Abstract
BACKGROUND:
Lichen planus is considered to be the most common dermatological disease involving the oral mucosa.
OBJECTIVE:
To investigate the profile, clinical features, and the presence of dysplasia and candidiasis in patients with oral lichen planus.
METHODS:
A total of 21 patients were selected from 258 patients at risk for oral cancer development.
RESULTS:
Most of the patients were white (76,2%), female (66,6%), with mean age of 58.8 years. Eight were smokers and seven were alcohol consumers. The buccal mucosa was the most affected site, followed by the tongue and the gingiva. The reticular pattern was the most common appearance. Histopathology depicted dysplasia in nine cases and cytopathology was positive for Candida in eight cases in the first appointment.
CONCLUSION:
Our data are similar to the literature. Cytopathology was important for the diagnosis of candidiasis. Although the presence of dysplasia was verified, further studies are necessary to clarify the importance of this finding.
Keywords: Candidiasis; chronic mucocutaneous; Epidemiology; Lichen planus, oral
INTRODUCTION
Lichen planus is a mucocutaneous disease characterized by nonspecific inflammation. It leads to the severe destruction of the epithelial basal layer.1 The prevalence of oral lichen planus (OLP) ranges from 0.5% to 2.2% of the population and it is considered the most common skin disease involving the oral mucosa. 1-3 The typical age of onset ranges from 30-60 years, and it is more common in women.2,3
OLP usually presents bilaterally on the oral mucosa and has various patterns, with reticular, erythematous (erosive), plaque and ulcerative being the most common. These patterns may coexist in the same region or may alternate in time.2
The most commonly affected sites are the buccal mucosa, the tongue and the gingiva. Involvement of the palate and lips is rare, and even rarer is the involvement of the oral floor. Burning symptoms, itching and pain are particularly seen in the ulcerative and erythematous variants.2
The diagnosis should be based on clinical and histopathological examination. In classical lesions, only clinical diagnosis is possible. 3 In the absence of typical manifestations of the reticular pattern, other patterns may be difficult to diagnose. In these cases, a biopsy is indicated.2
It is clear that OLP is an incurable disease. However, the disease has periods of exacerbation and remission. 2,3 During exacerbation, both the erythematous/ulcerated areas and the pain increase. These periods may be related to stress, anxiety or mechanical trauma .3 Several protocols for monitoring the disease have been described. They are usually based on the clinical aspect, the number of areas involved and the severity of symptoms.2
Several studies report the malignant potential of OLP. However, this topic is still quite controversial. The frequency of malignant transformation varies between 0 and 3.5%, and erythematous and erosive lesions show the highest index. 4 The association between smoking and OLP is still not clear, nor is the relevance of infection by Candida sp in OLP lesions.
The aim of this study is to investigate the clinical features and the presence of dysplasia and candidiasis in OLP lesions, as well as the profile of patients seen at the Ambulatório de Diagnóstico Oral of the Antônio Pedro University Hospital / UFF.
MATERIALS AND METHODS
This is a retrospective study conducted between 2005-2011 with 258 patients considered at risk for developing oral cancer. The mean follow-up interval for each patient was around 4 months. Of the total number of patients, 21 were diagnosed with OLP and were included in the final sample. All the data from each patient were registered in their respective medical records. These contained information on the clinical history and physical examination, which were necessary to characterize the profile of the patients. Details were described with emphasis on the lesions, using images captured during the intra-oral examination.
The clinical and histopathological diagnostic criteria for OLP were based on the studies by Van der Waal and Van der Meij.5 These studies report that the concomitant presence of clinical features (presence of: bilaterally symmetrical lesions; reticular lesions; and plaque, erosive, atrophic and bullous lesions are always associated with the reticulated pattern) and histopathological features (presence of predominantly lymphocytic infiltrate in band-like pattern, confined to the superior part of the connective tissue; hydropic degeneration of the basal layer; absence of epithelial dysplasia) would characterize a lichen planus lesion. Nevertheless, the absence of a clinical and/or histopathological feature would characterize a lichenoid lesion. In this study we also considered epithelial dysplasia according to Bánóczy & Csiba's criteria.6
The patients were initially examined by visual inspection, and all their lesions were photographed (digital camera Sony DSC-H1, China). Patients were subsequently examined with the aid of an intraoral video camera ("videoroscopy", intraoral camera IntraCam - V4 Active Ware Projects & Products®, Sao Paulo, Sao Paulo, Brazil) with magnification up to 28x. Each site of the oral mucosa clinically affected by the OLP and the different types of patterns were registered in the patient's medical record.
Cytological examination was performed in all lesions with the aid of an endocervical brush. We obtained three smears from each lesion. These were stained by Papanicolaou's (PAP) method and with periodic acid-Schiff (PAS). For the slides stained by Papanicolaou's method, the analysis of the cellular changes associated with candidiasis was performed according to the following criteria (Bibbo & WILBUR, 2008): presence of grouped and overlapping keratinized cells associated with polymorphonuclear leukocytes (PMN) and cellular alteration of inflammatory nature - presence of a perinuclear halo, as well as Candida spp hyphae and/or pseudohyphae (more easily identified in PAS-stained slides).
Histopathology was used for the definitive diagnosis of OLP and considered as the gold standard. All samples were fixed in 10% formalin and stained with hematoxylin and eosin, and PAS.
RESULTS
Fourteen patients (66.66%) were female. The mean age was 58.8 years for women and 55.8 for men. Most subjects were white (n=16; 76.2%). Seven (30%) participants were smokers and eight (38.1%) were alcohol consumers. Significantly more women than men reported never having smoked (47.6% and 19%) or consumed alcohol (42.8% and 19%).
Most subjects had multiple oral lesions. The buccal mucosa was the most commonly affected site (n=17; 81%), followed by the tongue and the gingiva (n= 7; 33.4% each). (Table 1)
TABLE 1.
Profile of patients with oral lichen planus: histopathology, cytopathology, presence of candidiasis and affected sites
| Patient | Gender | Smoker | Alcohol consumer | Dysplasia cytopathology | Biopsy | Dysplasia histopathology | Candidiasis | Affected sites | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Mild | Moderate | Severe | 1st appointment | Follow-up | Buccal mucosa | Tongue | Lip mucosa | Gingiva | Oral floor | Vestibular sac | Palate | Lip vermilion | |||||||
| 1 | F | X | X | X | X | R | ||||||||||||||||
| 2 | F | X | R | R | ||||||||||||||||||
| 3 | F | X | X | X | R | |||||||||||||||||
| 4 | F | X | X | X | X | X | X | R | ||||||||||||||
| 5 | F | X | X | P | ||||||||||||||||||
| 6 | F | X | X | X | R/P | |||||||||||||||||
| 7 | F | X | X | X | X | R | R | R | R | R | ||||||||||||
| 8 | M | X | X | X | X | X | R/E | |||||||||||||||
| 9 | F | X | X | X | R | |||||||||||||||||
| 10 | F | X | X | X | X | X | R | R | R | R/E/P | R/E/P | |||||||||||
| 11 | F | X | X | R | R | R | R | |||||||||||||||
| 12 | F | X | X | X | R | R/P | R | R | ||||||||||||||
| 13 | F | X | X | R | ||||||||||||||||||
| 14 | F | X | X | X | X | X | R | R | R | |||||||||||||
| 15 | M | X | X | X | X | X | R | R | ||||||||||||||
| 16 | M | X | R | R/P | ||||||||||||||||||
| 17 | M | X | X | X | X | R | R | R | ||||||||||||||
| 18 | M | X | X | X | X | X | R | R | R | R/E | R | R/E | ||||||||||
| 19 | M | X | X | X | R | R/P | R | R | ||||||||||||||
| 20 | M | X | X | X | R/E | R/P | ||||||||||||||||
| 21 | F | X | X | X | X | E | ||||||||||||||||
R: reticular; E: erosive; P: plaque
The reticular pattern alone was observed in eleven patients. The rest of patients showed reticular pattern associated with other patterns. The plaque pattern and the erosive pattern were the second (seven patients) and the third most commonly found patterns, respectively. In three patients, the latter was associated with other patterns. (Table 1)
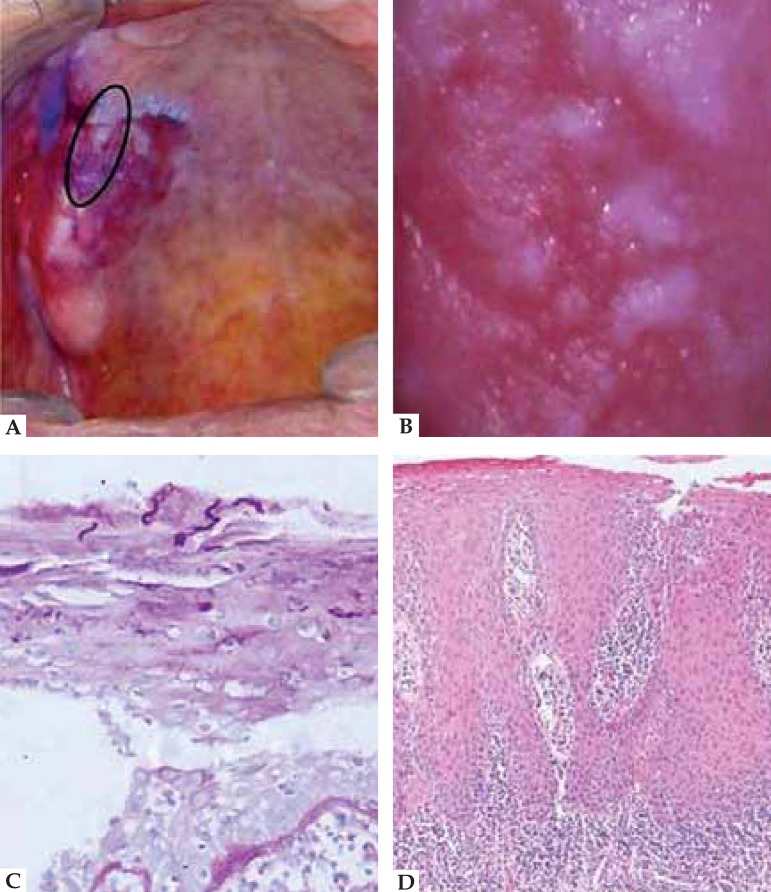
All patients had lesions clinically compatible with OLP. Eighteen patients underwent biopsy. Three patients refused to undergo biopsy. In all cases where a biopsy was performed diagnostic histopathological features of OLP were found. Nine cases showed epithelial dysplasia: eight cases had mild epithelial dysplasia and one case had moderate epithelial dysplasia. (Figure 1)
FIGURE 1.
A. Clinical case of OLP associated with candidiasis. Presence of a 2.0x2.0cm red area with white plaques, irregular contour and indefinite boundaries, located in the upper alveolar ridge and right hard palate; B. Clinical case of OLP associated with candidiasis. Image of the lesion captured by a intraoral camera at 28x magnification; C. Clinical case of OLP associated with candidiasis. PAS staining. Presence of Candida spp. hyphae; D. Clinical case of OLP associated with candidiasis. HE staining at 100x magnification: presence of severe exocytosis, degeneration of the basal layer, dysplastic changes such as irregular epithelial stratification, mitosis, mild hyperchromatism. These changes affected the basal and parabasal layers, and were consistent with moderate dysplasia and intense mononuclear infl ammatory infiltrate.
Cytopathological examination revealed an association with candidiasis in eight of the 21 cases in the first appointment and in 12 of the 19 patients who were being followed up. Cytopathology also revealed mild epithelial dysplasia in 10 patients (47.6%). One (4.76%) patient had moderate epithelial dysplasia. No severe epithelial dysplasia was observed in the cytopathological or histopathological examinations.
DISCUSSION
We found a predominance of OLP among female patients. This finding is in line with the literature, which reports a ratio of 2: 1.2,3,7-9
Most cases of OLP occur between the fourth and sixth decades of life. 1,2,7 One study has reported that most cases occurred in the seventh decade of life. 7 However, in this study we only found three cases older than this age group.
The clinical presentation of OLP can be variable and may initially go unnoticed. We found that the bilateral buccal mucosa was the most commonly affected site, followed by the tongue and the gingiva. This finding is in agreement with the literature.1,2,7,10 According to the literature, the reticular pattern is the most frequent pattern, followed by the erosive pattern. However, in this study we found that the reticular pattern was the most common pattern, followed by the plaque pattern. 2,7,11 The tongue and the gingiva are common sites of involvement of plaque-like OLP, which perhaps explains the occurrence of this pattern as being the second most commonly found in this study.12,13 Although many patients are asymptomatic and do not require therapy, some patients - especially those with erosive and atrophic lesions - pose a challenge to treatment. Systemic corticosteroids should be reserved for acute exacerbations and disseminated lesions, reducing inflammation and pain. During treatment of OLP the manifestation of candidiasis is a common consequence of the use of topical corticosteroids. 14 Chainani-Wu et al. reported that candidiasis was infrequent and associated with topical corticosteroids. 15 Inflammation and infection by Candida spp. may cause changes in the epithelium that may be interpreted as dysplasia. In our study, cytopathology revealed fungal infection in eight cases in the first appointment and in twelve cases during follow-up.
In general, Candida spp. may be found as a commensal organism in the oral cavity of the population. 16 The determinant of the type of relationship that will exist between Candida spp. and its host is the way it interacts with the colonized epithelial surface. There is clearly a delicate balance between the effects of the potentially harmful virulence factors produced by Candida spp. and the nature of the host's immune response. An imbalance in this mechanism causes the relationship between fungus and host to change from commensal to pathogenic.17 The Candida spp. colonizes the mouth in the form of yeasts. However, when the epithelium undergoes some kind of change with trauma, hormonal factors, immunosuppression, etc., the fungus may invade the underlying connective tissue. It then takes the form of hyphae and produces hydrolytic enzymes that are identified by the body as pathogenic factors, which triggers an immune response.16,18,19 Thus for the diagnosis of candidiasis it is necessary to identify the hyphae and/or pseudohyphae which are associated with the inflammatory criteria.20.21
Spolidorio et al. (2003) studied the occurrence of Candida spp. in oral mucosa lesions and found the presence of this fungus in nine lesions from a total of 54 patients with OLP. 22 They reported that the most accepted interpretation for the presence of candidiasis in these lesions is that it is a secondary colonizer of a previously altered mucosa.
Kragelund et al. (2012) reported the presence of Candida spp. in 16 of 30 patients with OLP. Five patients showed no signs or symptoms of the presence of this fungus.23 We found the cytopathological examination to be an important part of the treatment protocol of patients with OLP, and it may aid in the diagnosis and in therapeutic decision-making. Patients with candidiasis may or may not show signs and symptoms of the disease. Candidiasis may also exacerbate the symptoms of OLP. Cytopathology is a tool for the identification or confirmation of candidiasis and its treatment may alleviate the existing symptoms. As previously mentioned, candidiasis may alter the epithelium and the inflammatory response. The performance of the cytopathological examination - prior to biopsy - may aid in the diagnosis and treatment of candidiasis, providing the pathologist with better material for analysis and diagnosis.
As for tobacco and alcohol consumption, we found no difference between the sexes, nor an association between epithelial dysplasia - diagnosed by histopathology- and these habits. Rajentheran et al. suggest that the rate of malignant transformation of OLP in smokers and alcohol consumers may be lower than in most patients with oral cancer.8 Some studies emphasize the need for these patients to avoid or discontinue smoking and alcohol consumption in order to reduce the risk of malignant transformation.3,24 González-Garcia et al. reported that there is no significant association between OLP and tobacco and alcohol consumption.9 Murti et al. found no significant risk when comparing the relative risk of transformation of OLP into cancer in a smoker.10 In their study, the authors found epithelial atrophy in 74% of the 94 biopsies performed and suggested that this atrophy would result in a greater vulnerability against carcinogens. It was not the aim of this study to evaluate the influence of alcohol and tobacco consumption on OLP. However, given the data in the literature and the possibility of malignant transformation of OLP cited by some studies, we suggest that patients with these habits are more cautiously monitored and encouraged to discontinue smoking and alcohol consumption.
The clinical and histopathological definition of OLP was made by the WHO in 1978. Histopathology has been used in its diagnosis ever since. Van Der Meiji e Van Der Waal compared clinical and histopathological criteria of OLP and concluded that there appears to be a lack of clinicopathological correlation in the diagnosis.25 Fernández-González et al. considered the clinical and histopathological criteria established by the WHO and modified by Van Der Meiji and Van Der Waal, i.e., presence of bilateral lesions; reticular lesions; all atrophic, erosive, bullous or plaque lesions associated with the reticular pattern; presence of a subepithelial inflammatory infiltrate in band-like pattern, degeneration of the basal layer, and absence of epithelial dysplasia. If all clinical and histopathological criteria were present, the lesion would be considered to be lichen planus, in case some criterium was not present, it would be regarded as being compatible with lichen planus.11,25 In this study, according to this classification, we found a definite diagnostic correlation in 48% of patients. The rest of patients was classified as having lesions compatible with lichen planus.
All patients are currently being followed up. Some studies suggest that patients with OLP have a higher risk of developing squamous cell carcinoma than the general population.8,15 In 1978, Krutchkoff et al. warned about the lack of data in the literature supporting the number of reported cases of malignant transformation of OLP.26 Van der Meiji et al., agreed with this statement and claimed that two thirds of the cases of OLP with malignant transformation were not sufficiently documented to be considered.27 These authors believe that most cases of malignant transformation are the result of a mistake in diagnosis. In fact, the diagnosis of OLP demand experience and knowledge from clinicians and pathologists.
Van der Meiji et al. concluded that lichenoid lesions carry a much higher risk of malignant transformation than OLP lesions, and that the monitoring of lichenoid lesions with atrophic/erosive/ulcerative areas is of special importance.5 MURTI et al. found 4% of epithelial dysplasia in 94 biopsies. Only three cases developed cancer from OLP and two of them were smokers.10 In this study, nine of the 18 patients who underwent biopsy were found to have mild or moderate epithelial dysplasia. Thus, we believe that OLP really is a lesion with malignant potential and that, at some point, some dysplastic change will be present.
CONCLUSIONS
The profile of the patients who constituted our study sample showed no differences from the literature data. The most frequently observed pattern was the reticular pattern. However, the second most common pattern was the plaque pattern, which may explain the finding of the tongue as the second most common site of occurrence of OLP. Candidiasis was present in a little over a third of cases in the first appointment and in more than half of cases in the follow-up visits. Cytopathology proved to be an important tool for diagnosis. Dysplasia was identified in more than half of cases. Nevertheless, a longitudinal study should be conducted in order to investigate the meaning of this finding. Lesions clinically compatible with OLP should undergo biopsy for definitive diagnosis and should be followed up for life. In case changes in the appearance of these lesions are found during follow-up, further biopsies should be carried out, because their malignant potential is not yet clear.
Footnotes
Financial Support: CNPq.
Conflict of Interest: None.
How to cite this article: Werneck JT, Costa TO, Stibich CA, Dias EP, Silva Junior A, Leite CA. Oral lichen planus: study of 21 cases. An Bras Dermatol. 2015;90(3):321-6.
Study conducted at the Oral Diagnostic Outpatient Clinic of the Hospital Universitário Antônio Pedro - Universidade Federal Fluminense (HUAP-UFF) – Niterói (RJ), Brazil.
Reference
- 1.Sousa de FACG, Paradella TC. Malignant potential of oral lichen planus: A metaanalysis. Rev Odonto Ciênc. 2009;24:194–197. [Google Scholar]
- 2.van der Waal I. Oral lichen planus and oral lichenoid lesions; a critical appraisal with emphasis on the diagnostic aspects. Med Oral Patol Oral Cir Bucal. 2009;14:E310–E314. [PubMed] [Google Scholar]
- 3.Al-Hashimi I, Schifter M, Lockhart PB, Wray D, Brennan M, Migliorati CA, et al. Oral lichen planus and oral lichenoid lesions: diagnostic and therapeutic considerations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:S25.e1-12. doi: 10.1016/j.tripleo.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Fitzpatrick SG, Hirsch SA, Gordon SC. The malignant transformation of oral lichen planus and oral lichenoid lesions: a systematic review. J Am Dent Assoc. 2014;145:45–56. doi: 10.14219/jada.2013.10. [DOI] [PubMed] [Google Scholar]
- 5.van der Meij EH, van der Waal I. Lack of clinicopathologic correlation in the diagnosis of oral lichen planus based on the presently available diagnostic criteria and suggestions for modifications. J Oral Pathol Med. 2003;32:507–512. doi: 10.1034/j.1600-0714.2003.00125.x. [DOI] [PubMed] [Google Scholar]
- 6.Bánóczy J, Csiba A. Occurrence of epithelial dysplasia in oral leukoplakia. Analysis and follow-up study of 12 cases. Oral Surg Oral Med Oral Pathol. 1976;42:766–774. doi: 10.1016/0030-4220(76)90099-2. [DOI] [PubMed] [Google Scholar]
- 7.Oliveira Alves MG, Almeida JD, Balducci I, Guimarães Cabral LA. Oral lichen planus: A retrospective study of 110 Brazilian patients. BMC Res Notes. 2010;3:157. doi: 10.1186/1756-0500-3-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rajentheran R, McLean NR, Kelly CG, Reed MF, Nolan A. Malignant transformation of oral lichen planus. Eur J Surg Oncol. 1999;25:520–523. doi: 10.1053/ejso.1999.0689. [DOI] [PubMed] [Google Scholar]
- 9.González-García A, Diniz-Freitas M, Gándara-Vila P, Blanco-Carrión A, García-García A, Gándara-Rey J. Triamcinolone acetonide mouth rinses for treatment of erosive oral lichen planus: efficacy and risk of fungal over-infection. Oral Dis. 2006;12:559–565. doi: 10.1111/j.1601-0825.2006.01238.x. [DOI] [PubMed] [Google Scholar]
- 10.Murti PR, Daftary DK, Bhonsle RB, Gupta PC, Mehta FS, Pindborg JJ. Malignant potential of oral lichen planus: observations in 722 patients from India. J Oral Pathol. 1986;15:71–77. doi: 10.1111/j.1600-0714.1986.tb00580.x. [DOI] [PubMed] [Google Scholar]
- 11.Fernández-González F, Vázquez-Álvarez R, Reboiras-López D, Gándara-Vila P, García-García A, Gándara-Rey JM. Histopathological findings in oral lichen planus and their correlation with the clinical manifestations. Med Oral Patol Oral Cir Bucal. 2011;16:e641–e646. [PubMed] [Google Scholar]
- 12.Canto AM, Müller H, Freitas RR, Santos PS. Oral lichen planus (OLP): clinical and complementary diagnosis. An Bras Dermatol. 2010;85:669–675. doi: 10.1590/s0365-05962010000500010. [DOI] [PubMed] [Google Scholar]
- 13.Rad M, Hashemipoor MA, Mojtahedi A, Zarei MR, Chamani G, Kakoei S, et al. Correlation between clinical and histopathologic diagnoses of oral lichen planus based on modified WHO diagnostic criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:796–800. doi: 10.1016/j.tripleo.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Thongprasom K, Dhanuthai K. Steriods in the treatment of lichen planus: a review. J Oral Sci. 2008;50:377–385. doi: 10.2334/josnusd.50.377. [DOI] [PubMed] [Google Scholar]
- 15.Chainani-Wu N, Silverman S, Jr, Lozada-Nur F, Mayer P, Watson JJ. Oral lichen planus: patient profile, disease progression and treatment responses. J Am Dent Assoc. 2001;132:901–909. doi: 10.14219/jada.archive.2001.0302. [DOI] [PubMed] [Google Scholar]
- 16.Coronado-Castellote L, Jiménez-Soriano Y. Clinical and microbiological diagnosis of oral candidiasis. J Clin Exp Dent. 2013;5:e279–e286. doi: 10.4317/jced.51242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams DW, Jordan RP, Wei XQ, Alves CT, Wise MP, Wilson MJ, et al. Interactions of Candida albicans with host epithelial surfaces. J Oral Microbiol. 2013;5 doi: 10.3402/jom.v5i0.22434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sudbery P, Gow N, Berman J. The distinct morphogenic states of Candida albicans. Trends Microbiol. 2004;12:317–324. doi: 10.1016/j.tim.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Järvensivu A, Hietanen J, Rautemaa R, Sorsa T, Richardson M. Candida yeasts in chronic periodontitis tissues and subgingival microbial biofilms in vivo. Oral Dis. 2004;10:106–112. doi: 10.1046/j.1354-523x.2003.00978.x. [DOI] [PubMed] [Google Scholar]
- 20.Holmes AR, Bandara BM, Cannon RD. Saliva promotes Candida albicans adherence to human epithelial cells. J Dent Res. 2002;81:28–32. doi: 10.1177/002203450208100107. [DOI] [PubMed] [Google Scholar]
- 21.Rossie K, Guggenheimer J. Oral candidiasis: clinical manifestations, diagnosis, and treatment. Pract Periodontics Aesthet Dent. 1997;9:635–641. [PubMed] [Google Scholar]
- 22.Spolidorio LC, Martins VRG, Nogueira RD, Spolidorio DMP. Frequência de candida sp em biópsias de lesöes da mucosa bucal; The frequency of candida sp in biopsies of oral mucosal lesions. Pesqui Odontol Bras. 2003;17:89–93. doi: 10.1590/s1517-74912003000100017. [DOI] [PubMed] [Google Scholar]
- 23.Kragelund C, Kieffer-Kristensen L, Reibel J, Bennett EP. Oral candidosis in lichen planus: the diagnostic approach is of major therapeutic importance. Clin Oral Investig. 2013;17:957–965. doi: 10.1007/s00784-012-0757-6. [DOI] [PubMed] [Google Scholar]
- 24.Gorsky M, Epstein JB, Hasson-Kanfi H, Kaufman E. Smoking habits among patients diagnosed with oral lichen planus. Tob Induc Dis. 2004;2:103–108. doi: 10.1186/1617-9625-2-2-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van der Meij EH, Schepman KP, van der Waal I. The possible premalignant character of oral lichen planus and oral lichenoid lesions: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:164–171. doi: 10.1016/s1079-2104(03)00305-6. [DOI] [PubMed] [Google Scholar]
- 26.Krutchkoff DJ, Cutler L, Laskowski S. Oral lichen planus: the evidence regarding potential malignant transformation. J Oral Pathol. 1978;7:1–7. doi: 10.1111/j.1600-0714.1978.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 27.van der Meij EH, Schepman KP, Smeele LE, van der Wal JE, Bezemer PD, van der Waal I. A review of the recent literature regarding malignant transformation of oral lichen planus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:307–310. doi: 10.1016/s1079-2104(99)70033-8. [DOI] [PubMed] [Google Scholar]