Abstract
Objective
The goal of this study is to examine the developmental epidemiology of normative irritability and its tonic and phasic components in a longitudinal community sample of youth.
Method
Eight waves of data from the prospective, community Great Smoky Mountains Study (6,674 assessment of 1,420 participants) were used, covering children in the community aged 9–16 years old. Youth and one parent were interviewed using the Child and Adolescent Psychiatric Assessment to assess tonic (touchy/easily annoyed, irritable mood, angry or resentful) and phasic (temper tantrums or anger outbursts) components of irritability, including frequency, duration, onset, and cross-context variability.
Results
At any given point in childhood/adolescence, 51.4% (standard error [SE]=1.4) of participants reported phasic irritability, 28.3% (SE=1.2) reported tonic irritability, and 22.8% (SE=1.1) reported both. These prevalence levels decreased with age but did not vary by sex. The overlap between tonic and phasic irritability was high (OR=5.8, 95% CI, 3.3–10.5, p <.0001), with little evidence of tonic occurring without phasic irritability. Both tonic and phasic irritability predicted one another over time, supporting both heterotypic and homotypic continuity. Low levels of either tonic or phasic irritability increased risk for disrupted functioning including service use, school suspensions, parental burden, and emotional symptoms both concurrently and at one-year follow-up.
Conclusion
Irritability is relatively common, decreases with age but does not vary by sex, and at almost any level is associated with increased risk of disrupted functioning. Its relative components frequently overlap, although irritable outbursts are more common than irritable mood. Irritability appears to be a high-priority transdiagnostic marker for screening children in need of clinical attention.
Keywords: childhood, irritability, epidemiology, development, longitudinal
INTRODUCTION
In recent years, irritability has become the focus of increased scientific attention.1, 2 It is both a normative developmental phenomenon distributed dimensionally across the population, as well as an impairing symptom in multiple childhood psychopathologies.3, 4 Indeed, irritability is a criterion in various psychiatric disorders,2, 3, 5–8 and it may be a risk factor for later unipolar depression and anxiety.9–14 Irritability has been defined as a propensity to react with anger, grouchiness, or tantrums disproportionate to the situation.10, 15, 16 At a recent National Institute of Mental Health (NIMH) expert workshop on childhood irritability,17 the construct was conceptualized as having two components: tonic and phasic irritability. The tonic component was defined as a persistently angry, grumpy, or grouchy mood; phasic irritability was conceptualized as behavioral outbursts of intense anger.17 Even amongst this expert panel, little is known about these components; the presentation of tonic and phasic irritability, as well as their overlap and interplay across development, remains unknown. Moreover, the developmental manifestations that merit clinical attention require further research. The aim of this analysis is to use a community sample to study irritability and its components across middle childhood and adolescence.
Irritability has been typically studied as part of established psychopathologies, with much less attention to irritability itself and its respective tonic and phasic components. Using the Child Behavior Checklist (CBCL;18), a parent-report inventory, Althoff et al 11 found approximately 3.5% of a general Dutch population sample of youth were rated highly on aggressive behavior in addition to attention problems and anxiety and depression according to the CBCL-Dysregulation Profile (CBCL-DP).11 Similarly, Stringaris and Goodman12 found that more than 5% of the population by parent- and self-report endorsed “mood lability.” In a preschool sample, chronic irritability was associated with depression, oppositional defiant disorder, and functional impairment.19 Together, these studies have established that severe or chronic forms of irritability are associated with behavioral and emotional psychopathology, as well as adverse long-term functioning. None of these studies, however, have explicitly examined tonic and phasic manifestations of irritability.
Studies that have included both tonic and phasic components of irritability have examined them in the context of severe diagnostic phenotypes: severe mood dysregulation and its DSM-5 variant, disruptive mood dysregulation disorder. For example, Brotman et al 20 found a lifetime prevalence of 3.3% of youth meeting severe mood dysregulation (SMD),1, 21 a phenotype of severe irritability (i.e., tonic), temper outbursts (i.e., phasic), and hyperarousal symptoms.20 Similarly, the prevalence of DSM-5 disruptive mood dysregulation disorder was low across three community studies, but individual criteria for severe tantrums and negative mood were much higher.22 Rates were higher still in a sample of preschool children.23 These studies suggest individual irritability components may be quite common when extricated from severe psychopathology.
While research on pathological irritability has burgeoned, little is known about the developmental course of normative irritability. To date, only one study has examined the developmental trajectory of normative irritability 24; however, that study did not examine proposed tonic and phasic components. Our goals are threefold: 1) examine the prevalence of tonic and phasic manifestations of irritability during childhood and adolescence; 2) test the interplay and overlap between these components; and 3) determine normative levels of tonic or phasic irritability, and manifestations meriting clinical attention. Together, these analyses will determine the extent to which the components of tonic and phasic irritability are useful in understanding the developmental manifestations of irritability and its effects in childhood.
METHOD
Participants
The Great Smoky Mountains Study is a longitudinal, representative study of children in 11 predominantly rural counties of North Carolina (see 25). Three cohorts of children, ages 9, 11, and 13 years, were recruited from a pool of some 12,000 children using a two-stage sampling design, resulting in N = 1,420 participants (49% female; see also 25). American Indians were oversampled to constitute 25% of the sample; seven percent of the participants were African American. Annual assessments were completed on the 1,420 children until age 16. The youngest cohort was not interviewed at age 13, and only half of the youngest cohort was interviewed at age 14 because of funding limitations. Of 7,944 possible interviews during this period, 6,675 (84%) were completed. Four participants died, and 5.9% of participants only completed a single interview.
Interviews were completed by a parent figure and the participant to age 16. Before all interviews, parent and child signed informed consent/assent forms approved by the Duke University Medical Center Institutional Review Board. All interviewers had bachelor-level degrees, received one month of training, and had audio recordings of all interviews reviewed by a senior interviewer.
Childhood/Adolescent Irritability
The proposed tonic component of irritability consists of a persistently angry, grumpy, or grouchy mood. The phasic component refers to behavioral outbursts of intense anger. This study used an ongoing longitudinal study of development to examine these constructs post hoc. The full operational definition of each irritability component is provided in Table 1. The items used to operationalize the tonic and phasic components were assessed with the Child and Adolescent Psychiatric Assessment (CAPA)26, 27 interview completed with a parent figure and the child. As is currently the standard practice in child and adolescent psychiatric research, a construct was counted as being present if it was reported by either the parent or child. To minimize recall bias and forgetting, the timeframe for determining the presence of all irritabilityrelated constructs was the preceding 3 months; however, onset dates were collected for all items.
Table 1.
Operational Definitions of Tonic and Phasic Irritability
| Irritability | Construct | Definition | CAPA Items |
|---|---|---|---|
| Phasic | Temper tantrum | Discrete episodes of excessive temper, frustration or upset, manifested by shouting, crying or stamping, and involving violence or attempts at damage directed against people or property. | p/cge1i01, p/cge1f01, p/cge1f02, p/cge1f03, p/cge1d01, p/cge1o01 |
| Temper outburst | Discrete episodes of temper manifested by shouting or name calling but without violence and not meeting criteria for a temper tantrum. | p/cge0i01, p/cge0f02, p/cge0f03, p/cge0f04, p/cge0o01 | |
| Tonic | Irritability | Increased ease of precipitation of externally directed feelings of anger, bad temper, short temper, resentment, or annoyance. This rating is of a change in the child’s usual liability to be precipitated into anger. | p/cda8i01, p/cda8f01, p/cda8d01, p/cda8o01 |
| Touchy/easily annoyed | The child is generally more prone to FEELINGS of anger bad temper, short temper, resentment, sulking or annoyance, UNDER MINOR PROVOCATION than most children. This pattern need not represent a change in behavior. | p/cda6i01, p/cda6f01, p/cda6d01, p/cda6o01 | |
| Angry/resentful | The child is generally more prone to MANIFESTATIONS of anger or resentment (such as snappiness, shouting, quarreling or sulking) under minor provocation, than most children. This pattern need not represent a change in behavior. | p/cda7i01, p/cda7f01, p/cda7d01, p/cda7o01 |
Note: All assessed 4 to 7 times between ages 9 and 16 by structured interview with the child and their parent. Phasic constructs involved assessment of frequency in three settings (home, school, elsewhere), duration of episodes, and onset. Tonic constructs involved assessment of frequency, duration, and onset. Although the irritability items (p/cda8i01) require a change from typical liability and thus may not be considered strictly tonic, less than 1% of tonic cases were instances in which children reported this item alone. CAPA = Child and Adolescent Psychiatric Assessment.
The intercorrelations between the individual CAPA items are provided in Table S1, available online. Any phasic irritability was defined as reporting either a recent temper outburst or tantrum; any tonic irritability was defined as reporting irritable mood, being touchy or easily annoyed, or being angry/resentful. Associated features of these constructs assessed include duration, frequency onset, quality (violent or nonviolent for phasic outbursts only), and cross-context variability (phasic only). For phasic irritability, frequency is divided between home, school, and elsewhere. Onsets were the lowest-reported age of onset across all observations where irritability was reported, thus there is only one value per participant.
Markers of caseness
Nine concurrent and longitudinal characteristics were used to measure the impact of different levels of irritability to clarify normative vs. problematic irritability. Parents and child were asked whether they believed the child’s symptoms constituted a “problem” and whether they thought the child needed help. After the CAPA interview, the child and parent completed reports on use of mental health services with the Child and Adolescent Services Assessment.28, 29 For this analysis, we included receipt of specialty mental health (psychiatric hospital, general hospital psychiatry unit, residential treatment facility, community outpatient mental health center, private professional, outpatient drug and alcohol treatment) services and school-based services (counselor/social worker, special classes for emotional or behavioral problems, vocational support).
The Child and Adolescent Burden Assessment was completed by the parent and asks about 24 potential burdens—problems or burdens in their own lives—related to their child’s problems.30, 31 Areas covered included expenses and financial difficulties, problems in their relationship with their spouse, restriction on activities, and decreased feelings of well-being. For the current analysis, a single item was used to indicate the presence of any parental perceived burden due to the child’s symptoms. Psychosocial impairment secondary to symptoms were assessed in 17 areas of functioning related to life at home, school, and elsewhere as part of the CAPA.32, 33 An item indicating any psychosocial impairment was used in the current analysis. School suspension was looked at separate from other impairments. Finally, indicators were included for the total number of nonoverlapping anxiety and depression symptoms.
Analytic strategy
Sampling weights were applied to adjust for differential probability of selection and to insure that results represent unbiased estimates for the original population from which the sample was drawn. All reported prevalence rates are weighted and all samples sizes are unweighted. In addition, sandwich-type variance corrections34 were applied to adjust for the parameter and variance effects induced by the sampling stratification. Weighted regression analyses were completed using PROC GENMOD in SAS 9.2.35 Associations with caseness markers are reported in odds ratios for dichotomous outcomes and means ratios for symptom scales.
RESULTS
Prevalence of Irritability
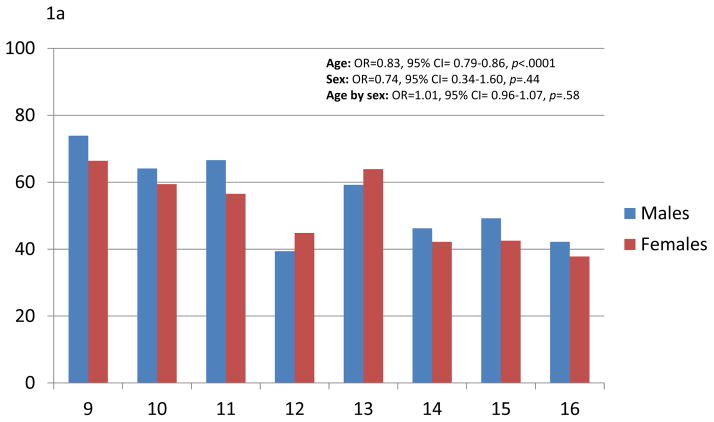
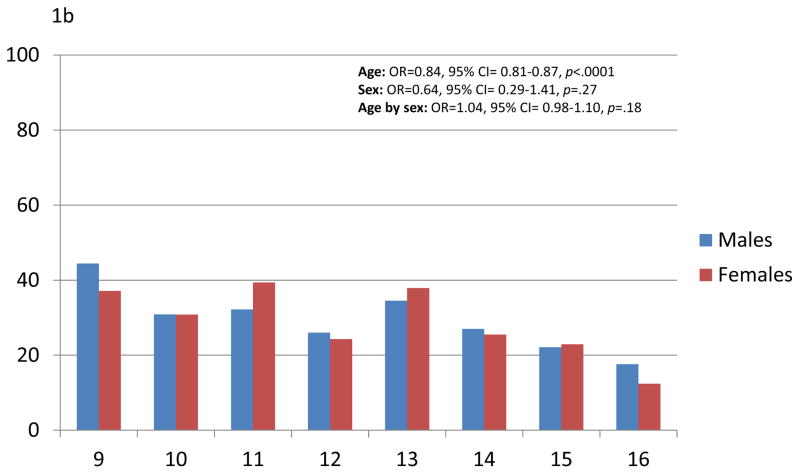
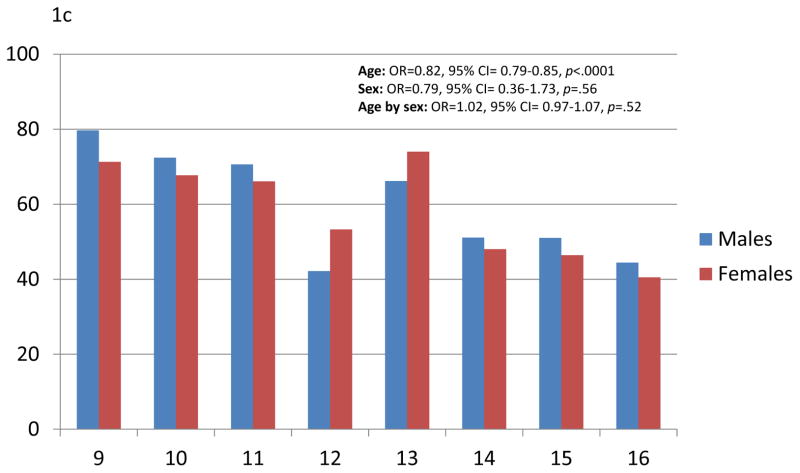
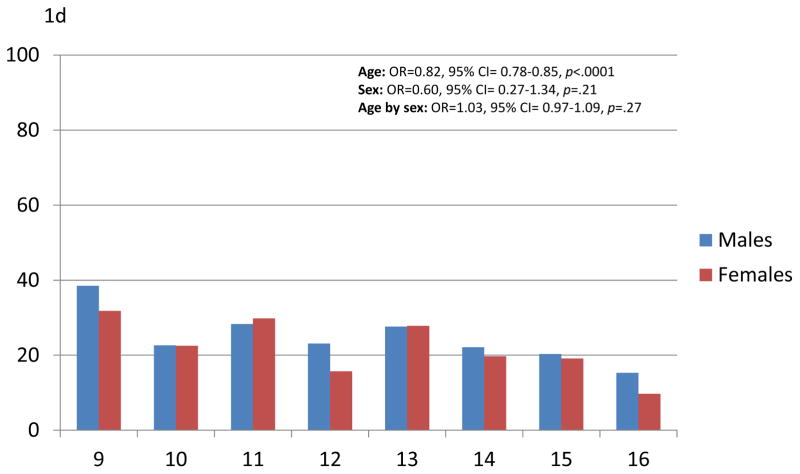
At any given point in childhood/adolescence, 51.4% (SE=1.4) of participants reported phasic irritability, 28.3% (SE=1.2) reported tonic irritability, 56.9% (SE=1.3) reported either, and 22.8% (SE=1.1) reported both. Figures 1A–D show the 3-month rates of any phasic irritability, tonic irritability, either or both, by age and sex. Rates of both types of irritability decreased significantly from middle childhood to adolescence but did not differ by sex. There was no evidence of age by sex interactions.
Figure 1.
Three-month prevalence rates of phasic (a) or tonic (b) irritability, either (c) or both (d) by age and sex. Note: OR = odds ratio.
The prevalence rates suggest that it is common to report some phasic and tonic irritability at any given point in time. Indeed, cumulatively across childhood and adolescence, the experience of irritability was nearly universal (see Table S2, available online): 86.8% reported phasic irritability at some point across childhood (n=1,236), 66.9% reported tonic irritability (n=1,000), 90.9% reported either tonic or phasic irritability (n=1,289), and 57.2% reported both tonic and phasic irritability (n=873). Again, there was no evidence of sex differences. Participants reported some type of irritability at a median of 3 assessments. It was only after reporting irritability at 6 or more assessments that one would be in the top 10% of participants.
Overlap between Phasic and Tonic irritability
It was most common to only report phasic irritability (28.7%; SE=1.1) alone, followed by those reporting both (22.8%; SE=1.1), and then solely reporting tonic irritability (5.3%; SE=0.5) alone. In other words, phasic irritability commonly presented by itself, whereas tonic irritability rarely presented without phasic irritability. The overlap was much greater than expected by chance (OR=5.8, 95% CI, 4.8–6.9, p <.0001). The overlap of frequency distributions was similarly high (mean ratio=1.2, 95% CI, 1.2–1.2, p <.0001).
Cumulatively across childhood, it was most common to report both tonic and phasic irritability concurrently (62.9%; SE=2.2), with much smaller groups reporting solely phasic (24.0%; SE=2.0) or 4.1% (SE=0.9) reporting tonic only. Again, the level of overlap was much greater than expected by chance (OR=5.8, 95% CI, 3.3–10.5, p <.0001). Figure S1a, available online, shows the levels of co-occurrence for those reporting either phasic or tonic irritability at any given assessment and cumulatively. Phasic irritability solely occurred some of the time, whereas tonic irritability rarely occurred alone. Figure S1b, available online, shows the cumulative overlap by the number of individual assessments at which an individual endorsed tonic or phasic irritability. The more often an individual reported tonic or phasic irritability, the more likely s/he was to also report the other type of irritability. In prospective observations, there was no set temporal presentation (Figures S2a–b, available online).
Continuity over time
Test of continuity tells us how stable a construct is over time. Continuity may be involve the same irritability component (homotypic; e.g., tonic to tonic), or a different component (heterotypic; e.g., tonic to phasic). Levels of both homotypic and heterotypic continuity were significant, suggesting significant stability in irritability (see Table S3, available online). Heterotypic continuity was even supported in adjusted models predicting current irritability from both past tonic and phasic irritability simultaneously. A participant with tonic irritability at one time point had a 71.3% likelihood of having either tonic or phasic irritability at 1-year follow-up. For those with phasic irritability, the likelihood was 75.6%.
Irritability features: Onset, Duration, Frequency, and Cross-context variability (phasic only)
Table 2 shows the weighted quantile thresholds for frequency, duration, and onsets for tonic and phasic irritability. Quantiles only include participants positive for the given irritability component. Duration and frequency are presented for two age bands: 9–12 and 13–16. Onsets were the lowest reported age of onset across all observations where irritability was reported, thus there is only one value per participant. Although phasic irritability was common overall, the typical frequency of phasic events was low with a median of 1 every 2 weeks. Conversely, tonic irritability was less common, but those reporting such irritability typically had 2–3+ occurrences per week. Neither frequency levels for tonic nor phasic irritability varied by either age (tonic: p = .09; phasic: p =.11) or sex (tonic: p = .68; phasic: p =.13).
Table 2.
Frequency, Duration, and Onset of Phasic and Tonic Irritability by Weighted Quantiles for Participants Reporting Either Tonic or Phasic Irritability
| 3-Month Frequency | Average Duration (in minutes) | Onset (in years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Phasic | Tonic | Phasic | Tonic | Phasic | Tonic | |||||||||
| Quantiles | 9–12 | 13–16 | Total | 9–12 | 13–16 | Total | 9–12 | 13–16 | Total | 9–12 | 13–16 | Total | Total | Total |
| 95% | 90 | 93 | 91 | 240 | 270 | 270 | 49.8 | 60 | 60 | 120 | 270 | 180 | 0.0 | 0.0 |
| 90% | 40 | 49 | 48 | 138 | 180 | 180 | 30 | 30 | 30 | 60 | 150 | 120 | 0.0 | 0.0 |
| 75% | 15 | 18 | 16 | 90 | 90 | 90 | 15 | 15 | 15 | 30 | 60 | 45 | 2.0 | 2.5 |
| 50%/Median | 6 | 6 | 6 | 26 | 36 | 36 | 7.2 | 5 | 5 | 11 | 18 | 15 | 4.5 | 5.5 |
| 25% | 2 | 3 | 2 | 12 | 12 | 12 | 3 | 2 | 2 | 5 | 7 | 5 | 7.5 | 9.5 |
Note: Frequency threshold heuristics: 13 ≤ Up to once a week; 45 = More days than not; 90 = Once a day; 180 ≥ 2+ times per day.
Consistent with their definitions, phasic occurrences were shorter than tonic events, but there was also substantial overlap such that those in the tip 75th percentile for phasic duration were at the median for tonic duration. There was some evidence that tonic but not phasic events have a longer duration in adolescence than middle childhood (tonic: p = .001; phasic: p =.11). There were no sex differences in duration for either (tonic: p = .53; phasic: p =.66).
Onsets for either type of irritability typically occurred quite early with a substantial subset (10%) reporting that they could not recall a time without irritability. For those endorsing phasic events, 15.9% (SE=1.1), they reported such incidents in more than one setting, typically home and school, and 11.3% (SE=1.0) endorsed incidents that involved violence. Both features were more common for males (multiple settings: 19.5% vs. 13.2%, p=.006; violence: 15.5% vs. 8.1%, p=.002).
What level of irritability is normative?
Based upon descriptive analyses, we tested the effect of different thresholds for predicting nine markers of caseness concurrently (see Table 3; additional analyses based on frequency, onset, duration, violence, and multiple settings in Tables S4–S7, available online). Onset was defined once all observations were available and thus was not associated with a given observation, as was the case for other thresholds. For caseness markers, we chose measures commonly used to measure the impact of a psychiatric disorder. In concurrent associations, every threshold group -- which varied from 7–50% of the sample -- was significantly associated with higher levels of every concurrent marker. Association patterns indicate that simply endorsing any tonic or phasic irritability identifies a group of children with current disrupted functioning. In follow-up analyses testing an interaction term between different irritability thresholds and developmental period (9–12 vs. 13–16), there was no evidence that risk for markers differed from childhood to adolescence.
Table 3.
Concurrent Associations Between Different Irritability Groups and Markers of Caseness
| Any Tonic | Any Phasic | Empirical Thresholds for Either Component | |||
|---|---|---|---|---|---|
| 90% Frequency | 90% Duration | 90% Onset | |||
| % of sample (# obs) | 27.5% (2148) | 51.2% (3485) | 7.0% (645) | 6.4% (506) | 22.9% (1591) |
| Caseness marker | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Perceived problem | 6.3 (4.7–8.6)*** | 3.5 (2.4–5.1)*** | 5.4 (3.7–7.8)*** | 4.3 (2.8–6.7)*** | 2.0 (1.5–2.9)*** |
| Perceived need for help | 7.0 (4.9–9.9)*** | 3.7 (2.5–5.6)*** | 3.9 (2.7–5.9)*** | 4.2 (2.6–6.8)*** | 2.0 (1.3–2.9)*** |
| Specialty MH services | 2.6 (2.0–3.5)*** | 1.9 (1.4–2.6)*** | 2.5 (1.5–4.1)*** | 2.3 (1.3–4.1)** | 1.6 (1.0–2.5)* |
| School services | 2.0 (1.6–2.7)*** | 2.3 (1.7–3.1)*** | 1.5 (1.1–2.2)** | 1.8 (1.2–2.9)* | 1.6 (1.2–2.3)** |
| School suspension | 1.8 (1.4–2.3)*** | 1.7 (1.4–2.2)*** | 2.2 (1.5–3.1)*** | 1.9 (1.2–3.0)** | 1.8 (1.3–2.5)** |
| Parental burden | 2.5 (1.9–3.1)*** | 1.9 (1.5–2.4)*** | 3.1 (2.3–4.4)*** | 2.9 (2.0–4.1)*** | 1.8 (1.4–2.5)*** |
| Any impairment | 2.2 (1.8–2.7)*** | 1.9 (1.6–2.2)*** | 2.6 (2.0–3.5)*** | 2.0 (1.4–2.8)*** | 1.7 (1.3–2.3)*** |
| Anxiety sxa.‡ | 2.2 (1.9–2.6)*** | 1.9 (1.6–2.2)*** | 2.0 (1.7–2.3)*** | 2.4 (2.0–3.0)*** | 1.4 (1.2–1.6)*** |
| Depression sxa.‡ | 1.8 (1.6–2.0)*** | 1.4 (1.2–1.5)*** | 1.9 (1.6–2.3)*** | 2.2 (1.9–2.5)*** | 1.5 (1.2–1.8)*** |
Note: MH = mental health; Obs = observations; sx = symptoms.
Ratios for symptoms are mean ratios rather than odds ratios (ORs).
p≤.05;
p≤ .01;
p ≤ .001.
Table 4 presents prospective associations at one-year follow-up in models controlling for current status. Thus, significant associations suggest that baseline irritability levels are predictive over and beyond what is known about current irritability. There was evidence of widespread effects, but these effects were generally stronger for higher thresholds (i.e., scoring at or above the 90th percentile for duration) and tonic versus phasic irritability. The longitudinal effects were strongest (OR ≥ 2.0 for 2+ groups) for perception of a problem, need for help, use of specialty mental health services, and use of school services. Additional analyses of other thresholds are available in Tables S8–S10, available online.
Table 4.
Longitudinal Associations Between Empirically-Derived Thresholds for Irritability and Markers of Caseness at 1-Year Follow-Up
| Any Tonic | Any Phasic | Empirical Thresholds for Either Component | ||
|---|---|---|---|---|
| 90% either | 90% either | |||
| Caseness marker | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Perceived problem | 1.5 (1.0–2.2)* | 1.3 (0.9–1.9) | 2.5 (1.6–3.8)*** | 2.1 (1.3–3.3)** |
| Perceived need for help | 1.6 (1.1–2.2)** | 1.3 (0.9–1.8) | 2.2 (1.3–3.6)** | 2.8 (1.7–4.7)*** |
| Specialty MH services | 2.1 (1.4–3.1)*** | 1.8 (1.2–2.6)** | 2.8 (1.7–4.4)*** | 2.3 (1.3–4.1)** |
| School services | 1.7 (1.2–2.3)** | 1.4 (1.0–2.0) | 2.2 (1.4–3.3)*** | 1.7 (1.0–2.9)* |
| School suspension | 1.5 (1.1–2.0)* | 1.0 (0.8–1.3) | 1.6 (1.1–2.3)** | 1.9 (1.2–3.0)** |
| Parental burden | 1.4 (1.1–1.7)** | 1.1 (0.8–1.4) | 1.2 (0.8–1.7) | 2.0 (1.4–2.9)*** |
| Any impairment | 1.5 (1.2–1.9)*** | 1.0 (0.8–1.2) | 1.4 (1.0–2.0) | 2.0 (1.4–2.8)*** |
| Anxiety sxa | 1.3 (1.1–1.5)* | 1.2 (1.0–1.4)* | 1.2 (0.9–1.4) | 1.6 (1.2–2.0)*** |
| Depression sxa | 1.2 (1.1–1.4)** | 1.2 (1.1–1.3)** | 1.0 (0.9–1.3) | 1.3 (1.1–1.5)** |
Note: All analyses controlled for current irritability levels. MH = mental health; sx = symptoms.
Ratios for symptoms are mean ratios rather than odds ratios (ORs).
p≤.05;
p≤ .01;
p ≤ .001.
DISCUSSION
Despite its ubiquity, little is known about how irritability and its components manifest in the community. Irritability is symptom of oppositional defiant disorder, disruptive mood dysregulation disorder, posttraumatic stress disorder, generalized anxiety disorder, and major depressive episodes, manic episodes, and associated features of many other disorders. This prospective, longitudinal study found that irritability is relatively common, decreases with age but does not vary by sex, and at almost any level is associated with a profile of disrupted functioning commonly seen with psychiatric disorders.
Previous work has suggested that irritability is common in childhood,4, 19, 24 including a study of disruptive mood dysregulation disorder in this sample.36 However, a number of aspects of our prevalence findings were surprising. First, the prevalence of both tonic and phasic irritability decreased with age. It is reasonable to expect phasic outbursts to decrease with age and increasing behavioral control, but adolescence is associated with increases in the rates of depression and generalized anxiety,37, 38 two disorders in which irritable mood is a prominent feature. In contrast to longstanding notions of mood lability during adolescence,39 this is a period where irritability—in either tonic or phasic form—is declining. Despite these overall changes, the frequency of either tonic or phasic events for those reporting irritability were similar to what was observed in childhood, although there was some evidence that tonic events were somewhat longer in adolescence. Perhaps most importantly, there was no evidence that risk for caseness markers differed from childhood to adolescence: The implications of developmental variation in irritability during this period for risk are modest. Levels of irritability did not differ by sex. Throughout childhood and adolescence behavioral disorders are significantly more common in boys than in girls, and emotional disorders are typically more common in girls after puberty.40 Irritability appears to be relatively distinct among childhood traits, displaying similar rates even when dissected into its respective components.
One goal of this analysis was to better understand the interplay between the components of irritability as proposed at a recent NIMH workshop.17 The overlap was consistent with levels of overlap seen between common childhood psychiatric disorders (which are also much less common).41 This overlap increased with the number of times irritability was reported. Furthermore, tonic irritability was as likely to predict tonic as phasic irritability at one-year follow-up, and vice versa. Finally, tonic and phasic irritability (and their respective features) tended to display similar associations with a broad range of caseness markers. Once thresholds were applied to account for the fact that phasic irritability is more common than tonic irritability, these components were largely interchangeable in terms of identifying children at risk. Even a simple yes/no for recent tonic or phasic irritability was sufficient to identify participants at risk at 2- to 5-fold risk for a range of markers. The 90th percentile duration thresholds were the best predictors of marker status at 1-year follow-up, but there was less evidence of strong linear effect of these thresholds than might have been expected. It is not clear either component is more pernicious than the other, and this question may be moot, given the high levels of overlap seen in the community throughout development. Indeed, increased research on individuals presenting with both tonic and phasic irritability may be most promising.
It is reasonable to ask whether the tonic/phasic distinction and its terminology is useful and valid. Our findings suggest similar intercorrelations between phasic and tonic items as within the constructs. Furthermore, the tonic and phasic distinction is primarily used in medicine to distinguish between the action of receptors, how quickly they respond, and the duration of their response.42 This would imply that tonic irritability would be a common background state punctuated by less frequent phasic outbursts. In this study, however, it was more common to report phasic events without any tonic irritability at all and the duration of tonic events were only about twice as long as that of phasic events, hardly suggesting a persistent state (except in very uncommon cases). In this sense, the nomenclature introduces assumptions that are not entirely consistent with the normative presentation of these constructs. This suggests 1) that it may be more useful to use descriptive language for these components (such as “irritable mood,” “temper outbursts”) and 2) that our assumptions about the interplay between irritable mood and outbursts may require reevaluation.
The strengths of the sampling procedure, study design, and assessment protocol have been discussed in detail,38 but the current sample is only representative of children from the area sampled, not all children in the US. While the study is able to look at irritability across middle childhood and adolescence, it is clear that many children have already displayed significant levels of irritability by middle childhood.43,44 The assessments sought to maximize accuracy of recall by focusing on a limited 3-month period, but this leaves 9 months unassessed between annual interviews. As such, our estimates are likely to represent the lower limit of the burden of irritability. Finally and most importantly, this study was not developed to study irritability itself, but common childhood psychopathology of which both tonic and phasic irritability are features.
Understanding the distinction between normative and non-normative manifestations of irritability enables clinicians, parents, and school personnel to determine which children may require clinical attention. By focusing on a range of cutoffs associated with frequency, duration, and onset, this study provides an important first step in addressing the question of how much is too much. Most of the thresholds studied could be assessed in a few minutes and require little expertise but can identify children at risk for problems up to a year later. Even low thresholds predicted disrupted functioning, suggesting irritability may provide a useful window for clinicians as to how well a child is navigating the core developmental tasks of emotional and behavioral regulation.45,46 Irritability appears to be a key transdiagnostic construct for understanding children at risk. For researchers, our findings highlight the importance of studying the full spectrum of irritability and challenge notions about how irritable mood and outbursts present and their interplay. The consequences of focusing on severe irritability may be missing the vast majority of struggling children. Community samples with broad distributions of irritability may be best positioned to study the development of irritability, its trajectory over time, and relations to other developmental constructs. Future studies should continue to examine the phenomenology of irritability, as well as neural, behavioral, and psychosocial underpinnings.
Supplementary Material
Supplemental Figure 1. Overlap between phasic and tonic irritability components at any given wave and cumulatively across childhood and adolescence (a). Figure 1b looks at the overlap cumulatively based upon the number of assessments with reported tonic or phasic irritability.
Supplemental Figure 2. Temporal sequence of irritability presentation for tonic cases (a) and phasic cases (b).
Table S1. Intercorrelations Between Individual Child and Adolescent Psychiatric Assessment (CAPA) Items Used to Define Irritability Components
Table S2. Cumulative Rates of Irritability Across All Childhood and Adolescent Observations
Table S3. Homotypic and Heterotypic Continuity in Irritability and Its Components
Table S4. Concurrent Associations Between Various Empirically-Derived Frequency Thresholds for Irritability and Markers of Caseness
Table S5. Concurrent Associations Between Empirically-Derived Onset Thresholds for Irritability and Markers of Caseness
Table S6. Concurrent Associations Between Empirically-Derived Duration Thresholds for Irritability and Markers of Caseness
Table S7. Concurrent Between Cross-Context Phasic Episodes and Violent Outbursts and Markers of Caseness
Table S8. Longitudinal Associations Between Empirically-Derived Frequency Thresholds for Irritability and Markers of Caseness at 1-Year Follow-Up
Table S9. Longitudinal Associations Between Empirically-Derived Duration Thresholds for Irritability and Markers of Caseness at 1-Year Follow-Up
Table S10. Longitudinal Associations Between Irritability Features and Markers of Caseness at 1-Year Follow-Up
Acknowledgments
The work presented here was supported by the National Institute of Mental Health (MH63970, MH63671, MH48085, MH094605), the National Institute on Drug Abuse (DA/MH11301), NARSAD (Early Career Award to First Author), and the William T Grant Foundation.
The authors would like to thank the participants of the Great Smoky Mountains Study and their families for their longstanding involvement in this study. Dr. Copeland had full access to all the data in the study, performed all statistical analyses, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Supplemental material cited in this article is available online.
Disclosure: Dr. Copeland has received research support from the National Institute of Mental Health, the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and the National Alliance for Research on Schizophrenia and Depression. Dr. Brotman has received research support from the National Institute of Mental Health. Dr. Costello has received research support from the National Institute of Mental Health and the National Institute on Drug Abuse. She was co-recipient of the 2009 National Alliance for Research on Schizophrenia and Depression Ruane Prize for Outstanding Child and Adolescent Psychiatric Research. She is co-author of the following assessment tools: Child and Adolescent Psychiatric Assessment (CAPA), Young Adult Psychiatric Assessment (YAPA), Child and Adolescent Impact Assessment (CAIA), Child and Adolescent Services Assessment (CASA), and Mood and Feelings Questionnaire (MFQ). No personal income is derived from any of these measures.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. William E. Copeland, Duke University Medical Center, Durham, NC.
Dr. Melissa A. Brotman, Emotion and Development Branch at the National Institute of Mental Health, Bethesda, MD.
Dr. E. Jane Costello, Duke University Medical Center, Durham, NC.
References
- 1.Leibenluft E. Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. The American journal of psychiatry. 2011;168(2):129–142. doi: 10.1176/appi.ajp.2010.10050766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stringaris A. Irritability in children and adolescents: a challenge for DSM-5. European child and adolescent psychiatry. 2011;20(2):61–66. doi: 10.1007/s00787-010-0150-4. [DOI] [PubMed] [Google Scholar]
- 3.Fava M, Hwang I, Rush AJ, Sampson N, Walters EE, Kessler RC. The importance of irritability as a symptom of major depressive disorder: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(8):856–867. doi: 10.1038/mp.2009.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pickles A, Aglan A, Collishaw S, Messer J, Rutter M, Maughan B. Predictors of suicidality across the life span: the Isle of Wight study. Psychol Med. 2010;40(9):1453–1466. doi: 10.1017/S0033291709991905. [DOI] [PubMed] [Google Scholar]
- 5.Stringaris A, Maughan B, Copeland WS, Costello EJ, Angold A. Irritable mood as a symptom of depression in youth: prevalence, developmental, and clinical correlates in the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2013;52(8):831–840. doi: 10.1016/j.jaac.2013.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Judd LL, Schettler PJ, Coryell W, Akiskal HS, Fiedorowicz JG. Overt irritability/anger in unipolar major depressive episodes: past and current characteristics and implications for long-term course. JAMA Psychiatry. 2013;70(11):1171–1180. doi: 10.1001/jamapsychiatry.2013.1957. [DOI] [PubMed] [Google Scholar]
- 7.Derks EM, Dolan CV, Hudziak JJ, Neale MC, Boomsma DI. Assessment and etiology of attention deficit hyperactivity disorder and oppositional defiant disorder in boys and girls. Behavior genetics. 2007;37(4):559–566. doi: 10.1007/s10519-007-9153-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loeber R, Burke JD. Developmental Pathways in Juvenile Externalizing and Internalizing Problems. Journal of research on adolescence: the official journal of the Society for Research on Adolescence. 2011;21(1):34–46. doi: 10.1111/j.1532-7795.2010.00713.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stringaris A, Baroni A, Haimm C, et al. Pediatric bipolar disorder versus severe mood dysregulation: risk for manic episodes on follow-up. J Am Acad Child Adolesc Psychiatry. 2010;49(4):397–405. [PMC free article] [PubMed] [Google Scholar]
- 10.Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry. 2009;166(9):1048–1054. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Althoff RR, Verhulst FC, Rettew DC, Hudziak JJ, van der Ende J. Adult outcomes of childhood dysregulation: a 14-year follow-up study. J Am Acad Child Adolesc Psychiatry. 2010;49:1105–1116. doi: 10.1016/j.jaac.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stringaris A, Goodman R. Mood lability and psychopathology in youth. Psychol Med. 2009;39(8):1237–1245. doi: 10.1017/S0033291708004662. [DOI] [PubMed] [Google Scholar]
- 13.Copeland WE, Shanahan L, Egger H, Angold A, Costello EJ. Adult Diagnostic and Functional Outcomes of DSM-5 Disruptive Mood Dysregulation Disorder. Am J Psychiatry. 2014;171(6):668–674. doi: 10.1176/appi.ajp.2014.13091213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leibenluft E, Cohen P, Gorrindo T, Brook JS, Pine DS. Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol. 2006;16(4):456–466. doi: 10.1089/cap.2006.16.456. [DOI] [PubMed] [Google Scholar]
- 15.Buss AH, Durkee A. An inventory for assessing different kinds of hostility. Journal of consulting psychology. 1957;21(4):343–349. doi: 10.1037/h0046900. [DOI] [PubMed] [Google Scholar]
- 16.Snaith RP, Taylor CM. Irritability: definition, assessment and associated factors. The British journal of psychiatry: the journal of mental science. 1985;147:127–136. doi: 10.1192/bjp.147.2.127. [DOI] [PubMed] [Google Scholar]
- 17.Leibenluft E, Avenevoli S. Paper presented at: National Institute of Mental Health workshop Childhood Irritability and the Pathophysiology of Mental Illness; 2014; Bethesda, Maryland. [Google Scholar]
- 18.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington: University of Vermont Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- 19.Dougherty LR, Smith VC, Bufferd SJ, et al. Preschool Irritability: Longitudinal Associations With Psychiatric Disorders at Age 6 and Parental Psychopathology. J Am Acad Child Adolesc Psychiatry. 2013;52:1304–1313. doi: 10.1016/j.jaac.2013.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brotman MA, Schmajuk M, Rich BA, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biological psychiatry. 2006;60(9):991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 21.Leibenluft E, Charney DS, Towbin KE, Bhangoo RK, Pine DS. Defining clinical phenotypes of juvenile mania. The American journal of psychiatry. 2003;160(3):430–437. doi: 10.1176/appi.ajp.160.3.430. [DOI] [PubMed] [Google Scholar]
- 22.Copeland WE, Angold A, Costello EJ, Egger H. Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. Am J Psychiatry. 2013;170(2):173–179. doi: 10.1176/appi.ajp.2012.12010132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dougherty L, Smith V, Bufferd S, et al. DSM-5 disruptive mood dysregulation disorder: correlates and predictors in young children. Psychological Medicine. 2014:1–12. doi: 10.1017/S0033291713003115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiggins JL, Mitchell C, Stringaris A, Leibenluft E. Developmental Trajectories of Irritability and Bidirectional Associations With Maternal Depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53(11):1191–1205. e1194. doi: 10.1016/j.jaac.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 26.Angold A, Prendergast M, Cox A, Harrington R, Simonoff E, Rutter M. The Child and Adolescent Psychiatric Assessment (CAPA) Psychological Medicine. 1995;25:739–753. doi: 10.1017/s003329170003498x. [DOI] [PubMed] [Google Scholar]
- 27.Angold A, Costello E. The Child and Adolescent Psychiatric Assessment (CAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- 28.Ascher BH, Farmer EMZ, Burns BJ, Angold A. The Child and Adolescent Services Assessment (CASA): Description and psychometrics. Journal of Emotional and Behavioral Disorders. 1996;4:12–20. [Google Scholar]
- 29.Burns BJ, Angold A, Magruder-Habib K, Costello EJ, Patrick MKS. The Child and Adolescent Services Assessment (CASA): Version 3.0. Durham, NC: Duke University Medical Center; 1992. [Google Scholar]
- 30.Messer SC, Angold A, Costello EJ, Burns BJ. The Child and Adolescent Burden Assessment (CABA): Measuring the family impact of emotional and behavioral problems. International Journal of Methods in Psychiatric Research. 1996;6:261–284. [Google Scholar]
- 31.Angold A, Messer SC, Stangl D, Farmer EMZ, Costello EJ, Burns BJ. Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health. 1998;88:75–80. doi: 10.2105/ajph.88.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative Prevalence of Psychiatric Disorders by Young Adulthood: A Prospective Cohort Analysis From the Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(3):252–261. doi: 10.1016/j.jaac.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Angold A, Costello EJ, Farmer EMZ, Burns BJ, Erkanli A. Impaired but undiagnosed. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:129–137. doi: 10.1097/00004583-199902000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Pickles A, Dunn G, Vazquez-Barquero J. Screening for stratification in two-phase (‘two-stage’) epidemiological surveys. Statistical Methods in Medical Research. 1995;4(1):73–89. doi: 10.1177/096228029500400106. [DOI] [PubMed] [Google Scholar]
- 35.SAS/STAT® Software: Version 9 [computer program] Cary, NC: SAS Institute, Inc; 2004. [Google Scholar]
- 36.Copeland WE, Angold A, Costello EJ, Egger H. Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. American Journal of Psychiatry. 2013;170(2):173–179. doi: 10.1176/appi.ajp.2012.12010132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological Bulletin. 1994;115(3):424–441. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- 38.Copeland WE, Angold A, Shanahan L, Costello EJ. Longitudinal Patterns of Anxiety From Childhood to Adulthood: The Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2014;53:21–33. doi: 10.1016/j.jaac.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Steinberg L, Sheffield Morris A. Adolescent development. Annual Review of Psychology. 2001;52:83–110. doi: 10.1146/annurev.psych.52.1.83. [DOI] [PubMed] [Google Scholar]
- 40.Eme RF. Sex differences in childhood psychopathology: A review. Psychological Bulletin. 1979;86(3):574–595. [PubMed] [Google Scholar]
- 41.Copeland WE, Shanahan L, Erkanli A, Costello EJ, Angold A. Indirect comorbidity in childhood and adolescence. Frontiers in psychiatry. 2013;4:144. doi: 10.3389/fpsyt.2013.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kardong KV. Vertebrates: comparative anatomy, function, evolution. Boston: McGraw-Hill; 2006. [Google Scholar]
- 43.Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. Journal of Child Psychiatry and Psychology. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- 44.Keenan K, Wakschlag LS. Are oppositional defiant and conduct disorder symptoms normative behaviors in preschoolers? A comparison of referred and nonreferred children. American Journal of Psychiatry. 2004;161:356–358. doi: 10.1176/appi.ajp.161.2.356. [DOI] [PubMed] [Google Scholar]
- 45.Kochanska G, Coy KC, Murray KT. The development of self-regulation in the first four years of life. Child Development. 2001;72:1091–1111. doi: 10.1111/1467-8624.00336. [DOI] [PubMed] [Google Scholar]
- 46.Sroufe LA. An organizational perspective on the self. In: Cicchetti D, Beeghly M, editors. The Self In Transition: Infancy to Childhood. Chicago: University of Chicago Press; 1990. pp. 281–307. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Overlap between phasic and tonic irritability components at any given wave and cumulatively across childhood and adolescence (a). Figure 1b looks at the overlap cumulatively based upon the number of assessments with reported tonic or phasic irritability.
Supplemental Figure 2. Temporal sequence of irritability presentation for tonic cases (a) and phasic cases (b).
Table S1. Intercorrelations Between Individual Child and Adolescent Psychiatric Assessment (CAPA) Items Used to Define Irritability Components
Table S2. Cumulative Rates of Irritability Across All Childhood and Adolescent Observations
Table S3. Homotypic and Heterotypic Continuity in Irritability and Its Components
Table S4. Concurrent Associations Between Various Empirically-Derived Frequency Thresholds for Irritability and Markers of Caseness
Table S5. Concurrent Associations Between Empirically-Derived Onset Thresholds for Irritability and Markers of Caseness
Table S6. Concurrent Associations Between Empirically-Derived Duration Thresholds for Irritability and Markers of Caseness
Table S7. Concurrent Between Cross-Context Phasic Episodes and Violent Outbursts and Markers of Caseness
Table S8. Longitudinal Associations Between Empirically-Derived Frequency Thresholds for Irritability and Markers of Caseness at 1-Year Follow-Up
Table S9. Longitudinal Associations Between Empirically-Derived Duration Thresholds for Irritability and Markers of Caseness at 1-Year Follow-Up
Table S10. Longitudinal Associations Between Irritability Features and Markers of Caseness at 1-Year Follow-Up