Abstract
Genital molluscum contagiosum is rare in children. We report a molluscum contagiosum around the vulva and anus of 9-year-old girl, which has atypical presentations and was finally confirmed by histopathological and electron microscopy findings.
Keywords: Child; Dermoscopy; Microscopy, electron, transmission; Molluscum contagiosum; Pathology
INTRODUCTION
Molluscum contagiosum (MC) is a highly contagious skin infection caused by molluscum contangiosum virus (MCV), a double-stranded DNA poxvirus. It primarily affects school-age children and occasionally adults and immunocompromised individuals. 1 MC usually presents on the face, trunk and extremities but rarely in the genital region. We report an infection by molluscum contagiosum around the vulva and anus of 9-year-old girl.
CASE REPORT
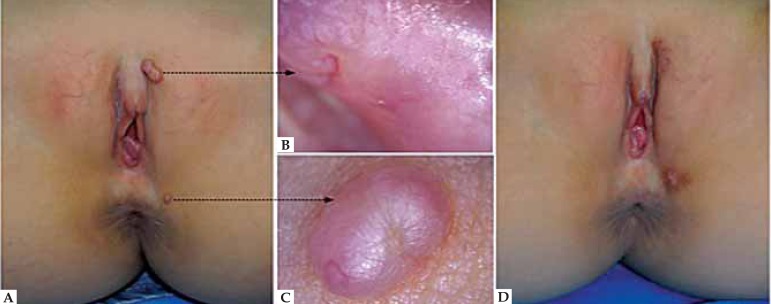
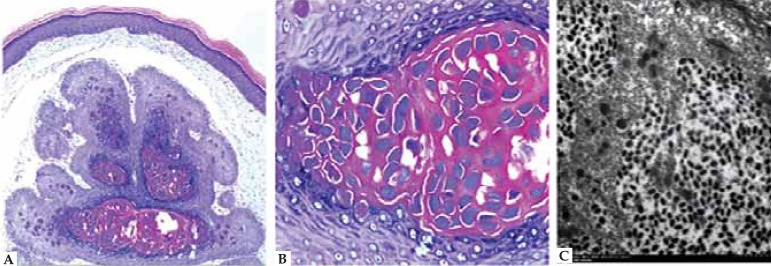
A 9-year-old girl had asymptomatic lesions with a pink raised nodule and a papule around the vulva and anus for 2 months (Figure 1A). Physical examination revealed a firm, tender, 0.5 X 1.1 cm nodule on the left of the vulva and a pink 0.4 X 0.3 cm papule around the anus. The dermoscopy using JD801G (Jiangsu JEDA Science and Technology Development Co., Ltd, China) showed smooth, reddish and piny surfaces of the lesions and a depression in the margin of the pink papule, on which a crown vessel was observed (Figure 1B and 1C). No similar lesions were found anywhere else on her body. A detailed inquiry revealed no evidence of child abuse and her family informed she often went swimming in a public pool. An excisional biopsy was performed on both lesions. Histopathologic findings revealed a bulk of eosinophilic and basophilic molluscum bodies surrounded by numerous keratinocytes (Figures 2A and B). The transmission electron microscope showed numerous mature viral particles (Figure 2C). Based on the histopathological and electron microscopy findings, the diagnosis of molluscum contagiosum was confirmed. There was no recurrence after a month of follow-up (Figure 1D).
FIGURE 1.
A. A 9-year-old girl developed a pink raised nodule of 0.5 X 1.1cm in diameter and a reddish 0.4 X 0.3cm papule around the vulva and anus respectively. B. Dermoscopic view of the nodule showed its smooth, reddish and piny surface with small shallow depressions. C. Under dermoscopy, a depression in the margin of the pink papule, on which a crown vessel was apparent. D. The lesions were completely removed by an excisional biopsy
FIGURE 2.
A. A bulk of characteristic molluscum bodies surrounded by numerous keratinocytes (Hematoxylin-Eosin X100). B. High magnifi cation of molluscum bodies reveals eosinophilic and basophilic cytoplasmic material (Hematoxylin-Eosin X400). C. The electron microscopic examination shows many mature viral particles, some of which have a core surrounded by an electron-transparent halo
DISCUSSION
MC is a common, benign virus infection of the skin, primarily affecting children, occasionally adults and immunocompromised individuals. Clinically, MC is easily diagnosed for its characterized manifestations of umbilicated papules. However, on rare occasions, atypical presentation in location, size and number increases the difficulty in making a diagnosis. Thus a biopsy and electron microscopic analysis of biopsy specimens could facilitate a definitive diagnosis. 2 In our case, the lesions around the vulva and anus, which showed smooth surfaces and no polylodular amorphous structure in the dermoscopy, were finally proved by the histopathologic and electron microscopic findings to be molluscum contagiosum.
In children, MC is frequently involved on the face, trunk and extremities but rarely occurs in the genital region, where molluscum contagiosum lesions are more likely to develop in adults as a sexually transmitted disease.3 Therefore, in genital MC of children, child abuse should be considered although autoinoculation of the poxvirus is a potential mode of transmission.1 Additionally, the molluscum lesions usually appear as umbilicated papules or nodules of 1-10 mm in diameter, rarely more than 1 cm. The giant one in uncommon regions, such as sole, scalp or eyelid, can easily cause clinical confusion with verruca vulgaris, keratoacanthoma and various adenomas.2
Although many potential modes of MCV transmission have been proposed, the exact mode of transmission is still unclear. Physical contact, formites and autoinoculation are considered as the main causes for the spread of MCV while swimming pool use has a widely accepted correlation with MC. Weismann et al described that seats around the pool or sitting on the pool edge were possible modes of infection.4 In our case, this girl often went swimming in a public swimming pool, which may be assumed as a predisposing factor in the occurrence of the molluscum lesion.
Acknowledgements
We thank Dr. Song Lei, Department of Pathology, West China Hospital, Sichuan University, for TEM technique support.
Footnotes
Financial Support: None.
Conflict of Interest: None.
How to cite this article: Zhuang KW, Ran Y, Xu F, Lama J. Atypical infantile genital Molluscum contagiosum. An Bras Dermatol. 2015; 90(3):403-5.
Work performed at the West China Hospital, Sichuan University – Sichuan, China.
Reference
- 1.Brown J, Janniger CK, Schwartz RA, Silverberg NB. Childhood molluscum contagiosum. Int J Dermatol. 2006;45:93–99. doi: 10.1111/j.1365-4632.2006.02737.x. [DOI] [PubMed] [Google Scholar]
- 2.Ha SJ, Park YM, Cho SH, Cho BK, Song KY. Solitary giant molluscum contagiosum of the sole. Pediatr Dermatol. 1998;15:222–224. doi: 10.1046/j.1525-1470.1998.1998015222.x. [DOI] [PubMed] [Google Scholar]
- 3.Fischer G, Rogers M. Vulvar disease in children: a clinical audit of 130 cases. Pediatr Dermatol. 2000;17:1–6. doi: 10.1046/j.1525-1470.2000.01701.x. [DOI] [PubMed] [Google Scholar]
- 4.Braue A, Ross G, Varigos G, Kelly H. Epidemiology and impact of childhood molluscum contagiosum: a case series and critical review of the literature. Pediatr Dermatol. 2005;22:287–294. doi: 10.1111/j.1525-1470.2005.22401.x. [DOI] [PubMed] [Google Scholar]