Abstract
Background
In this study, we investigated the long-term clinical results and survival rate of minimally invasive unicompartmental knee arthroplasty (UKA) by collecting cases that had been implanted more than 10 years ago.
Methods
One hundred and twenty-eight patients (166 cases) who underwent Oxford phase 3 medial UKA using the minimally invasive surgery from January 2002 to December 2002 were selected. The mean age of the patients at the time of surgery was 61 years, and the duration of the follow-up was minimum 10 years. Clinical and radiographic assessments were performed using the Knee Society clinical rating system, and the survival analysis was done by the Kaplan-Meier method with 95% confidence interval (CI).
Results
The mean Knee Society knee and function scores improved significantly from 53.8 points (range, 25 to 70 points) and 56.1 points (range, 35 to 80 points) preoperatively to 85.4 points (range, 58 to 100 points) and 80.5 points (range, 50 to 100 points) at 10-year follow-up, respectively (p < 0.001). Failures following the UKA occurred in 16 cases (9.6%), and the mean time of the occurrence of the failure was 6.2 years after the surgery. The 10-year survival rate was 90.5% (95% CI, 85.9 to 95.0) when failure was defined as all the reoperations, whereas the 10-year survival rate was 93.4% (95% CI, 89.6 to 97.1) when the cases in which only revision total knee arthroplasty was defined as failure.
Conclusions
The results of this study show outstanding functions of the knee joint and satisfactory 10-year survival rate after minimally invasive UKA. Therefore, minimally invasive UKA could be a useful method in the treatment of osteoarthritis in one compartment of knee joint.
Keywords: Arthroplasty, Replacement, Knee, Minimally invasive, Survival rate
The results of unicompartmental knee arthroplasty (UKA) are unsatisfactory at the initial period of implementation owing to the inferior prosthetic design, suboptimal surgical technique, and poor patient selection. However, numerous outstanding results with the improvements in the functions of the knee joint and the survival rate of implants have been reported recently through accurate selection criteria, ongoing improvements in the prosthetic design and surgical technique.1,2,3) Although majority of reports have satisfactory results on the functions of knee joint after the UKA at the moment, diverse range of results are being reported on the survivorship of UKA depending on the indications, types of implants and surgeons, therefore leaving substantial controversy in long-term results of UKA.4,5,6) In particular, minimally invasive UKA, as one of the key factors that improved the clinical results and increased the usage of UKA since its first introduction in the latter part of the 1990's, has been reported to produce satisfactory alignment of implants and outstanding clinical results if surgery is performed accurately through minimally invasive surgery.7,8,9) However, there are not many reports of the long-term clinical results of minimally invasive UKA as the duration of implementation is still short, and in particular, the survival rate by collecting only the cases of follow-up with > 10 years are scarcely reported.4,8,10,11,12,13,14,15)
Accordingly, the authors attempted to evaluate the long-term clinical results including 10-year survival rate of minimally invasive UKA by the follow-up examination of the cases that has been continued for > 10 years since the operation.
METHODS
Medial UKA on 180 cases in 142 patients was performed over a period of 1 year after the first introduction of minimally invasive UKA from January 2002 to December 2002. The percentage of UKA in the knee replacement during the study period was 23% (180 UKA and 614 total knee arthroplasty [TKA]). Among these, 166 cases in 128 patients for whom the follow-up examination 10 years after the surgery was possible, with the exclusion of 14 cases including 10 cases of follow-up loss and 4 cases of death, were used as the subject. A total of 128 patients were composed of 5 males (6 cases) and 123 females (160 cases), with the mean age of 61 years (range, 45 to 84 years). All the preoperative diagnosis was osteoarthritis of the knee joint (Table 1).
Table 1. Demographics.
| Characteristic | Value |
|---|---|
| Research period | January 2002 to December 2002 |
| Case no. | 142 patients, 180 cases of UKA |
| Death/follow-up loss | 4/10 cases |
| Last follow-up (10 yr) | 128 patients, 166 cases |
| Gender (male:female) | 5:123 |
| Age (yr) | 61.8 (45-84) |
| Failure (%) | 16 (9.6) |
| Mean time to failure (mo) | 74 (35-118) |
| Treatment: simple bearing change | 5 (3.0) |
| Revision total knee arthroplasty | 11 (6.6) |
Values are presented as mean (range) or cases (%).
UKA: unicompartemental knee arthroplasty.
Inclusion and Exclusion Criteria
The major indications for UKA were medial compartment degenerative arthritis of the knee joint with normal function of the anterior/posterior cruciate ligament, ≤ 15° varus deformity, ≤ 15° flexion contracture, and 110° ≥ range of the knee motion.
The inflammatory disease of the knee joint, cases with ligament instability, and cases with any degenerative changes in the lateral compartment were contraindications of UKA. Moreover, the cases in which there was pain in the anterior portion of the knee joint while walking or climbing down the stairs along with degenerative changes in the patellofemoral joint were also excluded from being selected as the indication. However, medial UKA was performed regardless of the grade of degenerative changes in patellofemoral joint unless patellofemoral symptoms were present.
Implants and Surgical Technique
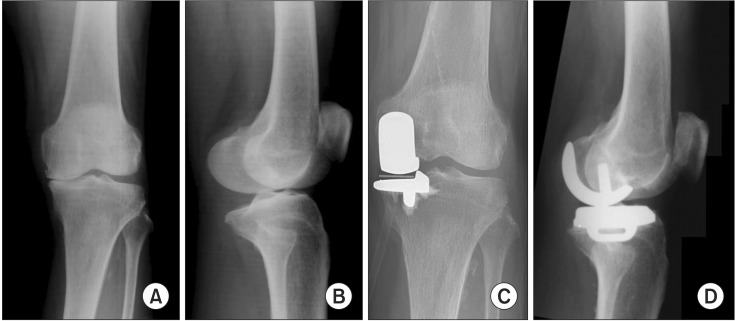
Oxford phase 3 implants (Biomet, Warsaw, IN, USA) were used in all the cases, and most of the cases were performed by two surgeons (KTK and SL) in Seoul Sacred Heart General Hospital. Minimally invasive surgery was performed using a short medial parapatellar approach. The medial tibial plateau was excised using the extramedullary tibial resection guide, and the posterior facet of the medial femoral condyle was excised using the femoral drill guide and femoral cutting block. After the insertion of the tibial template and femoral trial component, the flexion and extension gaps were measured using the feeler gauges. The flexion and extension gaps were equalized by the milling of the distal femoral condyle. After the insertion of the trial components, the stability of the joint and movement of the bearing through a full range of motion of the knee was checked. The tibial and femoral implants were fixed with antibiotic-impregnated cement, and a meniscal bearing was inserted between them (Fig. 1).16)
Fig. 1. (A, B) Preoperative radiographs of a 75-year-old woman show osteoarthritis of the medial compartment in the left knee. (C, D) The last follow-up radiographs show findings at more than 10 years after minimally invasive Oxford phase 3 unicompartmental knee arthroplasty.
Outcome Measures and Statistical Analysis
In all the cases, preoperative status was investigated by the prospective examination method, and the clinical assessment was performed through regularly scheduled follow-up examination after the surgery. Clinical and radiographic assessments were performed at month 3, 6, 9, and 12, and then annually after the surgery. The extent of the pain around the knee joint, range of motion of the knee joint, Knee Society knee and function scores of the patients were measured by the Knee Society clinical rating system.17) Radiographic assessment was performed through weight-bearing anteroposterior and lateral radiographs with the knee in full extension. The tibiofemoral angle was measured, and radiolucent line or loosening around the prosthesis and the progression of osteoarthritis to the lateral compartment was investigated. Periprosthetic radiolucent line was evaluated by the method of the Oxford group, in which the tibial prosthesis was divided into three areas, the medial, keel, and lateral zones.18) The thickness of the radiolucent line was measured in each area, and the mean thickness of the radiolucent line was calculated.
In cases which a part or all of the implant was removed or replaced by revision surgery during the follow-up were defined as a failure of UKA. Statistical analysis was performed using the paired t-test, and a p-value of < 0.05 was considered statistically significant. Survival analysis was confirmed by the Kaplan-Meier method including the death and lost to follow-up as censored with the 95% confidence interval (CI).
RESULTS
Clinical Results
In 150 cases (114 patients), by subtracting the 16 failures and 14 excluded cases (10 cases of follow-up loss and 4 cases of death) from the 180 cases, for whom the follow-up 10 years after the surgery was possible, the mean Knee Society knee score improved from 53.8 points (range, 25 to 70 points) preoperatively to 85.4 points (range, 58 to 100 points) at a 10-year follow-up, and the mean Knee Society function score improved from 56.1 points (range, 35 to 80 points) preoperatively to 80.5 points (range, 50 to 100 points) at 10-year follow-up. Both the Knee Society knee and function scores showed significant improvement under the final follow-up in comparison to the preoperative evaluation (p < 0.001). The mean range of the motion of the knee joint recovered from 128.6° (range, 110° to 135°) to 132.5° (range, 105° to 135°; p < 0.001) (Table 2).
Table 2. Clinical Results.
| Variable | Preoperative | Last follow-up | p-value* |
|---|---|---|---|
| Knee Society knee score | 53.8 ± 8.8 | 85.4 ± 9.2 | < 0.001 |
| Knee Society function score | 56.1 ± 10.0 | 80.5 ± 11.7 | < 0.001 |
| Range of knee motion (°) | 128.6 ± 7.9 | 132.5 ± 6.0 | < 0.001 |
| Tibiofemoral angle (°) | -0.2 ± 3.2 | 4.6 ± 2.6 | < 0.001 |
Values are presented as mean ± standard deviation.
*Paired t-test.
Radiographic Results
The tibiofemoral angle changed from the mean 0.2° of varus (7° of varus to 7° of valgus) to 4.6° of valgus (2° of varus to 11° of valgus) under the weight-bearing X-ray (p < 0.001) (Table 2). Non-progressive radiolucent lines were found in 31 cases (18.7%). All the radiolucent lines existed around the tibial component, and the mean thickness was 0.89 mm. As we defined the radiolucency > 2 mm of the thickness with the progression as a loosening, 4 femoral and 1 tibial components loosening were observed. There was no progression of the osteoarthritis to the lateral compartment that requires revision operation.
Failures
Failures following the UKA occurred in 16 cases in 14 patients out of a total of 166 cases (9.6%). Of the total of 14 patients, 1 was male (1 case), whereas 13 were female (15 cases), with the mean age of 67 years (range, 56 to 80 years). The time of occurrence of the failure ranged widely from 2 years and 11 months to 9 years and 10 months with the mean of 6 years and 2 months after the surgery, with 5 of the total of 16 cases (31%) occurring within 5 years after the surgery. The causes of the failure included 7 cases of simple dislocation of mobile-bearing, 4 cases of loosening of implant, 1 case of dislocation of mobile-bearing accompanied by loosening of implant, and 1 case of dislocation of mobile-bearing accompanied by the rupture of the medial collateral ligament (MCL). Moreover, there was 1 case of fracture of polyethylene bearing, 1 case of deep infection and 1 case of failure because of medial tibial condylar fracture (Table 3). Of the total of 16 cases of failures, 11 cases (69%) were treated with revision TKA, whereas 5 cases (31%) were treated with a simple change of mobile-bearing.
Table 3. Cause of Failure after Unicompartmental Knee Arthroplasty (2002.1-2002.12; 166 Cases).
| Complication | No. (%) |
|---|---|
| Bearing dislocation | 7 (4.2) |
| Bearing wear and breakage | 1 (0.6) |
| MCL rupture with bearing dislocation | 1 (0.6) |
| Stem loosening | |
| Femoral | 3 (1.8) |
| Femoral and tibial | 1 (0.6) |
| Stem loosening with bearing dislocation | 1 (0.6) |
| Tibial condylar fracture | 1 (0.6) |
| Infection | 1 (0.6) |
| Total (case) | 16 (9.6) |
MCL: medial collateral ligament.
Dislocation of mobile-bearing
Dislocation of mobile-bearing occurred in a total of 9 cases, and among these, there were 7 cases of simple dislocation, 1 case accompanied by the loosening of femoral and tibial implants, and 1 case accompanied by the rupture of MCL. Simple mobile-bearing dislocation cases showed lax MCL, however, no other apparent causes were observed occurring at a mean period of 6 years and 3 months following the surgery (3 years and 6 months to 9 years and 10 months). Three of the cases of simple dislocation of mobile-bearing were treated by a simple change using the thicker bearing (1 mm in 2 cases, 2 mm in 1 case). Four of the cases that needed > 3 mm thicker bearing were revised to TKA, because they had severe ligament laxity and could increase valgus deformity. The case of the mobile-bearing dislocation because of the rupture of MCL was treated by the means of repair of MCL and change of mobile-bearing.
Loosening of component
In a total of 4 cases, the loosening of the implant was detected under the radiographic images at the time of the follow-up examination, with 3 cases of the femoral component loosening and 1 case of both the femoral and tibial component loosening. Single loosening of the femoral component occurred after mean of 7 years of UKA (2 years and 11 months to 9 years), whereas the cases of the loosening of both the femoral and tibial implants occurred after 4 years and 10 months of the surgery. In all the cases of implant loosening, revision TKA was performed.
In one of the cases in which dislocation of mobile-bearing occurred, loosening of the femoral and tibial implants was detected intraoperatively while treating the dislocation of mobile-bearing that occurred after 6 years and 9 months of the surgery, although the loosening of the implant was not detected under the radiographic image at the time of the follow-up examination. This case was treated by means of revision TKA.
Infection
One case (0.6%) of failure occurred because of the infection at 5 years and 8 months after the surgery. After having been diagnosed with an acute hematogenous infection, two stage revision TKA was performed. There was no recurrence of the infection at the time of follow-up to 4 years after the second stage revision TKA.
Periprosthetic fracture
In one case, medial proximal tibial condylar fracture occurred around the tibial implant because of trauma from the collision at 5 years and 8 months following the surgery. The implant was revised by TKA using metal block as there was the intraoperative finding of the loosening of the tibial implant along with slight displacement of fracture.
Others
Wear and fracture of polyethylene bearing occurred in 1 case and was treated by changing the polyethylene bearing. No other failures due to the progression of arthritis into other compartment or ankylosis of the knee joint were observed.
Survival Rate of Implants
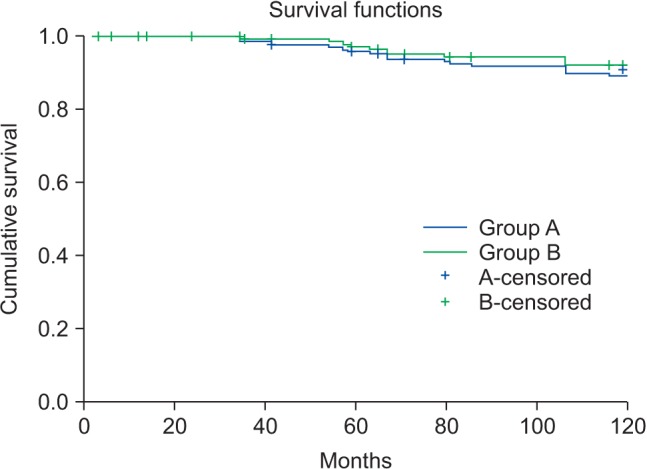
As the result of the measurement of the survival rate of implants, the 10-year Kaplan-Meier estimator of the cumulative survival rate of minimally invasive UKA was 90.5% (95% CI, 85.9 to 95.0) when failure was defined as all the reoperations including revision TKA and simple change of mobile-bearing, whereas the 10-year Kaplan-Meier estimator of cumulative survival rate was 93.4% (95% CI, 89.6 to 97.1) for the cases in which only revision TKA was defined as failure (Fig. 2).
Fig. 2. Kaplan-Meier survivorship analysis curve showing 10-year survival rate of minimally invasive unicompartmental knee arthroplasty of 90.5% (95% confidence interval [CI], 85.9 to 95.0) with failure for any reason as the end point (group A) and 93.4% (95% CI, 89.6 to 97.1) with the revision of total knee arthroplasty as the end point (group B).
DISCUSSION
Minimally invasive UKA was performed using the Oxford phase 3 implants and evaluated the long-term clinical results including 10-year survival rate of minimally invasive UKA by the follow-up examination of the cases that has been continued for > 10 years since the operation. In the present series, outstanding long-term clinical results including knee score, function score and range of knee motion were observed after minimally invasive UKA. Moreover, this study showed a 10-year survival rate of 90.5%.
Many authors have continuously reported from the early stage of the implementation of UKA that the outstanding results after UKA have been obtained including reduction in pain, recovery of the range of the knee motion, correction of the deformity, improvement in the knee score, function score, and level of satisfaction of the patients.2,3,4,19) Moreover, it has been reported that satisfactory arrangement of implant and outstanding clinical results can be obtained if surgery is performed accurately through minimally invasive incision.7,8,9) Current study was also able to confirm outstanding clinical results in terms of knee score, function score, and range of knee motion under the follow-up examination 10 years after minimally invasive UKA.
However, there have been numerous disputes on the longevity and survivorship of UKA. In the case of conventional UKA, although the survival rate was not good enough at the early period because of a high early failure rate, many authors reported a higher 10-year survival rate since 1998.20,21) Moreover, Egidy et al.1) reported an example of the maintenance over a period of 31 years following UKA. In many recent reports, 10-year survival rates of UKA have been reported in the range of 84% to 100%, thereby showing substantial differences in the survival rates depending on the types of the implants and surgeons.22,23,24) O'Rourke et al.5) reported long-term survival rates of 84% at 20 years and 72% at 25 years following UKA, and a correlation was observed between the revision rates and age. According to combined data from the Australian and Swedish Knee Registries, the revision rate following UKA significantly increases in younger age.24) According to the Finnish Arthroplasty Register, 10-year survival rate of UKAs implanted during the period of 1985 to 1990 was 63%, and 10-year survival rate of UKAs implanted during the period of 1991 to 1996 was 74%. The 10-year survival rate was 81% for Oxford implant, 79% for Miller-Galante II implant, 78% for Duracon implant, and 53% for PCA implant, illustrating a substantial differences depending on the types of implants.25) In 2011, Parratte et al.6) reported the 20-year survival rates of mobile-bearing and fixed-bearing types UKA to be 83% and 80%, respectively. In 2012, Epinette et al.,26) as the result of the analysis of 418 failures of UKA, reported that the problems related to surgical techniques were indeed the main causes of the failure in 11% of cases. Lyons et al.,23) as the result of the comparison of 5,605 cases of TKA with 279 cases of UKA, Kaplan-Meier survivorship at 10 years was 94.9% in TKA and 90.4% in UKA. Minimally invasive UKA was first introduced by Repicci and Eberle9) in the latter half of 1990's and used in earnest since the 2000's. There are not many reports on the long-term survival rates of minimally invasive UKA since the duration of follow-up is still short, and therefore report on 10-year survival rates of implants are also very rare scares (Table 4). Regarding the mid- to long-term survival rate of minimally invasive UKA using fixed-type implant, Biswal and Brighton10) and Konyves et al.11) reported 94% and 86.7% of 8-year survival rate, and O'Donnell and Neil4) reported 78% of 9-year survival rate. For the mid to long-term survival rate of minimally invasive UKA using Oxford phase 3, which is a mobile-bearing type, although Pandit et al.15) reported a 7-year survival rate of 97.3% in 2006, while Kort et al.12) reported that the 7-year survival rate was 89%, and Lisowski et al.14) reported a 7-year cumulative survival rate of 94.4% in 2011. In 2012, Pandit et al.8) reported that the 10-year survival rate of minimally invasive UKA was 96% through the prospective study of the first 1,000 phase 3 Oxford medial UKA at the mean follow-up of 5.6 years, while whereas Lim et al.13) reported the 10-year survival rate was of 94% for the Oxford phase 3 performed on 400 cases at the mean follow-up of 5.2 years. The 10-year survival rate in this study is 90.5%, which is relatively lower than the 10-year survival rate reported by Pandit et al.8) and Lim et al.13) However, it is deemed that the difference in the mean follow-up period must be considered.
Table 4. Survivorship of the Minimally Invasive Unicompartmental Knee Arthroplasty.
| Study | Year | Prosthesis | Number | Follow-up (yr) | Survival rate (%) (yr) |
|---|---|---|---|---|---|
| Pandit et al.15) | 2006 | Oxford phase 3 | 688 | 1-8 | 97 (7) |
| Kort et al.12) | 2007 | Oxford phase 3 | 154 | 2-7 | 89 (7) |
| Lisowski et al.14) | 2011 | Oxford phase 3 | 244 | 4.2 (1-10) | 94 (7) |
| Biswal and Brighton10) | 2010 | Allegretto | 128 | 5.7 (3-8) | 94 (8) |
| Konyves et al.11) | 2010 | Allegretto and EIUS | 15 and 15 | 6.9 and 8.9 | 87 (8) |
| O'Donnell and Neil4) | 2010 | Repicci II | 114 | 7.4 (5-9) | 78 (9) |
| Pandit et al.8) | 2012 | Oxford phase 3 | 1,000 | 5.6 (1-11) | 96 (10) |
| Lim et al.13) | 2012 | Oxford phase 3 | 400 | 5.2 (1-10) | 94 (10) |
| Current study | 2013 | Oxford phase 3 | 166 | 10 | 90.5 (10) |
In order to obtain good results after UKA, the usage of appropriate implant and accurate surgical techniques along with proper selection of patient are necessary. In 1989, Kozinn and Scott27) stated that the most appropriate candidates for the procedures include patients > 60 years of age and weighing < 180 lb (82 kg), with a low level of activity and minimal rest pain, and many authors have been agreeing with this assertion until now. However, the Oxford group reported that satisfactory results could be obtained regardless of the age, weight, obesity, and activity of the patient when Oxford knee, which is a mobile implant, is used.21) Our indication for UKA in this study was the same as that of Oxford group. The design of the implants is one of the very important factors in UKA.3,6) Fixed-type UKA may cause substantial wear of polyethylene implant because of the large amount of contact stress per unit surface area, and numerous cases of failure were reported because of the occurrence of the loosening of tibial implant. Mobile-type UKA has the advantage of reducing failure due to the loosening of tibial implant as well as minimal wear of polyethylene implant. However, the surgical technique for mobile-bearing UKA is more difficult, and there are more early failures because of the dislocation of mobile-bearing compared to fixed-bearing UKA. The Oxford knee, developed in 1978, is the most popular implant among the mobile-bearing UKA based on the assumption that the design would stimulate the normal meniscus of the knee with a mobile congruous design. Oxford phase 3 implants were used in all the cases in this study. Surgical technique and instrumentation are highly important in UKA for reducing complications and failures, and the results following UKA can manifest diversely depending on the surgical method and experience of the surgeon. UKA was performed using Oxford phase 3 implants and minimally invasive surgery using a short medial parapatellar approach in all the cases. The medial tibial plateau was excised using the extramedullary guide, and the level of horizontal tibial saw cut was made by sawing 2-3 mm below the deepest part of erosion to avoid over-resection of the bone. The posterior facet of the medial femoral condyle was excised using the intramedullary guide, and avoided extensive gap between femoral component and femoral condyle which might loosen the component because of excessive load. The ligament balancing was made by sizing and positioning of the implants and osteophyte removal. Normal soft tissue tension was restored by the insertion of appropriate sized implants and not by the release of soft tissue.
Complications of UKA are relatively few; however, there is controversy about the causes of complication and appropriate treatment. It is known that complications after UKA are polyethylene wear and breakage, aseptic loosening, the dislocation of polyethylene spacer, contralateral osteoarthritis, infection, tibial plateau fracture, limited motion, and unexplained severe pain.16) Most complications of Oxford phase 3 UKA are related to inappropriate patient selection or technical errors at the time of surgery; however, the implant design must also be considered. Failure mode of Oxford UKA has special characteristics. The failure from polyethylene wear or breakage is rare; however, there is a peculiar complication such as mobile-bearing dislocation, because of free movable bearing between the femoral and tibial components. Moreover the possibility of the disease progression exists, because it puts more stress on the lateral side of the joint. During this study, 16 cases (14 patients) of failures were observed among 166 cases (9.6%). Among those, mobile-bearing dislocations were the most common cause of failures (7 cases, 4.2%). There are many factors for mobile-bearing dislocation including patient selection, surgical technique, and lifestyle of patients. Moreover, the implant design is one of the most important factors. There was no failure because of the progression of osteoarthritis into the lateral compartment in this study. Some cases which showed the progression of degenerative changes in the lateral compartment and patellofemoral joint; however, no case needed revision surgery because of the lateral compartment or patellofemoral osteoarthritis. Aseptic loosening of the prosthesis is another common cause of failure after UKA. For the detection of aseptic loosening, differentiating pathologic radiolucency from physiologic radiolucency is very important. Physiologic radiolucency is narrow and non-progressive and is usually surrounded by a radiodense line. Pathologic radiolucency is progressive, broad, poorly defined and not surrounded by a radiodense line. Its presence can be suggestive of the implant loosening.18) Physiologic radiolucent line is almost always < 2 mm thick and is defined by a thin radiodense line.28) In this study, physiologic radiolucent lines were found in 31 cases (18.7%). As we defined the radiolucency > 2 mm of thickness with the progression as a loosening, 4 femoral and 1 tibial components loosening were observed. In all cases of implant loosening, revision TKA was performed.
The main strength of this study is that all the cases were followed up more than > 10 years, and it is significant that the survival rate was measured at 10 years after the operation only for the cases of the follow-up with > 10 years. For this study, clinical and radiographic assessments were performed preoperatively and regularly followed after the surgery from the first case of minimally invasive UKA. The main limitation of this study is that the 10-year survival rate is not enough for the final decision of the longevity of the minimally invasive UKA. Another limitation of this study is unequal male to female ratio. We guessed that it is caused by the difference in lifestyle between Western and Korean people; however, the exact cause is not known. The results of the longer follow-up clinical results of minimally invasive UKA including survival rate through further follow-up will be reported in the near future. The causes of the failures of minimally invasive UKA based on this survival study are under investigation.
Although the functions of the knee joint following the minimally invasive UKA are outstanding, and the survivorship of the implant improved substantially in comparison to the initial period according to advancement of the implant design and surgical technique, long-term survival rate of UKA is still known to be inferior to TKA. However, as manifested by the results of this study, minimally invasive UKA show satisfactory results in terms of the functions of the knee joint following the surgery, along with gradual improvement in the long-term survival rate of the implant. Therefore, minimally invasive UKA is anticipated to increase gradually in the future and will be a useful method in the treatment of osteoarthritis in one compartment of the knee joint.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Egidy CC, Sherman SL, Macdessi SJ, Cross MB, Windsor RE. Long-term survivorship of a unicondylar knee replacement: a case report. Knee. 2012;19(6):944–947. doi: 10.1016/j.knee.2012.03.015. [DOI] [PubMed] [Google Scholar]
- 2.Panni AS, Vasso M, Cerciello S, Felici A. Unicompartmental knee replacement provides early clinical and functional improvement stabilizing over time. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):579–585. doi: 10.1007/s00167-011-1613-y. [DOI] [PubMed] [Google Scholar]
- 3.Saccomanni B. Unicompartmental knee arthroplasty: a review of literature. Clin Rheumatol. 2010;29(4):339–346. doi: 10.1007/s10067-009-1354-1. [DOI] [PubMed] [Google Scholar]
- 4.O'Donnell T, Neil MJ. The Repicci II® unicondylar knee arthroplasty: 9-year survivorship and function. Clin Orthop Relat Res. 2010;468(11):3094–3102. doi: 10.1007/s11999-010-1474-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Rourke MR, Gardner JJ, Callaghan JJ, et al. The John Insall Award: unicompartmental knee replacement: a minimum twenty-one-year followup, end-result study. Clin Orthop Relat Res. 2005;440:27–37. doi: 10.1097/01.blo.0000185451.96987.aa. [DOI] [PubMed] [Google Scholar]
- 6.Parratte S, Pauly V, Aubaniac JM, Argenson JN. No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2012;470(1):61–68. doi: 10.1007/s11999-011-1961-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Munk S, Dalsgaard J, Bjerggaard K, Andersen I, Hansen TB, Kehlet H. Early recovery after fast-track Oxford unicompartmental knee arthroplasty: 35 patients with minimal invasive surgery. Acta Orthop. 2012;83(1):41–45. doi: 10.3109/17453674.2012.657578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW. Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br. 2011;93(2):198–204. doi: 10.1302/0301-620X.93B2.25767. [DOI] [PubMed] [Google Scholar]
- 9.Repicci JA, Eberle RW. Minimally invasive surgical technique for unicondylar knee arthroplasty. J South Orthop Assoc. 1999;8(1):20–27. [PubMed] [Google Scholar]
- 10.Biswal S, Brighton RW. Results of unicompartmental knee arthroplasty with cemented, fixed-bearing prosthesis using minimally invasive surgery. J Arthroplasty. 2010;25(5):721–727. doi: 10.1016/j.arth.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 11.Konyves A, Willis-Owen CA, Spriggins AJ. The long-term benefit of computer-assisted surgical navigation in unicompartmental knee arthroplasty. J Orthop Surg Res. 2010;5(1):94. doi: 10.1186/1749-799X-5-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kort NP, van Raay JJ, Cheung J, Jolink C, Deutman R. Analysis of Oxford medial unicompartmental knee replacement using the minimally invasive technique in patients aged 60 and above: an independent prospective series. Knee Surg Sports Traumatol Arthrosc. 2007;15(11):1331–1334. doi: 10.1007/s00167-007-0397-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim HC, Bae JH, Song SH, Kim SJ. Oxford phase 3 unicompartmental knee replacement in Korean patients. J Bone Joint Surg Br. 2012;94(8):1071–1076. doi: 10.1302/0301-620X.94B8.29372. [DOI] [PubMed] [Google Scholar]
- 14.Lisowski LA, van den Bekerom MP, Pilot P, van Dijk CN, Lisowski AE. Oxford Phase 3 unicompartmental knee arthroplasty: medium-term results of a minimally invasive surgical procedure. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):277–284. doi: 10.1007/s00167-010-1213-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pandit H, Jenkins C, Barker K, Dodd CA, Murray DW. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br. 2006;88(1):54–60. doi: 10.1302/0301-620X.88B1.17114. [DOI] [PubMed] [Google Scholar]
- 16.Kim KT, Lee S, Park HS, Cho KH, Kim KS. A prospective analysis of Oxford phase 3 unicompartmental knee arthroplasty. Orthopedics. 2007;30(5 Suppl):15–18. [PubMed] [Google Scholar]
- 17.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;(248):13–14. [PubMed] [Google Scholar]
- 18.Rea P, Short A, Pandit H, et al. Radiolucency and migration after Oxford unicompartmental knee arthroplasty. Orthopedics. 2007;30(5 Suppl):24–27. [PubMed] [Google Scholar]
- 19.Borjesson M, Weidenhielm L, Mattsson E, Olsson E. Gait and clinical measurements in patients with knee osteoarthritis after surgery: a prospective 5-year follow-up study. Knee. 2005;12(2):121–127. doi: 10.1016/j.knee.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 20.Murray DW, Goodfellow JW, O'Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br. 1998;80(6):983–989. doi: 10.1302/0301-620x.80b6.8177. [DOI] [PubMed] [Google Scholar]
- 21.Berger RA, Nedeff DD, Barden RM, et al. Unicompartmental knee arthroplasty: clinical experience at 6- to 10-year followup. Clin Orthop Relat Res. 1999;(367):50–60. [PubMed] [Google Scholar]
- 22.Whiteside LA. Making your next unicompartmental knee arthroplasty last: three keys to success. J Arthroplasty. 2005;20(4) Suppl 2:2–3. doi: 10.1016/j.arth.2005.03.029. [DOI] [PubMed] [Google Scholar]
- 23.Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, Mc-Calden RW. Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res. 2012;470(1):84–90. doi: 10.1007/s11999-011-2144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.W-Dahl A, Robertsson O, Lidgren L, Miller L, Davidson D, Graves S. Unicompartmental knee arthroplasty in patients aged less than 65. Acta Orthop. 2010;81(1):90–94. doi: 10.3109/17453671003587150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78(1):128–135. doi: 10.1080/17453670610013538. [DOI] [PubMed] [Google Scholar]
- 26.Epinette JA, Brunschweiler B, Mertl P, Mole D, Cazenave A; Unicompartmental knee arthroplasty modes of failure: wear is not the main reason for failure: a multicentre study of 418 failed knees. Orthop Traumatol Surg Res. 2012;98(6 Suppl):S124–S130. doi: 10.1016/j.otsr.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 27.Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989;71(1):145–150. [PubMed] [Google Scholar]
- 28.Goodfellow J, O'Connor J, Dodd C, Murray D. Postoperative management and radiography. In: Goodfellow J, O'Connor J, Dodd C, Murray D, editors. Unicompartmental arthroplasty with the Oxford knee. Oxford: Goodfellow; 2011. pp. 117–128. [Google Scholar]