Abstract
Background:
Infection prevention and control measures are critical to prevent the possible spread of Middle East Respiratory Syndrome-coronavirus (MERS-CoV) in healthcare facilities. Therefore, healthcare workers should be aware of all procedures concerning prevention of and protection from MERS-CoV.
Objective:
The aim of this study is to improve the knowledge of the dental students and evaluate their awareness about MERS-CoV.
Materials and Methods:
A questionnaire was made according to MOH information and 200 dental students (Al-Farabi Colleges, Jeddah) were interviewed to evaluate their knowledge about MERS-CoV.
Results:
More than half of the dental students (54%) interviewed had good knowledge about the etiology, symptoms, and treatment of MERS-CoV. Measurements for infection control and protection were also known (79%). The sources of information for the students were: college (27%), MOH (25%), media (24%), and social community (23%), while 17% of the students interviewed had no idea about it.
Conclusion:
Dental students had good knowledge about MERS-CoV. However, more information still must be provided by MOH and college for the medical staff.
Keywords: Aerosol infection, coronavirus, Middle east respiratory syndrome, respiratory infection-health-care workers, virus infection
INTRODUCTION
Middle East Respiratory Syndrome-coronavirus (MERS-CoV) is a major global concern. MERS-CoV was first reported in September 2012, when a novel β coronavirus was isolated from a Saudi Arabian patient in Jeddah, who had died of severe pneumonia and multiple organ failure in June 2012.[1] This novel coronavirus has been named Middle East Respiratory Syndrome-coronavirus.[2] MERS-CoV can also infect nonhuman primate, porcine, bat, civet, rabbit, and horse cell lines.[3,4,5]
Geographic distribution
Since April 2012, over 1100 laboratory-confirmed human infections with MERS-CoV have been reported to the World Health Organization (WHO), occurring in several countries in the Arabian Peninsula, including Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, the United Arab Emirates, and Yemen. The majority of cases (>85%) have occurred in Saudi Arabia, including some case clusters.[6,7] In the European and Asian countries as well as in Algeria, Egypt, Tunisia, and the United States, patients developed illness after returning from the Arabian Peninsula. There have been a total of 572 cases of MERS-CoV infection reported by WHO globally as of May 15, 2014, with 173 deaths (30% mortality rate).[8]
Possible sources and modes of transmission
Bats
Studies performed in Europe, Africa, and Asia, including the Middle East, have shown that coronavirus RNA sequences are found frequently in bat fecal samples and that some of these sequences are closely related to MERS-CoV sequences.[9,10,11]
Although bats might be a reservoir of MERS-CoV, it is unlikely that they are the immediate source for most human cases because human contact with bats is uncommon.[12]
Camels
As noted above, it is likely that camels serve as hosts for MERS-CoV. The strongest evidence of camel-to-human transmission of MERS-CoV comes from a study in Saudi Arabia, in which MERS-CoV was isolated from a man with fatal infection and from one of his camels; full-genome sequencing demonstrated that the viruses isolated from the man and his camel were identical.[13]
These results suggest that MERS-CoV can infect dromedary camels and can be transmitted from them to humans by close contact.
Camels in the Arabian Peninsula and in part of North and East Africa have been shown to carry the virus.[14] However, it is still too early to say definitely that they are the main source of primary infections in humans. Younger animals seem to be virus-positive more often than adult animals. As young camels lose their maternal immunity, they become more susceptible to MERS-CoV infection. The high number of MERS-CoV cases (229 cases) reported between April 11, 2014 and May 4, 2014 by Saudi Arabia were probably seasonal, related to the birthing season of camels.[15]
According to Ziad Memish, Saudi Arabia's Deputy, professor in the College of Medicine at Al Fasial University in Riyadh (See Reference: www.thelancet.com Volume 383/May 24/2014), “more than two-thirds of the primary human cases have no links to camels.” He suggested the possibility of another species in acting as an intermediary. After a bat of the Taphozous genus was found in a fragments of the MERS sequence,[14] bats have been accused as a possible source of transmission. But contacts between bats and people are rare, and this idea still needs more study and is considered a hypothesis.
Human-to-human transmission
More than half of all laboratory-confirmed secondary cases have been associated with healthcare settings.[16] The majority of cases in the spring of 2014 in Saudi Arabia were acquired through human-to-human transmission in healthcare settings, likely due, at least in part, to systemic weaknesses in infection control.[6,17,18]
Case definitions
For epidemiologic purposes, the following MERS-CoV infection case definitions have been proposed by the WHO:[19] Confirmed case by laboratory confirmation or Probable case by symptoms and signs.
Clinical manifestations
Incubation period
In an outbreak of MERS-CoV in Saudi Arabia that resulted in laboratory-confirmed MERS-CoV in 23 individuals, the median incubation period was 5.2 days (95% CI: 1.9–14.7 days).[20]
The WHO and the United States Centers for Disease Control and Prevention (CDC) recommend that an evaluation for MERS-CoV be considered in individuals with a syndrome of MERS who returned from travel to the Arabian peninsula or neighboring countries within the past 14 days.[21]
Clinical features
Most patients with MERS-CoV infection have been severely ill with pneumonia and acute respiratory distress syndrome, and some have had acute kidney injury.[1,21,22,23,24,25]
It remains unclear whether persons with specific conditions are disproportionately infected with MERS-CoV or have more severe disease.[26] In a study of 47 patients with MERS-CoV infection in Saudi Arabia, 45 (96%) had underlying comorbidities, including diabetes mellitus (68%), hypertension (34%), chronic cardiac disease (28%), and chronic kidney disease (49%).[25] The mortality rate is around 30%, and there is currently no vaccine or specific treatment available.[14]
People with diabetes, renal failure, chronic lung disease, and immunocompromised patients are considered to be at high risk of severe disease from MERS-CoV infection. Therefore, these people should avoid contact with camels, drinking camel's urine, or eating meat that has not been properly cooked.[27]
The WHO emergency committee concluded that the number of cases reported among healthcare workers from hospitals in Jeddah was amplified due to overcrowding and inadequate infection control measures.[28]
Acute viral respiratory tract infections, such as severe acute respiratory syndrome (SARS) and MERS, predominantly spread by large respiratory droplets (≥10 μm in diameter) during coughing and sneezing, whereas contact with fomite (including hand contamination) might be another potential source of transmission.[29,30]
The MERS-CoV outbreak in Jeddah and the importance of the knowledge of etiology and protection from MERS-CoV led us to conduct this study on dental students, with an aim to evaluate their knowledge and awareness of MERS-CoV.
Treatment
As with other coronaviruses, no antiviral agents are recommended for the treatment of MERS-CoV infection.[31] In a retrospective cohort study in patients with severe MERS-CoV infection, combination therapy with ribavirin and interferon alfa-2a, started a median of 3 days after diagnosis (20 patients), was associated with significantly improved survival at 14 days, compared with 24 patients who received only supportive care (70 vs 29% survival), but the outcome was not significant at 28 days (30 vs 17% survival, a nonsignificant difference).[32,33,34] It is difficult to interpret the results of this retrospective study, and further evaluation by conducting randomized trials is needed before treatment recommendations can be made.
Prevention
Infection control
The WHO and the CDC have issued recommendations for the prevention and control of MERS-CoV infections in healthcare settings.[35,36,37] An increased level of infection control precautions is recommended when caring for patients with probable or confirmed MERS-CoV infection, compared to that used for patients with community-acquired coronaviruses or other community-acquired respiratory viruses.
The WHO recommends that standard and droplet precautions must be used when caring for patients with acute respiratory tract infections.[35] Contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS-CoV infection. Airborne precautions should be used when performing aerosol-generating procedures. The CDC recommends the use of standard, contact, and airborne precautions for the management of hospitalized patients with known or suspected MERS-CoV infection.[26,36,37]
Interim home care and isolation
The CDC recommends that ill individuals who are being evaluated for MERS-CoV infection and do not require hospitalization may be cared for and isolated in their home.[38]
Avoiding camels
The WHO recommends that individuals at high risk of severe disease, such as immunocompromised hosts and those with diabetes, chronic lung disease, or pre-existing renal failure, should take precautions when visiting farms, barn areas, camel pens, or market environments where camels are present.[39] These measures include avoiding contact with camels, practicing good hand hygiene, avoiding drinking raw camel milk or camel urine, avoiding eating meat that has not been cooked thoroughly, and avoiding eating food that may be contaminated with animal secretions or products unless they are properly washed, peeled, or cooked.
Travel recommendations
The WHO does not recommend either special screening for MERS-CoV at points of entry or the application of any travel or trade restrictions. However, the WHO recommends that countries outside the affected region maintain a high level of vigilance, especially the ones with a large numbers of travelers or guest workers returning from the Middle East.[35]
MATERIALS AND METHODS
Study participants were recruited from among the dental students of Al-Farabi College, Jeddah (high level 9 + 10 - male and female) who are in direct contact with the patients and this was considered as the main criterion of selection.
The questionnaire contained 12 questions which were formulated based on the information given by MOH for MERS-CoV. The questionnaire was edited in English and distributed to the dental group (see the questionnaire in Appendix 1).
The questionnaire was divided into multiple sections to assess definition, symptoms, source of infection, infection control, protection, and treatment. The questionnaire included specific questions exploring the knowledge, such as rate of mortality, period of incubation, and way of spreading; a single-item scale was used to record the respondents’ replies.
RESULTS
There were 200 respondents in the study. The respondents comprised 81 (40%) male and 119 (60%) female. More than 73% (145) of respondents were under 25 years and 27% (55) were over 25 years of age. About 44% of respondents knew the definition of MERS as Middle East Respiratory Syndrome and 27% knew other definitions, while 18% of respondents had no idea. Furthermore, 27% of respondents had gained their knowledge about MERS from college and 25% from MOH, while 17% of respondents had no idea. The majority of respondents (75%) considered that MERS is contagious and 54% knew related symptoms such as severe acute respiratory illness, fever, cough, and gastrointestinal symptoms [Figure 1]. One-third of the respondents 27% were aware that the period of incubation for MERS is about 2–14 days.
Figure 1.
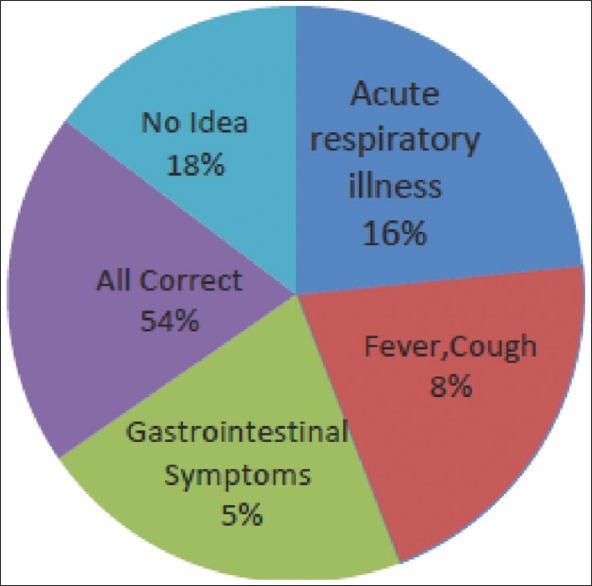
MERS-CoV symptoms
A sizable proportion (48%) of the respondents reported that the source of MERS-CoV is camels, 18% gave the answer as bats, and 32% had no idea [Figure 2]. More than two-thirds (64%) of the respondents knew that close contact with confirmed MERS patient spreads the infection and 79% applied methods of protection such as washing hands with alcohol sanitizer, using mask, goggles, and avoiding personnel contact with the confirmed patient [Figure 3]. Also, 52% of respondents could distinguish between SARS and MERS. One-third of the respondents reported that the percentage of death in MERS is about 30% and 77% knew that there is no vaccination for MERS. Also, two-thirds of the respondents (60%) considered that the treatment is supportive based on clinical condition of the patient.
Figure 2.
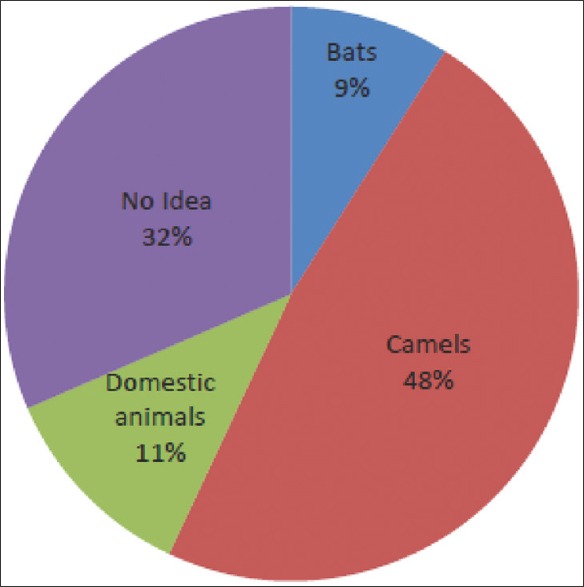
MERS-CoV Source of infection
Figure 3.
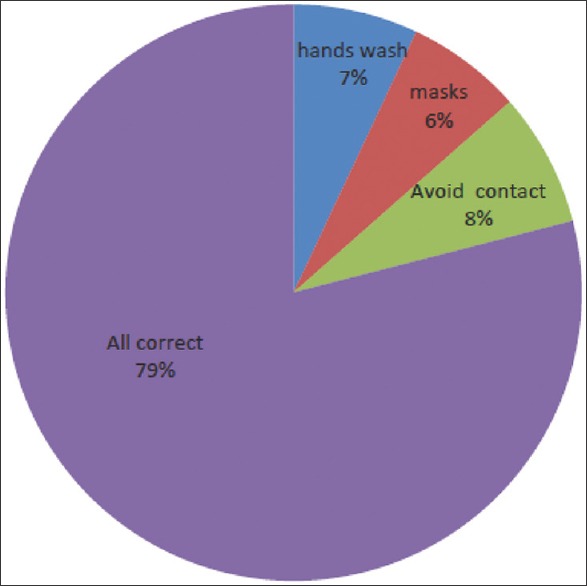
MERS-CoV ways of protection
DISCUSSION
Knowledge
The respondents in this study had higher education level (level 9–10 dental school) according to their level in dental school and were mainly female (60%), which indicates that females are more concerned with medical outbreak of the disease than males.
About 44% of respondents knew the definition of MERS and that MERS-CoV is an airborne pathogen, 54% recognized the symptoms, and 48% realized that the probable source of MERS virus is camels, while 64% were aware about the way of spreading by close contact and 79% had knowledge of instructions and measures for protection. However, this finding at least reveals respondents’ awareness of mode of transmission and the importance of following the instructions for protection.
Attitudes
Aerosol is now considered the major route of MERS transmission.[40] Respondents identified that close contact with a patient of MERS-CoV is one of the main routes of spreading the virus (64%). Also, a high proportion (79%) of respondents was aware about the instructions of protection. So, this indicates that the information related to the way of contamination and spreading of MERS-CoV and the measures for protection is well known.
Perception about infection control
The main infection prevention and control measures for managing acute viral respiratory tract infection are simple and well documented.[8,29,41]
First droplet precaution is wearing a surgical mask within 1 m of the patient; contact precaution is also important by wearing gown and gloves on entering the room and removing them on leaving. Eye protection should be added when caring for probable or confirmed cases of MERS-CoV infection.
However, the majority of respondents (79%) were aware of the measures adopted for protection and 75% knew that MERS-CoV is contagious, and therefore, it is very important to apply the methods of protection.
From the results of this survey, it is very encouraging to conclude that our dental students had good knowledge of MERS-CoV (etiology, symptoms, protection) and this may reflect the successful distribution of the information about MERS-CoV by college 27% and MOH 25%. More awareness of MERS-CoV hazards is required by medical staff who are the first people in contact with patients infected by the virus.
Our data indicate the necessity for further continuing education among medical staff, as well as improving public education about infection control.
The MERS-CoV outbreak in Jeddah and the increasing number of healthcare workers affected remind us of the need to acquire the basics information of infection control which is the main principle for protection from MERS-CoV.
Summary and recommendations
A novel coronavirus, MERS-CoV, causing severe respiratory illness emerged in 2012 in Saudi Arabia. MERS-CoV is closely related to coronaviruses found in bats, suggesting that bats might be a reservoir of MERS-CoV. Camels likely serve as hosts for MERS-CoV. The presence of case clusters strongly suggests that human-to-human transmission occurs
There is currently no treatment recommended for coronavirus infections, except for supportive care as needed
An increased level of infection control precautions is recommended when caring for patients with MERS-CoV infection
Dental students had good knowledge about MERS-CoV. However, more information still must be provided by MOH and college for medical staff
We emphasized on the necessity of providing more information about prevention of any susceptible viral infection to the healthcare workers.
Appendix 1: Questionnaire for MERS-CoV
Assessment of the awareness level of dental students towards Middle East Respiratory Syndrome – coronavirus
Put a circle in the correct answer
-
1)
Describe yourself : Male-Female
-
2)
What is MERS-CoV ?
-
a)Middle East Respiratory Syndrome
-
b)Viral respiratory illness
-
c)Syndrome Coronavirus
-
d)All answers are correct
-
e)No idea
-
a)
-
3)
From where did you hear about MERS-CoV before?
-
a)College
-
b)Media
-
c)MOH
-
d)Social community
-
e)No idea before
-
a)
-
4)
Is MERS contagious ?
-
a)Yes
-
b)Non
-
a)
-
5)
What are Symptoms of MERS ?
-
a)Severe acute respiratory illness
-
b)Fever,cough
-
c)Gastrointestinal symptoms
-
d)All answers are correct
-
e)No idea
-
a)
-
6)
Did know periode of incubation for MERS ?
-
a)2-14 days
-
b)3 weeks
-
c)1 month
-
d)3 month
-
a)
-
7)
What is the source of MERS virus ?
-
a)Bats
-
b)Camels
-
c)Domestic animal
-
d)No ideaage: under 25 y - over 25 y
-
a)
-
8)
How does the virus MERS spread ?
-
a)From ill person to other through close contact
-
b)Fast food
-
c)Contact with domestic animal
-
d)No idea
-
a)
-
9)
Did you know the way of prevention from MERS?
-
a)Washing hands with alcohol-based hand sanitizer
-
b)Cover nose, mouth with tissue when coughing or sneezing
-
c)Avoid personal contact (kissing, sharing cup,---etc)
-
d)All answers are correct
-
a)
-
10)
Is MERS-CoV same as SARS virus ?
-
a)Yes
-
b)Non
-
a)
-
11)
Did you know approximate percentage of death with person infected with MERS ?
-
a)50%
-
b)30%
-
c)5%
-
d)No idea
-
a)
-
12)
Treatment for MERS-CoV is ?
-
a)Supportive treatment
-
b)Vaccination
-
c)No any treatment
-
d)No idea
-
a)
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367:1814–20. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 2.de Groot RJ, Baker SC, Baric RS, Brown CS, Drosten C, Enjuanes L, et al. Middle East respiratory syndrome coronavirus (MERS-CoV): Announcement of the Coronavirus Study Group. J Virol. 2013;87:7790–2. doi: 10.1128/JVI.01244-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan JF, Chan KH, Choi GK, To KK, Tse H, Cai JP, et al. Differential cell line susceptibility to the emerging novel human betacoronavirus 2c EMC/2012: Implications for disease pathogenesis and clinical manifestation. J Infect Dis. 2013;207:1743–52. doi: 10.1093/infdis/jit123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Müller MA, Raj VS, Muth D, Meyer B, Kallies S, Smits SL, et al. Human coronavirus EMC does not require the SARS-coronavirus receptor and maintains broad replicative capability in mammalian cell lines. MBio. 2012;3 doi: 10.1128/mBio.00515-12. pii: e00515-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meyer B, García-Bocanegra I, Wernery U, Wernery R, Sieberg A, Müller MA, et al. Serologic assessment of possibility for MERS-CoV infection in equids. Emerg Infect Dis. 2015;21:181–2. doi: 10.3201/eid2101.141342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Middle East Respiratory Syndrome Coronavirus (MERS-CoV): Summary of Current Situation, Literature Update and Risk Assessment-as of 5th February 2015. [Last accessed on 2015 Mar 04]. Available from: http://www.who.int/csr/disease/coronavirus_infections/mers-5-february-2015.pdf?ua=1 .
- 7.World Health Organization. Global Alert and Response. Middle East respiratory Syndrome Coronavirus (MERS-CoV)-Saudi Arabia. [Last accessed on 2015 Apr 17]. Available from: http://www.who.int/csr/don/16-april -2015-mers-saudi-arabia/en/
- 8.WHO. Global Alert and Response. Middle East Respiratory Syndrome Coroonavirus (MERS-CoV)-15th May 2014. [Last accessed on 2014 May 19]. Available from: http://www.who.int/csr/don/2014_05_15_mers/en/
- 9.Annan A, Baldwin HJ, Corman VM, Klose SM, Owusu M, Nkrumah EE, et al. Human betacoronavirus 2c EMC/2012-related viruses in bats, Ghana and Europe. Emerg Infect Dis. 2013;19:456–9. doi: 10.3201/eid1903.121503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ithete NL, Stoffberg S, Corman VM, Cottontail VM, Richards LR, Schoeman MC, et al. Close relative of human Middle East respiratory syndrome coronavirus in bat, South Africa. Emerg Infect Dis. 2013;19:1697–9. doi: 10.3201/eid1910.130946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Memish ZA, Mishra N, Olival KJ, Fagbo SF, Kapoor V, Epstein JH, et al. Middle East respiratory syndrome coronavirus in bats, Saudi Arabia. Emerg Infect Dis. 2013;19:1819–23. doi: 10.3201/eid1911.131172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Lancet Infectious Diseases. Need for global cooperation in control of MERS-CoV. Lancet Infect Dis. 2013;13:639. doi: 10.1016/S1473-3099(13)70205-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Azhar EI, El-Kafrawy SA, Farraj SA, Hassan AM, Al-Saeed MS, Hashem AM, et al. Evidence for camel-to-human transmission of MERS coronavirus. N Engl J Med. 2014;370:2499–505. doi: 10.1056/NEJMoa1401505. [DOI] [PubMed] [Google Scholar]
- 14.WHO. MERS-CoV Enigma Deepens as Reported Cases Surge. [Last accessed on 2014 May 24];383 doi: 10.1016/S0140-6736(14)60866-7. Available from: http://www.thelancet.com . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO. Infection Control and MERS-CoV in Health-Care Workers. [Last accessed on 2014 May 31];383 doi: 10.1016/S0140-6736(14)60852-7. Available from: http://www.thelancet.com . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Middle East respiratory Syndrome Coronavirus (MERS-CoV) Summary and Literature Update - As of 20th Jan 2014. [Last accessed on 2014 Jan 29]. Available from: http://www.who.int/csr/disease/coronavirus_infections/MERS_CoV_Update_20_Jan_2014.pdf .
- 17.Oboho IK, Tomczyk SM, Al-Asmari AM, Banjar AA, Al-Mugti H, Aloraini MS, et al. 2014 MERS-CoV outbreak in Jeddah-a link to health care facilities. N Engl J Med. 2015;372:846–54. doi: 10.1056/NEJMoa1408636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. WHO Statement on the 8th Meeting of the IHR Emergency Committee Regarding MERS-CoV. [Last accessed on 2015 Mar 10]. Available from: http://www.who.int/mediacentre/news/statements/2015/8th-mers-emergency-committee/en/
- 19.World Health Organization. Revised Case Definition for Reporting to WHO-Middle East Respiratory Syndrome Coronavirus-Interim Case Definition as of 14th July 2014. [Last accessed on 2015 Mar 06]. Available from: http://www.who.int/csr/disease/coronavirus_infections/case_definition/en/
- 20.Assiri A, McGeer A, Perl TM, Price CS, Al Rabeeah AA, Cummings DA, et al. KSA MERS-CoV Investigation Team. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013;369:407–16. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drosten C, Seilmaier M, Corman VM, Hartmann W, Scheible G, Sack S, et al. Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect Dis. 2013;13:745–51. doi: 10.1016/S1473-3099(13)70154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Memish ZA, Zumla AI, Al-Hakeem RF, Al-Rabeeah AA, Stephens GM. Family cluster of Middle East respiratory syndrome coronavirus infections. N Engl J Med. 2013;368:2487–94. doi: 10.1056/NEJMoa1303729. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. Global Alert and Response. Novel Coronavirus Summary and Literature Update-As of 17th May 2013. [Last accessed on 2013 May 17]. Available from: http://www.who.int/csr/disease/coronavirus_infections/update_20130517/en/index.html# .
- 24.Guery B, Poissy J, el Mansouf L, Séjourné C, Ettahar N, Lemaire X, et al. Clinical features and viral diagnosis of two cases of infection with Middle East Respiratory Syndrome coronavirus: A report of nosocomial transmission. Lancet. 2013;381:2265–72. doi: 10.1016/S0140-6736(13)60982-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, Al-Rabiah FA, Al-Hajjar S, Al-Barrak A, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: A descriptive study. Lancet Infect Dis. 2013;13:752–61. doi: 10.1016/S1473-3099(13)70204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC). Updated information on the epidemiology of Middle East respiratory syndrome coronavirus (MERS-CoV) infection and guidance for the public, clinicians, and public health authorities, 2012-2013. MMWR Morb Mortal Wkly Rep. 2013;62:793–6. [PMC free article] [PubMed] [Google Scholar]
- 27.Breban R, Riou J, Fontanet A. Interhuman transmissibility of Middle East Respiratory Syndrome coronavirus: Estimation of pandemic risk. Lancet. 2013;382:694–9. doi: 10.1016/S0140-6736(13)61492-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systemic review. PloS One. 2012;7:e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hui DS, Memish ZA, Zumla A. Severe acute respiratory syndrome vs. the Middle East Respiratory Syndrome. Curr Opin Pulm Med. 2014;20:233–41. doi: 10.1097/MCP.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 30.Seto WH, Conly JM, Pessoa-Silva CL, Malik M, Eremin S. Infection prevention and control measures for acute respiratory infection in healthcare setting: An update. East Mediterr Health J. 2013;19(Suppl 1):539–47. [PubMed] [Google Scholar]
- 31.World Health Organization. Interim Guidance Document. Clinical Management of Severe Acute Respiratory Infections when Novel Coronavirus is Suspected: What to do and What Not to do. [Last accessed on 2013 Apr 09]. Available from: http://www.who.int/csr/disease/coronavirus_infections/InterimGuidance-ClinicalManagement_NovelCoronavirus_11Feb13.pdf .
- 32.Falzarano D, de Wit E, Martellaro C, Callison J, Munster VJ, Feldmann H. Inhibition of novel β coronavirus replication by a combination of interferon-α2b and ribavirin. Sci Rep. 2013;3:1686. doi: 10.1038/srep01686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Falzarano D, de Wit E, Rasmussen AL, Feldmann F, Okumura A, Scott DP, et al. Treatment with interferon-α2b and ribavirin improves outcome in MERS-CoV-infected rhesus macaques. Nat Med. 2013;19:1313–7. doi: 10.1038/nm.3362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Omrani AS, Saad MM, Baig K, Bahloul A, Abdul-Matin M, Alaidaroos AY, et al. Ribavirin and interferon alfa-2a for severe Middle East respiratory syndrome coronavirus infection: A retrospective cohort study. Lancet Infect Dis. 2014;14:1090–5. doi: 10.1016/S1473-3099(14)70920-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Summary and Literature Update-As of 9th May 2014. [Last accessed on 2014 May 12]. Available from: http://www.who.int/csr/disease/coronavirus_infections/MERS_CoV_Update_09_May_2014.pdf?ua=1 .
- 36.Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Hospitalized Patients with Middle East Respiratory Syndrome Coronavirus (MERS-CoV) [Last accessed on 2015 Apr 06]. Available from: http://www.cdc.gov/coronavirus/mers/downloads/mers-infection-control-guidance-051414.pdf .
- 37.Harriman K, Brosseau L, Trivedi K. Hospital-associated Middle East respiratory syndrome coronavirus infections. N Engl J Med. 2013;369:1761. doi: 10.1056/NEJMc1311004. [DOI] [PubMed] [Google Scholar]
- 38.Bialek SR, Allen D, Alvarado-Ramy F, Arthur R, Balajee A, Bell D, et al. Centers for Disease Control and Prevention (CDC). First confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection in the United States, updated information on the epidemiology of MERS-CoV infection, and guidance for the public, clinicians, and public health authorities-May 2014. MMWR Morb Mortal Wkly Rep. 2014;63:431–6. [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization. Middle East Respiratory Syndrome Coronavirus (MERS-CoV)-13th June 2014. Update on MERS-CoV Transmission from Animals to Humans, and Interim Recommendations for at-risk Groups. [Last accessed on 2014 Jun 17]. Available from: http://www.who.int/csr/disease/coronavirus_infections/MERS_CoV_RA_20140613.pdf?ua=1 .
- 40.Seto WH, Tsang D, Yung RW, Ching TY, Ng TK, Ho M, et al. Effectiveness of precaution against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1519–20. doi: 10.1016/S0140-6736(03)13168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.CDC. Interim Infection Prevention and Control Recommendation for Hospitalized Patient with Middle East Respiratory Syndrome Coronavirus. [Last accessed on 2014 May 15]. Available from: http://cdc.gov/coronavirus/mers/infection-prevention-control .


