Abstract
Background
Postoperative pain relief can be achieved with various modalities. However, there are only few reports that have analyzed postoperative analgesic techniques in total hip arthroplasty patients. The aim of this retrospective study was to compare the postoperative outcomes of three different analgesic techniques after total hip arthroplasty.
Methods
We retrospectively reviewed the influence of three analgesic techniques on postoperative rehabilitation after total hip arthroplasty in 90 patients divided into three groups (n = 30 patients per group). Postoperative analgesia consisted of continuous epidural analgesia (Epi group), patient-controlled analgesia with morphine (PCA group), or a continuous femoral nerve block (CFNB group). We measured the following parameters relating to postoperative outcome: visual analog scale scores, the use of supplemental analgesia, side effects, length of the hospital stay, plasma D-dimer levels, and the Harris hip score.
Results
Each group had low pain scores with no significant differences between the groups. The PCA group had a lower frequency of supplemental analgesia use compared to the Epi and CFNB groups. Side effects (nausea/vomiting, inappetence) and day 7 D-dimer levels were significantly lower in the CFNB group (p < 0.05). There were no significant differences between the groups in terms of the length of the hospital stay or the Harris hip score.
Conclusions
Although there were no clinically significant differences in outcomes between the three groups, the CFNB provided good pain relief which was equal to that of the other analgesics with fewer side effects and lower D-dimer levels in hospitalized patients following total hip arthroplasty.
Keywords: Nerve block, Epidural anesthesia, Morphine, Total hip arthroplasty
Total hip arthroplasty (THA) is the primary orthopaedic surgical procedure used to alleviate hip pain due to degenerative diseases and improve quality of life. However, early physical therapy following THA can be hindered by postoperative pain. Postoperative pain relief after joint surgery can be achieved with various modalities such as patient-controlled analgesia (PCA) with morphine, epidural analgesia (Epi), and lumbar plexus and/or sciatic blocks.1,2,3,4,5) Each of these analgesic options has advantages and disadvantages. The advantages of PCA are fewer technical problems, and uniform and sustained analgesia with autonomy.6,7) The advantages of Epi are based on the associated improved postoperative analgesia, and a reduction in blood loss during surgery.1) Although both PCA and continuous Epi provide sufficient pain relief, they are associated with multiple side effects, including arterial hypotension, respiratory depression, nausea/vomiting, and enuresis.5) Continuous femoral nerve block (CFNB) after total knee arthroplasty (TKA) is one of the more popular types of analgesia with fewer side effects associated with the use of morphine or fentanyl.1,5) On the other hand, there are a few studies reporting on good outcomes using CFNB after THA.2,5,8) The effects of CFNB on immediate postoperative outcome in patients undergoing THA have not been fully evaluated.
Deep venous thrombosis (DVT) is a common postoperative complication that can cause significant morbidity and mortality after orthopaedic surgery, especially THA and TKA.9,10) D-dimer is a degradation product of cross-linked fibrin; plasma levels increase after the cleavage of thrombi by activated plasmin and have been suggested to be a useful marker for the diagnosis of DVT.11,12) There are few reports comparing the influence of different postoperative analgesia techniques on patient outcomes, including D-dimer levels, after THA.
The aim of the present study was to compare pain relief with continuous Epi, PCA with morphine, and continuous three-in-one femoral nerve block on postoperative outcomes, including D-dimer levels, after THA.
METHODS
We retrospectively reviewed and analyzed the clinical outcomes of three postoperative analgesia techniques after THA. We initially included110 patients (14 males and 96 females) who were admitted to Okayama Medical Center with hip pain and scheduled for THA under general anesthesia. Patients with any of the following criteria were excluded: local infection, cemented THA, revision THA, preoperative DVT, renal failure, bleeding tendency due to anticoagulant therapy, or allergy to local anesthetics or opioids. We obtained informed consent from patient before surgery and ethical approval was obtained from the Institutional Review Board. Ninety patients (14 males and 76 females; mean age, 68 years; range, 31 to 86 years) were included in this study. Preoperative comorbidity was analyzed according to the comorbidity index.13)
All patients in this study had been operated on by the three experienced hip surgeons. The direct-lateral (modified Hardinge) approach was used in all patients. In this study, we used the cementless implants for THA (Summit, DePuy, Warsaw, IN, USA). Anesthesiologists instituted one of the following analgesic modalities: continuous Epi group (n = 30), PCA with morphine (PCA group, n = 30), or a CFNB group (n = 30) (Table 1). On postoperative day 1, all patients in the PCA and CFNB groups started fondaparinux (2.5 mg/day), which was continued for 14 days. In the Epi group, the first fondaparinux injection was administered 2 hours after removal of the epidural catheter on postoperative day 2. On postoperative day 1, all patients began a regimen of movement and strengthening exercises; they were encouraged to complete full weight-bearing exercises on postoperative day 2. On postoperative day 7, all patients underwent contrast-enhanced computed tomography (CT) to rule out DVT and/or pulmonary embolism (PE).
Table 1. Patient Background.
| Variable | Epi (n = 30) |
PCA (n = 30) |
CFNB (n = 30) |
p-value |
|---|---|---|---|---|
| Age (yr) | 64 ± 10.4 | 66.6 ± 12.7 | 68 ± 11.0 | 0.53 |
| Female | 23 | 26 | 26 | 0.63 |
| Body mass index (kg/m2) | 23.4 ± 3.8 | 24.4 ± 4.1 | 23.4 ± 4.2 | 0.68 |
| Disease | ||||
| Osteoarthritis | 25 | 27 | 25 | |
| Rheumatoid arthritis | 1 | 1 | 1 | |
| ANFH | 3 | 1 | 3 | |
| Femoral neck fracture | 1 | 1 | 1 | |
| Comorbidity index (point) | 2.7 ± 1.7 | 3.0 ± 2.2 | 3.1 ± 1.0 | 0.64 |
| Harris hip score (point) | 36.7 ± 13.3 | 37.8 ± 13.2 | 35 ± 19.0 | 0.37 |
| Operation time (min) | 87.1 ± 22.0 | 87.8 ± 20.6 | 81.8 ± 18.6 | 0.53 |
| Bleeding (mL) | 262 ± 147 | 233 ± 153 | 207 ± 127 | 0.42 |
Values are presented as mean ± standard deviation.
Epi: epidural analgesia, PCA: patient-controlled analgesia, CFNB: continuous femoral nerve block, ANFH: avascular necrosis of the femoral head.
In the Epi group, Epi was administered before general anesthesia at the level of L2-3 or L3-4. An 18-gauge (G) catheter (Perifix, B-Brown, Tokyo, Japan) was threaded 4 to 5 cm into the epidural space. After a negative test, a dose of 0.2% ropivacaine (2 mg/mL) with 0.5 mg of fentanyl (4.5 × 10-3 mg/mL) was injected at a rate of 2-4 mL/hr postoperatively; epidural fentanyl was continued for 48 hours, and the epidural catheter was removed on postoperative day 2.
In the PCA group, each patient was educated about the use of PCA. All patients were provided with PCA devices supplying 1.0 mg/hr of morphine at a demand dose of 1.0 mg and a lockout interval of 20 minutes. The patients were encouraged to take a bolus as often as needed.
In the CFNB group, a continuous 3-in-1 block was administered following the induction of general anesthesia according to the method described by Winnie et al.14) The femoral artery was located below the inguinal ligament, and an 18-G needle (1.3 × 50 mm, Contiplex, B-Braun) connected to a nerve stimulator (Stimuplex HNS12, B-Braun) was inserted just lateral to the artery via echography (MICROMAXX, SonoSite). The femoral nerve was accurately identified by eliciting contractions of the quadriceps with minimal stimulator settings (frequency, 2 Hz; current, 0.5 mA).15) Using the Seldinger technique, a20-G catheter (0.85 × 1,000 mm, Contiplex, B-Braun) was placed 10-15 cm into the psoas compartment, secured in place with Steri-strips (3M Health Care, Tokyo, Japan), and covered with a transparent dressing (Tegaderm, 3M Health Care). After a negative aspiration test for blood, 0.2% ropivacaine (2 mg/mL) was injected at a rate of 4 mL/hr postoperatively.
Patients with intolerable pain were given loxoprofen sodium (60 mg) by mouth up to every 6 hours. If the pain persisted after 30 minutes, a diclofenac sodium suppository (25 mg) was administered. The patient's pain intensity at rest was self-assessed using a visual analog scale (VAS) at 24 hours postoperatively. The VAS for pain self-assessment is a widely used, valid, and reliable tool to measure pain intensity.16) A 100-mm VAS was employed, and patients could rate pain intensity from no pain (0 mm) to unbearable pain (100 mm). Metoclopramide hydrochloride was used to treat nausea and vomiting. Clinical severity was assessed using the Harris hip score (HHS) on postoperative day 10.17)
Food intake, use of supplemental analgesia, side effects, and the length of the hospital stay were recorded for each group. Peripheral blood samples were obtained from all patients preoperatively and on days 1, 3, and 7. All samples were analyzed within 1 hour of being obtained. The D-dimer level was determined at each time-point and used to assess coagulation and fibrinolytic factors.
Statistical Analysis
All data were normally distributed and are expressed as means with standard deviation. Differences between groups were compared using a one-way analysis of variance (ANOVA) with the Bonferroni post hoc test. Fischer's exact test was used to compare differences in the gender ratio and the side effects between the three groups. All differences were considered statistically significant at a p-value < 0.05.
A pilot study was carried out on ten patients in each group. As a result of the pilot study, the mean D-dimer levels (by postoperative day 7) were 6.5 g/mL in the Epi group, 6.6 g/mL in the PCA group, and 4.4 µg/mL in the CFNB group, with a standard deviation of 3. Based on the effect size in this pilot study, a power calculation for a trial (effect size, 0.34; α, 0.05; power, 0.8) suggest that 29 patients would be needed in each group.
RESULTS
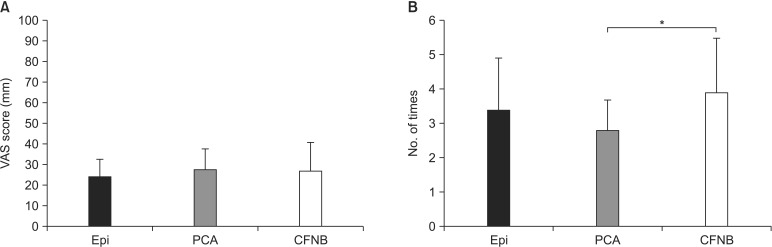
No significant differences were identified in the population data (race, age, gender ratio, body mass index, disease, and comorbidity index), preoperative HHS, operation time, or bleeding between the three groups (Table 1). The VAS score on postoperative day 1 did not significantly differ between the groups (p = 0.72) (Fig. 1A). The amount of loxoprofen sodium hydrate and diclofenac sodium suppositories used by the CFNB group were significantly greater than that used by the PCA group (p < 0.05) (Fig. 1B).
Fig. 1. (A) VAS for each group at 24 hours postoperatively. The VAS scores were not significantly different among the three groups. (B) Additional analgesic treatment was given to each of the three groups for two days after surgery. Values are presented as mean ± standard deviation. VAS: visual analog scale, Epi: epidural analgesia, PCA: patient-controlled analgesia, CFNB: continuous femoral nerve block. *p < 0.05.
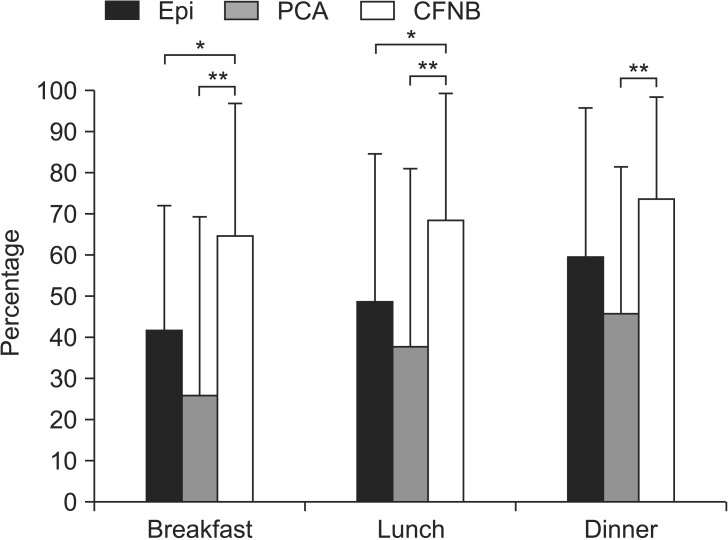
Seven patients in the Epi group, eight in the PCA group, and one in the CFNB group developed nausea and/or vomiting after THA (p < 0.05). Patients with nausea were unable to begin movement and strengthening exercises on postoperative day 1. An ANOVA test showed that there were significant differences in the mean amount of food intake on postoperative day 1 between the three groups (p < 0.05). The amount of food intake on postoperative day 1 was significantly greater in the CFNB group (70% ± 32%) relative to the Epi (50% ± 41%, p < 0.05) and PCA groups (37% ± 34%, p < 0.01). Food consumption during breakfast and lunch was significantly greater in the CFNB group relative to the Epi group (p < 0.05), whereas food consumption during all meals (breakfast, lunch, and dinner) was significantly greater in the CFNB group relative to the PCA group (p < 0.01) (Fig. 2). The mean hospital stay, including postoperative rehabilitation, was 25.3 ± 5.1, 23.3 ± 4.6, and 23 ± 3.1 days for the Epi, PCA, and CFNB groups, respectively; there was no significant difference in the length of the hospital stay between the three groups (p = 0.17).
Fig. 2. Food intake of the three groups on postoperative day 1. Values are presented as mean ± standard deviation. Epi: epidural analgesia, PCA: patient-controlled analgesia, CFNB: continuous femoral nerve block. *p < 0.05. **p < 0.01.
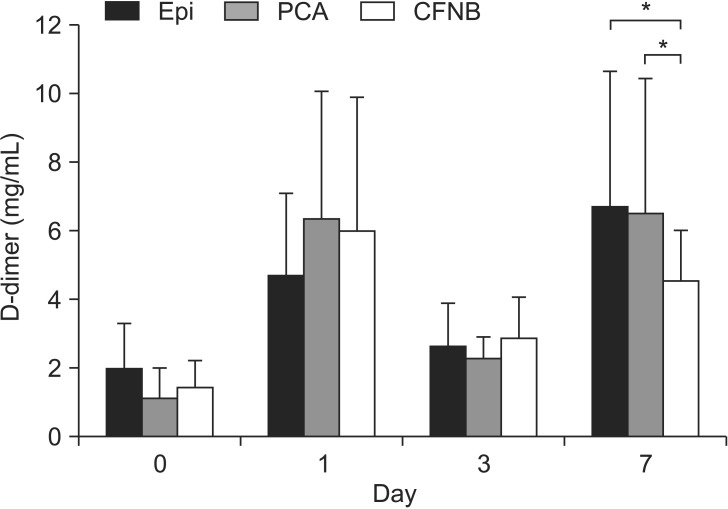
There were no significant differences in D-dimer levels between the three groups, except for on day 7, when the mean D-dimer level was significantly lower in the CFNB group (4.5 ± 1.5 µg/mL) compared with the Epi (6.7 ± 4.0 µg/mL) and PCA (6.4 ± 4.0 µg/mL) groups (p < 0.05) (Fig. 3). On postoperative day 7, all patients underwent contrast-enhanced CT to rule out DVT and/or PE. DVT was identified by contrast-enhanced CT in two of 30 patients (6.7%) in both the Epi and PCA groups. No patients with DVT were identified in the CFNB group. There was not a significant difference in the incidence of DVT and/or PE as detected by contrast-enhanced CT (p = 0.54). There was no significant difference in the HHS on postoperative day 10 between the groups (p = 0.10).
Fig. 3. D-dimer levels preoperatively (day 0) and on postoperative days 1, 3, and 7. Values are presented as mean ± standard deviation. Epi: epidural analgesia, PCA: patient-controlled analgesia, CFNB: continuous femoral nerve block. *p < 0.05.
DISCUSSION
Postoperative pain control after THA enables patients to achieve earlier hip mobilization and restoration of function. Compared with PCA and continual Epi, CFNB provides good pain relief and is associated with fewer side effects such as nausea/vomiting, hematomas, arterial hypotension, and drowsiness.2,8) In our study, a significant number of patients in the Epi and PCA groups developed nausea and/or vomiting, which resulted in poor appetites and prevented these patients from starting postoperative rehabilitation on the day after surgery. We injected 0.2% ropivacaine (2 mg/mL) with 0.5 mg of fentanyl (4.5 × 10-3 mg/mL) in the Epi group. A high incidence of nausea/vomiting in the Epi and PCA groups might be influenced by the use of fentanyl or morphine. Different results might be obtained if studied without fentanyl in the Epi group. However, because a pure local anesthetic may provide dense sensory and motor blockade, a combination of an opioid and a local anesthetic is recommended.6)
Postoperative analgesics promote early recovery with a lower incidence of DVT/PE.18) Although no significant difference was found in the rate of DVT/PE between the three groups in this study, D-dimer levels were significantly higher in both the Epi and PCA groups compared with the CFNB group on postoperative day 7D-dimer is a protein fragment formed following the degradation of a fibrin clot; it is a useful indicator of several conditions, including venous thromboembolism, disseminated intravascular coagulation, and cardiovascular disease.19) The higher D-dimer levels in the Epi and PCA groups in our study might have been affected by inadequate fluid and dietary intake due to postoperative nausea and vomiting. Delayed rehabilitation, including active exercise and walking, may have also contributed to the increase in D-dimer levels in these groups. Accordingly, the lower D-dimer levels in the CFNB group might have been influenced by early mobilization, rehabilitation, and a lower incidence of side effects.
However, it might not be valid to compare D-dimer levels of the Epi group with those of the PCA and CFNB groups, since patients in the Epi group did not receive chemical anticoagulation for 2 days in order to reduce the risk of bleeding. In patients receiving Epi, the risk of clinically significant bleeding increases in response to preventive measures against DVT/PE. According to the regional anesthesia and anticoagulation guidelines formulated by the American Society of Regional Anesthesia and Pain Medicine,20) it is important to prevent epidural hematomas,21) which is a potential disadvantage of this modality. To minimize the risk of hematomas, we cannot use fondaparinux or other anticoagulants in a patient under Epi. If it is necessary to remove an epidural catheter earlier than desired in order to use an antithrombotic agent, the use of nonsteroidal anti-inflammatory drugs can be increased. In general, CFNB may be a more advantageous technique in patients receiving anticoagulants.
A potential disadvantage of CFNB is a higher risk of falling. Because patients have an increased risk of falling as a consequence of persistent quadriceps muscle weakness after receiving high doses of this type of analgesia, both the density and flow of a CFNB should be controlled in accordance with its effect.22) Although we did not use any knee immobilizers in this study, no patients in the CFNB group complained of postoperative quadriceps muscle weakness. In past studies, among patients receiving ropivacaine 0.2% at 8 mL/hr, 42% to 43% experienced quadriceps femoris weakness,23) which may have resulted in an increase number of falls. Ilfeld et al.24) recommended that if patients receiving ropivacaine 0.2% at 6 mL/hr experienced quadriceps femoris weakness, the basal administration rate should be reduced by half (to 3 mL/hr). Based on our experience, we consider a ropivacaine (0.2%) rate of 4 mL/hr to be appropriate in minimizing the risk of falling after THA. A variety of techniques, including continuous Epi, PCA, and CFNB have been used and compared in terms of their efficacy and postoperative rehabilitation outcomes in TKA patients.5,25) However, only a few reports have analyzed these three analgesic techniques in THA patients.2,8) In this study, we integrated the use of ultrasound-guided CFNB and compared it with the postoperative outcomes of these techniques after THA. There was no significant difference in the VAS score between the groups, and each group had good pain relief, which is in accordance with a previous report.5) Although the amount of loxoprofen sodium hydrate administered in the PCA group was significantly lower than that administered in the CFNB group (p < 0.05), this difference might be due to the ability of the PCA group to self-administer additional boluses of morphine. However, when large amounts of loxoprofen sodium hydrate are given, side effects may develop. Additionally, the frequent dosing of loxoprofen sodium hydrate increases the duties of the floor nurse.
Although CFNB enables selective anesthesia at the surgical site, the peripheral nerves have a complicated distribution and ectopia can make it more challenging. Although permanent neurological injury after regional anesthesia is rare in contemporary anesthetic practice, the rate of neurological complications after CFNB is higher than epidural anesthesia.26) The use of supplemental devices enabled us to place the local nerve block with more precision in this study. We utilized echography, which is widely used owing to its portability and functionality. In the current study, there was no neurological injury after CFNB. The resulting enhanced echographic image quality and concurrent use of an electrostimulator enabled us to accurately identify the nerve and its innervation zone.
This study has some limitations and weakness. Firstly, the present study's retrospective nature is a weakness. A prospective, randomized, controlled study should be conducted to eliminate selection bias and obtain more consolidated results. Secondly, the sample size is relatively small, which makes explaining the effect of three different postoperative analgesia techniques difficult. To validate our findings, future studies with large sample sizes and a prospective design are needed to further define the efficacy of CFNB. Thirdly, we performed THA under general anesthesia in this study. However, some clinical studies support a transition to spinal conduction blockade for intraoperative anesthetic management of orthopedic surgery. This technique has lower complications rate,27) including reduced blood loss28) and decreased incidence of DVT.29) It is possible that we might have obtained different outcomes if we had used intraoperative spinal anesthesia in this study. Moreover, in previous studies, the length of the hospital stay was shorter in patients who underwent TKA under spinal anesthesia compared with general anesthesia,27) making spinal anesthesia more cost-effective.30) In our study, there was no significant difference between the length of the hospital stay or the costs between the three groups because Japan's universal health insurance system keeps medical expenses relatively low for all patients, and patients tend to stay in the hospital until they complete their postoperative rehabilitation. Finally, all THAs in this study were performed through the Hardinge approach. It is not possible to perform CFNB using the anterior approach, including the direct anterior approach because of the skin incision adjacent to CFNB. Additionally, if studied in the patients undergoing THA via the posterolateral approach, dividing short rotators and quadratus femoris, a different outcome might be obtained.
Although there were no significant differences in postoperative HHS between the three groups in our study, postoperative CFNB use achieved good pain relief-equal to that of other analgesics-with fewer side effects in hospitalized patients following THA.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Chelly JE, Greger J, Gebhard R, et al. Continuous femoral blocks improve recovery and outcome of patients undergoing total knee arthroplasty. J Arthroplasty. 2001;16(4):436–445. doi: 10.1054/arth.2001.23622. [DOI] [PubMed] [Google Scholar]
- 2.Singelyn FJ, Ferrant T, Malisse MF, Joris D. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous femoral nerve sheath block on rehabilitation after unilateral total-hip arthroplasty. Reg Anesth Pain Med. 2005;30(5):452–457. doi: 10.1016/j.rapm.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Buckenmaier CC, 3rd, Xenos JS, Nilsen SM. Lumbar plexus block with perineural catheter and sciatic nerve block for total hip arthroplasty. J Arthroplasty. 2002;17(4):499–502. doi: 10.1054/arth.2002.32176. [DOI] [PubMed] [Google Scholar]
- 4.Chelly JE, Schilling D. Thromboprophylaxis and peripheral nerve blocks in patients undergoing joint arthroplasty. J Arthroplasty. 2008;23(3):350–354. doi: 10.1016/j.arth.2007.05.045. [DOI] [PubMed] [Google Scholar]
- 5.Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998;87(1):88–92. doi: 10.1097/00000539-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res. 2009;467(6):1418–1423. doi: 10.1007/s11999-009-0728-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sinatra RS, Torres J, Bustos AM. Pain management after major orthopaedic surgery: current strategies and new concepts. J Am Acad Orthop Surg. 2002;10(2):117–129. doi: 10.5435/00124635-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Singelyn FJ, Gouverneur JM. Postoperative analgesia after total hip arthroplasty: i.v. PCA with morphine, patient-controlled epidural analgesia, or continuous "3-in-1" block?: a prospective evaluation by our acute pain service in more than 1,300 patients. J Clin Anesth. 1999;11(7):550–554. doi: 10.1016/s0952-8180(99)00092-6. [DOI] [PubMed] [Google Scholar]
- 9.Niimi R, Hasegawa M, Shi DQ, Sudo A. The influence of fondaparinux on the diagnosis of postoperative deep vein thrombosis by soluble fibrin and D-dimer. Thromb Res. 2012;130(5):759–764. doi: 10.1016/j.thromres.2011.11.046. [DOI] [PubMed] [Google Scholar]
- 10.Piovella F, Wang CJ, Lu H, et al. Deep-vein thrombosis rates after major orthopedic surgery in Asia: an epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. J Thromb Haemost. 2005;3(12):2664–2670. doi: 10.1111/j.1538-7836.2005.01621.x. [DOI] [PubMed] [Google Scholar]
- 11.Yukizawa Y, Inaba Y, Watanabe S, et al. Association between venous thromboembolism and plasma levels of both soluble fibrin and plasminogen-activator inhibitor 1 in 170 patients undergoing total hip arthroplasty. Acta Orthop. 2012;83(1):14–21. doi: 10.3109/17453674.2011.652886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shiota N, Sato T, Nishida K, et al. Changes in LPIA D-dimer levels after total hip or knee arthroplasty relevant to deep-vein thrombosis diagnosed by bilateral ascending venography. J Orthop Sci. 2002;7(4):444–450. doi: 10.1007/s007760200077. [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 14.Winnie AP, Ramamurthy S, Durrani Z. The inguinal paravascular technic of lumbar plexus anesthesia: the "3-in-1 block". Anesth Analg. 1973;52(6):989–996. [PubMed] [Google Scholar]
- 15.Hunt KJ, Bourne MH, Mariani EM. Single-injection femoral and sciatic nerve blocks for pain control after total knee arthroplasty. J Arthroplasty. 2009;24(4):533–538. doi: 10.1016/j.arth.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Bellamy N, Kirwan J, Boers M, et al. Recommendations for a core set of outcome measures for future phase III clinical trials in knee, hip, and hand osteoarthritis: consensus development at OMERACT III. J Rheumatol. 1997;24(4):799–802. [PubMed] [Google Scholar]
- 17.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 18.Grass JA. The role of epidural anesthesia and analgesia in postoperative outcome. Anesthesiol Clin North America. 2000;18(2):407–428. doi: 10.1016/s0889-8537(05)70170-x. [DOI] [PubMed] [Google Scholar]
- 19.Lippi G, Franchini M, Targher G, Favaloro EJ. Help me, Doctor! My D-dimer is raised. Ann Med. 2008;40(8):594–605. doi: 10.1080/07853890802161015. [DOI] [PubMed] [Google Scholar]
- 20.Horlocker TT, Wedel DJ, Rowlingson JC, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Third Edition) Reg Anesth Pain Med. 2010;35(1):64–101. doi: 10.1097/aap.0b013e3181c15c70. [DOI] [PubMed] [Google Scholar]
- 21.Christie IW, McCabe S. Major complications of epidural analgesia after surgery: results of a six-year survey. Anaesthesia. 2007;62(4):335–341. doi: 10.1111/j.1365-2044.2007.04992.x. [DOI] [PubMed] [Google Scholar]
- 22.Kandasami M, Kinninmonth AW, Sarungi M, Baines J, Scott NB. Femoral nerve block for total knee replacement: a word of caution. Knee. 2009;16(2):98–100. doi: 10.1016/j.knee.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Ilfeld BM, Ball ST, Gearen PF, et al. Ambulatory continuous posterior lumbar plexus nerve blocks after hip arthroplasty: a dual-center, randomized, triple-masked, placebo-controlled trial. Anesthesiology. 2008;109(3):491–501. doi: 10.1097/ALN.0b013e318182a4a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ilfeld BM, Mariano ER, Madison SJ, et al. Continuous femoral versus posterior lumbar plexus nerve blocks for analgesia after hip arthroplasty: a randomized, controlled study. Anesth Analg. 2011;113(4):897–903. doi: 10.1213/ANE.0b013e318212495b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baker MW, Tullos HS, Bryan WJ, Oxspring H. The use of epidural morphine in patients undergoing total knee arthroplasty. J Arthroplasty. 1989;4(2):157–161. doi: 10.1016/s0883-5403(89)80069-5. [DOI] [PubMed] [Google Scholar]
- 26.Brull R, McCartney CJ, Chan VW, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg. 2007;104(4):965–974. doi: 10.1213/01.ane.0000258740.17193.ec. [DOI] [PubMed] [Google Scholar]
- 27.Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013;95(3):193–199. doi: 10.2106/JBJS.K.01682. [DOI] [PubMed] [Google Scholar]
- 28.Modig J. Regional anaesthesia and blood loss. Acta Anaesthesiol Scand Suppl. 1988;89:44–48. doi: 10.1111/j.1399-6576.1988.tb02842.x. [DOI] [PubMed] [Google Scholar]
- 29.Modig J, Malmberg P, Karlstrom G. Effect of epidural versus general anaesthesia on calf blood flow. Acta Anaesthesiol Scand. 1980;24(4):305–309. doi: 10.1111/j.1399-6576.1980.tb01553.x. [DOI] [PubMed] [Google Scholar]
- 30.Gonano C, Leitgeb U, Sitzwohl C, Ihra G, Weinstabl C, Kettner SC. Spinal versus general anesthesia for orthopedic surgery: anesthesia drug and supply costs. Anesth Analg. 2006;102(2):524–529. doi: 10.1213/01.ane.0000194292.81614.c6. [DOI] [PubMed] [Google Scholar]