Summary
Background
Hepatic portal venous gas (HPVG) is an ominous radiological sign suggestive of underlying intestinal sepsis, infection or trauma. Portal pneumatosis secondary to gastric pathologies is rare.
Case Report
We report a rare case of a 34-year-old man who presented with acute epigastric pain and vomiting, diagnosed to have an incarcerated diaphragmatic hernia causing gastric pneumatosis and resultant portal venous gas.
Conclusions
Our case highlights an unusual presentation of gastric pneumatosis secondary to an incarcerated hiatal hernia with resultant portal venous gas involving only the left lobe of the liver. An aberrant left gastric vein was responsible for this phenomenon in our case. A sound understanding of anatomical variants is thus crucial to radiological diagnosis.
MeSH Keywords: Hernia, Diaphragmatic; Imaging, Three-Dimensional; Portal Vein
Background
Hepatic portal venous gas (HPVG) is a sinister radiological sign suggestive of a serious underlying abdominal pathology. Although first described in infants with necrotizing enterocolitis (NEC), it signifies bowel ischemia and can be associated with a number of other conditions like infective, inflammatory or malignant intestinal pathologies, intra-abdominal abscesses, diverticulitis, appendicitis, superior mesenteric artery syndrome, and a condition following liver transplantation or gastrointestinal investigations and interventions [1]. HPVG due to gastric causes is rare (around 3%) [2] and is secondary to either gastric dilatation or gastric pneumatosis [1]. We report an unusual case of an incarcerated diaphragmatic hernia causing extensive gastric pneumatosis and resultant gas embolization of the portal vein. Radiological imaging was unexpected in our case as the gas was located only in the left lobe of the liver. Intraoperatively, the patient was found to have an aberrant left gastric vein (coronary vein) draining into the intrahepatic branch of the left portal vein instead of the main portal trunk, explaining the cause for the gas being confined to the left portal venous system.
Case Report
A 74-year-old male presented with a one-day history of acute-onset, sharp shooting, and constant pain located in the anterior chest wall and epigastric region associated with severe retching and vomiting. On examination the patient was febrile (38°C) and appeared to be in respiratory distress with a respiratory rate of 27/min and a heart rate of 96/min. On examination, severe tenderness was elicited in the epigastric region. His total leucocyte count was raised to 16,500/mm3 with a predominance of polymorphonuclear cells (84%). Liver function tests were normal. A screening abdominal ultrasound revealed poorly defined, highly echogenic particles in the hepatic parenchyma. However, to our surprise, those echogenic foci were confined only to the left lobe of the liver with sparing of the right lobe (Figure 1). A non-enhanced computed tomography of the chest and abdomen showed a grossly distended stomach with intrathoracic extension of the stomach in the posterior mediastinum located behind the heart and anterior to the spine and aorta suggestive of a diaphragmatic hernia, with intramural gas in the stomach wall indicative of incarceration and resultant gastric pneumatosis (Figure 2). Isolated left hepatoportal gas was confirmed by the presence of low-attenuation hypodensities extending from the porta to within 2 cm of the liver peripheral margin but located only in the left lobe of the liver (Figure 3). The nasogastric aspirate revealed coffee ground material and an emergency upper gastrointestinal endoscopy showed excessive oedema, erosions and sloughing of the gastric mucosa. An emergency open surgical repair was planned for the patient and the dissection demonstrated an aberrant left gastric vein which directly joined the left branch of the portal vein instead of draining into the main portal trunk. The patient being elderly, could not survive due to electrolyte imbalance. This case highlights an extremely unusual radiological sign of isolated left hepatic portal venous gas due to an aberrant left gastric vein secondary to an incarcerated hernia and gastric pneumatosis. Incarcerated hiatal hernia gave rise to gastric pneumatosis (intramural air) which drained through the left aberrant gastric vein. This aberrant vein draining the lower part of the oesophagus and the upper part of the stomach joins the left portal vein rather than the main portal vein giving rise to isolated left hepatic portal venous gas (Figures 4, 5).
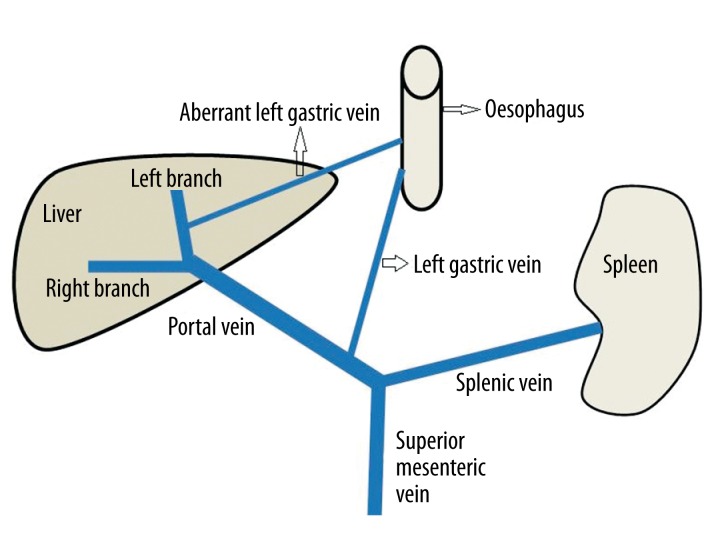
Figure 1.
Ultrasonography of the liver, subcostal view, showing the gall bladder (white arrowhead), the plane dividing the liver into the right and left lobe. Note the poorly defined, highly echogenic foci (black arrowheads) confined only to the left lobe of the liver with sparing of the right lobe, suggestive of isolated left hepatic portal venous gas.
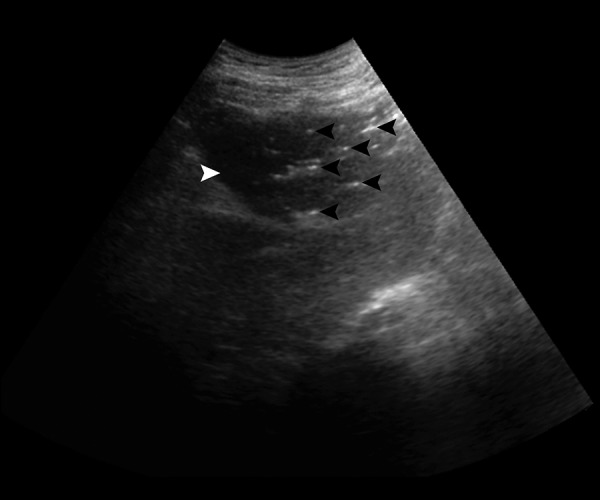
Figure 2.

Axial CT scan of the chest shows the location of the stomach in the posterior mediastinum, behind the heart, anterior to the spine and aorta with accompanying abdominal fat suggestive of diaphragmatic hernia. Note the presence of air specks within the gastric wall (white arrowheads) indicative of gastric pneumatosis.
Figure 3.
Axial CT scan of the upper abdomen confirms the presence of isolated left hepatic portal venous gas (white arrowheads). Sparing of the right lobe is seen (single white broad arrow). Note the associated gastric pneumatosis depicted in the upper abdominal sections (multiple white thin arrows).
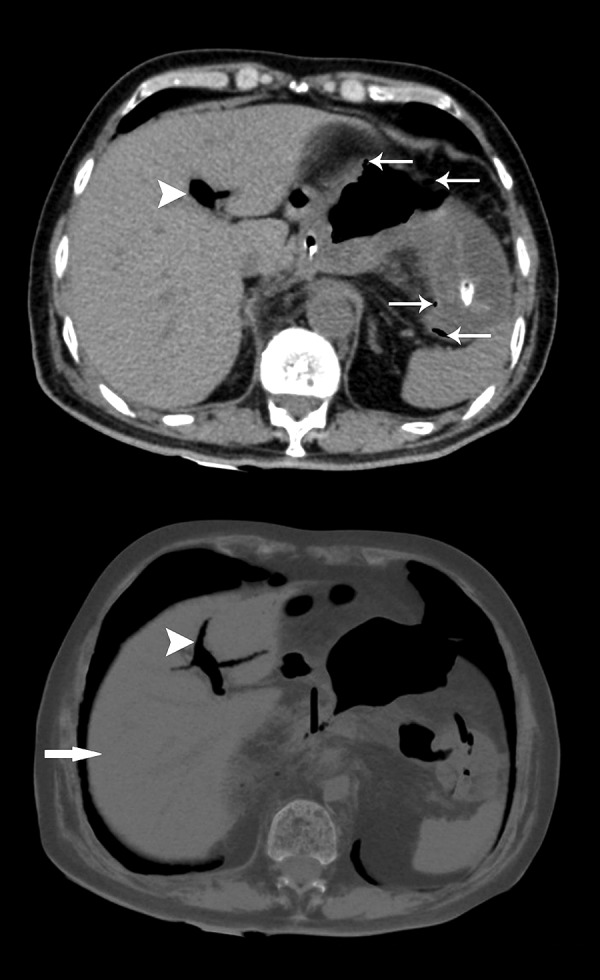
Figure 4.
Image showing normal porto-venous drainage of the left gastric vein at the confluence of the superior mesenteric vein and the splenic vein. Note the aberrant left gastric vein draining into the left portal vein.
Figure 5.
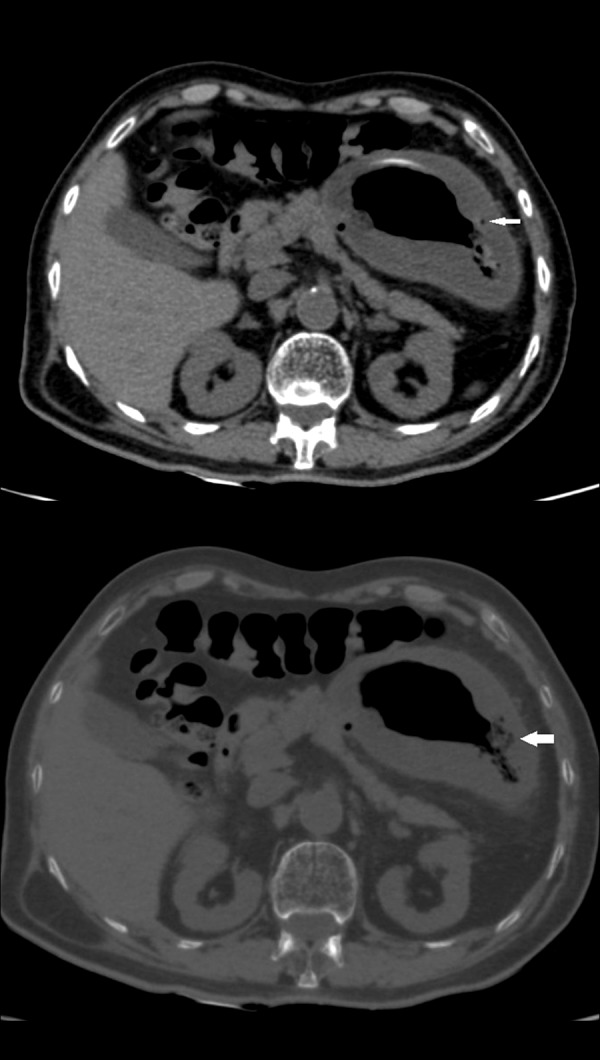
Axial CT scan of the upper abdomen showing gastric pneumatosis depicted in the abdominal sections (white solid arrows).
Discussion
Hepatic portal venous gas (HPVG) has been described extensively in literature, generally indicative of an underlying ominous abdominal pathology. This sign was first reported in 1955 in children suffering from NEC by Wolfe and Evans, and in adults by Susman and Senturia in 1960 [1,3]. The combined use of abdominal radiography, ultrasound, colour Doppler and CT imaging has led to increased sensitivity and early detection of cases [1]. HPVG appears as branching radiolucencies extending to within 2 cm of the liver capsule on abdominal radiography [1,2]. It is vital to distinguish HPVG from pneumobilia which does not extend till the liver periphery. Gas in the biliary tree is distributed towards the centre owing to the centripetal flow of bile towards the porta hepatis, while the centrifugal flow of blood is responsible for the air lucencies to extend towards the periphery in case of HPVG [1,2]. Leibmen et al. [2] concluded that HPVG is associated with necrotic bowel (72%), ulcerative colitis (8%), intra- abdominal abscess (6%), small bowel obstruction (3%), and gastric ulcer (3%) [2]. Gastric pathologies causing portal venous gas are rare and are secondary to either gastric dilatation or gastric pneumatosis [1].
Intramural gas in the stomach wall (pneumatosis) is a rare radiological imaging sign, first described by Bourdeal in 1895 [3] and only 50 cases have been described in literature [3,4]. Infiltration of the stomach by air is unusual since it is resistant to ischemia owing to its rich vascular supply [5]. Intramural gas in the stomach wall can have two variants – emphysematous gastritis (or phlegmatous gastritis) attributed to infectious colonization by gas-producing organisms and gastric pneumatosis due to non-infectious etiology [3,4]. The latter can be ascribed to either increased intramural pressure or mucosal damage as seen in gastric outlet obstruction, malignancies, gastritis, massive gastric dilatation or aerophagia [3,4].
Incarcerated hiatal hernia as a cause of gastric pneumatosis, as in our case, is rarely documented in literature [6,7]. Gastric pneumatosis secondary to diaphragmatic hernia with resultant portal venous gas is even rarer and to the best of our knowledge only one such case has been described [1,8]. Our case was novel because the portal gas was located only in the left portal system owing to the aberrant left gastric vein.
The gastric veins generally accompany the corresponding arteries and drain into either the splenic vein or the superior mesenteric vein, ultimately draining into the portal vein, although some pass directly into the main portal vein. The short gastric veins draining the fundus and part of the greater curvature drain into the splenic vein; the left gastroepiploic vein draining the anterior and posterior surface of the stomach and the adjacent greater omentum drains into the splenic vein; the right gastroepiploic vein draining the distal body, antrum and greater omentum drains into the superior mesenteric vein; the left gastric vein after receiving the lower esopshageal veins and the right gastric vein after receiving the prepyloric vein drains into the main portal vein [9]. The drainage of the left gastric vein intrahepatically into the left branch of the portal vein instead of its conventional drainage into the main portal vein is extremely rare (<1%) [10].
Conclusions
Our case highlights an unusual presentation of gastric pneumatosis secondary to an incarcerated hiatal hernia with resultant portal venous gas involving only the left lobe of the liver. An aberrant left gastric vein was responsible for this phenomenon in our case. A sound understanding of anatomical variants is thus crucial to radiological diagnosis.
References
- 1.Abboud B, El Hachem J, Yazbeck T, Doumit C. Hepatic portal venous gas: Physiopathology, etiology, prognosis and treatment. World J Gastroenterol. 2009;15(29):3585–90. doi: 10.3748/wjg.15.3585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liebman PR, Patten MT, Manny J, et al. Hepatic-portal venous gas in adults: etiology, pathophysiology and clinical significance. Ann Surg. 1978;187(3):281–87. doi: 10.1097/00000658-197803000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sen I, Samarasam I, Chandran S, Mathew G. Gastric intramural and portal venous gas following blunt abdominal injury. Arch Trauma Res. 2013;2(2):95–96. doi: 10.5812/atr.10866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soon M-S, Yen H-H, Soon A, Lin OS. Endoscopic ultrasonographic appearance of gastric emphysema. World J Gastroenterol. 2005;11(11):1719–21. doi: 10.3748/wjg.v11.i11.1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shaha NR, Dossicka DS, Maduraa JA, Heppell JP. Use of diagnostic laparoscopy in a patient with gastric pneumatosis and portal venous gas. Case Rep Gastroenterol. 2013;7:261–65. doi: 10.1159/000351876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ilyas C, Young AL, Lewis M, et al. Parastomal hernia causing gastric emphysema. Ann R Coll Surg Engl. 2012;94(2):e72–73. doi: 10.1308/003588412X13171221588613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Medefind JN, Adams WC. Merced incarcerated hiatal hernia with gangrene of the entire stomach. California Medicine. 1963;99:200–1. [PMC free article] [PubMed] [Google Scholar]
- 8.Haswell DM, Carsky EW. Hepatic portal venous gas and gastric emphysema with survival. Am J Roentgenol. 1979;133:1183–85. doi: 10.2214/ajr.133.6.1183. [DOI] [PubMed] [Google Scholar]
- 9.Borley NR. Gastrointestinal tract-Stomach and abdominal oesophagus. In: Healy JC, editor. Gray’s Anatomy, The Anatomical Basis of Clinical Practice. Thirty ninth edition. Chapter 71. Section 7. pp. 1149–50. [Google Scholar]
- 10.Sugimoto H, Takeda S, Inoue S, et al. Hepatobiliary and pancreatic: Aberrant left gastric vein. J Gastroenterol Hepatol. 2005;20:155. doi: 10.1111/j.1440-1746.2004.03755.x. [DOI] [PubMed] [Google Scholar]