Abstract
Background: Hypertension is a major, modifiable risk factor for cardiovascular and kidney disease and premature mortality that is improved by the DASH (Dietary Approaches to Stop Hypertension) diet. The DASH diet emphasizes increased consumption of fruit and vegetables, whole grains, low-fat dairy, nuts, and poultry and fish and reduced intakes of fats, red meats (including pork), sodium, and added sugars.
Objective: We sought to evaluate whether the consumption of lean pork compared with the consumption of chicken and fish as the predominant protein source in a DASH-style diet affected blood pressure (BP) control in men and women with elevated BP.
Design: In a randomized crossover study, 13 women and 6 men [mean ± SEM age: 61 ± 2 y; BMI (in kg/m2): 31.2 ± 1.4] with elevated BP [systolic blood pressure (SBP)/diastolic blood pressure (DBP): 130 ± 2/85 ± 2 mm Hg] consumed a DASH-style diet for two 6-wk controlled dietary interventions (with a 4-wk diet washout between interventions) with either lean pork [DASH diet with pork (DASH-P)] or chicken and fish [DASH diet with chicken and fish (DASH-CF), the control diet] as the major protein source (55% of total protein intake). SBP and DBP were measured manually and with a 24-h BP monitoring system on 3 d before and 3 d at the end of each diet intervention.
Results: Preintervention manual BP (DASH-P: 130/84 ± 2/1 mm Hg; DASH-CF: 129/84 ± 2/1 mg Hg) and postintervention manual BP (DASH-P: 122/79 ± 2/1 mm Hg; DASH-CF: 123/78 ± 3/1) were not different between the DASH-P and DASH-CF. Consumption of these DASH-style diets for 6 wk reduced all measures of BP (P < 0.05) with no differences in responses between the DASH-CF and DASH-P.
Conclusion: The results indicate that adults with elevated BP may effectively incorporate lean pork into a DASH-style diet for BP reduction. This trial was registered at clinicaltrials.gov as NCT01696097.
Keywords: blood pressure, DASH diet, pork, red meat, poultry, fish, protein source
INTRODUCTION
Hypertension is the most commonly treated chronic condition in primary care settings and is a major and modifiable risk factor for cardiovascular and kidney diseases (1). According to data from the NHANES 2011–2012, nearly 30% of American adults have hypertension. The condition is especially prevalent in older adults with 65% of those >60 y of age being affected (2). The adoption of the DASH6 (Dietary Approaches to Stop Hypertension) diet, which emphasizes increased consumption of fruit and vegetables, whole-grains, low-fat dairy, nuts, and poultry and fish and reduced intakes of fats, red meats (beef, pork, veal, lamb, and mutton), sodium, and added sugars (3), was previously shown to decrease blood pressure (BP) by ∼7/4 mm Hg (4–6). Therefore, the widespread adoption of a DASH-style diet eating pattern would be expected to have a large public health impact by decreasing risk of cardiovascular disease in at-risk individuals (7).
Red meat consumption is limited to 0.5 servings/d in the DASH diet (4), and this is one potential barrier to such a widespread adoption of this eating pattern. Red meats represent ∼58% of total meat intake in the United States or 85 g per capita per day (8). Pork is the third most commonly consumed meat in the United States behind chicken and beef and accounts for 42% of red meat consumption (9). The recommendation to limit red meat consumption is a strategy for reducing total and saturated fat intakes as well as sodium intake, especially in processed meats (3, 7, 8). The fat and iron content of red meats may also increase inflammation and oxidative stress (8), which are implicated in the development of hypertension (10). However, many cuts of red meat, including beef or pork tenderloin and fresh ham, meet the USDA guidelines for lean (<10 g total fat and <4.5 g saturated fat/100 g) or extra lean (<5 g total fat and <2 g saturated fat/100 g) (11). The use of these cuts of red meat would be consistent with the current recommendation from the American Heart Association to limit saturated fat intake to<7% of daily energy intake (3, 7). Indeed, the inclusion of lean beef into a DASH-style diet produced reductions in BP in adults with BPs in the clinically normal (12) and prehypertensive (13) ranges as well as decreases in total cholesterol and LDL cholesterol (14). However, the effects of including lean cuts of pork in a DASH-style diet require investigation.
Therefore, the primary objective of this randomized crossover study was to assess changes in BP while subjects consumed a DASH-style diet with either lean pork [Dietary Approaches to Stop Hypertension diet with pork (DASH-P)] or chicken and fish [Dietary Approaches to Stop Hypertension diet with chicken and fish (DASH-CF)] as the predominant protein source. We hypothesized that consumption of a DASH-style diet would lower BP and that the predominant protein source (lean pork or chicken and fish) would not influence expected improvements (lowering) in BP. Secondary outcomes included measurements of body composition and other clinical indicators of metabolic and cardiovascular health that comprise metabolic syndrome (15).
METHODS
Subjects
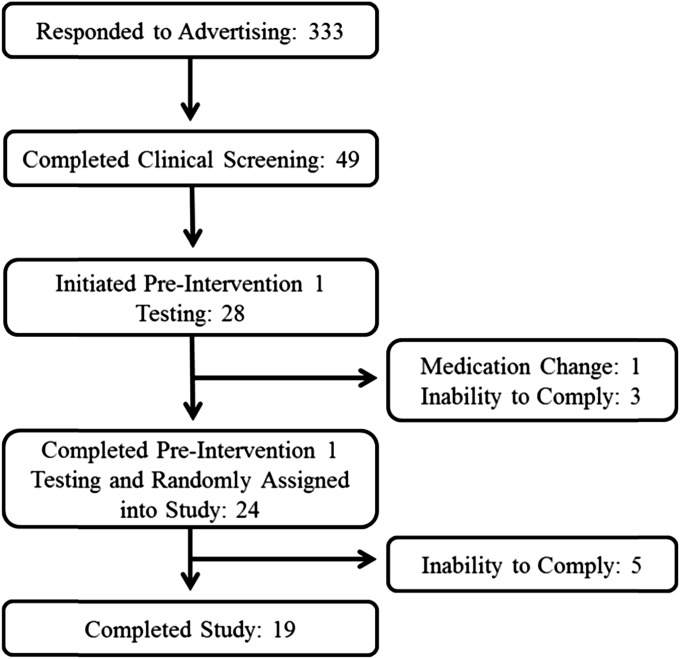
Twenty-eight individuals (19 women and 9 men) were recruited from the greater Lafayette, Indiana, community and signed a study informed consent form for participation in the study (Figure 1). Of these 28 participants, 4 individuals withdrew from the study during baseline testing but before random assignment into the study intervention. Reasons for withdrawal included an inability to comply with testing procedures or time conflicts (n = 3) and a medication change (n = 1). Five of the remaining 24 subjects withdrew from the study after completing baseline testing but before completing any postintervention testing. An inability to comply with the prescribed dietary intervention was the primary reason for study withdrawal for these 5 individuals. Individuals who withdrew from the study were younger (mean ± SEM age: 53 ± 8 y) than those who completed the study (age: 61 ± 2 y), but they did not differ by other baseline characteristics. Nineteen subjects (13 women and 6 men) completed all study procedures, which resulted in a dropout rate of 21% (Figure 1). Study inclusion criteria were as follows: man or woman, aged ≥21–75 y, systolic blood pressure (SBP) ≥120 mm Hg or diastolic blood pressure (DBP) ≥80 mm Hg, no acute illness, not diabetic, not currently (or within the past 3 mo) participating in a vigorous exercise regimen or weight-loss program, willingness to eat study foods, ability to travel to the testing facility, and urinary continence. Individuals who were taking prescription medication for hypertension were included if there were no changes in the medication type or dosage for ≥90 d before and during the study period. All subjects provided written informed consent and received a monetary stipend. The consent form and all study procedures and documents were approved for use by the Purdue University Biomedical Institutional Review Board. This trial was registered at clinicaltrials.gov as NCT01696097.
FIGURE 1.
Study recruitment flow diagram.
Experimental design
Subjects first completed preintervention assessments over a 2-wk period and were randomly assigned to consume a DASH-style diet with a majority of protein from pork (DASH-P) or chicken and fish (DASH-CF) for 6 wk. After a 4-wk washout period, subjects repeated preintervention assessments and consumed the DASH-style diet with the alternate protein source for an additional 6 wk. All assessments performed during the 2 preintervention periods were repeated during the final 2 wk of the DASH-P and DASH-CF interventions. For descriptive purposes, measurements made before the start of the 2 intervention periods are described as preintervention 1 (PI-1) and preintervention 2 (PI-2).
Diet intervention
Subjects were asked to consume their habitual diets during PI-1, the washout period, and PI-2. For two 6-wk intervention periods, subjects consumed controlled DASH-style diets with targeted macronutrient distributions of 55% carbohydrate, 27% fat, and 18% protein as previously described (16, 17). Sodium intake was prescribed at the “Intermediate Sodium Level” as described by Sacks et al. (5) and Svetkey et al. (17), which corresponds to an average of ∼2500 mg Na/d. During each DASH-style diet intervention, 55% of total protein intake was from either lean pork or chicken and fish. The remaining 45% of dietary protein was from dairy, vegetable, and other animal (beef) sources. No chicken or fish was consumed during the DASH-P, and no pork was consumed during the DASH-CF.
Dietary controls were accomplished by using dietary counseling to follow a prescribed menu (7-d cycle) of specific foods and beverages to achieve desired energy, macronutrient, and micronutrient intakes. All meat products were provided to subjects and included fresh pork tenderloin and uncured ham trimmed of visible fat during the DASH-P and boneless, skinless chicken breast and tilapia fillets during the DASH-CF. Two servings of beef tenderloin trimmed of visible fat were provided per week during both interventions. Other items, including some snacks and condiments, were also provided to control sodium intake. The remaining items on the menu were purchased by subjects at a local grocery store by using a detailed, brand-specific shopping list provided by the research dietitian. The 6-wk DASH-style diet interventions (DASH-P and DASH-CF) were designed to meet 100% of subjects’ estimated daily energy requirements on the basis of the Institute of Medicine energy-requirement equations for overweight and obese adults (18). All menus were developed with Pronutra software (version 3.3; Viocare Inc.). Subjects completed a daily menu checklist during the DASH-P and DASH-CF to record meal times and note any deviations from the prescribed menu, which were used for the determination of dietary compliance. Menu checklists from 3 d during the last 2 wk of each intervention period (including any deviations from the prescribed menu) and 3-d dietary records completed during PI-1 and PI-2 were assessed for energy and nutrient contents by a registered dietitian with Nutrition Data System for Research software (NDSR 2012; Nutrition Coordinating Center). All diet-related activities and assessments were performed in conjunction with the NIH-supported Indiana Clinical Research Center Bionutrition Facility at Purdue University.
Body mass and composition
Body mass and percentage of body fat were determined by using the BOD POD Gold Standard Body Composition Tracking System (COSMED USA Inc.).
BP assessment
BP was assessed manually (HEM-780; Omron Healthcare Inc.) and by using a 24-h ambulatory BP monitoring system (Oscar2; SunTech Medical Inc.) on 3 d during PI-1 and PI-2 and 3 d during the final 2 wk of DASH-P and DASH-CF interventions. The ambulatory BP monitor measured BP at 30-min intervals during the day (0800–2100) and at 90-min intervals during the night (2100–0800). Twenty-four-hour ambulatory BP assessments were considered valid if ≥80% of scheduled measurements were obtained without error. If the error rate exceeded 20%, subjects were asked to wear the monitor for an additional 24 h. Manual BP was measured in seated and supine positions in the morning after 15 min of rest. Two manual BP measurements were made in each position (a third measurement was done if these BP values differed by ≥3 mm Hg) and were averaged.
Blood and urine analyses
Fasting state blood samples were collected on 1 d during PI-1 and PI-2 and during the final week of DASH-P and DASH-CF interventions. Blood samples were collected into serum separator tubes and centrifuged for 15 min at 4400 rpm and 4°C to obtain serum. Serum samples were stored at −80°C until thawed for analyses. Fasting glucose, total cholesterol, HDL cholesterol, triacylglycerol, and blood urea nitrogen (BUN) were analyzed with enzymatic colorimetry by using oxidase methods on a COBAS Integra 400 analyzer (Roche Diagnostic Systems). LDL cholesterol was calculated automatically on a COBAS Integra 400 analyzer by using measured values for total cholesterol, HDL cholesterol, triacylglycerol, and the following equation:
 |
Fasting serum insulin was analyzed by using an electrochemiluminescence immunoassay method on an Elecsys 2010 analyzer (Roche Diagnostic Systems).
On 3 d during PI-1 and PI-2 and the final 2 wk of DASH-P and DASH-CF interventions, 24-h urine volumes [weight divided by specific gravity (Digital Probe Refractometer; Misco Products Division)] were obtained from 24-h urine collections, and aliquots were stored at −20°C until thawed for subsequent analyses of urinary urea nitrogen (UUN) (COBAS Integra 400).
Statistical analysis
Power calculations for the estimation of the required sample size were completed by using changes in SBP observed in the original DASH study. In a parallel study design, the DASH diet reduced SBP by a mean (±SD) of 5.5 ± 8.2 mm Hg more than the control diet did (4). This result corresponded to an effect size of 0.67, and our power calculations indicated that a sample size of 19 was sufficient to determine an effect of this magnitude under the following assumptions: power = 0.8, α = 0.05, and with the use of a 2-tailed paired test. Primary outcomes for this study included within-diet changes in BP (pre– compared with post–DASH diet interventions) and comparisons of postintervention BP values for the DASH-P and DASH-CF.
All statistical analyses were completed with SAS software (version 9.2; SAS Institute), and data are presented as means (±SEMs). Analyses were completed by using data from the 19 subjects who completed all study procedures. The 5 subjects who withdrew from the study after random assignment did so before completing any postintervention testing. Therefore, data necessary to perform an intent-to-treat analysis were not available for these subjects. Comparisons of seated manual SBP and DBP at PI-1 and PI-2 were made by using paired t tests to assess the effectiveness of the 4-wk washout period. A doubly repeated-measures ANOVA (MIXED procedure; SAS version 9.2) was used to assess main effects of time (preintervention compared with postintervention), diet (DASH-P compared with DASH-CF), sex, and intervention order (first compared with second intervention periods) as well as interactions on changes in BP, indexes of metabolic health, and diet composition. A Tukey-Kramer adjustment for multiple comparisons was used as necessary for post hoc analyses.
In addition to the doubly repeated-measures ANOVA model, a repeated-measures ANOVA (MIXED procedure; SAS version 9.2) was used for direct comparisons of diet-level effects by comparing mean preintervention and postintervention values and change values (postintervention minus preintervention) for all measures of manual and ambulatory BP during the DASH-P and DASH-CF. This ANOVA model also assessed main effects intervention order. Statistical significance was assigned at P < 0.05 for all analyses.
RESULTS
Subject characteristics
On average, the 19 subjects who completed the study were 61 y old, obese, and presented with manual seated BP measurements in the prehypertensive range as defined by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (19) (Table 1). Seven subjects (37%) were taking antihypertensive medications, and 3 subjects (16%) were taking medications for hypercholesterolemia. Average values at PI-1 for fasting serum glucose, insulin, total cholesterol, LDL cholesterol, HDL cholesterol, triacylglycerol, and BUN were within normal reference ranges (Table 1). At PI-1, an unpaired t test indicated that manual SBP, fasting serum glucose, and UUN were greater in men than in women, whereas women had a greater percentage of body fat and HDL cholesterol concentrations (P < 0.05).
TABLE 1.
Participant characteristics at preintervention 11
| Variable | Combined (n = 19) | Women (n = 13) | Men (n = 6) |
| Age, y | 61 ± 2 | 60 ± 2 | 63 ± 3 |
| Body mass, kg | 86.4 ± 3.7 | 80.7 ± 3.3 | 98.8 ± 7.3* |
| BMI, kg/m2 | 30.9 ± 1.4 | 30.5 ± 1.8 | 31.8 ± 2.4 |
| Percentage of body fat | 41.7 ± 2.1 | 44.7 ± 2.0† | 35.2 ± 4.2 |
| Manual SBP,2 mm Hg | 130 ± 2 | 127 ± 3 | 136 ± 3* |
| Manual DBP,2 mm Hg | 85 ± 2 | 85 ± 2 | 86 ± 4 |
| Total 24-h SBP, mm Hg | 133 ± 2 | 131 ± 2 | 137 ± 3 |
| Total 24-h DBP, mm Hg | 78 ± 2 | 78 ± 2 | 80 ± 3 |
| Glucose, mg/dL | 93 ± 2 | 90 ± 1 | 100 ± 4* |
| Insulin, μU/mL | 12.61 ± 2.10 | 10.39 ± 1.48 | 17.42 ± 5.66 |
| Total cholesterol, mg/dL | 199 ± 9 | 206 ± 12 | 186 ± 8 |
| LDL cholesterol, mg/dL | 120 ± 8 | 123 ± 11 | 114 ± 7 |
| HDL cholesterol, mg/dL | 54 ± 2 | 58 ± 3† | 47 ± 3 |
| Triglycerides, mg/dL | 121 ± 11 | 121 ± 15 | 119 ± 18 |
| BUN, mg/dL | 15 ± 1 | 15 ± 1 | 17 ± 1 |
| UUN, mg/d | 10,428 ± 677 | 8971 ± 484 | 13,586 ± 1045* |
All values are means ± SEMs. *,†Unpaired t tests were used to test for differences in participant characteristics at preintervention 1; *greater than women, P < 0.05; †greater than men, P < 0.05. BUN, blood urea nitrogen; DBP, diastolic blood pressure; SBP, systolic blood pressure; UUN, urinary urea nitrogen.
Measured in the seated position.
Diet analysis
Compliance to the dietary intervention was ≥95% for both the DASH-P and DASH-CF on the basis on comparisons of the prescribed menus and deviations from the menu reported on menu checklists (Supplemental Table 1). No differences in energy intake, macronutrient distribution, and micronutrient consumption were detected between pre–DASH-P and pre–DASH-CF interventions (Table 2). Total energy intake, carbohydrate (g/d), fat (g/d), saturated fat (g/d and percentage of energy), and micronutrient consumption during the DASH-P and DASH-CF were not different when all reported menu deviations were accounted for. Macronutrient distributions (percentage of carbohydrate:percentage of protein:percentage of fat) were 58:17:25 during the DASH-P and 55:18:27 during the DASH-CF, and minor differences in macronutrient distributions were statistically confirmed. The reported percentages of energy from protein and fat were slightly lower and the percentage of energy from carbohydrates was slightly higher during the DASH-P than during DASH-CF (Table 2). Compared with pre–DASH-style diet intervention periods, subjects reported greater consumption of total energy, carbohydrate, protein, fiber, calcium, potassium, and magnesium and decreased total fat and sodium consumption during DASH-P and DASH-CF interventions (Table 2). As expected, men consumed greater amounts of total energy, carbohydrate, protein, fat, saturated fat, fiber, calcium, sodium, potassium, magnesium, and iron than women did. However, when expressed as percentages of total energy, carbohydrate, protein, fat, and saturated fat intakes were not different between men and women. Reported fiber intakes for men and women were not different at pre–DASH-style diet intervention periods (men: 22 ± 2 g/d; women: 21 ± 2 g/d), but men reported greater fiber intake during DASH-style diet interventions (53 ± 4 g/d) than did women (39 ± 1 g/d). No other sex × time interactions were observed.
TABLE 2.
Reported daily dietary intakes1
| Pre–DASH-P | DASH-P | Pre–DASH-CF | DASH-CF | |
| Energy, kcal/d | 2186 ± 148c | 2546 ± 124a,b | 2272 ± 124b,c | 2613 ± 122a |
| Carbohydrate, En% | 46.0 ± 0.9c | 58.1 ± 0.5a | 47.0 ± 1.2c | 54.7 ± 0.6b |
| Protein, En% | 16.1 ± 0.7b,c | 16.5 ± 0.2b,c | 15.1 ± 0.7c | 17.9 ± 0.4a |
| Fat, En% | 37.9 ± 1.0a | 25.4 ± 0.5c | 37.9 ± 1.0a | 27.3 ± 0.5b |
| Saturated fat, En% | 13.0 ± 0.5a | 7.5 ± 0.2b | 12.3 ± 0.7a | 7.5 ± 0.2b |
| Carbohydrate, g/d | 251 ± 17b | 370 ± 19a | 265 ± 15b | 359 ± 18a |
| Protein, g/d | 87 ± 7c | 105 ± 4b | 84 ± 5c | 116 ± 5a |
| Fat, g/d | 93 ± 7a,b | 72 ± 4c | 97 ± 7a | 79 ± 4b,c |
| Saturated fat, g/d | 32 ± 3a | 21 ± 1b | 32 ± 3a | 22 ± 1b |
| Fiber, g/d | 20 ± 2b | 43 ± 2a | 23 ± 2b | 43 ± 3a |
| Sodium, mg/d | 3453 ± 368a | 2579 ± 112b | 3495 ± 240a | 2665 ± 112b |
| Calcium, mg/d | 936 ± 98b | 1714 ± 125a | 957 ± 68b | 1795 ± 99a |
| Potassium, mg/d | 2746 ± 157a | 5162 ± 253a | 2809 ± 172b | 4995 ± 256a |
| Magnesium, mg/d | 303 ± 23b | 523 ± 24a | 338 ± 17b | 526 ± 22a |
| Iron, mg/d | 14.3 ± 1.1b | 19.9 ± 1.5a | 16.4 ± 1.4a,b | 18.2 ± 1.1a,b |
All values are means ± SEMs, n = 19. Energy and nutrient intakes were determined from menu checklists (including all menu deviations) from 3 d during the last 2 wk of the DASH-P and DASH-CF interventions and from 3-d dietary records, which were completed during preintervention phases. A repeated-measures ANOVA (MIXED procedure, SAS version 9.2; SAS Institute) was used to test differences in dietary intake during study phases. Values in the same row with different superscript letters are significantly different, Tukey-adjusted P < 0.05. DASH-CF, Dietary Approaches to Stop Hypertension diet with chicken and fish; DASH-P, Dietary Approaches to Stop Hypertension diet with pork; En%, percentage of energy.
Body composition
Body mass was higher during the first DASH-style diet intervention than the second diet intervention (main effect of intervention order). However, this effect was not influenced by the diet type (DASH-P or DASH-CF). Body mass was 2.3 ± 0.2 kg lower (P < 0.05) at postintervention than at preintervention (postintervention: 83.3 ± 2.6 kg; preintervention: 85.5 ± 2.6 kg), and the body fat percentage tended to be lower at postintervention (preintervention: 41.1 ± 1.5%; postintervention: 39.2 ± 1.6%; P = 0.06).
Blood and urine analyses
Consumption of DASH-style diets for 6 weeks did not affect fasting serum glucose (preintervention: 93 ± 1 mg/dL; postintervention: 94 ± 1 mg/dL), insulin (preintervention: 13.4 ± 2.1 μU/mL; postintervention: 10.8 ± 1.0 μU/mL), triacylglycerol (preintervention: 115 ± 8 mg/dL; postintervention: 105 ± 5 mg/dL), LDL-cholesterol (preintervention: 119 ± 5 mg/dL; postintervention: 106 ± 5 mg/dL), or BUN (preintervention: 16 ± 1 mg/dL; postintervention: 16 ± 1 mg/dL) concentrations. UUN was increased at postintervention (11,545 ± 470 mg/d) compared with at preintervention (10,546 ± 476 mg/d), and this effect was not influenced by the diet type (DASH-P or DASH-CF) or intervention order. Significant time × diet interactions (P < 0.05) were observed for changes in total cholesterol and HDL cholesterol after the DASH-style diet interventions. Specifically, total cholesterol was decreased after the DASH-P (preintervention: 202 ± 9 mg/dL; postintervention: 176 ± 7 mg/dL; P-within-diet change < 0.05) but not the DASH-CF (preintervention: 196 ± 8 mg/dL; postintervention: 183 ± 8 mg/dL; P-within-diet change = 0.16). Similarly, HDL cholesterol was decreased after the DASH-P (preintervention: 58 ± 4 mg/dL; postintervention: 52 ± 3 mg/dL; P-within-diet change < 0.05) but not the DASH-CF (preintervention: 55 ± 3 mg/dL; postintervention: 52 ± 3 mg/dL; P-within-diet change = 0.17). However, a direct comparison of postintervention values indicated no differences in total cholesterol (P = 0.11) or HDL cholesterol (P = 0.60) after the DASH-P and DASH-CF.
BP
No differences in manual seated SBP (130 ± 2 compared with 129 ± 2 mm Hg; P = 0.38) or DBP (85 ± 2 compared with. 84 ± 1 mm Hg; P = 0.09) were observed between PI-1 and PI-2, respectively, which confirmed the effectiveness of the washout period. Preintervention measures of manual (seated and supine) and ambulatory (total 24 h, daytime, and nighttime) SBP and DBP were not different (Supplemental Tables 2 and 3).
A doubly repeated-measures ANOVA indicated that seated and supine manual SBP and DBP and total 24-h, daytime, and nighttime SBP and DBP were decreased after the DASH-style diet interventions, and these reductions in BP were not influenced by the diet type (DASH-P or DASH-CF) or intervention order (Supplemental Tables 2 and 3).
To further evaluate the effects of the predominant protein source in a DASH-style diet on BP, mean postintervention values for DASH-P and DASH-CF were compared by using a repeated-measures ANOVA. Postintervention values after the DASH-P and DASH-CF were not different (Table 3).
TABLE 3.
Postintervention manual and 24-h ambulatory blood pressure measurements1
| DASH-P | DASH-CF | |
| Manual blood pressure, mm Hg | ||
| Seated SBP | 122 ± 2 | 123 ± 3 |
| Seated DBP | 79 ± 1 | 78 ± 1 |
| Supine SBP | 118 ± 2 | 118 ± 2 |
| Supine DBP | 73 ± 1 | 72 ± 1 |
| Ambulatory blood pressure, mm Hg | ||
| Total 24-h SBP | 127 ± 2 | 123 ± 2 |
| Total 24-h DBP | 76 ± 1 | 73 ± 1 |
| Daytime SBP | 129 ± 2 | 127 ± 2 |
| Daytime DBP | 78 ± 1 | 75 ± 2 |
| Nighttime SBP | 118 ± 2 | 115 ± 2 |
| Nighttime DBP | 69 ± 1 | 66 ± 1 |
All values are means ± SEMs, n = 19. A repeated-measures ANOVA (MIXED procedure, SAS version 9.2; SAS Institute) was used to test for differences between post–DASH-P and post–DASH-CF mean values of seated and supine manual and total 24-h, daytime (0800–2100), and nighttime (2100–0800) ambulatory SBP and DBP. No differences in mean postintervention SBP or DBP values were observed between the DASH-P and DASH-CF. DASH-CF, Dietary Approaches to Stop Hypertension diet with chicken and fish; DASH-P, Dietary Approaches to Stop Hypertension diet with pork; DBP, diastolic blood pressure; SBP, systolic blood pressure.
DISCUSSION
The primary aim of this study was to assess whether the inclusion of lean, minimally processed pork into a DASH-style dietary pattern would influence the expected beneficial effects on BP (4–6). Consistent with our hypothesis, consumption of a DASH-style dietary pattern reduced BP, and the substitution of lean pork for chicken and fish did not influence these effects. These results indicate that lean pork can be effectively incorporated into a DASH-style eating pattern for lowering BP in adults with elevated BP.
In the current study, DASH-style diets decreased manual seated SBP/DBP by 7/6 mm Hg and total 24-h SBP/DBP decreased 7/4 mm Hg. These BP reductions were similar to those reported in a recent meta-analysis of the effects of a DASH diet on BP reduction in people with hypertension (−7/−4 mm Hg) (6) and to those reported by Sacks et al. (5) for the intermediate sodium-level DASH diet (−7/−3 mm Hg).
Total cholesterol and HDL cholesterol were decreased after the DASH-P but not after the DASH-CF. However, note that our study was statistically powered to detect changes in BP. Measurements of body composition and other indicators of cardiometabolic health were secondary outcomes, and therefore, changes in these variables should be interpreted with caution. For comparison, a study that assessed effects of incorporating lean beef into a DASH-style dietary pattern in hypercholesterolemic patients showed no differences in changes in total cholesterol and LDL cholesterol in DASH-style diets that were rich in either poultry and fish or lean beef (14).
Participants lost ∼2 kg body mass during the 6-wk interventions despite a prescription for energy balance and higher reported energy intakes during the DASH-style diet interventions compared with during preintervention periods. This discrepancy between reported energy intake and changes in body weight were likely explained by the known issues with underreporting on diet records in obese individuals (20). Regardless, reported intakes of macronutrients and micronutrients during the DASH-style diets were consistent with the transition from a typical American diet to a DASH-style dietary pattern. Specifically, increases in calcium, magnesium, and potassium are indicative of increases in consumption of dairy foods, whole grains, and fruit and vegetables, and a decrease in sodium reflects decreased salt consumption.
The novelty of the current study is supported by the apparent lack, to our knowledge, of any previously published studies on the inclusion of pork in a DASH-style diet. However, at least 2 studies assessed the effects of including lean beef in a DASH-style diet on BP responses (12, 13). In the BOLD (Beef in an Optimal Lean Diet) study, SBP was decreased by 4 mm Hg after the consumption of a DASH-style diet with 153 g lean beef/d but was not decreased after DASH-style diets with 113 or 28 g lean beef/d, and DBP was not influenced by any of the 3 DASH-style diets (12). The BOLD study was conducted in normotensive subjects, whereas the majority of DASH-style diet interventions have studied individuals with elevated BP (6).
Our results are perhaps more directly comparable to those of Nowson et al. (13), who studied subjects of a similar average age (60 y), BMI (in kg/m2; 29.5), and SBP/DBP (128/81 mm Hg) as in the current study (age: 61 y; BMI: 30.9; SBP/DBP: 130/85 mm Hg). A DASH-style diet with six 100-g servings of lean beef/wk reduced SBP/DBP by 6/4 mm Hg compared with consumption of a low-fat diet with ≤2 servings red meat/wk, which lowered SPB/DBP by 3/3 mm Hg (13). Collectively, results from the current, BOLD (12), and Nowson et al. (13) studies showed that the inclusion of lean red meat in DASH-style diets does not influence their effectiveness to reduce BP. In addition, results of the current study further support previous research that showed that diets rich in lean pork do not adversely affect cardiometabolic health compared with other animal sources of protein (21–23).
It is common for healthy diet patterns, including the DASH (3), American Heart Association diet (7), and Mediterranean diet (24), to recommend limiting red meat consumption on the basis of concerns regarding saturated fat and sodium contents and a positive correlation between consumption of red meat and mortality (25, 26), cardiovascular disease (27, 28), and cancer (29–31). However, the extent of processing may have a modulating effect on these relations. Minimally processed (typically described as unprocessed) red meat often shows no or an attenuated correlation with chronic disease risk compared with that for more extensively processed meat (typically described as processed) (25, 32, 33). However, some studies suggested increased risk of cardiovascular disease regardless of the extent of processing (26, 28). Of particular relevance to the current study, a large prospective study of 44,616 French women reported a 17% increased rate of hypertension in women who consumed ≥5 servings of processed red meat/wk, but no increased risk was shown for high consumers (≥5 servings/wk) of unprocessed red meat (RR: 0.99; 95% CI: 0.91, 1.08) (33).
It is also important to consider the degree of variability in total and saturated fat in cuts of unprocessed red meats that may differentially affect disease risk. With regard to pork specifically, total and saturated fat contents range from 3.5 and 1.2 g/100 g raw pork tenderloin, respectively, to 23.4 and 7.0 g/100 g raw pork spareribs, respectively, according to USDA analyses (34), and the fat content of unprocessed beef is similarly variable (35). Being cognizant of this variability, the results of the current study should be interpreted narrowly and only apply to cuts of unprocessed lean pork used in the study (tenderloin and fresh, uncured ham trimmed of visible fat) and other unprocessed cuts of pork meeting USDA guidelines for extra lean and lean. In addition, disease risk may be influenced by the larger dietary pattern, and therefore, results of this study apply only to the consumption of minimally processed lean pork in the context of a highly controlled DASH-style diet for a 6-wk period. Whether the consumption of these cuts of pork in the context of other dietary patterns and for longer periods of time would be similarly effective for BP reduction, and a potential reduction in chronic disease risk, requires additional investigation.
The current study had several strengths. With the use of a randomized crossover study design with an effective washout period, the current study achieved reductions in BP that were similar to previously published results from other DASH diet interventions. With the provision of study participants with all meat products (pork, chicken, fish, and beef) and intensive counseling and menu planning with a registered dietitian, we were able to achieve a high level of dietary adherence to the DASH-style dietary pattern as verified by daily menu checklists. BP measurements can be highly variable and are often influenced by the environment (e.g., “white coat hypertension”) (36, 37). To account for this known issue with the assessment of changes in BP, ∼30 manual and >450 ambulatory BP measurements were collected on each participant throughout his or her participation in the study, which increased the confidence in the results considerably. A limitation of the current study was the relatively high dropout rate. Of 9 subjects who withdrew, 5 individuals did so during the first 2 wk of dietary intervention, which indicated the potential challenges of adhering to a DASH-style dietary pattern. This challenge is likely even greater in a free-living setting where individuals would be responsible for planning and selecting their own food.
In conclusion, the substitution of lean pork for chicken and fish as the predominant source of dietary protein does not influence the effectiveness of a DASH-style diet to reduce systolic and diastolic BPs in adults with elevated BP. The results, which were obtained when BPs were measured by using traditional clinical and 24-h ambulatory techniques, support that minimally processed lean pork can be included in DASH-style diet for BP reduction.
Acknowledgments
We thank Jan Green and Lauren O’Connor for their assistance with clinical assessments and data entry.
The authors’ responsibilities were as follows—WWC: designed the research project; AJW: created diet intervention menus and oversaw dietary counseling with study participants; RDS: was responsible for participant recruitment and conducting the research; NC and RDS: performed statistical analyses; RDS and WWC: wrote the manuscript; and all authors: took responsibility for the final content of the manuscript. WWC received funding from the National Pork Board for the research reported in this article. RDS, AJW, and NC reported no conflicts of interest.
Footnotes
Abbreviations used: BP, blood pressure; BOLD, Beef in an Optimal Lean Diet; BUN, blood urea nitrogen; DASH, Dietary Approaches to Stop Hypertension; DASH-CF, Dietary Approaches to Stop Hypertension diet with chicken and fish; DASH-P, Dietary Approaches to Stop Hypertension diet with pork; DBP, diastolic blood pressure; PI-1, preintervention 1; PI-2, preintervention 2; SBP, systolic blood pressure; UUN, urinary urea nitrogen.
REFERENCES
- 1.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20. [DOI] [PubMed] [Google Scholar]
- 2.Nwankwo T, Yoon SS, Burt V, and Gu Q, Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011-2012. NCHS Data Brief 2013;133:1–8. [PubMed]
- 3.Vogt TM, Appel LJ, Obarzanek E, Moore TJ, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Cutler JA, Windhauser MM, et al. Dietary Approaches to Stop Hypertension: rationale, design, and methods. DASH Collaborative Research Group. J Am Diet Assoc 1999;99(8 Suppl):S12–8. [DOI] [PubMed] [Google Scholar]
- 4.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997;336:1117–24. [DOI] [PubMed] [Google Scholar]
- 5.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 6.Saneei P, Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. Nutr Metab Cardiovasc Dis 2014;24:1253–61. [DOI] [PubMed] [Google Scholar]
- 7.Eckel RH, Jakicic JM, Ard JD, Hubbard VS, de Jesus JM, Lee IM, Lichtenstein AH, Loria CM, Millen BE, Miller NH, et al. AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(25 Suppl 2):S76–99. [DOI] [PubMed] [Google Scholar]
- 8.Daniel CR, Cross AJ, Koebnick C, Sinha R. Trends in meat consumption in the USA. Public Health Nutr 2011;14:575–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis CG, Lin BH. Factors affecting U.S. pork consumption. Washington (DC): Economic Research Service/USDA; 2005.
- 10.Touyz RM, Briones AM. Reactive oxygen species and vascular biology: implications in human hypertension. Hypertens Res 2011;34:5–14. [DOI] [PubMed] [Google Scholar]
- 11.FDA [Internet]. Guidance for industry: a food labeling guide (10. Appendix B: additional requirements for nutrient content claims). 2014 [cited 2015 Feb 12]. Available from: http://www.fda.gov/food/guidanceregulation/guidancedocumentsregulatoryinformation/labelingnutrition/ucm064916.htm.
- 12.Roussell MA, Hill AM, Gaugler TL, West SG, Ulbrecht JS, Vanden Heuvel JP, Gillies PJ, Kris-Etherton PM. Effects of a DASH-like diet containing lean beef on vascular health. J Hum Hypertens 2014;28:600–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nowson CA, Wattanapenpaiboon N, Pachett A. Low-sodium Dietary Approaches to Stop Hypertension-type diet including lean red meat lowers blood pressure in postmenopausal women. Nutr Res 2009;29:8–18. [DOI] [PubMed] [Google Scholar]
- 14.Roussell MA, Hill AM, Gaugler TL, West SG, Heuvel JP, Alaupovic P, Gillies PJ, Kris-Etherton PM. Beef in an Optimal Lean Diet study: effects on lipids, lipoproteins, and apolipoproteins. Am J Clin Nutr 2012;95:9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120:1640–5. [DOI] [PubMed] [Google Scholar]
- 16.Karanja NM, Obarzanek E, Lin PH, McCullough ML, Phillips KM, Swain JF, Champagne CM, Hoben KP. Descriptive characteristics of the dietary patterns used in the Dietary Approaches to Stop Hypertension Trial. DASH Collaborative Research Group. J Am Diet Assoc 1999;99(8 Suppl):S19–27. [DOI] [PubMed] [Google Scholar]
- 17.Svetkey LP, Sacks FM, Obarzanek E, Vollmer WM, Appel LJ, Lin PH, Karanja NM, Harsha DW, Bray GA, Aickin M, et al. The DASH Diet, Sodium Intake and Blood Pressure Trial (DASH-Sodium): rationale and design. DASH-Sodium Collaborative Research Group. J Am Diet Assoc 1999;99(8 Suppl):S96–104. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine (US), Panel on Macronutrients. and Institute of Medicine (US), Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington (DC): National Academies Press; 2005.
- 19.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr. , et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206–52. [DOI] [PubMed] [Google Scholar]
- 20.Trabulsi J, Schoeller DA. Evaluation of dietary assessment instruments against doubly labeled water, a biomarker of habitual energy intake. Am J Physiol Endocrinol Metab 2001;281:E891–9. [DOI] [PubMed] [Google Scholar]
- 21.Murphy KJ, Thomson RL, Coates AM, Buckley JD, Howe PR. Effects of eating fresh lean pork on cardiometabolic health parameters. Nutrients 2012;4:711–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murphy KJ, Parker B, Dyer KA, Davis CR, Coates AM, Buckley JD, Howe PR. A comparison of regular consumption of fresh lean pork, beef and chicken on body composition: a randomized cross-over trial. Nutrients 2014;6:682–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wycherley TP, Noakes M, Clifton PM, Cleanthous X, Keogh JB, Brinkworth GD. A high-protein diet with resistance exercise training improves weight loss and body composition in overweight and obese patients with type 2 diabetes. Diabetes Care 2010;33:969–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, Trichopoulos D. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr 1995;61(6 Suppl):1402S–6S. [DOI] [PubMed] [Google Scholar]
- 25.Larsson SC, Orsini N. Red meat and processed meat consumption and all-cause mortality: a meta-analysis. Am J Epidemiol 2014;179:282–9. [DOI] [PubMed] [Google Scholar]
- 26.Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Stampfer MJ, Willett WC, Hu FB. Red meat consumption and mortality: results from 2 prospective cohort studies. Arch Intern Med 2012;172:555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen GC, Lv DB, Pang Z, Liu QF. Red and processed meat consumption and risk of stroke: a meta-analysis of prospective cohort studies. Eur J Clin Nutr 2013;67:91–5. [DOI] [PubMed] [Google Scholar]
- 28.Bernstein AM, Sun Q, Hu FB, Stampfer MJ, Manson JE, Willett WC. Major dietary protein sources and risk of coronary heart disease in women. Circulation 2010;122:876–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Song P, Lu M, Yin Q, Wu L, Zhang D, Fu B, Wang B, Zhao Q. Red meat consumption and stomach cancer risk: a meta-analysis. J Cancer Res Clin Oncol 2014;140:979–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhu HC, Yang X, Xu LP, Zhao LJ, Tao GZ, Zhang C, Qin Q, Cai J, Ma JX, Mao WD, et al. Meat consumption is associated with esophageal cancer risk in a meat- and cancer-histological-type dependent manner. Dig Dis Sci 2014;59:664–73. [DOI] [PubMed] [Google Scholar]
- 31.Chan DS, Lau R, Aune D, Vieira R, Greenwood DC, Kampman E, Norat T. Red and processed meat and colorectal cancer incidence: meta-analysis of prospective studies. PLoS ONE 2011;6:e20456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation 2010;121:2271–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lajous M, Bijon A, Fagherazzi G, Rossignol E, Boutron-Ruault MC, Clavel-Chapelon F. Processed and unprocessed red meat consumption and hypertension in women. Am J Clin Nutr 2014;100:948–52. [DOI] [PubMed] [Google Scholar]
- 34.Patterson KY, Trainer D, Holden JM, Howe JC. USDA nutrient data set for fresh pork (from SR), Release 2.0. Beltsville (MD): Agricultural Research Service/USDA; 2009.
- 35.Roseland JM, Nguyen QV, Williams JR, Patterson KY. USDA nutrient data set for retail beef cuts from SR, release 3.0. Beltsville (MD): Agricultural Research Service/USDA; 2013.
- 36.Turner JR, Viera AJ, Shimbo D. Ambulatory blood pressure monitoring in clinical practice: a review. Am J Med 2015;128:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Franklin SS, Thijs L, Hansen TW, O'Brien E, Staessen JA. White-coat hypertension: new insights from recent studies. Hypertension 2013;62:982–7. [DOI] [PubMed] [Google Scholar]