Abstract
Background
A multidisciplinary team in Australia and New Zealand utilized a current decision-making theory to develop the ‘My Kidneys, My Choice’ decision aid (MKDA) to support end-stage kidney disease (ESKD) treatment options in decision-making. Assessment of the MKDA was deemed critical to practice integration.
Methods
A multisite pre-test, post-test study design was used. Routine ESKD education was supported by the MKDA. Knowledge levels, worries and priorities were assessed pre- and post-education with Likert-scale questions. MKDA usability and treatment option preferences were surveyed post-test. Data were analysed in SPSS.
Results
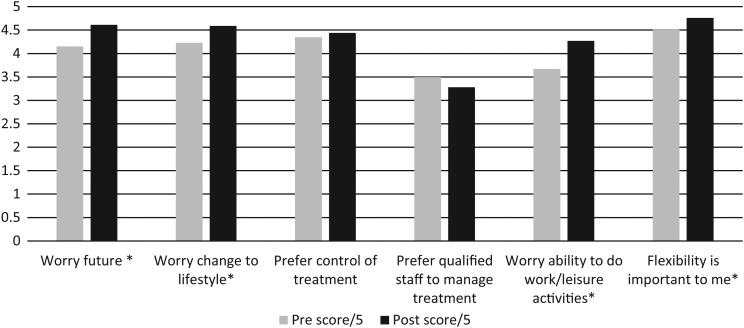
Ninety-seven participants completed the pre-survey and 72 (70%) the post-survey. Mean pre-test knowledge scores ranged from: 0.88 (SD 1.5) for conservative care to 1.32 (SD 1.3) for centre-based dialysis. Post-decision-making knowledge levels increased significantly (P < 0.001). Worry and flexibility scores all increased significantly (P < 0.05) from pre- to post-test; about future pre- 4.15 (SD 1.3), post- 4.61 (SD 0.76); change to lifestyle 4.23 (SD 1.05), 4.59 (SD 0.8); ability to work/do leisure activities 3.67 (SD 1.56) 4.27 (SD 1.17) and desire for flexibility 4.51 (SD 0.86), 4.76 (SD 0.66). MKDA usability scores were high: easy to understand 4.64, (SD 0.77), easy to follow 4.65, (SD 0.66) and supporting decision-making 4.76 (SD 0.61). MKDA section scores ranged from 4.21 (SD 0.75) for writing treatment choices to 4.90 (SD 0.41) for the use of the treatment option comparison grid.
Conclusions
Preliminary MKDA assessment revealed high patient acceptance and usability. Patients had equitable knowledge of all treatment options but experienced higher post-worries levels than anticipated.
Keywords: decision aid, dialysis, education, ESRD, shared decision-making
Introduction
Chronic kidney disease (CKD) in Australia is estimated to progress to end-stage kidney disease (ESKD) leading to commencement of treatment for ∼2544 people per year [1]. One key aim of management of ESKD is to adequately educate and prepare for renal replacement therapy (RRT). RRT includes dialysis and transplantation, but conservative care (CC) is also chosen by many. Dialysis options include haemodialysis (HD), which can be centre-based (CBD) or done at home (HHD), and peritoneal dialysis (PD) which can be continuous ambulatory PD (CAPD) or automated PD (APD). Lifestyle, particularly for those on dialysis, and to a lesser extent health outcomes, are affected by the choice of treatment. CC is management by diet, medications and palliative care but no dialysis meaning that life is not artificially prolonged.
Informed decision-making for patients and carers is acknowledged by international renal guidelines as a critical component of treatment option decision-making [2–4]. Shared decision-making (SDM) is a more advanced strategy for decision-making that has more recently become the gold standard. SDM is defined as the health professional with clinical expertise, supporting the life experts; the patient and their significant others through an SDM process [5]. SDM can be enhanced by the use of a patient decision aid (ptDA), particularly where lifestyle influences the SDM process as with ESKD [6].
In 2009, a world-wide systematic review of decision-making for those with ESKD yielded zero primary articles of research [7]. A further search in 2012 found four ESKD ptDA were in use or under development; an online Canadian tool [8], a paper-based decision aid from Yorkshire (YoDDA) in the UK [9], the American Match-D tool [10] and a comprehensive Canadian 159 page education handbook with a video [11].
A 2013 literature search focusing on effectiveness of ptDAs in assisting participants in making a decision for lifesaving treatment options revealed three randomized, controlled trials evaluating ptDAs and two studies which were a pre-test, post-test design without a control group for other clinical conditions (Grennan, unpublished) [12, 13] but none related to ESKD. YoDDA however has since been evaluated utilizing multiple strategies including qualitative interviews on content, a before-and-after acceptability study and an online survey demonstrating high consumer acceptance [14]. A 2014 Cochrane review of ptDA validates their use and demonstrates an increase in patients selecting an option related to their values [relative risk (RR) 1.51, 95% confidence interval (CI) 1.17–1.96], reduced decision-making passivity (RR 0.66, 95% CI 0.53–0.81), reduced conflict and improved levels of knowledge [6].
Educational practices for ESKD treatment option decision-making in Australian renal units during 2012 demonstrated wide variance with no reported use of ptDA [15]. This was initiated following a 2011 Australian dialysis consumer perspectives survey that found that 49% of patients did not have a choice in their dialysis type [16]. Knowledge of current SDM theory and determination of these local practice gaps led to the development of ‘My Kidneys, My Choice’ ptDA (MKDA) by a multidisciplinary group, including consumer input. It followed the principles of the International Patient Decision Aid Standards Collaboration (IPDAS) guidelines for ptDA development [17]. The first version was completed in November 2012 [18, 19]. The MKDA is split into five clear sections. ‘My Kidneys’ and ‘My Lifestyle’, which aim to enhance the process of SDM by prioritizing the value of the patient lifestyle, ‘My Options’ which are two summary grids, ‘My Choice’ and ‘My Questions’.
The IPDAS (2005) guidelines specify that, in order to establish the effectiveness of a ptDA, it is critical to provide evidence that the ptDA ‘(i) improves the quality of the decision-making process and (ii) decision quality, that is the quality of the choice that is made’ [20]. This is reported through measurable outcomes, such as the patient's knowledge levels and decisional conflict. Preliminary evaluation of MKDA was therefore undertaken within the Kidney Health Australia ESKD education project.
Materials and methods
Subjects
All adults who were referred for ESKD education at participating sites and who had English as a first language were eligible to participate.
The survey design was a multisite, prospective quasi-experimental design with a one-group pre-test, post-test. The survey questions were designed by the authors with input from renal health professionals experienced in research. Surveys were piloted by five consumers who used the MKDA and the final iteration was developed.
Each question offered options on a 5-point ordinal scale: strongly disagree, disagree, neutral, agree, strongly agree. Ordinal scale questions targeted knowledge, worries, values and decision-making experience with the decision aid. Additional yes/no questions targeted education methods experienced, utilization levels of the decision aid, whether decision-making involved significant others and ranking of preferred treatment options. Demographics were collected but only de-identified data were provided to the investigators. Ethical approval was obtained in accordance with the Helsinki declaration of 1975.
Four sites were enrolled; one each from Sydney, Melbourne, Perth and Brisbane. Ethics was completed according to NHMRC and hospital guidelines. The target cohort was 100 patients recruited over 12 months. The option to participate was offered to all site patients attending for first-time education with the pre-dialysis education team and who had English as a first language. Explicit consent was obtained from each participant. Control groups were not used because of site limitations on potential participants within the proposed time-frame.
The pre-survey was administered upon referral for education and mailed to the research team. Normal education processes were completed, coordinated by a specialist education nurse, with the addition of the MKDA to support decision-making. Once a decision had been made about a preferred treatment option, the participants were invited to complete the second survey.
Data analysis
The ordinal scale responses were allocated a score to allow the calculation of means. SPSS version 22 was used for analysis which included descriptive statistics, Pearson two-tailed correlations and ANOVA comparisons. Age was split at 65 years for analysis which was the median for the group and incidentally reflects the usual age of retirement.
Results
A total of 97 participants were recruited (Table 1) and completed the first survey. The second survey was completed by 72 patients (70%) with 26 patients either lost to follow-up [17], death [5] or regained renal function [4]. The only significant differences in demographics between those who did and those who did not complete the second survey was the state, with those in New South Wales (NSW) more likely to complete the second survey.
Table 1.
Demographics
| Post-survey group |
||
|---|---|---|
| Number (%) | ANZDATA | |
| Age (years) | 63.2 (SD 13.54, range 30–89) | 60 (entering dialysis) |
| Gender male | 61% | 62% |
| NSW | 47 (65%) | 31% |
| VIC | 6 (8%) | 25% |
| WA | 6 (8%) | 10% |
| QLD | 13 (18%) | 18% |
| Caucasian | 50 (69%) | 72% |
| Aboriginal/Torres Strait | 1 (1%) | 10% |
| Asian | 10 (14%) | 10% |
| European | 4 (6%) | NS |
| Other | 7 (10%) | 8% |
Acceptance of the decision aid
Acceptance of the different sections of the MKDA was high with mean scores out of 5 ranging from 4.21 (SD 0.75) for writing down treatment choices up to 4.77 (SD 0.65) and 4.90 (SD 0.41) for the use of the treatment option comparison grids (Grid 1 is a summary of all ESKD treatment options and Grid 2 is more detailed regarding dialysis options) (Table 2). For acceptance related to usability, the MKDA was also rated highly; easy to understand (4.64, SD 0.77) and easy to follow (4.65, SD 0.66). Acceptance levels were not significantly different between gender, age split by 65 years, state or ethnicity.
Table 2.
Acceptance and usability of the MKDA
| Mean score (of 5) | SD | |
|---|---|---|
| Use of treatment options grid (dialysis only) | 4.90 | 0.49 |
| Use of treatment options grid (all treatments) | 4.77 | 0.65 |
| Support for decision-making | 4.76 | 0.62 |
| Easy to follow | 4.65 | 0.66 |
| Easy to understand | 4.64 | 0.77 |
| Writing down treatment choices | 4.21 | 0.75 |
| Writing down lifestyle preferences | 4.13 | 0.78 |
The opportunity for input about future change to the MKDA was not widely used, but two comments asked for more information on private dialysis and CC, three asked for pictures, one asked for larger words and the remainder were happy with the current format.
Decision-making support
The ability of the MKDA to support decision-making was rated extremely high at 4.76 (SD 0.61). Eighty-three percent of respondents reported that they showed the MKDA to at least one significant other; 64% to partners and 32% to children. Where people reported sharing the MKDA with someone, there was a significant correlation with that person being involved in the decision-making process (P < 0.001). Partners were involved in 55% of decisions and children in 18%.
Knowledge levels
Self-reported knowledge levels about treatment options prior to education and decision-making were similar for each treatment option (Table 3). The mean score out of 4 ranged from 0.88 (SD 1.5) for CC to 1.32 (SD 1.3) for CBD. Post-decision-making knowledge levels increased significantly for all treatment options (P < 0.001) ranging from a mean of 2.93 (SD 1.0) for transplant to 3.62 (SD 0.8) for CAPD.
Table 3.
Pre- and post-scores for knowledge levels, worries, flexibility and control
| Pre score | SD | Post score | SD | Sig. P-value | |
|---|---|---|---|---|---|
| I have a thorough understanding of CBD | 1.32 | 1.564 | 3.28 | 0.897 | <0.001 |
| I have a thorough understanding of HHD | 1.11 | 1.478 | 3.23 | 0.913 | <0.001 |
| I have a thorough understanding of APD | 0.97 | 1.332 | 3.35 | 0.739 | <0.001 |
| I have a thorough understanding of CAPD | 1.06 | 1.413 | 3.62 | 0.799 | <0.001 |
| I have a thorough understanding of transplant | 1.14 | 1.476 | 2.93 | 1.046 | <0.001 |
| I have a thorough understanding of conservative care | 0.88 | 1.266 | 3.10 | 0.966 | <0.001 |
| I am worried about my future with kidney disease | 4.15 | 1.218 | 4.61 | 0.765 | <0.05 |
| I am worried about change to my lifestyle with kidney disease | 4.23 | 1.058 | 4.59 | 0.803 | <0.05 |
| I would prefer control of my treatment | 4.35 | 1.070 | 4.44 | 0.937 | |
| I would prefer qualified staff to manage my treatment | 3.50 | 1.556 | 3.28 | 1.485 | |
| I worry about my ability to work or do leisure activities | 3.67 | 1.364 | 4.27 | 1.171 | <0.05 |
| Flexibility is important to me | 4.51 | 0.856 | 4.76 | 0.665 | <0.05 |
There were significant differences in total knowledge levels, of 24, for females who scored a mean pre-education score of 7.5 compared with males who scored 5.6. Mean total post-education scores for females were 18.3, compared with 20.3 for males (increases of 10.8 and 14.7, respectively). The post-knowledge scores were significantly higher (P < 0.01) for CAPD, HHD, CBD and CC in NSW compared with Queensland (QLD). There were no knowledge differences by age or ethnicity. The pre-knowledge levels were not significantly different between the participants who did or did not complete the study.
There were significant correlations between positive evaluation of use of the MKDA and knowledge levels for CAPD (P < 0.01), APD (P < 0.05), transplant (P < 0.05) and CC (P < 0.05). There were significant correlations (P < 0.001) between the level of knowledge a participant had for one treatment option with them having similar knowledge level for all other treatment options.
Worries, flexibility and control
Prior to education and decision-making, self-reported scores out of 5 for worry, flexibility and control were fairly high (Table 3). The desire for flexibility scored the highest at 4.51 (SD 0.86) and the desire for staff to manage the treatment scored the lowest at 3.50 (SD 1.6). Males had higher mean scores than females (range +0.25 to 0.4) for every value except for preferring control of their treatment where similar values were seen. Those who were <65 years were more worried about their ability to work and their future life prior to education (P < 0.05). There were no other significant differences by state, age or ethnicity.
After decision-making, there were significant increases (P < 0.05) in all aspects of worry and the desire for flexibility (Figure 1). Preference for control only changed slightly with preference for qualified staff managing treatment declining and remaining the lowest score. There were no significant differences in mean scores between age, gender, state or ethnicity after education. However the education factors of group education, written materials, meeting patients and social worker support were significantly associated with higher level of worries (P < 0.05).
Fig. 1.
Worries, control and flexibility pre- and post-decision-making. Asterisk denotes statistically significant P value = 0.05.
Education methods
Most respondents reported multiple education methods/staff as being included during their education. This included a specialist education nurse (95%), written materials (82%), nephrologist (75%), group sessions (70%), DVDs (70%), other patients (63%), social worker (61%), dietician (39%), websites (27%) and HHD or PD staff (7 and 11%, respectively). There were state variances in education practice with those in NSW reporting an average use of 7.3 sources, QLD 4.2, Victoria (VIC) 3.5 and Western Australia (WA) 2.5.
There were significant correlations (P < 0.001) between states and education factors including provision of group education, DVD use, written information provision, involvement of other patients, input by nephrologists and social workers. In NSW, 100% of respondents reported using written materials and 95% attended group education. The involvement of a social worker, written materials and group education was associated with significantly increased worry about lifestyle, the future and the ability to work or do leisure activities (P < 0.001).
Treatment options choices
Home dialysis options were the preferred choice overall (Table 4). Sixty-two percent of people selected a home dialysis modality as their first choice; 30% CAPD, 16% APD and 16% HHD. Only 11% selected CBD, 16% transplant and 11% CC as their first choice. There were no statistically significant differences by gender although females demonstrated a tendency to choosing CAPD or CC (mean score female 2.7 versus 2.4 and 5.3 versus 4.9, respectively) and males demonstrated a higher preference for HHD and transplant (mean score male 3.3 versus 2.8 and 3.9 versus 3.5).
Table 4.
Treatment option preferences
| Mean score (rank 1–6 with 1 as preferred and 6 as last preferred) | SD | |
|---|---|---|
| Continuous ambulatory peritoneal dialysis | 2.52 | 1.40 |
| Automated peritoneal dialysis | 2.56 | 1.25 |
| Home haemodialysis | 3.09 | 1.35 |
| Centre-based dialysis | 3.43 | 1.41 |
| Transplant | 3.79 | 1.67 |
| Conservative care | 5.07 | 1.77 |
Those under 65 were more likely to select transplant (P < 0.001) compared with those over 65 years and less likely to select CBD or CC (P < 0.05). All home dialysis options were equally selected by age split by 65 years. Those in NSW were more likely to select CAPD or APD than those in QLD (P = 0.05).
Discussion
This preliminary assessment of consumer acceptance of the MKDA is positive indicating that use of a ptDA is a useful adjunct to the traditional education practices which precede decision-making about ESKD treatment options.
Knowledge levels
A key goal of the MKDA was to ensure that participants understood all treatment options equitably. A 2012 Australian survey of educational practice [15] determined that units did not present all options of treatment, further supporting the similar findings of a 2011 consumer perspectives survey [16]. This was also found in the USA where 31% of 977 patients reported that treatment options were not presented equally [21].
This survey found that there were no significant differences in levels of knowledge between different treatment types for each individual indicating equitable exposure. Interestingly, there were gender score differences pre and post, with females starting the most knowledgeable but males completing education more knowledgeable. This may indicate that females start education with some self-driven fact-finding but males once engaged are more driven to make an informed choice.
Despite a wide age range, there were no significant differences in self-reported knowledge levels between those under or over 65 years. Post-decision-making however there were some differences by state which correlated with the use of increased education methods. A Taiwanese group found that an intervention of repeat exposure to DVDs found significantly higher knowledge levels compared with standard education, resulting in less decisional conflict and highlighting that more intensive education interventions can change knowledge levels [22].
MKDA design
The MKDA was integrated successfully into education practice despite local variability in this practice. Delivering education to a wide range of individuals is also a challenge in Australian because the renal cohort varies considerably by ethnicity, educational level and age. This awareness drove the initial development of MKDA to focus mainly on the decision-making process [19]. The varied use of educational tools to support treatment options decision-making demonstrated how nurses adjust and create patient-centred education, justifying the ‘overview’ approach of MKDA. The risk of this however is that, despite similar demographics of the respondents, some sites appeared to have limited the additional education options provided from that site.
The YoDDA decision aid contrasts in design because it is both a guide to decision-making and a comprehensive educational tool [9]. It has been well received in a relatively homogenous population in the UK with 106 patients showed significant improvement in decision-making clarity and patient knowledge levels about treatment options [23]. Further research would be needed to determine the best approach to education and decision-making; all inclusive or multiple separate tools for Australia.
Worries, flexibility and control
It was anticipated that comprehensive education and supported decision-making, a desired position for consent and SDM, would reduce worries. However, the opposite was found and this correlated with factors that suggest more comprehensive and effective education. One theoretical explanation could be the reality of understanding the burden of treatment without there being adequate experience yet or support to manage these concerns because dialysis had not yet started. Indeed, PtDA have been found to improve realistic expectations of treatment [24]. Further qualitative surveys may better explain this phenomenon for the MKDA. It has been identified that research should also determine whether genuine understanding improves adaptability to treatment at a later stage [25].
Participants remained consistent in the level of control they desired, possibly reflecting their natural personality. The relatively low desire for control by staff was reflected in the treatment choices where CBD was the first choice for only 11% of patients. Both this and the extreme level of desire for flexibility are important messages for renal services where CBD traditionally offers limited control and low rates of flexibility.
Decision-making support
The MKDA was accepted positively by patients for supporting decision-making, a surrogate measure for reduced decisional conflict. The validated Decisional Conflict Scale (16-item scale with 5 sub-scales) defines decisional conflict as ‘uncertainty about the course of action to take when choice among options involves risk, loss, regret or challenge to personal life values’ [26]. Decisional conflict is an important aspect of decision-making that has been demonstrated in the Cochrane review to be reduced by the use of a ptDA [6].
Reducing decisional conflict is important in practice because patients who have lower decisional conflict are also reported to be more satisfied with the consultation [24, 27]. Unfortunately, while studies have determined that patients may also prefer SDM when choosing treatment options, there is a significant gap between their desired role and their actual role in decisions [12, 28]. Current theory and our findings therefore support the use of a ptDA to enhance SDM and reduce decisional conflict.
Treatment choices
A home dialysis option was selected by 62% of respondents as their preferred treatment choice. This was 79% of those whose first treatment option was to have some type of dialysis. This finding of preference for home is supported by many studies who also found that, during decision-making, home treatments are preferred, particularly if control is important [21, 29, 30].
For patients without clinical constraints, there are no clear criteria that should prevent them choosing and utilizing the treatment to suit their lifestyle [31]. Despite the high preference for home modalities and only 11% preferably selecting CBD, 37% of RRT patients are actually on CBD, not accounting for CC. As determined in a study that found that only 59 of 124 patients who selected PD started on PD, a better understanding of this mismatch regarding choice and actual therapy is needed [32]. Additionally assisted home dialysis is a model that 39% of patients completing the Australian dialysis consumer survey favoured [16], but one that is only available in pilot models in Australia. Ensuring timely surgery and mitigating geographical and support factors that reduce access to home training may be some keys to ensuring patients achieve their preferred choices.
Limitations
Resources limited the capacity to engage a control group to determine whether knowledge levels, worries or treatment choices were actually impacted upon by the MKDA compared with usual education practice. Randomized use with comparative assessment of these factors is recommended for future research. Decisional conflict was not measured by a validated scale but is targeted as future research.
The participants were from limited sites and dominated by the NSW cohort. However, the results related to every aspect of usability of the MKDA, worries and pre-knowledge levels were comparative between the states indicating that the MKDA should be suitable for most jurisdictions. The greatest state differences that were found related to how education delivery varied and possibly related to this post-knowledge levels showed variance. The states who showed lower knowledge levels still displayed equity of knowledge between treatment options, but this did suggest that the role of the MKDA is as an adjunct to education and not a replacement. A larger or wider sample size would be needed to confirm this.
Those who did not have English as a first language or rural/remote indigenous populations were not tested. Therefore, validation and ongoing research are strongly recommended, particularly for minority groups. A validated decisional conflict was not used as a measure in this study but would be a useful tool to validate the MKDA in future practice.
Conclusion
In this preliminary survey, acceptance and usability rating of the My Kidneys, My Choice decision aid was high with little variance across demographics. It was rated as highly effective in supporting decision-making. MKDA use was also associated with equitable increased knowledge levels across all treatment options. Home dialysis options were the preferred choice for 62% of participants. In this cohort, the levels of worry about the future, lifestyle and ability to continue a current daily lifestyle were increased in those who received broader education which contradicts current belief that worry is decreased by being well-informed but indicates high understanding of treatment options and future lifestyle.
Transparency declarations
D.F. and T.S. have received an honorarium from Baxter Healthcare.
Conflicts of interest statement
The results published in this manuscript have not been published previously in whole or in part except in abstract.
Acknowledgements
The authors acknowledge the multidisciplinary team who developed the decision aid and the staff who supported the research. Baxter Healthcare provided an unrestricted educational grant to a steering committee to support the meetings and the specialist psychologist team associated with the development of the decision aid. Kidney Health Australia receives funds for the ‘ESKD education project’ via the Commonwealth Chronic Disease Prevention and Improvement Flexible Fund. This funding supports distribution, education and assessment of the decision aid.
References
- 1.McDonald S, Clayton P, Hurst K. Thirty Fifth Annual Report of the Australian and New Zealand Dialysis and Transplant Registry. 2012. www.anzdata.org.au/v1/report_2012.html (23 November 2014, date last accessed)
- 2.Key S. Optimizing dialysis modality choices around the world: a review of literature concerning the role of enhanced early pre-ESRD education in choice of renal replacement therapy modality. Nephrol Nurs J 2008; 35: 387–394 [PubMed] [Google Scholar]
- 3.National Institute for Health and Care Excellence. NICE guidelines, Planning, Initiating and Withdrawing of RRT. 2013. www.renal.org/Clinical/GuidelinesSection/RenalReplacementTherapy.aspx (22 March 2015, date last accessed)
- 4.Wheeler D, Becker G. Summary of KDIGO guideline. What do we really know about management of blood pressure in patients with chronic kidney disease? Kidney Int 2013; 83: 377–383 [DOI] [PubMed] [Google Scholar]
- 5.Barry M, Edgman-Levitan S. Shared decision making—pinnacle of patient centred care. N Engl J Med 2012; 366: 780–781 [DOI] [PubMed] [Google Scholar]
- 6.Stacey D, Legare F, Col N, et al. Decision aids for people facing health treatment or screening decisions, 2014. www.thecochranelibrary.com (22 March 2015, date last accessed) [DOI] [PubMed]
- 7.Murray M, Brunier G, Chung J, et al. A systematic review of factors influencing decision-making in adults living with chronic kidney disease. Pat Educ Counsel 2009; 76: 149–158 [DOI] [PubMed] [Google Scholar]
- 8.Healthwise. Kidney failure—what type of dialysis should I have? Ottawa Hospital Research Institute, 2013. www.healthwise.net/cochranedecisionaid (23 November 2014, date last accessed) [Google Scholar]
- 9.Bekker H, Wilkie M, Mooney A, et al. Development of a patient decision aid (PtDA), in paper and web formats, to improve renal patients’ informed decisions about dialysis modality. Leeds University; 2012. http://www.leeds.ac.uk/hsphr/research/AUPBS/ptda.html (12 March 2014, date last accessed) [Google Scholar]
- 10.Home Dialysis Central. Method to Assess Treatment Choices for Home Dialysis (MATCH-D). 2013. [updated March 15]; http://homedialysis.org/match-d (22 March 2015, date last accessed)
- 11.Ameling J, Auguste P, Ephraim P, et al. Development of a decision aid to inform patients and families renal replacement therapy selection decisions. BMC Med Inform Dec Mak 2012; 12: 140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fiset V, O'Connor A, Evans W, et al. Development and evaluation of a decision aid for patients with stage IV non-small cell lung cancer. Health Expect 2000; 3: 125–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Auvinen A, Hakama M, Ala-Opas M, et al. A randomized trial of choice of treatment in prostate cancer: the effect of intervention on the treatment chosen. BJU Intern 2004; 93: 52–56 [DOI] [PubMed] [Google Scholar]
- 14.Winterbottom A, Bekker H, Conner M, et al. Choosing dialysis modality: decision making in a chronic disease context. Health Expect 2012; 17: 710–723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fortnum D, Morton RL, Ludlow M. Renal unit characteristics and patient education practices that predict a high prevalence of home-based dialysis in Australia. Nephrol 2014; 19: 587–593 [DOI] [PubMed] [Google Scholar]
- 16.Ludlow M, Lauder L, Mathew T, et al. Australian consumer perspectives on dialysis: first national census. Nephrology 2012; 17: 703–709 [DOI] [PubMed] [Google Scholar]
- 17.Elwyn G, O'Connor AM, Bennett C, et al. Assessing the quality of decision support technologies using the international patient decision aid standards instrument (IPDASi). PLoS ONE 2009; 4: e4705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kidney Health Australia. My Kidneys My Choice Decision Aid for End-stage Kidney Disease, Kidney Health Australia, 2013. http://homedialysisorgau/health-professional/publications/ (22 March 2015, date last accessed) [Google Scholar]
- 19.Fortnum D, Smolonogov T, Walker R. My Kidneys My Choice Decision Aid: supporting shared decision making. J Ren Care 2015; 41: 81–87 [DOI] [PubMed] [Google Scholar]
- 20.Sepucha K, Thomson R, Borkhoff C, et al. Update of the International Patient Decision Aids Standards (IPDAS) Collaboration Background Document. 2012. Chapter L. 2012 http://ipdas.ohri.ca/IPDAS-Chapter-L.pdf (22 March 2015, date last accessed)
- 21.Fadem S, Walker D, Abbott G, et al. Satisfaction with renal replacement therapy and education: the American Association of Kidney Patients Survey. Clin J Am Soc Nephrol 2011; 6: 605–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chiou C, Chung Y. Effectiveness of multimedia interactive patient education on knowledge, uncertainty and decision-making in patients with end-stage renal disease. J Clin Nurs 2012; 21: 1223–1231 [DOI] [PubMed] [Google Scholar]
- 23.Winterbottom A, Gavaruzzi T, Mooney A, et al. Patient acceptability of the Yorkshire Dialysis Decision Aid (YODDA) with or without value clarification: a controlled before and after study in usual predialysis care. 2013.
- 24.Vandemheen K, O'Connor A, Bell S, et al. Randomized trial of a decision aid for patients with cystic fibrosis considering lung transplantation. Am J Resp Crit Care Med 2009; 180: 761–768 [DOI] [PubMed] [Google Scholar]
- 25.Jones R, Steeves R, Ropka M, et al. Capturing treatment decision making among patients with solid tumors and their caregivers. Oncol Nurs Forum 2013; 40: E24–E31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Connor A. User Manual—Decisional Conflict Scale. © 1993 (updated 2010) 2010. www.ohri.ca/decisionaid. (23 November 2014, date last accessed)
- 27.Leighl N, Shepherd H, Butow P, et al. Supporting treatment decision making in advanced cancer: a randomized trial of a decision aid for patients with advanced colorectal cancer considering chemotherapy. J Clin Oncol 2011; 29: 2077. [DOI] [PubMed] [Google Scholar]
- 28.Sepucha K, Ozanne E, Partridge A, et al. Is there a role for decision aids in advanced breast cancer? Med Decis Making 2009; 29: 475–482 [DOI] [PubMed] [Google Scholar]
- 29.Morton RL, Tong A, Howard K, et al. The views of patients and carers in treatment decision making for chronic kidney disease systematic review and thematic synthesis of qualitative studies. Br Med J 2010; 340: 340–350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wyld M, Morton R, Hayen A, et al. A systematic review and meta-analysis of utility based quality of life in chronic kidney disease treatments. PLOS Med 2012; 9: e1001307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee A, Gudex C, Povlsen J, et al. Patients’ views regarding choice of dialysis modality. Nephrol Dial Transplant 2008; 23: 3953–3959 [DOI] [PubMed] [Google Scholar]
- 32.Liebman S, Bushinsky D, Dolan J, et al. Differences between dialysis modality selection and initiation. Am J Kidney Dis 2012; 63: 390–395 [DOI] [PMC free article] [PubMed] [Google Scholar]