Abstract
Objectives
Most research examining the impact of patients seeking online health information treats internet information homogenously, rather than recognizing that there are multiple types and sources of available information. The present research was conducted to differentiate among sources and types of internet information that patients search for, intend to discuss with their doctors, and recall discussing with their doctors, and to determine how accurate and hopeful patients rate this information.
Methods
We surveyed 70 breast cancer patients recruited from the waiting rooms of breast medical oncology and surgery clinics. The main variables in the study were as follows: (1) the sources and types of online information patients have read, intended to discuss, and actually discussed with their doctors, and (2) how accurately and hopefully they rated this information to be.
Results
Patients read information most frequently from the websites of cancer organizations, and most often about side effects. Patients planned to discuss fewer types of information with their doctors than they had read about. They most often intended to discuss information from cancer organization websites or WebMD, and the material was most often about alternative therapies, side effects, and proven or traditional treatments. Some 76.8% of total participants rated the information they had read as very or somewhat accurate, and 61% rated the information they had read as very or somewhat hopeful.
Significance of Results
Internet information varies widely by source and type. Differentiating among sources and types of information is essential to explore the ways in which online health information impacts patients’ experiences.
Keywords: Doctor–patient communication, Online health information-seeking, Internet health information, Trusted health sources
INTRODUCTION
It is well established in the literature that use of the internet to research health information is common among cancer patients (Castleton et al., 2011). Patients’ use of internet information has many potential benefits (e.g., it may improve patients’ self-help skills, which is less expensive than professional care [Bennett-Clark, 1996]). Health-related internet use has demonstrated an association with greater belonging and support and less loneliness than internet use for other reasons or internet nonuse (Fogel et al., 2002). The internet provides a medium through which the medical community and patients may exchange and update information (Peters, 1997). Disease-specific websites, electronic mailing lists, and online support groups provide valuable informational and emotional support for patients and care-givers (Eysenbach, 2003; Meier et al., 1997; Rains & Young, 2009). Finally, access to information about one’s health condition online may increase patients’ sense of control and ability to participate actively in making healthcare decisions; this may result in better psychological outcomes for the patient (Bass et al., 2006; Kaplan & Frosch, 2005; Lee et al., 2010).
Despite these positive outcomes, online health information may also have a downside for both patients and caregivers. Oncology is an area in which people are likely to be confronted with several equally valid treatment options (Burstein, 2000). Cancer-related internet information can introduce conflicting medical information and treatment options, causing patients to become overwhelmed, nervous, anxious, and confused (Sabel et al., 2005; Helft et al., 2005). Also, the accuracy of health information obtained online has been called into question. Eysenbach (2002) reviewed studies that evaluated the quality of health-related websites and showed that 70% of studies concluded that information quality is a problem on the internet and that only 9% of studies evaluated information found on websites positively overall, suggesting that the likelihood of obtaining high-quality health-related information on the internet is low.
As of 2007, 25.7% of all people who had used the internet and had visited a health professional within the year had talked to a doctor, nurse, or other health professional about health information they had accessed online. Discussions about internet information may impact the doctor–patient relationship (Burstein, 2000). In the past, physicians were responsible for providing all the information about the diagnosis, prognosis, and treatment options for patients (Fogel et al., 2002). Increased access to information provided by the internet serves to level this imbalance of power (Eysenbach, 2002). Doctors report difficulty in having discussions with their patients about information they have accessed on the internet (Helft et al., 2003). Doctors’ reactions to patients’ concerns based on information they have read online have implications for patient satisfaction as well (Bylund et al., 2007; Bylund et al., 2010), and poor doctor–patient communication can lead to negative health outcomes (Ong et al., 1995).
In general, research on patients seeking cancer-related information online and research on patients discussing that information with their doctors often treat internet information as a single, homogenous entity (see, e.g., Fogel et al., 2002; Mancini et al., 2006; Raupach & Hiller, 2002). However, the research has shown that patients who use the internet for cancer information do not value all the information they encounter equally. Fogel and colleagues (2002) found that the favorite websites of breast cancer patients tended to contain reliable and credible information. Further, it is well established that the rates and styles of information-seeking on the internet vary by cancer type (Mancini et al., 2006; Sabel et al., 2005).
In a recent review of internet utilization among patients with cancer, Castleton and colleagues (2011) stated, “Understanding the characteristics of patients who use the internet for health-related information and the details of their online search is an important step in improving the interaction among healthcare providers, patients, and the internet” (p. 1184). The present study highlights that another important step for improving interactions among healthcare providers, patients, and the internet is to understand the types and sources of internet information that patients intend to discuss and choose to discuss with their healthcare providers. In order to better understand how varying sources and types of internet information-seeking may affect breast cancer patients’ experiences with their doctors, our study addressed the following research questions:
RQ1: What are the most common sources and types of information about breast cancer that patients (a) read online, (b) intend to talk about with their doctors, and (c) actually talk about with their doctors?
RQ2: How accurate do breast cancer patients rate the sources and types of the information that they (a) read online, (b) intend to talk about with their doctors, and (c) actually talk about with their doctors?
RQ3: How hopeful do breast cancer patients rate the sources and types of information that they (a) read online, (b) intend to talk about with their doctors, and (c) actually talk about with their doctors?
RQ4: Are there associations between the types of information read on the internet and patients’ demographic, disease, or visit characteristics?
METHOD
Data Collection
A research study assistant approached 576 patients in the waiting rooms of the breast medical oncology and surgery clinics at Memorial Sloan-Kettering Cancer Center over a 19-month period of time from July 2008 to January 2010. Each approached patient had met the prescreening criteria of having a breast cancer diagnosis, being female, and being 21 years or older. Eighteen of the patients approached did not speak English and were excluded from the study, leaving 558 patients who were asked the screening question(s) described below. Fifteen doctors participated in the study, including nine medical doctors and six breast surgeons. This study was approved by the institutional review board.
The study was conducted in two recruitment phases. In phase one, 299 eligible patients were asked, “In the past month, have you read information on the internet related to your breast cancer?” Of those approached, 67 patients responded affirmatively, and 36 (54%) of those were recruited to the study. In phase 2, recruitment strategies were broadened to include those patients with a history of obtaining breast cancer–related internet information, despite not accessing such information during the past month. Eligible patients were first asked, “Have you read information on the internet related to your breast cancer since your diagnosis?” If the patient responded affirmatively, she was then asked a follow-up question: “When was the last time you read internet information about your breast cancer?” Of the 259 patients approached during phase two, 49 patients reported having read since their diagnosis, and 17 patients reported having read internet information during the past month. Six (35%) were recruited for the study. Of the 32 patients who reported having read internet information at some point since their diagnosis, although not within the past month, 28 (87%) agreed to participate in a smaller, survey-only study. Patients in both groups made up our total sample (N = 70). The recruiting schema and results are presented in Figure 1.
Fig. 1.
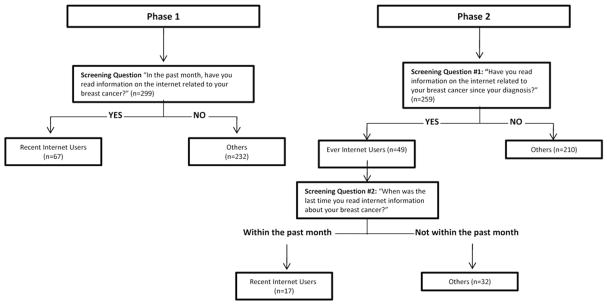
Screening schema and results.
We refer to the group of 42 patients who had looked up internet information within the past month as Recent Internet Users (RIUs). We refer to the group of 28 patients who had looked up internet information at some point since their diagnosis, but not within the past month, as Ever Internet Users (EIUs).
Participants
A total of 70 patients were recruited. Common reasons cited for refusal to participate included feeling stressed, not feeling well, and a lack of time. To address the research questions focusing on information that patients reported reading online, we have analyzed data from the 42 RIUs and 28 EIUs. We analyzed data from 19 RIUs who intended to discuss the internet information with their doctors in order to address the research questions focusing on the information patients intended to discuss with their doctors. To address the research questions focusing on information patients reported discussing with their doctors in the past, we analyzed the 22 EIUs who reported that they had discussed internet information with their doctor.
The demographic information is presented in Table 1. Participants were predominantly Caucasian (78.6%), married (67.7%), and highly educated (84.3% with an undergraduate or postgraduate degree). Participants were between the ages of 27.5 and 79.3 years (M = 52.5, SD = 10.5). Average time since cancer diagnosis was 3.6 years (range = 0.03–21.7 years, SD = 4.6). The majority of participants had stage I disease (41.4%) and nonrecurrent disease (90%). Most participants were seeing their doctor for a follow-up visit (77.1%) at the time they were consented.
Table 1.
Sample demographics
| Participants (N=70) | |
|---|---|
| Patient Characteristics | |
| Age | M=52.5 years (SD = 10.5) |
| Race | |
| Caucasian | 55 (78.6%) |
| African American | 8 (11.4%) |
| Unknown | 3 (4.3%) |
| Latino/Hispanic | 2 (2.9%) |
| Asian | 2 (2.9%) |
| Marital status | |
| Married | 47 (67.7%) |
| Single | 11 (15.7%) |
| Other | 8 (11.4%) |
| Living w/partner | 2 (2.9%) |
| Divorced/separated | 1 (1.4%) |
| Unknown | 1 (1.4%) |
| Education level | |
| Postgraduate degree | 31 (44.3%) |
| Undergraduate degree | 28 (40%) |
| High school | 8 (11.4%) |
| Technical degree | 3 (4.3%) |
| Disease characteristics | |
| Disease stage | |
| Stage I | 29 (41.4%) |
| Stage II | 18 (25.7%) |
| Stage III | 7 (10%) |
| Stage IV | 16 (22.9%) |
| Recurrent disease | 7 (10%) |
| Time since diagnosis | M = 3.6 years (SD = 4.6) |
| Visit characteristics | |
| Visit type | |
| Follow-up | 54 (77.1%) |
| New visit | 16 (22.9%) |
| Number of visits (w/oncologist) | M = 10.2 (SD = 13.6) |
| Time since 1st visit | M = 1.8 years (SD = 2.6) |
Materials
Following consent, each patient completed a questionnaire about her internet use and demographic information. Patients were given a list of 13 sources of internet information (e.g., government websites, cancer websites) and asked to mark all those from which they had read information. Patients were also given a list of 12 types of internet information (e.g., prognosis, clinical trials) and asked to mark all those about which they had read. The items were repeated when asking patients specifically about information they intended to discuss or that they had discussed. Answers to these questions were not mutually exclusive; patients could mark as many sources and types that applied. Patients were also asked to rate their perceptions of accuracy and hopefulness of internet information.
RESULTS
Sources and Types of Internet Information
Patients reported reading information from an average of 3.76 categories of sources (SD = 2.2), the most frequent being websites of cancer organizations (55.7%), hospital or cancer center websites (54.3%), WebMD (41.4%), and government websites (41.4%) (see Table 2). Patients reported reading an average of 4.61 types of information (SD = 2.4), most frequently about side effects (72.9%), diagnosis (62.9%), prognosis (61.4%), and proven or traditional treatments (51.4%) (see Table 3).
Table 2.
Sources of Information about Breast Cancer Information Accessed on the Internet
| Sources of information accessed on internet (N = 70) | Sources of information that people intended to discuss with doctors (N = 19) | Sources of internet information that people discussed with doctors (N = 22) | |
|---|---|---|---|
| Source of information | n (%) | n (%) | n (%) |
| Cancer Organization Website (e.g., NCCN) | 39 (56%) | 9 (47%) | 10 (46%) |
| Hospital/Cancer Center Website | 38 (54%) | 8 (42%) | 11 (50%) |
| Web MD | 29 (41%) | 9 (47%) | 5 (23%) |
| Government Website (e.g., NCI) | 29 (41%) | 3 (16%) | 11 (50%) |
| Comprehensive Internet Service Provider (e.g., AOL) | 28 (40%) | 6 (32%) | 2 (9%) |
| Foundation Website (e.g., Susan G. Komen Foundation) | 21 (30%) | 2 (11%) | 6 (27%) |
| Scientific Journal Article | 16 (23%) | 4 (21%) | 0 (0%) |
| Pharmaceutical or Drug Website | 11 (16%) | 4 (21%) | 1 (5%) |
| Pub Med Literature Search | 11 (16%) | 2 (11%) | 0 (0%) |
| Media Website (e.g., CNN.com) | 16 (23%) | 3 (16%) | 3 (14%) |
| individuals’ homepages or weblogs | 16 (23%) | 1 (5%) | 3 (14%) |
| Health Chat Room or Message Board | 6 (9%) | 0 (0%) | 3 (14%) |
| Other | 3 (4%) | 2 (11%) | 0 (0%) |
Table 3.
Types of breast cancer information accessed on the internet
| Type of Internet Information Accessed by Participants (N = 70) | Type of Internet Information Participants Intended to Discuss with Doctors (N = 19) | Type of Internet Information Participants Discussed with Doctors (N = 22) | |
|---|---|---|---|
| Type of information | n (%) | n (%) | n (%) |
| Side effects | 51 (73%) | 10 (53%) | 8 (36%) |
| Diagnosis | 44 (63%) | 9 (47%) | 3 (14%) |
| Prognosis (i.e., what you expect in the future) | 43 (61%) | 8 (42%) | 11 (50%) |
| Proven or traditional treatments | 36 (51%) | 10 (53%) | 9 (41%) |
| Alternative therapies | 29 (41%) | 10 (53%) | 3 (14%) |
| Experiences of other cancer patients | 29 (41%) | 2 (11%) | 6 (27%) |
| Cancer facts and figures (e.g., incidence, prevalence, risk factors) | 25 (36%) | 1 (5%) | 0 (0%) |
| Clinical trials | 23 (33%) | 4 (21%) | 4 (18%) |
| Treatments offered by other doctors or cancer centers | 16 (23%) | 2 (11%) | 0 (0%) |
| Psychosocial support services | 11 (16%) | 1 (5%) | 0 (0%) |
| Genetic counseling | 8 (11%) | 0 (0%) | 0 (0%) |
| Other | 7 (10%) | 2 (11%) | 1 (5%) |
Similar to other results (Bylund et al., 2009), 19 of the 42 RIUs (45%) reported an intention to discuss the internet information they had read with their doctor. They reported an average of 2.84 sources of information that they intended to discuss. Most frequently, this information came from cancer organization websites (47.4%), WebMD (47.4%), and hospital or cancer center websites (42.1%) (see Table 2). These patients intended to discuss an average of 3.11 types of information, most frequently alternative therapies, side effects, and proven or traditional treatments (all at 52.6%) (see Table 3).
Some 22 of the 28 EIUs reported that they had discussed information from the internet with their doctor. They reported that the information they had discussed came from an average of 2.5 categories of sources — most frequently hospital or cancer websites (50.0%), government websites (50.0%), and cancer organization websites (45.5%) (see Table 2). They reported discussing 2.05 types of online information, most frequently about prognosis (50%), proven or traditional treatments (40.9%), and side effects (36.4%) (see Table 3).
Accuracy of Information
About three quarters of the participants (76.8%) rated the information they had read as very or somewhat accurate. Of the RIUs who intended to talk with their doctor about the information, there was no difference in accuracy ratings between the subset of information they intended to discuss and all the information they had read. Similarly, for EIUs who had discussed internet information in the past, there was no difference between ratings of the information they discussed and ratings of all of the information they had read. Merging the RIU and the EIU groups, there were nonsignificant trends that showed information that was discussed or intended to be discussed was rated as less accurate than all the information they had chosen (p = 0.11).
Hopefulness of Information
Some 61% of total participants rated the information they had read as very or somewhat hopeful. Of those RIUs who intended to talk to their doctor about the internet information, there was no difference in hopefulness ratings between the subset of information they intended to discuss and all the information they had read. Similarly, for EIUs who had discussed internet information in the past, there was no difference between ratings of the information they discussed and ratings of all the information they had read.
Differences in Information Read by Patient Characteristics
The final research question asked if there were patient demographic, disease, or visit characteristic differences found in the types of breast cancer information read online. For consistency, we only analyzed the data from the RIUs for this research question, as all of these respondents were answering the questions about information they had read in the past month. Because of the small sample size and exploratory nature of the study, we also reported statistical trends of p = 0.10 and less. A summary of these findings is presented in Table 4.
Table 4.
Differences in Information read based on patient characteristics
| Type of Information Read | Patient Characteristics
|
Seeing a Surgeon | Seeing a Medical Oncologist | Diagnosed for Less Time | Younger | ||
|---|---|---|---|---|---|---|---|
| Stage 2 or Higher | Without Recurrence | New Visit | |||||
| Prognosis | p = 0.09 | ||||||
| Alternative therapies | p = 0.07 | ||||||
| Diagnosis | p < 0.05 | p < 0.05 | p = 0.08 | ||||
| Side effects | p = 0.10 | ||||||
| Proven/traditional treatments | p = 0.10 | ||||||
| Experience of other cancer patients | p < 0.01 | ||||||
| Treatments offered by other doctors or cancer centers | p < 0.05 | ||||||
| Clinical trials | p < 0.01 | p < 0.01 | |||||
| Genetic counseling | p = 0.06 | ||||||
Prognosis
There was a trend for women who had read information online about prognosis during the past month to be more likely to have been diagnosed with later-stage disease, such that those diagnosed with stage II breast cancer or higher were more likely to read online information than those diagnosed at stage I (x2 = 2.89, p = 0.09).
Alternative therapies
Those who had read about alternative therapies trended toward being more likely to be without a recurrence of their cancer (x2 = 3.20, p = 0.07).
Diagnosis
Patients who reported reading internet information about diagnosis in the past month were more likely to be coming for a new visit than for follow-up (x2 = 4.81, p < 0.05) and more likely to be seeing a surgeon than a medical oncologist (x2 = 5.54, p < 0.05). In addition, there was a trend for patients who had read about diagnosis in the past month to have been diagnosed for less time than those who had not (M = 1.03 vs. 2.37 years, p = 0.08).
Side effects
Those who had read about side effects tended to be without a recurrence of their cancer (x2 = 2.75, p = 0.10).
Proven or traditional treatments
Those who had read in the last month about traditional treatments trended toward being more likely to be seeing a medical oncologist than a surgeon (x2 = 2.78, p = 0.10).
Experience of other cancer patients
Patients who read online about the experiences of other cancer patients were younger than those who had not (M = 46.4 vs. 54.4 years, p < 0.01).
Treatments offered by other doctors or cancer centers
Patients who had read in the last month about treatments offered by other doctors or cancer centers were more likely to be coming for a new visit than for follow-up (x2 = 4.20, p < 0.05).
Clinical trials
Patients who had read in the last month about clinical trials were more likely to be diagnosed as stage II or higher than stage I (x2 = 7.63, p < 0.01) and more likely to be visiting a medical oncologist than a surgeon (x2 = 7.53, p < 0.01).
Genetic counseling
There was a trend for those who had read internet information about genetic counseling to be younger than the patients who had not (M = 44.03 vs. 52.36 years, p = 0.06).
DISCUSSION
Past research on the impact of internet information on patient experiences has provided valuable information about the common demographic characteristics of patients who choose to seek information online (Mancini et al., 2006), patients’ motivation to read information (Nagler et al., 2010), patterns of use (Lee et al., 2010), decisions to discuss the information or not (Diaz et al., 2002), and doctors’ reactions to such discussions (Helft et al., 2003). Most of this work, however, treats the concept of internet information as unidimensional. Our study highlights the need to recognize the multifaceted nature of health information-seeking. As researchers continue to explore the effects of online health information on patients’ experiences, it is essential that study methods be designed to capture the variation in types and sources of internet information that patients read. The results of the exploratory study reported here demonstrate that internet information is multidimensional in both source and type.
When internet information is treated as a single entity, a common fallacy is that, because misinformation about untested and alternative therapies exists on the internet, patients who use the internet are likely to become misinformed about their health conditions and treatment options, and to challenge their physicians’ treatment recommendations based on this misinformation. For example, in response to findings that 63% of breast cancer patients used the internet to look up information on alternative treatments, Burstein (2000) noted, “These therapies generally lack the scientific, preclinical basis, traditional clinical trials and safety examinations, and peer-reviewed medical publications that provide the foundation for standard medical care” (p. 154). The author further warned that patients’ searching for this type of information is likely to introduce future challenges to the physician–patient relationship: “The freewheeling nature of the internet has afforded prime visibility for alternative medicine, and oftentimes, physicians can be inundated by questions about these various health practices” (Burstein, 2000, p. 154). This type of speculation assumes that patients are unable to distinguish between legitimate and illegitimate treatments discussed online, and that they are likely to challenge their physicians with all of the information they read.
The data from our study contrast Burstein’s (2000) predictions. We found that breast cancer patients favor reliable and credible websites, most frequently using and discussing information from websites sponsored by cancer organizations, hospitals and cancer centers, the government, and WebMD. Taken together with other studies discussed below, these results suggest that patients are more likely to use the internet as a supplemental tool to inform themselves to work in conjunction with their physicians, rather than using the internet as a tool to challenge physician recommendations.
We also found that breast cancer patients are most likely to both read about and decide to talk with their doctors about internet information regarding diagnosis, prognosis, proven or traditional treatments, and side effects. Alternative therapies were read about by approximately 40% of participants, and more than half of those who were planning to discuss inter-net information with their doctors reported planning to talk about alternative therapies. This is a particularly interesting finding given a past systematic review of published data on the use of complementary and alternative medicine in cancer care in 13 different countries, which found that use of alternative medicine is highly prevalent (nearly a third of cancer patients reported using complementary and/or alternative methods) (Ernst, 1998).
When the sample was divided into subgroups depending on whether patients had discussed information with doctors, there were no data to suggest that the information that patients chose to discuss with their doctors was perceived to be more or less accurate or hopeful compared to information they chose not to discuss. When we collapsed these two groups into one, however, we found a trend in patients intending to discuss internet information that they believed it to be less accurate. This suggests that, rather than using internet information to challenge information provided by doctors, perhaps patients view doctors as a credible source of expertise who can con-firm or debunk the claims they read online. This is consistent with research that has shown that, even though patients more often search online to find specific health information, they still rate physicians as the preferred and most trusted source of specific health information (Hesse et al., 2005). It is also consistent with research which has found that two of the main reasons cancer patients and their caregivers discuss internet information with their doctors are to get the doctor’s advice and to become more educated (Bylund et al., 2009).
Underscoring the importance of examining variations in internet information was our finding that the type of information read was associated with patients’ age, stage of cancer, time since diagnosis, whether or not she had a recurrence, the type of doctor she was seeing, and whether she was coming for a new visit or follow-up. This speaks to the importance of recognizing the information-seeking needs of newly diagnosed patients, acknowledging that different search motivations depend on cancer type and stage of disease. Much more focused research will be necessary to get a clear picture of the complex issue of internet cancer information-seeking and the impact it may have on the doctor–patient relationship.
LIMITATIONS
Several limitations should be noted. First, our sample was not very demographically diverse. Participants were predominantly Caucasian, married, and highly educated. Past studies have shown that the tendency to search for internet information online and judgments about credibility and accuracy vary based on these demographics (e.g., Helft et al., 2005; Shim, 2008). Therefore, our study is valuable in that questions about internet cancer information-seeking and discussions with physicians should examine trends among specific groups in isolation from one another, but it is limited in that results should not be generalized beyond the demographics of the study participants.
Second, because recent internet users (those who had sought information about their cancer online during the past month) were not as common as we had expected, we had to expand the study midway through the data collection phase to include people who had ever researched information about their cancer online. Due to the small sample size, we collapsed these two groups for analyses used to answer the first three research questions. When these groups were separated out to address research question 4, systematic differences between groups emerged. Future research must take a broader approach to recruitment (e.g., recruiting from multiple cancer clinics) in order to obtain a large enough sample to be able to examine these questions more robustly. This type of recruitment requires resources that were beyond the scope of our project. Nonetheless, we feel that this study takes a first step in identifying key differences in internet information-seeking behaviors and decisions to discuss or withhold information from physicians. These findings provide a foundation for future study, in the hope of improving communication about internet information between breast cancer patients and their physicians.
Acknowledgments
This research was funded by National Cancer Institute Grant CA 130591 and National Cancer Institute Grant T32 CA009461.
References
- Bass SB, Ruzek SB, Gordon TF, et al. Relationship of internet health information use with patient behavior and self-efficacy: Experiences of newly diagnosed cancer patients who contact the National Cancer Institute’s Cancer Information Service. Journal of Health Communication: International Perspectives. 2006;11(2):219–236. doi: 10.1080/10810730500526794. [DOI] [PubMed] [Google Scholar]
- Bennett-Clark J. Where health information is byte-size: Online advice can help you manage health cost. Kiplinger’s Personal Finance. 1996:96–97. [Google Scholar]
- Burstein HJ. Commentary on “Internet usage among women with breast cancer: An exploratory study. Clinical Breast Cancer. 2000;1(2):154–155. doi: 10.3816/CBC.2000.n.013. [DOI] [PubMed] [Google Scholar]
- Bylund CL, Sabee CM, Imes RS, et al. Exploration of the construct of reliance among patients who talk with their providers about internet information. Journal of Health Communication. 2007;12(1):17–28. doi: 10.1080/10810730601091318. [DOI] [PubMed] [Google Scholar]
- Bylund CL, Gueguen JA, D’Agostino TA, et al. Cancer patients’ decisions about discussing internet information with their doctors. Psycho-Oncology. 2009;18:1139–1146. doi: 10.1002/pon.1511. [DOI] [PubMed] [Google Scholar]
- Bylund CL, Gueguen JA, D’Agostino TA, et al. Doctor–patient communication about cancer-related internet information. Journal of Psychosocial Oncology. 2010;28:127–142. doi: 10.1080/07347330903570495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castleton K, Fong T, Wang-Gillam A, et al. A survey of internet utilization among patients with cancer. Supportive Care in Cancer. 2011;19:1183–1190. doi: 10.1007/s00520-010-0935-5. [DOI] [PubMed] [Google Scholar]
- Diaz JA, Griffith RA, Ng JJ, et al. Patients’ use of the internet for medical information. Journal of General Internal Medicine. 2002;17(3):180–185. doi: 10.1046/j.1525-1497.2002.10603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst E. The prevalence of complementary/alternative medicine in cancer. Cancer. 1998;83:777–782. doi: 10.1002/(sici)1097-0142(19980815)83:4<777::aid-cncr22>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Eysenbach G. Infodemiology: The epidemiology of (mis)information. The American Journal of Medicine. 2002;113(9):763–765. doi: 10.1016/s0002-9343(02)01473-0. [DOI] [PubMed] [Google Scholar]
- Eysenbach G. The impact of the internet on cancer outcomes. CA: A Cancer Journal for Clinicians. 2003;53(6):356–371. doi: 10.3322/canjclin.53.6.356. [DOI] [PubMed] [Google Scholar]
- Fogel J, Albert SM, Schnabel F, et al. Internet use and social support in women with breast cancer. Health Psychology. 2002;21(4):398–404. [PubMed] [Google Scholar]
- Helft PR, Hlubocky F, Daugherty CK. American oncologists’ views of internet use by cancer patients: A mail survey of American Society of Clinical Oncology members. Journal of Clinical Oncology. 2003;21(5):942–947. doi: 10.1200/JCO.2003.08.007. [DOI] [PubMed] [Google Scholar]
- Helft PR, Eckles RE, Johnson-Calley CS, et al. Use of the internet to obtain cancer information among cancer patients at an urban county hospital. Journal of Clinical Oncology. 2005;23(22):4954–4962. doi: 10.1200/JCO.2005.09.621. [DOI] [PubMed] [Google Scholar]
- Hesse B, Nelson D, Kreps G, et al. Trust and sources of health information: The impact of the internet and its implications for health care providers: Findings from the Health Information National Trends Survey. Archives of Internal Medicine. 2005;165:2618–2624. doi: 10.1001/archinte.165.22.2618. [DOI] [PubMed] [Google Scholar]
- Kaplan RM, Frosch DL. Decision making in medicine and health care. Annual Review of Clinical Psychology. 2005;1(1):525–556. doi: 10.1146/annurev.clinpsy.1.102803.144118. [DOI] [PubMed] [Google Scholar]
- Lee CJ, Gray SW, Lewis N. Internet use leads cancer patients to be active health care consumers. Patient Education and Counseling. 2010;81(Suppl 1):S63–S69. doi: 10.1016/j.pec.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini J, Nogues C, Adenis C, et al. Patients’ characteristics and rate of internet use to obtain cancer information. Journal of Public Health. 2006;28(3):235–237. doi: 10.1093/pubmed/fdl019. [DOI] [PubMed] [Google Scholar]
- Meier A, Lyons JE, Frydman G, et al. How cancer survivors provide support on cancer-related internet mailing lists. Journal of Medical Internet Research. 1997;9(2):e12. doi: 10.2196/jmir.9.2.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler R, Romantan A, Kelly B, et al. How do cancer patients navigate the public information environment? Understanding patterns and motivations for movement among information sources. Journal of Cancer Education. 2010;25(3):360–370. doi: 10.1007/s13187-010-0054-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong LML, de Haes JCJM, Hoos AM, et al. Doctor–patient communication: A review of the literature. Social Science & Medicine. 1995;40(7):903–918. doi: 10.1016/0277-9536(94)00155-m. [DOI] [PubMed] [Google Scholar]
- Peters RS. Digital dialogue: Sharing information and interests on the internet. The Journal of the American Medical Association. 1997;277(15):1258–1260. doi: 10.1001/jama.277.15.1258. [DOI] [PubMed] [Google Scholar]
- Rains SA, Young VA. Meta-analysis of research on formal computer-mediated support groups: Examining group characteristics and health outcomes. Human Communication Research. 2009;35(3):309–336. [Google Scholar]
- Raupach JCA, Hiller JE. Information and support for women following the primary treatment of breast cancer. Health Expectations. 2002;5:289–301. doi: 10.1046/j.1369-6513.2002.00191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabel MS, Strecher VJ, Schwartz JL, et al. Patterns of internet use and impact on patients with melanoma. Journal of the American Academy of Dermatology. 2005;52(5):779–785. doi: 10.1016/j.jaad.2004.10.874. [DOI] [PubMed] [Google Scholar]
- Shim M. Connecting internet use with gaps in cancer knowledge. Health Communication. 2008;23(5):448–461. doi: 10.1080/10410230802342143. [DOI] [PubMed] [Google Scholar]


