Abstract
Double-bundle (DB) anterior cruciate ligament (ACL) reconstruction using a four-strand semitendinosus tendon was started in our department in July 1994. The motivation for starting the procedure was that the EndoButton with an inside-out procedure instrument became available in Japan. A review article of our DB ACL reconstruction procedure was summarized for the twentieth anniversary of the surgical procedure. Initial tension setting of the two grafts was changed in the first 8 years to achieve better stability during DB ACL reconstruction. A randomized clinical trial (RCT) was started in July 2002 to clarify superiority of the DB procedure to single-bundle (SB) reconstruction under the concept of anatomic reconstruction. Several anatomic studies were performed to describe normal ACL anatomy, which is essential for realizing anatomic reconstruction. A remnant-preserving technique would be an additional option for our DB procedure to improve reconstruction outcomes. Thus, a new remnant-preserving DB procedure was started in 2012. The reproducibility of the new procedure was investigated using three-dimensional computed tomography images. More complex procedures were performed using a transtibial technique and EndoButtons. Initial tension balancing between the two grafts was important for a better outcome. Superiority of knee stability after the DB compared to that after the SB procedure was clarified by the RCT. However, no patient consensus has been reached on any subjective advantage to the DB procedure. Studies of normal ACL anatomy have left questions unresolved regarding where the two tunnels should be created for direct and indirect insertions based on normal anatomy. A new remnant-preserving DB ACL procedure has been practiced. The procedure was more reproducible with respect to creating the femoral tunnel. DB ACL reconstruction using a semitendinosus tendon is an attractive option when pursuing a better outcome for patients.
Keywords: Anterior cruciate ligament reconstruction, Anatomy, Tunnel, Remnant
The year 2014 was the twentieth anniversary of the double-bundle (DB) anterior cruciate ligament (ACL) reconstruction using a semitendinosus (ST) tendon with the EndoButton (Smith & Nephew Endoscopy Inc., Andover, MA, USA) for femoral fixation, which we began performing in July 1994.1) Surgeons often attempt to develop new procedures to achieve better outcomes from their surgeries. We also do our best to implement better practices, as I have reflected on the many years I have worked as a ligament surgeon. This review continues the work achieved up to the present of attempts to improve outcomes in our patients with a ruptured ACL. This review summarizes the work achieved to the present.
DEVELOPMENT OF DB ACL RECONSTRUCTION
A prospective study was performed to investigate the differences between single-bundle (SB) ACL reconstruction using a four-strand ST tendon and bone-patellar tendon-bone (BPTB) grafts from April 1992 to June 1994.2) While clinical research was being performed, features of the hamstring tendon and BPTB were not well understood as popular graft tissues in knee and sports medicine groups, because a ligament augmentation device made of polypropylene fiber had been used for ACL reconstruction since 19863) in our department.
The results of the comparative study showed that more poor stability cases occurred in the SB-ST group.2) In contrast, poorly satisfied patients were more frequent in the BPTB group.4) These results revealed the future direction for inventing a new ACL reconstruction method with an ST graft that provides better stability.
Arthroscopically assisted inside-out ACL reconstruction instruments and the EndoButton system became available in Japan in December 1994, suggesting that more complex procedures would be possible with those systems. "How could it be possible to improve postoperative stability using a hamstring tendon graft?" More accurate tunnel placement would be possible using the inside-out single incision technique. ACL reconstruction consisted of anteromedial (AM) and posterolateral (PL) bundles that were more anatomic with better stability using the same hamstring tendon. DB ACL reconstruction using an ST tendon with two EndoButtons began to be used in July 1994.1) The procedure consisted of forming two tibial and two femoral tunnels with a pullout fixation. The concept of tunnel placement was based on graft isometricity, with the femoral tunnel placed high in the intercondylar lateral wall in the flexion position.5) Tunnel position was described as 0:30 for the AM tunnel and 1:30 for the PL tunnel on the intercondylar clock.6) The AM tibial guidewire was placed in the center of the natural ACL stump and the PL guidewire was more posteriorly placed 3-4 mm away from the AM guidewire. The procedure was performed arthroscopically with a better understanding of the idea of notch impingement in the 1990s.7)
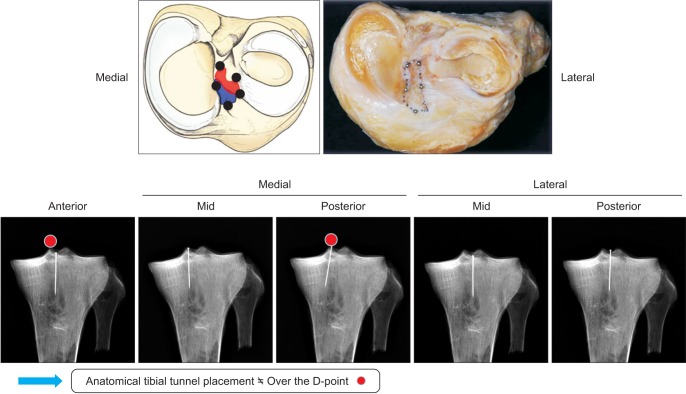
At the beginning, the most promising features of the DB procedure were that a greater tendon-bone junction area would initiate better stabilizing function of the graft, the greater tendon-bone junction area facilitates graft healing; and anterior notch plasty could be performed less frequently because the thinner two isolated grafts could be easily put in the natural ACL stump with four tunnels. For example, a 6-mm diameter DB graft is identical in volume to a 9-mm diameter SB graft, but the circumference of the combined graft is 1.4 times greater than the single same sized graft (Fig. 1).
Fig. 1. A greater tendon-bone junction area is achieved with the double-bundle (DB) technique. DB reconstruction features: (1) greater tendon-bone junction area facilitating better stabilization of the graft, (2) greater tendon-bone junction area facilitating graft healing, (3) less anterior notch plasty, and (4) the possibility to realize ideal initial graft settings.
OUTCOMES OF THE INITIAL DB VS. SB STUDY GROUPS FROM APRIL 1992 TO 1994
Outcome of the Initial Pilot Study
The clinical outcomes 2 years postoperatively in 54 of 62 consecutive patients were reported. The preliminary reresults suggested that the DB procedure tended to result in better anterior stability according to manual knee laxity tests. Fewer patients with anterior laxity > 5-mm difference measured with the KT-1000 (MEDmetric, San Diego, CA, USA)were found compared with our SB technique results under the same aggressive rehabilitation 2 years after surgery.1)
Mid- To Long-term Results of the Initial Study Groups
A retrospective case-control study was performed to investigate the mid-term results of DB ACL reconstruction and to compare those of the SB group. The SB group consisted of 56 patients with a follow-up period ≥ 24 months (mean, 46.5 months). The DB group consisted of 79 patients with a follow-up period ≥ 24 months (mean, 40.8 months). A significantly greater number of patients in the SB group were positive on the Lachman test (34% in the SB group and 13% in the DB group). Mean KT-1000 anterior laxity of 2.7 ± 2.3 mm in the SB group was signficnatly greater than the 1.9 ± 1.9 mm in the DB group. The total Lysholm knee scale score was 93 points in both groups. The subjective recovery scores were equivalent (82% in the SB group and 86% in the DB group; 100% = full mark), respectively.8)
CHANGE IN INITIAL FORCE SETTING BETWEEN AM AND PL GRAFTS FROM 1994 TO 2002
"How can outcomes be improved for DB reconstruction, particularly regarding stability?" We changed the initial force setting between AM and PL grafts to achieve better outcomes during the first 8 years of using DB ACL reconstruction.9) A total of 151 primary unilateral DB ACL procedures were performed by the author from 1994 to 2002, with follow-up of 24 months or more, and were included in the study. The patients were divided into the following three groups according to the initial force setting of the AM and PL grafts. Higher initial tension was applied manually to the group I (n = 59) AM grafts compared to the PL grafts. Higher tension was applied to the group II (n = 53) PL grafts compared to the AM grafts. An attempt was made to set the initial tension equally between the two grafts in group III (n = 39). All fixations were performed at 30° of flexion. The results did not suggest that maximum manual initial tension be applied to the AM or PL graft with an imbalance in graft tension at 30° of flexion during DB ACL reconstruction to achieve better clinical outcomes. It reminded us that balancing tension between AM and PL grafts is important during DB ACL reconstruction.
A recent randomized clinical trial (RCT) study in our department investigated this issue in more detail. Ninety patients who underwent primary DB ACL reconstruction with an autologous ST tendon were prospectively included. PL graft fixation angles were randomly set as follows: (1) 0° of flexion (P0; n = 30), (2) 20° (P20; n = 30), and (3) 45° (P45; n = 30). The AM grafts in all groups were fixed at 20°. Initial tension was controlled using the Stress Equalization Graft Tensioning System (Conmed Linvatec, Largo, FL, USA). The pivot shift test resulted in the P0 and P20 groups being significantly better than those in the P45 group. KT measurements in the P20 group were better than those in the P45 group (mean: P0, 0.4 mm; P20, 0.3 mm; P45, 1.3 mm), and more patients developed graft failure (KT measurement ≥ 4 mm) in the P45 group.10) The graft tension patterns of the three fixation methods showed an equivocal pattern of the two grafts in the P45 group; thus, as AM tension increased, PL tension decreased during flexion. The normal equivocal pattern of the two bundles of a normal ACL was realized by P45 fixation. These results again suggests that it is important to equalize balance between the AM and PL grafts.
HOW MUCH IS A DB ACL RECONSTRUCTION WORTH DOING?
A comparative study between SB and DB reconstructions became necessary to convince ligament surgeons worldwide to continue performing DB ACL reconstructions. Our first RCT was planned and conducted.11) The femoral drill-hole position during DB reconstruction at the time of the 2002-2004 RCT was as follows: the AM and PL grafts were placed in a drill hole with an anterior border at resident's ridge. The femoral drill hole for the PL graft was offset deeply in the flexion position. The RCT results indicated that DB ACL reconstruction using a four-strand ST was superior to the SB technique with regard to anterior and rotational stability. Manual knee laxity testing revealed that negative Lachman and pivot-shift test results were more frequent in patients in the DB group than those in the SB group. The mean KT measurements were 2.4 mm in the SB group and 1.4 mm in the DB group (p < 0.05). However, the study failed to show any subjective difference. The statistical analysis did not reveal any differences in the modified International Knee Documentation Committee-categorized data between the two groups. The majority of meta-analysis studies on DB vs. SB ACL reconstruction have reached the same conclusion.12,13)
The mid- and long-term results of the RCT have been published.14) The study found that DB reconstruction maintains significant superiority for SB reconstruction regarding anterior and rotational stability during the 3- to 12-year follow-up. The Tegner score was also better in the DB group; however, there were no differences in the other subjective findings.
A few pieces of biomechanical evidence suggest superiority of DB reconstruction for rotational stability.15,16) Our recent in vivo biomechanical study using a triaxial accelerator (KiRA, Orthokey, Lewes, DE, USA) indicated that DB reconstruction better controls rotational instability than SB reconstruction during the pivot-shift test (under submission).
BETTER UNDERSTANDING OF NORMAL ACL ANATOMY TO SEEK A BETTER RECONSTRUCTION ROUTE
Previous knee observation studies have described anatomic placement for femoral tunnels. The position and area for each DB of the AM and PL portions of a natural ACL was described by its central structure with the surface membrane removed.17)
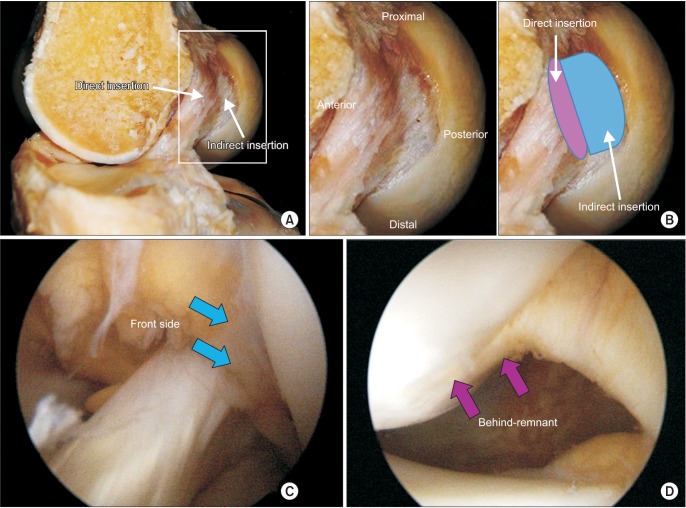
A macroscopically normal ACL consists of small, 1-mm diameter bundles, based on our observations. Detailed observation of the divided smaller bundles will lead to a better understanding of tunnel placement during anatomic ACL reconstruction. A normal cadaveric ACL was divided into AM and PL bundles and separated into ten 2-mm diameter bundles. Their attachment sites were marked with colored markers. The positional relationship between the femoral and tibial attachments of each small bundle was investigated. Small bundles constituting the ACL have a relatively layered arrangement between the two attachments. The results indicate that the tibial attachment form two patterns of oblique and transverse types. The vascular bundles were located in the center of the PL bundle, suggesting that tibial attachment of the PL bundle is in a rather posteromedial portion of the tibial fossa.18) A radiographic assessment combined with the anatomic landmarks during surgery suggested that the drill guide for tibial drill hole placement should not be put over the D-point laterally (Fig. 2).
Fig. 2. Tibial drill hole placement: anatomic landmarks and radiographic findings. Guidewires should not be placed over the D-point laterally.
Direct or indirect insertion of the ACL remains controversial. Iwahashi et al.19) investigated direct and indirect insertion of the femoral ACL histologically using embalmed cadaveric knees. They quantitatively measured the direct femoral insertion area using a three-dimensional (3D) volume-rendered (VR) computed tomography (CT) model. A meticulous histological analysis and the 3D VR CT model showed that direct insertion of the ACL coincided with a crescent-shaped hollow just behind the linear bony ridge. Sasaki et al.20) observed the femoral insertion of the ACL macroscopically, histologically, and immunohistologically using embalmed cadaveric knees. They reported the variety of femoral insertion methods for the ACL and described that the insertion area was relatively wide and separated from the posterior cartilage. They concluded that femoral ACL insertion observed macroscopically corresponded to direct insertion observed microscopically. The posterior portion behind the lateral intercondylar posterior ridge was the indirect insertion microscopically and appeared membrane-like macroscopically. Mochizuki et al.21) measured the direct (fibrous) and indirect (membranous) attachment areas separately as 50.8 ± 12.6 m2 and 91.4 ± 23.7 m2, respectively. The different opinions regarding direct and indirect femoral attachments of a normal ACL may be related to differences between young fresh ACLs and elderly cadaveric embalmed ACLs.
HAS DB ACL RECONSTRUCTION IMPROVED?
DB reconstruction using four-strand ST reconstruction has been consistently performed for 20 years. Knee stability outcomes from November 1994 to December 2008 were compared by dividing patients who were operated on at the university hospital by the author into three periods of from 11/1/1994 to 10/1/2000, from 11/1/2002 to 7/1/2004, and from 1/1/2006 to 12/31/2008 based on changing creation of the tibial and femoral tunnels.Table 1 shows the significant improvement in stability over time period. However, no evidence indicated that the "anatomic" DB procedure was superior to "isometric" or "non-anatomic" procedures and we have not found any either. Only a few comparative studies concluded that the anatomic DB procedure is superior to the isometric or non-anatomic procedures. The position of the tibial tunnel has made no difference.
Table 1. Has Double-Bundle Anterior Cruciate Ligament Reconstruction Improved?
| Variable | 1994.11-2000.10 (n=46) | 2002.11-2004.07 (n=44) | 2006.01-2008.12 (n=71) |
|---|---|---|---|
| Lachman test | A41 B04 C01 D0 | A41 B03 C0 D0 | A68 B03 C0 D0 |
| Anterior drawer test | A40 B02 C04 D0 | A39 B05 C0 D0 | A64 B07 C0 D0 |
| Pivot-shit test | A39 B05 C02 D0 | A42 B02 C0 D0 | A59 B12 C0 D0 |
| KT measurements* (mm, mean±SD) | 1.9±1.8 | 1.6±1.4 | 1.1±1.3 |
| Tunnel replacement | |||
| Femoral | AM, PL: high | AM, PL: low | AM, PL: low |
| Tibial | Posterior | Posterior | Anterior |
SD, standard deviation; AM, anteromedial; PL, posterolateral.
*Differences of anterior laxity between the injured and uninjured knees measured by the KT-1000 arthrometer.
REMNANT-PRESERVING ACL RECONSTRUCTION FROM 1990 TO PRESENT
The ACL remnant has been preserved, at least at the tibial attachment point, as a landmark for the tibial tunnel since 1989 when medial hamstring tendon ACL reconstruction started in our hospital. Remnant-preserving procedures have been practiced along with the technical improvements and the significant advantages of remnant-preserving procedures.
However, the meaning of ACL remnant volume itself has not been well investigated. Therefore, the background of remnant volume was investigated retrospectively. Eighty-eight patients underwent 105 unilateral DB anatomic ACL reconstructions between 2006 and 2008 and were followed up for ≥ 24 months and preoperative knee laxity was evaluated under anesthesia. Postoperative outcomes were evaluated based on knee extension and flexion strength, manual laxity tests, KT measurements, etc. Overall knee condition and sports performance were evaluated with the Lysholm Knee Score and a subjective rating scale. Then, the patients were divided into three subgroups based on remnant volume (remnant volume: ≤ 30%, 35%-55%, and ≥ 60%). The evaluation was performed and analyzed statistically among the three subgroups. Preoperative laxity tests showed a weak correlation with ACL remnant volume. Postoperative knee stability also had a weak correlation with ACL remnant volume. The statistical analyses revealed differences among the three groups regarding age at surgery, preoperative period, number giving-way, and preoperative KT measurements. Significant differences in the Lachman test, KT measurements, Lysholm knee scale, and subjective and sports performance recovery scores were observed postoperatively. These results suggest that the remnant volume is important as a background preoperative conditions, a predictor of operative outcome, and that a remnant-preserving surgery may not simply be better than a non-preserving technique with regard to a subjective evaluation and sports performance recovery.22)
Our results suggest that remnant-preserving DB ACL reconstruction is theoretically worth performing. However, a retrospective evaluation cannot conclude the significance of a technique because patient's backgrounds are different based on the remnant volume. Therefore, a prospective comparison between the preserving and non-preserving technique is necessary to confirm advantages of the remnant-preserving technique.
RECENT BEHIND-REMNANT APPROACH TO A REMNANT-PRESERVING DB ACL RECONSTRUCTION
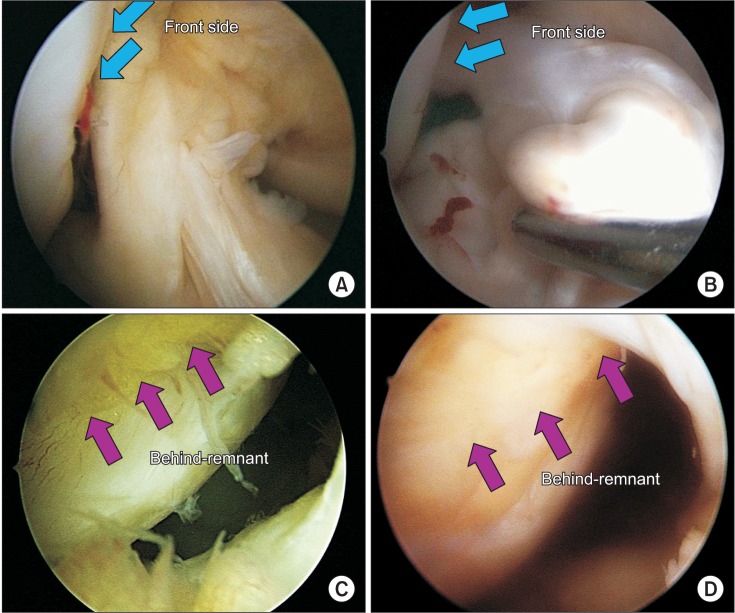
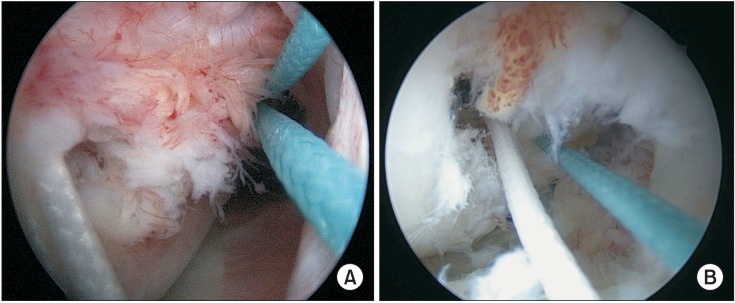
A new behind-remnant approach has been developed based on the superiority of the DB procedures and the theoretical advantages of the remnant-preserving technique and has good reproducibility. A normal ACL consists of direct and indirect insertions. These insertions cannot be separated from the articular surface with continuous extension (Fig. 3). The front side of an injured ACL, particularly the AM portion, is well preserved as a roof of the femoral remnant. The posterior part of the ACL remnant in the behind-remnant of an injured ACL is an indirect insertion but is usually scarred to some degree due to inflammation (Fig. 4).
Fig. 3. Normal anterior cruciate ligament (ACL) anatomy. (A) Direct insertion is bundle-like and exists on the lateral wall of the intercondylar notch. (B) Indirect insertion is membranous in cadaveric knees and its ligamentous function has not been well evaluated. (C) Arthroscopic observation of normal femoral ACL femoral attachment. A normal ACL consists of direct and indirect insertions. (D) The insertions cannot be separated with continuous extension from the articular surface.
Fig. 4. (A, B) The front side of an injured anterior cruciate ligament (ACL). Particularly, the anteromedial portion is rather preserved as a roof of the femoral attachment in two cases. Blue arrows indicate anterior border of the ACL. (C, D) Two cases of findings behind the remnant of an injured ACL. The posterior part of the ACL remnant is an indirect insertion, and it is ruptured and scarred with some inflammation in two cases. Pink arrows indicate scarred indirect insertion with synovial tissue.
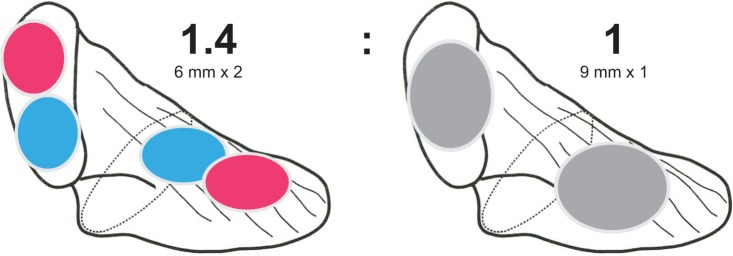
The procedures to create a femoral tunnel are described briefly. The behind-remnant space of the injured ACL is wide enough to be observed from its proximal to distal portions using a 30° scope. The expanded fibrous portion of the ACL remnant (indirect insertion) is covered with varying degrees of synovial cell proliferation depending on the case. Direct insertion of the proximal portion of the injured ACL is rather preserved as the roof of the behind-remnant space (Fig. 4). The original insertion of the PL bundle is usually less preserved than that of the AM bundle. It is important to assure 90° knee flexion when checking the correct rotational alignment and the direction of the remnant and knee joint. The femoral tunnel is created without removing remnant tissue in the behind-remnant approach. The AM tunnel guidewire was inserted at the posterior border of the direct insertion site of the remnant tissue with about a 5-mm margin from the articular surface proximally and posteriorly. The PL tunnel guidewire was inserted at the distal end and posterior border of the direct insertion site of the remnant tissue with about a 5-mm margin from the articular surface distally and posteriorly (Fig. 5).
Fig. 5. (A, B) Two cases of anteromedial and posterolateral femoral tunnels created behind the remnant.
The reproducibility of creating a tunnel using the new and standard procedures was compared on 3D-CT. Two approaches were practiced consecutively from 2010 to 2012 to create femoral tunnels during DB ACL reconstruction. One approach was the standard approach from the front in which the ACL remnant is peeled off from the attachment, and two guidewires were inserted based on anatomic bony landmarks (standard group). The other approach was the new behind-remnant approach in which the ACL remnant remains untouched and two guidewires are inserted at the posterior margin of the direct ACL insertion site (behind-remnant group). A total of 75 CT scans (36 in standard group and 39 in behind-remnant group) were analyzed. The position of the AM and PL femoral tunnels was expressed on a 3D-CT scan using the quadrant method described by Bernard et al.23) An unpaired t-test was used to determine the difference between the two groups regarding femoral tunnel position with significance set at a p-value < 0.05. Reproducibility of placing the femoral tunnel was assessed using the coefficient of variation (CV = standard deviation/average × 100) for each measurement between the two groups. The depth of the AM center was 24% ± 6% (mean and standard deviation) in the standard group and 22% ± 5% in the behind-remnant group. The height of the AM tunnel center was 22% ± 8% in the standard group and 31% ± 8% in the behind-remnant group. The depth of the PL tunnel center was 32% ± 6% in the standard group and 35% ± 5% in the behind-remnant group. The height of the PL tunnel center was 47% ± 9% in the standard group and 55% ± 7% in the behind-remnant group. The AM and PL femoral tunnels in both groups were created within the normal anatomic footprint of previous studies. The behind-remnant approach created significantly lower femoral tunnel for both the AM and PL tunnels. The depth of the AM and PL tunnels was not significantly different between the two groups. Every CV for tunnel placement was smaller in the behind-remnant group than that in the standard group. The reproducibility of the behind-remnant technique was not inferior to that of the standard technique for creating a femoral tunnel based on CV.24)
The new behind-remnant procedure may be technically demanding at the beginning, but it is simple, anatomic, and reproducible as a remnant-preserving ACL reconstruction procedure. The transtibial, transportal, and outside-in techniques were performed by us. All features of the operative methods will be clarified using the behind-remnant approach in the near future.
DB reconstruction has theoretical advantages over SB reconstruction, based on our 20 years experience in DB reconstruction using a multi-strand hamstring tendon graft. Better stability is achieved following DB reconstruction compared with that after SB reconstruction; however, the subjective patient evaluation has not improved. Many things need to be done for patients. Remnant volume reflects the status of an ACL-injured knee. We hope that the behind-remnant approach for ACL reconstruction will become a standard technique.
ACKNOWLEDGEMENTS
The author thanks all doctors in the Joint Surgery and Sports Medicine Group and Department of Orthopaedic Surgery, Tokyo Medical and Dental University Hospital: Drs. Ichiro Sekiya, Toshifumi Watanabe, Tomoyuki Mochizuki, Hideyuki Koga, Masafumi Horie, Tomomasa Nakamura, and Koji Otabe for their dedicated effort to the team. The author also thanks Ms. Miyoko Ojima for her special dedication to data collection.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Muneta T, Sekiya I, Yagishita K, Ogiuchi T, Yamamoto H, Shinomiya K. Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy. 1999;15(6):618–624. doi: 10.1053/ar.1999.v15.0150611. [DOI] [PubMed] [Google Scholar]
- 2.Muneta T, Sekiya I, Ogiuchi T, Yagishita K, Yamamoto H, Shinomiya K. Effects of aggressive early rehabilitation on the outcome of anterior cruciate ligament reconstruction with multi-strand semitendinosus tendon. Int Orthop. 1998;22(6):352–356. doi: 10.1007/s002640050276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamamoto H, Ishibashi T, Muneta T, Furuya K, Mizuta T. Effusions after anterior cruciate ligament reconstruction using the ligament augmentation device. Arthroscopy. 1992;8(3):305–310. doi: 10.1016/0749-8063(92)90060-o. [DOI] [PubMed] [Google Scholar]
- 4.Muneta T, Sekiya I, Ogiuchi T, Yagishita K, Yamamoto H, Shinomiya K. Objective factors affecting overall subjective evaluation of recovery after anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 1998;8(5 Pt 1):283–289. doi: 10.1111/j.1600-0838.1998.tb00484.x. [DOI] [PubMed] [Google Scholar]
- 5.Hefzy MS, Grood ES, Noyes FR. Factors affecting the region of most isometric femoral attachments. Part II: the anterior cruciate ligament. Am J Sports Med. 1989;17(2):208–216. doi: 10.1177/036354658901700210. [DOI] [PubMed] [Google Scholar]
- 6.Yamazaki J, Muneta T, Koga H, et al. Radiographic description of femoral tunnel placement expressed as intercondylar clock time in double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(3):418–423. doi: 10.1007/s00167-010-1243-9. [DOI] [PubMed] [Google Scholar]
- 7.Howell SM, Clark JA, Farley TE. A rationale for predicting anterior cruciate graft impingement by the intercondylar roof: a magnetic resonance imaging study. Am J Sports Med. 1991;19(3):276–282. doi: 10.1177/036354659101900312. [DOI] [PubMed] [Google Scholar]
- 8.Muneta T, Koga H, Morito T, Yagishita K, Sekiya I. A retrospective study of the midterm outcome of two-bundle anterior cruciate ligament reconstruction using quadrupled semitendinosus tendon in comparison with one-bundle reconstruction. Arthroscopy. 2006;22(3):252–258. doi: 10.1016/j.arthro.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Muneta T, Koga H, Ju YJ, Yagishita K, Sekiya I. Effects of different initial bundle tensioning strategies on the outcome of double-bundle ACL reconstruction: a cohort study. Sports Med Arthrosc Rehabil Ther Technol. 2011;3(1):15. doi: 10.1186/1758-2555-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koga H, Muneta T, Yagishita K, et al. Effect of posterolateral bundle graft fixation angles on clinical outcomes in double-bundle anterior cruciate ligament reconstruction: a randomized controlled trial. Am J Sports Med. 2015 Feb 2; doi: 10.1177/0363546514567069. [Epub]. http://dx.doi.org/10.1177/0363546514567069. [DOI] [PubMed] [Google Scholar]
- 11.Muneta T, Koga H, Mochizuki T, et al. A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy. 2007;23(6):618–628. doi: 10.1016/j.arthro.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Tiamklang T, Sumanont S, Foocharoen T, Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2012;11:CD008413. doi: 10.1002/14651858.CD008413.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu M, Gao S, Zeng C, et al. Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trials. Arthroscopy. 2013;29(2):357–365. doi: 10.1016/j.arthro.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 14.Koga H, Muneta T, Yagishita K, et al. Mid- to long-term results of single-bundle versus double-bundle anterior cruciate ligament reconstruction: randomized controlled trial. Arthroscopy. 2015;31(1):69–76. doi: 10.1016/j.arthro.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 15.Araki D, Kuroda R, Kubo S, et al. A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop. 2011;35(3):439–446. doi: 10.1007/s00264-010-1110-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hemmerich A, van der Merwe W, Batterham M, Vaughan CL. Knee rotational laxity in a randomized comparison of single- versus double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(1):48–56. doi: 10.1177/0363546510379333. [DOI] [PubMed] [Google Scholar]
- 17.Mochizuki T, Muneta T, Nagase T, Shirasawa S, Akita KI, Sekiya I. Cadaveric knee observation study for describing anatomic femoral tunnel placement for two-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2006;22(4):356–361. doi: 10.1016/j.arthro.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 18.Hara K, Mochizuki T, Sekiya I, Yamaguchi K, Akita K, Muneta T. Anatomy of normal human anterior cruciate ligament attachments evaluated by divided small bundles. Am J Sports Med. 2009;37(12):2386–2391. doi: 10.1177/0363546509340404. [DOI] [PubMed] [Google Scholar]
- 19.Iwahashi T, Shino K, Nakata K, et al. Direct anterior cruciate ligament insertion to the femur assessed by histology and 3-dimensional volume-rendered computed tomography. Arthroscopy. 2010;26(9 Suppl):S13–S20. doi: 10.1016/j.arthro.2010.01.023. [DOI] [PubMed] [Google Scholar]
- 20.Sasaki N, Ishibashi Y, Tsuda E, et al. The femoral insertion of the anterior cruciate ligament: discrepancy between macroscopic and histological observations. Arthroscopy. 2012;28(8):1135–1146. doi: 10.1016/j.arthro.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 21.Mochizuki T, Fujishiro H, Nimura A, et al. Anatomic and histologic analysis of the mid-substance and fan-like extension fibres of the anterior cruciate ligament during knee motion, with special reference to the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2014;22(2):336–344. doi: 10.1007/s00167-013-2404-4. [DOI] [PubMed] [Google Scholar]
- 22.Muneta T, Koga H, Ju YJ, Horie M, Nakamura T, Sekiya I. Remnant volume of anterior cruciate ligament correlates preoperative patients' status and postoperative outcome. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):906–913. doi: 10.1007/s00167-012-2023-5. [DOI] [PubMed] [Google Scholar]
- 23.Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL: radiographic quadrant method. Am J Knee Surg. 1997;10(1):14–21. [PubMed] [Google Scholar]
- 24.Muneta T, Koga H, Nakamura T, et al. A new behind-remnant approach for remnant-preserving double-bundle anterior cruciate ligament reconstruction compared with a standard approach. Knee Surg Sports Traumatol Arthrosc. 2014 Sep 11; doi: 10.1007/s00167-014-3300-2. [Epub]. http://dx.doi.org/10.1007/s00167-014-3300-2. [DOI] [PubMed] [Google Scholar]