also in cases of post hepatic surgeries. An iatrogenic hepatogastric fistula can be done for biliary drainage in infants with congenital obstructive jaundice.
The presentations of hepatogastric fistula secondary to amebic liver abscess can be as an anchovy sauce color vomitus or stool, hematemesis or malena[6]. In our patient decompression of the abscess into the stomach probably lead to the anchovy sauce color of stool and subsequent improvement of pain. Diagnosis was made based on the imaging and endoscopic findings. ELISA test for detecting antibodies was done for confirming entaameba histolytica as the causative agent. On the CT scan images the abscess seen with air pocket in continuation with the stomach was also a clue to the presence of the fistula (if it was performed before the endoscopy). On esophagogastroduodenoscopy the fistulous opening was seen as deep ulcer with (as in our case) or without bilious discharge[3]. In our case the diagnosis was confirmed taking into account the serology, CT finding and endoscopic findings. Rupture of an amebic liver abscess into an adjacent structure such as pleural and peritoneal cavity is a life threatening condition but rupture into stomach is not a dreaded complication.
Definitive management is surgical but if the patient’s general condition does not permit surgery (as in our case) conservative management has also showed improvement[7]. Conservative treatment includes metronidazole for clearance in extraintestinal site and diloxanide furoate or paromomycin for luminal clearance. In certain cases of impending rupture of sub capsular abscess, pigtail drainage of the liver abscess has to be done to avoid complications. Biliary stenting has been found to hasten the recovery due to selective drainage of bile through common bile duct[8]. Nutrition can be given through per oral, nasojejunal tube, or feeding jejunostomy. Spontaneous closure of fistula can be seen within 5 wk of conservative management which was observed in our case[9]. If no improvement is observed on conservative management or if there is clinical worsening then surgical excision of the fistulous tract with gastric anastomosis is an option. Complications of hepatogastric fistulas include sepsis, debilitation and electrolyte imbalance[10].
In conclusion, hepatogastric fistula is a very unusual complication of liver abscess. One has to have a high index of suspicion for it to be diagnosed early. Management can either be conservative, endoscopic or surgical. We have managed this patient conservatively as patient was Child Pugh C status and high risk for surgery.
ACKNOWLEDGMENTS
We acknowledge Dr. Ravindra Surude, Dr. Samit Jain and Dr. Dharmesh Shah for their help.
COMMENTS
Case characteristics
A 47-year-old male, chronic alcoholic presented with pain and distention of abdomen along with jaundice followed by brownish black diarrhea for 5 to 6 d.
Clinical diagnosis
Patient was having symptoms of chronic liver disease along with hepatomegaly and pain specifically in right upper quadrant.
Differential diagnosis
This is a case of chronic liver disease with either hepatocellular carcinoma or liver abscess or spontaneous bacterial peritonitis causing decompensation of liver disease.
Laboratory diagnosis
Patient had anemia and high leucocyte count along with inversion of albumin and globulin ratio and presence of antibodies to entaameba suggestive of chronic liver disease along with infection.
Imaging diagnosis
Ultrasonography and computed tomography suggestive of liver abscess with air in left lobe abscess probably fistulous opening which is confirmed on esophagogastroduodenoscopy.
Treatment
Patient was managed conservatively with metronidazole, diloxanide furoate.
Related reports
Very few case reports were published related to hepatogastric fistula due to hepatocellular carcinoma, iatrogenic and abscess.
Term explanation
Hepatogastric fistula is communication of liver with stomach due to various etiologies.
Experiences and lessons
High index of suspicion is required for diagnosis of hepatogastric fistula. Patient had marked improvement in pain and upper right quadrant swelling once he had brownish black stools for 5 to 6 d. Though rare, knowledge of this complication leads to early diagnosis and prompt treatment.
Peer-review
This is a well prepared and detailed case report referring to a rare complication of amebic liver abscess, a hepatogastric fistula. The manuscript is well organized with a comprehensive discussion section.
Footnotes
Informed consent statement: The study participant provided informed written consent.
Conflict-of-interest statement: There are no conflicts of interest of any authors.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: November 22, 2014
First decision: December 12, 2014
Article in press: May 28, 2015
P- Reviewer: Al-Shamma S, Betrosian AP, Mentes O, Nakayama Y S- Editor: Gong XM L- Editor: A E- Editor: Jiao XK
References
- 1.Parasite related diarrhoeas. WHO Scientific Working Group. Bull World Health Organ. 1980;58:819–830. [PMC free article] [PubMed] [Google Scholar]
- 2.Wells CD, Arguedas M. Amebic liver abscess. South Med J. 2004;97:673–682. doi: 10.1097/00007611-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Budhiraja S, Dhatt GS, Babra RS. Hepatogastric fistula in a pediatric patient. Pediatr Surg Int. 2006;22:853–855. doi: 10.1007/s00383-006-1743-3. [DOI] [PubMed] [Google Scholar]
- 4.Park H, Kim SU, Choi J, Park JY, Ahn SH, Han KH, Chon CY, Park YN, Kim do Y. Hepatogastric fistula caused by direct invasion of hepatocellular carcinoma after transarterial chemoembolization and radiotherapy. Korean J Hepatol. 2010;16:401–404. doi: 10.3350/kjhep.2010.16.4.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang CY, Leung SW, Wang JH, Yu PC, Wang CC. Delayed spontaneous hepatogastric fistula formation following transcatheter arterial embolisation and radiotherapy for hepatocellular carcinoma. Br J Radiol. 2009;82:e105–e107. doi: 10.1259/bjr/63705954. [DOI] [PubMed] [Google Scholar]
- 6.Siddiqui MN, Rizvi SB, Ahmed M, Rizvi IH. Case report: amoebic liver abscess complicated by a hepatoduodenal fistula. Clin Radiol. 1992;46:142–143. doi: 10.1016/s0009-9260(05)80324-1. [DOI] [PubMed] [Google Scholar]
- 7.Moazam F, Nazir Z. Amebic liver abscess: spare the knife but save the child. J Pediatr Surg. 1998;33:119–122. doi: 10.1016/s0022-3468(98)90376-1. [DOI] [PubMed] [Google Scholar]
- 8.Sandeep SM, Banait VS, Thakur SK, Bapat MR, Rathi PM, Abraham P. Endoscopic biliary drainage in patients with amebic liver abscess and biliary communication. Indian J Gastroenterol. 2006;25:125–127. [PubMed] [Google Scholar]
- 9.Sheldon GF, Gardiner BN, Way LW, Dunphy JE. Management of gastrointestinal fistulas. Surg Gynecol Obstet. 1971;133:385–389. [PubMed] [Google Scholar]
- 10.Chung MA, Wanebo HJ. Surgical management and treatment of gastric and duodenal fistulas. Surg Clin North Am. 1996;76:1137–1146. doi: 10.1016/s0039-6109(05)70502-8. [DOI] [PubMed] [Google Scholar]


