Abstract
Aim:
The purpose of this study was the early detection of premalignant and malignant oral soft lesions by fluorescent light (VELscope).
Materials and Methods:
A total of 748 patients were evaluated through clinical and fluorescent light analysis of the entire oral cavity. Any lesion that was detected underwent a surgical excision biopsy as the golden standard for the detection of the lesion's histology; then a comparison was made between the results to assure the efficacy of the fluorescent light analysis outcome.
Results:
About 9.4% of the lesions detected were abnormal lesions and 83.09% had loss of fluorescent light effect. Based on the use of surgical biopsy, the machine had a sensitivity of 74.1% and a specificity of 96.3%. According to the statistical analysis, the P value was much lower than 0.05, so we can conclude that at 95% confidence level, there was significant agreement between VELscope results and biopsy results. Kappa coefficient value was approximately 0.5, which means that the strength of the agreement was medium.
Conclusion:
VELscope can be used as a clinical diagnostic aid in the detection of premalignant and malignant lesions of the oral cavity. In addition, it helps in the detection of the borders in both surgical biopsy and surgical excision.
Keywords: Biopsy, fluorescent light, malignancy, premalignancy, sensitivity, specificity, VELscope
INTRODUCTION
Oral cancer is considered as an international health disease that affects an individual's health, psychology, lifestyle, and loads the whole family with its effect.[1] On the other hand, these kinds of diseases load the governments as well with economical overheads including the need for developmental programs and advanced research groups and centers. The total number of cases of oral cancer is around 263,900 and the mortality rate is 40%. The recurrence rate ranges from 40 to 50% after 5 years of treatment. But when the disease is detected early, the percentage of recurrence is reduced to 10–20%.[1] Unfortunately, only 35% of the malignant lesions are detected in the early stages due to the fact that these lesions start at the basal cell layer and cannot be seen by the naked eye.[2]
Potentially malignant oral lesions are those lesions that exhibit a change in shape or color on clinical or histological appearance. These kinds of changes are due to the different types of biopsies, which, in most cases, are surgical in nature and may cause trauma for the patient. So, it is important to have another technique to detect such lesions, especially in their early stages, such as using fluorescent light.
Risk factors associated with oral cancer:
Smoking: The risk of oral cancer is about 5–10 times greater among smokers compared to people who never smoked.[4] This risk further multiplies among smokers who also drink alcohol.[4,5] On the other hand, several studies relate this habit with the consumption of alcohol, as well as the number of cigarettes smoked and the period of smoking
Alcohol consumption: Many studies showed that more than 75–80% of the oral cancer patients drink alcohol continuously.[3,6] It is thought that the effect of alcohol on the liver, especially liver cirrhosis, might be one of the main reasons for oral cancer
Human papillomavirus (HPV): This virus plays an important role in the epithelial cancer of the tonsils and oropharynx, wherein more than 10% of these cancers have HPV DNA integrated in their genome[7,8]
Syphilis: The percentage of cancerous ability of the leukoplakia originating from syphilis is 30–100%. But the disease is rare even in the Third World[9]
Age: More than 98% of oral cancers occur at more than 40 years of age[10]
Malnutrition: There is epidemic evidence to the relation of deficiency of vitamin A and oral epithelial cancer[11]
Intraoral infections[9]
Direct sunlight: Direct exposure to ultraviolet light for long periods of time is considered as an important risk factor for oral cancers, and it incidence is higher in Whites than others[12]
Precancerous lesions: The transformation of white lesions in the oral cavity into malignant ones is low; but, on the other hand, it is high when they are red lesions and traumatic ulcers which is one of the categories.[12,13,14]
Early detection of the oral lesions
Clinical objective analysis remains the most important method for the early detection of oral cancers so far.[15,16,17,18]
It was noticed that only 13% of the American population performed routine check-up in 2010 and it is hoped that this number will increase to 20% in 2020.[19,20]
Nevertheless, the use of other instruments and machines is highly important in conjunction with visual examination, such as the brush biopsy, OralCDx, toluidine coloration, ViziLite machine, and VELscope.
MATERIALS AND METHODS
The study sample consisted of 748 randomized patients. These patients were attending the College of Dentistry, Al-Moasat Hospital, Al-Mojtahed Hospital, and Al-Karama Nursing home, all in Damascus.
The basic forms were used to record the personal information, social information, and medical history and habits of the patients. Medical history collected two important feedbacks: 1. The influence on the way the dental treatment will be provided and 2. the intraoral lesion might be a part of a systemic disease.
Many questions were asked about the patient: 1. The duration of the lesion since its occurrence; 2. the change in the size of the lesion; 3. Did the characteristics of the lesion change? 4. What are the signs and symptoms associated with the lesion, such as pain, sensation alteration, anesthesia, paresthesia, swellings, bad taste or odor, and enlargement or pain of nearby lymph nodes? 5. Any general symptoms associated with the lesion, such as fever, vomiting, nausea, etc., 6. Was there any related disorder with the lesion like continuous trauma to the site or dental diseases at the site?
Then, a through clinical objective examination was carried out.
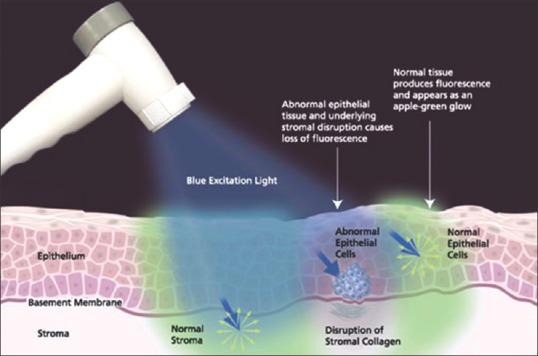
This was followed by examination with the VELscope. It is one of the machines used for the detection of oral cancers that uses blue light with a special wavelength of 400–460 nm as the source that penetrates the epithelial layer and the basal layer reaching the stroma (Led Dental, Burnaby, Canada, 2007). This ability is called autofluorescence in which invisible fluorescent light filtered from the blue light gives fluorescent color to the normal tissues and different dark green colors reaching black color to the abnormal tissues [Figure 1].[21]
Figure 1.
The VELscope machine and intraoral camera (Led Dental, Canada, 2007)
The machine is portable, easily stored as it does not need much space in the clinic, painless for the patient, and it needs <2 min for its application saving time for the patient and the practitioner. The machine has been supplied with many accessories to make it safe from the cross-infection prospective, such as plastic protectors for its lens and a plastic sleeve for the body of the machine.[21]
In case of finding any incidence of malignancy, one of the shapes of biopsies has to be performed, and histological scanning will assure the intraoral findings.
In this study, two different types of biopsies were selected:
Incisional biopsy in which part of the lesion is obtained when the lesion is either large in size (>1 cm) or is located at a critical place or has high susceptibility for malignancy
Excisional biopsy carried out in small lesions (<1 cm) and has normal readings.
The biopsies were sent to the histopathology department in Damascus University College of Dentistry. After obtaining the histopathological results, comparison was made between the clinical and histopathological findings.
Statistical analysis
Potentially malignant lesions observed in each patient were examined twice: The first examination consisted of a biopsy while the second one was with VELscope instrument. The malignancy of each detected lesion was determined; 26 cases were high-risk lesions. Sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were calculated using the following formulas:
Sensitivity = [true positives/(true positive + false negative)] ×100
Specificity = [true negatives/(true negative + false positives)] ×100
Accuracy = sensitivity + specificity
Predictive value for a positive result (PV+) = [true positive/(true positive + false positive)] ×100
Predictive value for a negative result (PV−) = [true negatives/(true negatives + false negatives)] ×100.
RESULTS
Patient distribution
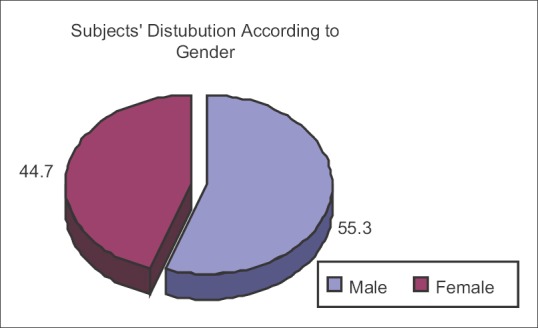
The sample distribution was statistically analyzed. The sample consisted of 414 males and 334 females with a mean age of 37 years [Figure 2].
Figure 2.

The study sample according to gender
Clinically differential lesions according to gender and type of lesion variable
The results presented in Figure 3 show the occurrence and gender wise distribution of potential malignant lesions. Clinically undifferentiated lesions were higher in females (92.2%) compared to males (89.1%), while clinically differentiated lesions were higher in males than females (10.9%).
Figure 3.
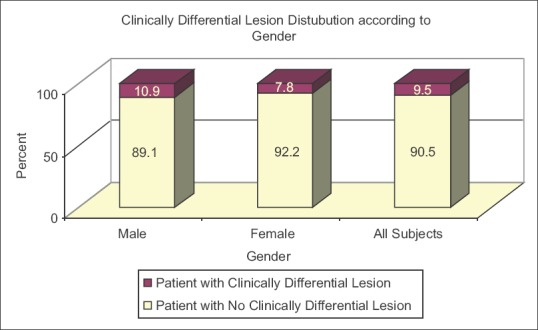
Data distribution according to gender
There were no statistically significant differences between male and female patients with potentially malignant lesions, as shown in Figure 3 and Table 1.
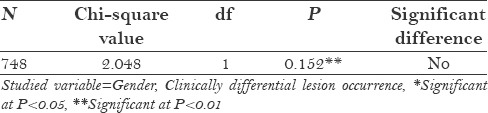
Table 1.
Potential malignant lesions’ occurrence and gender wise distribution*
Subjects’ distribution according to the types of lesions is shown in Figure 4. Traumatic ulcer had the highest incidence (26.8%) and ossifying fibroma or pemphigus vulgaris (1.4%) was the least common.
Figure 4.
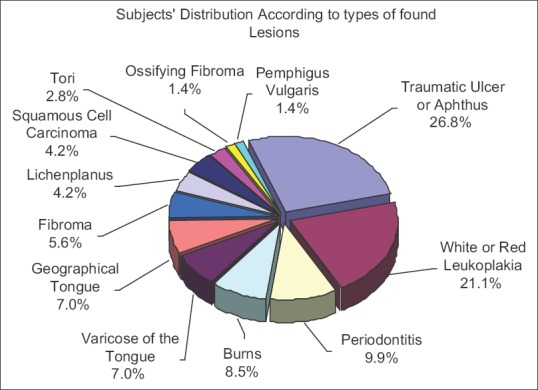
Distribution according to the types of lesions
Tables 2–4 show that the percentage of benign lesions was 61.5% according to their histological analysis, while the efficiency of VELscope in detecting lesions was higher (81.7%).
Table 2.
Lesions’ malignancy according to their histological analysis
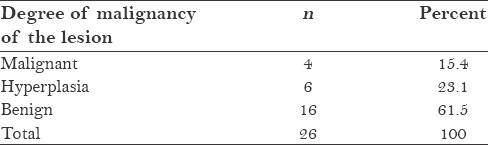
Table 4.
Chi-square test of benign and malignant in biopsy group*
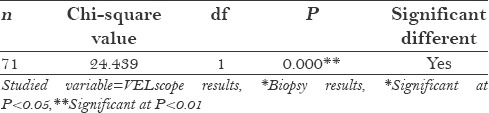
Table 3.
VELscope's efficiency in detecting lesions’ malignity
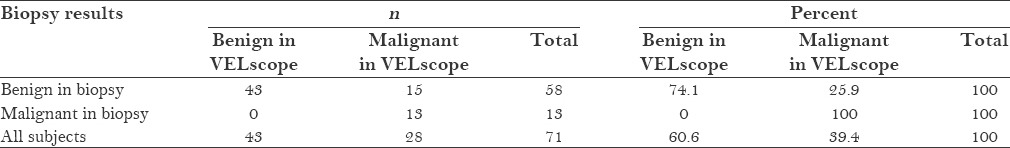
Table 4 shows that P value was much lower than 0.05, so we can conclude that at 95% confidence level, there were significant differences in VELscope results between benign in biopsy group and malignant in biopsy group subjects; percentage of benign subjects in benign in the biopsy group was greater than the percentage of benign subjects in malignant in the biopsy group. Also, the percentage of malignant subjects in benign in the biopsy group was lower than the percent of malignant subjects in malignant in the biopsy group. So, VELscope was statistically effective in detecting lesions’ malignity [Table 5].
Table 5.
Agreement between VELscope results and biopsy results
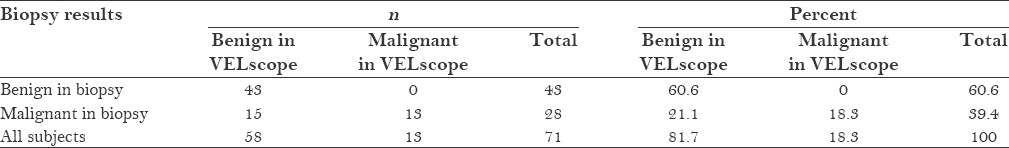
To know if there were significant differences in VELscope results between benign in biopsy group and malignant in biopsy group subjects, a Chi-square test was applied as shown in Table 4.
Agreement between VELscope results and biopsy results
Kappa coefficient value was calculated between VELscope results and biopsy results, as shown in Table 6.
Table 6.
VELscope results in statistical calculations

Table 6 shows that P value was much lower than 0.05, so we can conclude at 95% confidence level, there was significant agreement between VELscope results and biopsy results. Kappa coefficient value was approximately 0.5, which means that the strength of the agreement was medium.
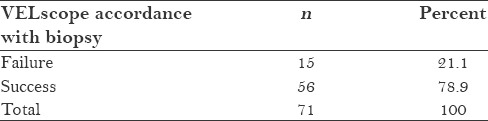
Table 7 shows the true-/false-positive and -negative status. Table 8 shows the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value, while Table 9 shows that accordance between VELscope and biopsy failure was 21.1% and between VELscope and biopsy success was about 78.9%.
Table 7.
True-/false-positive and -negative status of the results

Table 8.
Sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of the calculated results
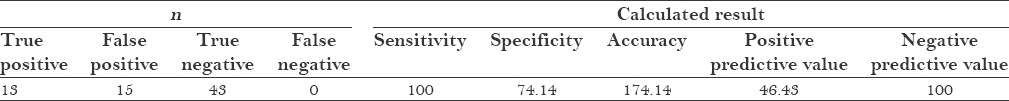
Table 9.
Accordance between VELscope results and biopsy results
After applying fluorescent light to the patients’ tissues, the response of the tissues reveals the nature of the tissues as shown in Figure 5; in case of tissues with malignant or premalignant lesions, the color changes into dark colors as shown in Figure 6.[22]
Figure 5.
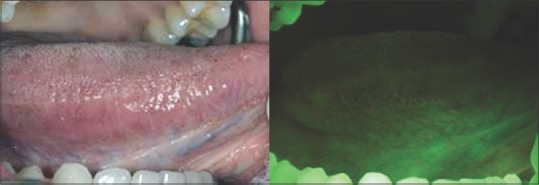
Normal fluorescent color of the tongue using VELscope, as seen in our study
Figure 6.
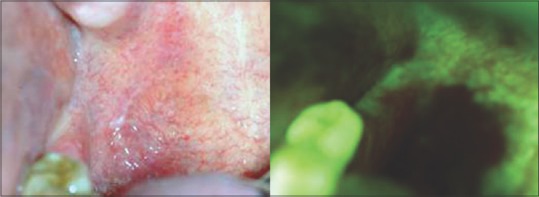
Fluorescent discontinuity and dark color showing abnormal tissues. By biopsy it has been detected as Saethre–Chotzen syndrome
DISCUSSION
The survival rate for the patients suffering from oral cancer depends on three main factors:
Early detection of the lesion
A good differential diagnosis of the lesion
The way of treatment.
Elimination of the risk factors should be taken into consideration, such as smoking and alcohol drinking. Clinical intraoral examination and proper radiographic study are important for the detection of the lesion, but unfortunately, they are not enough for detecting malignant and premalignant lesions.
Final diagnosis should be based on surgical biopsy. The VELscope machine is an efficient diagnostic instrument for the differentiation of premalignant and malignant lesions.[23]
Several techniques have been introduced to aid in the early detection of malignant or premalignant lesions, such as OralCDx, Toluidine coloring, ViziLite machine, Identafi machine, and VELscope.[24] This explains the big number of articles explaining the importance of these techniques as non-traumatic procedures in comparison with surgical biopsy. Therefore, we had this study done to evaluate the role of VELscope in such detection.
This machine works based on fluorescence activity [Figure 2] as it uses blue light with a wavelength of 400–460 nm inside the oral cavity, penetrating the epithelial tissues and reaching the stroma through the basal layer. This will allow the practitioner to observe the suspicious lesions in different colors [Figure 7]. As and when the light comes across abnormal tissue, it will discontinue its’ fluorescence activity that was seen on the normal tissues by changing from the green fluorescent light to a dark green color.[25]
Figure 7.
The mode of action of fluorescent light
The machine's efficiency to act as a diagnostic instrument for the differentiation of malignant and the premalignant lesions, depends on the final decision made on the basis of the golden standard “surgical biopsy.”
The results of our study are in accordance with the results of Laneh et al. who found in 2006 that in the differentiation between normal and defective mucosa, the sensitivity value was 98% and the specificity value was 92%.[26]
Poh et al. in 2006 stated they had used the machine inside the surgical chamber while performing an enucleation. Also, they obtained a good match between the machine and the histopathological result.[21]
We obtained results similar to that of Trolneck and Erikson (2009) whom did a comparative study between different ways of early detection of intraoral lesions using ViziLite and biopsy from OralCDx and VELscope; they obtained a sensitivity of 98–100% and a specificity of 94–100%.[27,28]
In 2011, Matsomoto et al. studied 74 cases with 37 of them being malignant and the rest were benign. They noticed that the machine was a good aid in the detection of changes in tissues.
The results of this study are concordant with that of Dayyani et al.,[7] as they obtained an SE of 92% and an SP of 77%. The study emphasized that the machine has a good sensitivity as the clinical examination, and it can be used as an additional device for diagnosis in patients with risk factors. The reason for the lesser value of sensitivity was that the study included all the intraoral lesions in the high-risk patients and not only the lesions that were diagnosed histopathologically as malignant or hyperplastic in nature.[29] But we agree with them that we can use the machine as an aiding device with the clinical examination.
Our study results agreed with the study of Lee and Wong[30] who reported in their study that the sensitivity and specificity of the machine is high and almost absolute when it comes to the diagnosis of malignant lesions; they performed their study on lesions that were prediagnosed as Saethre–Chotzen syndrome.
Our results are similar to the results of Farah et al.[31] who studied 44 cases histologically and by the machine clinically, and obtained a sensitivity of 100% and a specificity of 96%.
But our results are not in agreement with that of Camily and Ledegy as their study showed that the machine is not effective in the detection of hyperplasia as the sensitivity was 30% and the specificity was 63%.[32] The difference in results could be because the machine was depended as a single definitive diagnostic tool in their study without clinical examination.
Also, we do not agree with Ardoor et al.[32] as their study did not support using the machine in suspected lesion, as the sensitivity was 87.1% and the specificity was 20%. This drop might be due to not combining the clinical examination with the use of the machine. They noticed loss of fluorescent effect on benign lesions like varicose of the tongue and pigmentation.
So, based on the results it can be concluded that we can depend on the machine as a reassuring device for the clinical examination, especially in the examination of the high-risk population, and the big advantage is that it is a non-traumatic technique used by dentists for the detection of premalignant and malignant lesions in early stages.
CONCLUSION
The use of VELscope is effective in the detection of malignant and premalignant lesions
VELscope aids in the detection of the site of biopsy
VELscope is used an aiding tool inside the surgical theater for the detection of the borders on enucleation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.American Cancer Society. Oral Cancer. [Last accessed on 2011 Jul 02]. Available from: http://www.cancer.org/acs/groups/content/@nho/documnets/document/oralcancerpdf.pdf .
- 2.American Cancer Society. Oral Cavity and Oropharyngeal Cancers Detailed Guide. [Last accessed on 2015 Feb 16]. Last Medical Review: 2/26/2013. Available from: http://www.cancer.org .
- 3.Oral Cancer Foundation. Rates of Occurrence in the United States. [Last accessed on 2006 Jan 23]. Available from: http://www.oralcancerfoundation.org/facts/index.htm .
- 4.Kois JC, Truelove E. Detecting oral cancer: A new technique and case reports. Dent Today. 2006;25:94. 967. [PubMed] [Google Scholar]
- 5.International Agency for Research on Cancer, World Health Organization. Vol. 44. Lyon, France: International Agency for Research on Cancer; 1988. IARC Monographs on the Evaluation of Carcinogens Risks to Humans: Alcohol Drinking. Summary of Data Reported and Evaluation; p. 18. [Google Scholar]
- 6.Atlanta, Georgia: American Cancer Society Center; 2005. American Cancer Society. Alcohol and Cancer. No. 3002.12. 2015. [Google Scholar]
- 7.Dayyani F, Etzel CJ, Liu M, Ho CH, Lippman SM, Tsao AS. Metaanalysis of the impact of human papillomavirus (HPV) on cancer risk and overall survival in head and neck squamous cell carcinomas (HNSCC) Head Neck Oncol. 2010;2:15. doi: 10.1186/1758-3284-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chaturvedi AK. Epidemiology and clinical aspects of HPV in head and neck cancers. Head Neck Pathol. 2012;6(Suppl 1):S1624. doi: 10.1007/s12105-012-0377-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leão JC, Gueiros LA, Porter SR. Oral manifestations of syphilis. Clinics (Sao Paulo) 2006;61:1616. doi: 10.1590/s1807-59322006000200012. [DOI] [PubMed] [Google Scholar]
- 10.Lissowska J, Pilarska A, Pilarski P, SamolczykWanyura D, Piekarczyk J, BardinMikollajczak A, et al. Smoking, alcohol, diet, dentition and sexual practices in the epidemiology of oral cancer in Poland. Eur J Cancer Prev. 2003;12:2533. doi: 10.1097/00008469-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Saraf S. New Delhi: Jaypee; 2006. Text Book of Oral Pathology; p. 52. [Google Scholar]
- 12.Neville BW, Day TA. Oral cancer and precancerous lesions. CA Cancer J Clin. 2002;52:195215. doi: 10.3322/canjclin.52.4.195. [DOI] [PubMed] [Google Scholar]
- 13.Padmanabhan MY, Pandey RK, Aparna R, Radhakrishnan V. Neonatal sublingual traumatic ulceration Case report and review of the literature. Dent Traumatol. 2010;26:4905. doi: 10.1111/j.1600-9657.2010.00926.x. [DOI] [PubMed] [Google Scholar]
- 14.Lane PM, Gilhuly T, Whitehead P, Zeng H, Poh CF, Ng S, et al. Simple device for the direct visualization of oralcavity tissue fluorescence. J Biomed Opt. 2006;11:024006. doi: 10.1117/1.2193157. [DOI] [PubMed] [Google Scholar]
- 15.Satgé D, Clémenson P, Nishi M, Clémenson A, Hennequin M, Pacaut C, et al. A mucoepidermoid carcinoma in a young man with intellectual disability: Review of oral cancer in people with intellectual disability. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:e227. doi: 10.1016/j.oooo.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Bouquot JE. Common oral lesions found during a mass screening examination. J Am Dent Assoc. 1986;112:507. doi: 10.14219/jada.archive.1986.0007. [DOI] [PubMed] [Google Scholar]
- 17.Baroni A, Capristo C, Rossiello L, Faccenda F, Satriano RA. Lingual traumatic ulceration (RigaFede disease) Int J Dermatol. 2006;45:10967. doi: 10.1111/j.1365-4632.2004.02554.x. [DOI] [PubMed] [Google Scholar]
- 18.Ceyhan AM, Yildirim M, Basak PY, Akkaya VB, Ayata A. Traumatic lingual ulcer in a child: RigaFede disease. Clin Exp Dermatol. 2009;34:1868. doi: 10.1111/j.1365-2230.2008.02796.x. [DOI] [PubMed] [Google Scholar]
- 19.Ozcelik O, Haytac MC, Akkaya M. Iatrogenic trauma to oral tissues. J Periodontol. 2005;76:17937. doi: 10.1902/jop.2005.76.10.1793. [DOI] [PubMed] [Google Scholar]
- 20.Rawal SY, Claman LJ, Kalmar JR, Tatakis DN. Traumatic lesions of the gingiva: A case series. J Periodontol. 2004;75:7629. doi: 10.1902/jop.2004.75.5.762. [DOI] [PubMed] [Google Scholar]
- 21.Matsumoto K. Detection of potentially malignant and malignant lesions of oral cavity using autofluorescence visualization device. Kokubyo Gakkai Zasshi. 2011;78:7380. [PubMed] [Google Scholar]
- 22.Poh CF, Zhang L, Anderson DW, Durham JS, Williams PM, Priddy RW, et al. Fluorescence visualization detection of field alterations in tumor margins of oral cancer patients. Clin Cancer Res. 2006;12:671622. doi: 10.1158/1078-0432.CCR-06-1317. [DOI] [PubMed] [Google Scholar]
- 23.Meena A, Satoskar SK. Early detection of oral precancerous lesions: Recent advances. Int J Med Public Health. 2012;2:14. [Google Scholar]
- 24.Lingen MW, Kalmar JR, Karrison T, Speight PM. Critical evaluation of diagnostic aids for the detection of oral cancer. Oral Oncol. 2008;44:1022. doi: 10.1016/j.oraloncology.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fitzpatrick SG, Hirsch SA, Gordon SC. The malignant transformation of oral lichen planus and oral lichenoid lesions: A systematic review. J Am Dent Assoc. 2014;145:4556. doi: 10.14219/jada.2013.10. [DOI] [PubMed] [Google Scholar]
- 26.TrullenqueEriksson A, MuñozCorcuera M, CampoTrapero J, CanoSánchez J, BasconesMartínez A. Analysis of new diagnostic methods in suspicious lesions of the oral mucosa. Med Oral Patol Oral Cir Bucal. 2009;14:E2106. [PubMed] [Google Scholar]
- 27.Williams PM, Poh CF, Hovan AJ, Ng S, Rosin MP. Evaluation of a suspicious oral mucosal lesion. J Can Dent Assoc. 2008;74:27580. [PubMed] [Google Scholar]
- 28.Marzouki HZ, Tuong Vi Vu T, Ywakim R, Chauvin P, Hanley J, Kost KM. Use of fluorescent light in detecting malignant and premalignant lesions in the oral cavity: A prospective, singleblind study. J Otolaryngol Head Neck Surg. 2012;41:1648. [PubMed] [Google Scholar]
- 29.Lee YH, Wong DT. Saliva: An emerging biofluid for early detection of diseases. Am J Dent. 2009;22:2418. [PMC free article] [PubMed] [Google Scholar]
- 30.Farah CS, McIntosh L, Georgiou A, McCullough MJ. Efficacy of tissue autofluorescence imaging (VELScope) in the visualization of oral mucosal lesions. Head Neck. 2012;34:85662. doi: 10.1002/hed.21834. [DOI] [PubMed] [Google Scholar]
- 31.Ardore M, Tempia Valenta G, Pentenero M, Gandolfo S. Using the VELscope test in the evaluation of suspicious lesions of the oral mucosa oncologically. Dent Cadmos. 2012;80:53842. 5456. [Google Scholar]
- 32.Pewsner D, Battaglia M, Minder C, Marx A, Bucher HC, Egger M. Ruling a diagnosis in or out with “SpPIn” and “SnNOut”: A note of caution. BMJ. 2004;329:209–13. doi: 10.1136/bmj.329.7459.209. [DOI] [PMC free article] [PubMed] [Google Scholar]


