Abstract
Although basal cell carcinoma can be effectively managed through surgical excision, the most suitable surgical margins have not yet been fully determined. Furthermore, micrographic surgery is not readily available in many places around the world. A review of the literature regarding the surgical treatment of basal cell carcinoma was conducted in order to develop an algorithm for the surgical treatment of basal cell carcinoma that could help the choice of surgical technique and safety margins, considering the major factors that affect cure rates. Through this review, it was found that surgical margins of 4mm seem to be suitable for small, primary, well-defined basal cell carcinomas, although some good results can be achieved with smaller margins and the use of margin control surgical techniques. For treatment of high-risk and recurrent tumors, margins of 5-6 mm or margin control of the surgical excision is required. Previous treatment, histological subtype, site and size of the lesion should be considered in surgical planning because these factors have been proven to affect cure rates. Thus, considering these factors, the algorithm can be a useful tool, especially for places where micrographic surgery is not widely available.
Keywords: Ambulatory surgical procedures; Carcinoma, basal cell; Margin
INTRODUCTION
In general, the best treatment for basal cell carcinoma (BCC) is surgical excision.1,2 A 5-year cure rate of at least 95% is considered reasonable and an acceptable goal to achieve.2 The lesion must be totally removed at the first surgical intervention, because primary BCC have higher cure rates than recurrent ones.3 Furthermore, there is a tendency that recurrent lesions become more aggressive. Consequently, the appropriate margins for complete removal of recurrent BCC should be almost twice as big as those for complete removal of primary BCC.4,5 Complete removal is the key for surgical treatment and it can be achieved either with safety margins or with micrographic control. Site, histological subtype, and size of the tumor are the main factors that can influence cure rates, and should be considered during surgical planning.
METHODS
A review of the literature on surgical margins for BCC was carried out. We also included articles on incomplete excision and articles which tried to identify predictive factors of recurrence. Each article was analyzed regarding surgical margins, cure rates, follow-up period, histological subtype, site and size of the tumor. Some data were grouped and presented in tables.
An algorithm was developed in order to systematize existing techniques and direct surgical treatment of BCC. Such an algorithm is not needed by Mohs micrographic surgeons, who already possess extremely effective techniques, but they are very useful in places where access to micrographic surgery is still not widely available.
Non-surgical options, although popular and particularly useful for non-facial superficial BCC, will not be covered by this paper.
RESULTS
Surgical Margins
For small and primary BCC, Bisson et al. have advocated the use of 3-mm margins. (Table 1) 6-11 However, complete excision was achieved in only 93% of the cases.9 Kimay-Asadi et al. 6 have used transoperative histological control of margins and concluded that small, nodular, well-defined BCC located on the face should be excised with 4-mm margins from the borders of the tumors. Similarly, Wolf & Zitelli 7 found that 4-mm margins totally cleared 98% of well-defined BCC smaller than 2 cm in diameter (but 9% of their 117 cases were larger than that). They have also found that BCCs larger than 2 cm in diameter tend to display more subclinical invasion than smaller ones.
TABLE 1.
Tumor eradication according to various surgical margins
| Surgical Margins | 1mm | 2mm | 3mm | 4mm | 5mm | 6mm | 8mm | 11mm |
|---|---|---|---|---|---|---|---|---|
| Sample Size | ||||||||
| n:13413 | 84% | 76% | 87% | |||||
| n:117 * 6 | - | 75% | 85% | 98% | - | - | - | - |
| n:917 | 64% | 76% | 89% | 96% | - | - | - | - |
| n:100 8 | 83% | 92% | 96% | - | - | - | - | - |
| n:49 •9 | - | - | - | - | 61,26% | - | 91,83% | 97,95 |
| n:862 ••10 | - | 53,7% | - | 87,9% | - | 97,5% | 99,1% | - |
Basal Cell Carcinoma (BCC) <2cm
high-risk BCC
primary and recurrent BCC
Likewise, Thomas et al 8 have concluded that the majority of non-melanoma skin cancers smaller than 2 cm in diameter should be excised with 4-mm margins, assisted by loupe magnification. However, they have also stated that well-defined tumors could be excised using 3-mm margins.
Kumar et al. 12 have found an incidence of incomplete excision of 4.2%, 4.1%, and 2.9% in 757 BCCs treated with margins of 1 to 2.5 mm, 3 to 4 mm, and 5 mm or more, respectively.
Pichardo-Velázquez et al. 10 have resected 83 high-risk BCCs with transoperative histological control, according to their definition: infiltrative > 5mm, nodular > 10mm, and nose tumors. Persistent tumors were re-excised with additional margins of 3 mm until clearance. After 25 months without recurrence, they recommended 5-mm margins plus transoperative histological control when Mohs micrographic surgery (MMS) was not available.
Incomplete Excision
Incomplete excision rates have been reported to range from 1.54% to 28.5%.10,12-37 Incomplete excision was more frequent in lateral margins (Table 2). This is consistente with what is widely reported in the literature. 12-16,18,29,38,39
TABLE 2.
Grouped incomplete excision rates according to positive margins 12-16,38,39
| Positive lateral margin | Positive deep margin | Positive lateral and deep margins |
|---|---|---|
| 66.19% (562/849) | 21.08% (179/849) | 9.89% (84/849) |
- In 3.53% (30/849) of cases there was no reference to which margin has been affected
- Three lesions which had simultaneously positive deep and lateral margins were included into all three groups 14
Palmer et al. 40 have re-operated incompletely excised BCCs with MMS in a mean time of 11 weeks, and found histological evidence of residual tumor in 69% of the cases. The presence of clinically visible tumors at the time of re-excision was associated with an unexpectedly large number of required stages.
Defining factors on choosing surgical margins
1. Previous treatment
The recurrence rates for primary BCC range from 0.5% to 10.1%, and from 2% to 11.6% for previously treated BCC.3,11,13,21,23,24,27,41-45 Higher recurrence rates occur with incompletely excised BCC and range from 14% to 41%.17,18,23-25,32,33,39,46
2. Histologic subtype
According to the data gathered in table 3, incomplete excision of the tumor was more common in aggressive subtypes (infiltrative, mixed and sclerosing).12,13,47,48
TABLE 3.
Grouped incomplete excision rates according to histological subtype
| Histological subtype | Histological growth | % Incomplete excision |
|---|---|---|
| Infiltrative ** 12,13,47 | Aggressive | 22.42% (50/223) |
| Mixed □ 12,47 | Aggressive | 22.08% (55/249) |
| Sclerosing 12,13,47 | Aggressive | 15.78% (12/76) |
| Superficial * 12,13,47 | Indolent | 7.56% (19/251) |
| Nodular 12,13,47 | Indolent | 3.18% (19/596) |
Grouped subtypes:
8 superficial + 7 multifocal 13
29 infiltrative+ 1 micronodular 12
24 infiltrative + 59 micronodular 47
Crowson’s classification 48 does not consider the mixed (pleomorphic) subtype Sexton 47 divided mixed tumors into nodular/micronodular pattern (16.5% or 19/115 with incomplete excision) and infiltrative pattern (30.1% or 31/103 with incomplete excision)
Through the resection of primary BCC with MMS, Salache has realized that sclerosing tumors had greater subclinical extension than other tumors. 49 Similarly, Lang and Lee et al. have found that aggressive recurrent BCC had greater subclinical extensions than non-aggressive ones.50,51 Welsch et al. have found that deep invasion was more frequent in aggressive BCC, mainly in the micronodular and infiltrative types.52
Sexton et al. have found that aggressive subtypes had the highest incomplete excision rates (micronodular 18.6%, infiltrative 26.5% and sclerosing 33.3%), whereas nodular and superficial BCC treated by standard surgery had high complete excision rates (93.6% and 96.4%, respectively).47
3. Site
The most frequent sites for incomplete excision are the nose, the ear and the area around the eyes (Table 4).12-21,38
TABLE 4.
Grouped incomplete excision rates according to lesion site
| Site | % Incomplete excision |
|---|---|
| Nose 12-15,17-21,38 | 13.6 (315/2301) |
| Ears area 12-15,17-21,38 | 13.2 (147 /1108 ) |
| Periocular 12-15,17-21,38 | 11.7 (142/1204) |
| Lips 12,13,18,20,21,38 | 9.2 (22/237) |
| Rest of the face 13,15,17-21 | 7.78 (154/1979) |
| Fronto-temporal area 12-15,18-21,38 | 6.81 (185/2713) |
| Scalp 12-15,18-21,38 | 6.2 (29/465) |
| Trunk 12,14,15,18-21,38 | 5.0 (69/1374) |
| Members 12,14,15-21,38 | 4.0 (82/2043) |
| Neck 12,14,15,18,19,21,38 | 1.6 (21/744) |
4. Size
There is controversy whether the size affects or not BCC recurrence rate. However, some authors have noted that incomplete excision was more common in larger lesions. 3,12,14,23,41,42,53,54
5. Gender
It is not well known whether gender can influence the recurrence rate of BCC. There are reports which state that BCC recurs more often in men. Silverman et al. 3 have identified the male gender as an independent factor for recurrence.3,42,55 On the other hand, incomplete excision was more common in women.12,15,19,35
DISCUSSION
The recurrence rate is higher in incompletely excised lesions, and primary BCC recurs less often than previously treated BCC.3 Therefore, the proper use of suitable surgical margins for BCC is a key point, given that the greatest chance of cure lies in the first approach.
The identification of clinical margins is the first step to correctly apply surgical margins. Apparently, preoperative use of loupe magnification or dermoscopy may favor recognition of the margins, improving complete excision rates.8,56-58 Caresana and Giardini have reported a 98.5% complete excision rate of BCC excised with 2-mm margins, demarcated with the use of dermoscopy.59
Surgical Margins
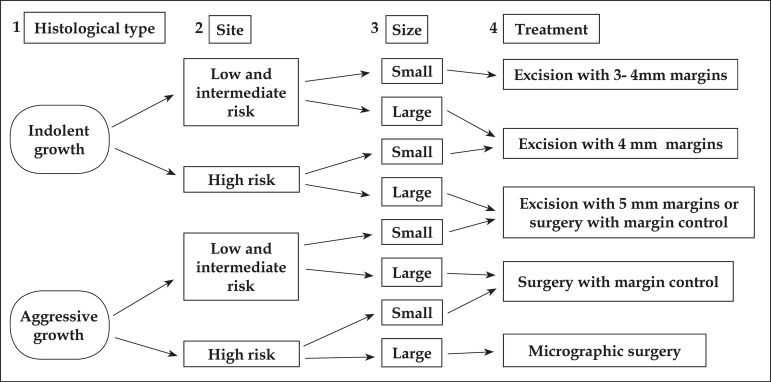
By analyzing table1, it can be concluded that the use of 4-mm margins were satisfactory for primary well-defined BCCs smaller than 2 cm in diameter. Similar cure rates were achieved with 3-mm margins, although, occasionally, 2-mm margins may be enough. 9,12 Nevertheless, Bisson has found that margins smaller than 3 mm increase recurrence risk, even if histopathology is tumor-free.9 Based on that, this paper suggests excision with 3- to 5-mm margins for: - any primary BCCs with indolent histology; or - small BCCs with aggressive growth outside the high-risk areas. For other aggressive types of BCCs, we suggest surgery with margin control (Figure 1).
FIGURE 1.
Algorithm for treatment of primary Basal Cell Carcinoma
1- Aggressive: infiltrative, sclerosing and metatypical
Indolent: nodular and superficial
The authors suggest to classify the mixed (pleomorphic) subtype as aggressive for treatment purposes, even if the predominant pattern is indolent
2- Low risk: trunk and extremity
Intermediate risk: scalp, neck, forehead and cheek
High risk: centrofacial, nose, temple, periocular region, perioral and ears
3-There is no consensus on the classification of tumor size. The authors suggest to classify large lesions as lesions larger than 1cm in high-risk áreas; lesions larger than 2cm in intermediate-risk áreas; and lesions larger than 4cm in low-risk areas
4-The control of margins can be done by several micrographic techniques or by freezing.
Micrographic surgery can be performed using the Mohs technique, the Munich technique or the Tübingen technique.
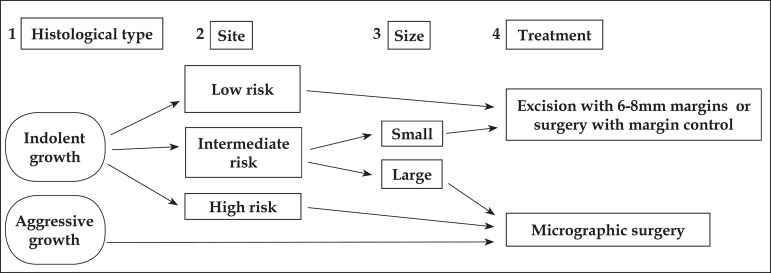
There is a gap in the literature on the ideal surgical margins for excision of high-risk and recurrent BCCs. Despite the fact that micrographic control is the best choice, some authors have suggested 5-mm margins for high-risk and 6-mm margins for reccurent BCCs as still appropriate. Based on these results, this paper suggests excision with at least 6-mm margins or surgery with margin control for recurrent BCC with indolent growth in low-risk areas and intermediate-risk areas, provided that they are small.10,11 For other large tumors with indolent growth and for all aggressive recurrent BCCs, the authors suggest micrographic surgery, given that the subclinical extension of these lesions is unpredictable (Figure 2).
FIGURE 2.
Algorithm for treatment of primary Basal Cell Carcinoma
In general, our indications for surgical excision with controlled margins are in agreement with the AAD/ACMS/ASDSA/ASMS guidelines. 60 However, this paper suggests alternative techniques when micrographic techniques are not accessible (Figures 1 and 2).
Defining factors on choosing the surgical margins
1.Previous treatment
Any comparison between recurrence rates reported in the literature should be made carefully as the studies differ on the surgical techniques and follow-up time used, on the status of the tumor and on recurrence rates after incomplete excision.
Silverman et al.61 have reported that follow-up time, status of tumor and different statistical methodologies interfered with the results. Rowe et al.,62 in a systematic review, have found that the 5-year recurrence rate was at least 3.5 times greater when the follow-up time was shorter.
Classifying primary or recurrent tumors is essential for surgical planning, because primary BCCs have lower recurrence rates than previously treated BCCs and the margins necessary for complete eradication of recurrent tumors are almost twice as big as those required to eradicate primary BCCs. 3,5,11 Moreover, recurrent lesions have higher risk of recurrence, greater subclinical extension and a tendency to become more aggressive than the original tumor. 1,5,50,63
Consequently, the choice of technique must consider the previous treatment history. For primary tumors, conventional surgery with suitable margins can be applied safely to most cases (Figure 1).1 In the case of recurrent tumors, although micrographic surgery is the treatment of choice, satisfactory outcomes have been obtained with other margin control methods and/or excision with wider margins. 11 Therefore, the present paper suggests at least 6-mm margins or surgical margin control, either using a micrograph or not (Figure 2).
2. Histological subtype
Because some histological subtypes are more associated with high rates of incomplete excision and recurrence, the analysis of histological growth pattern is a key factor to be considered when planning surgery.
In 2006, Crowson48 classified BCC as indolent (superficial and nodular) or aggressive (infiltrative, metatypical, micronodular and sclerosing). Previously, it had been shown that more aggressive histological growth was associated with increased subclinical extension, indicating that more aggressive tumors require larger surgical margins to be eradicated.64 Crowson's classification is simple and practical, therefore it was adapted and included in our algorithm. In this paper, a mixed subtype was considered aggressive because of high incomplete resection rates. Furthermore, Betti et al,65 have also concluded that mixed BCC have a potential aggressive behavior. They have observed that the superficial or nodular subtype was associated with infiltrative/morpheiform types in more than 40% of cases and margin involvement was more prevalent in mixed than in single BCC.
The aggressive subtypes are clearly more likely to recur and should be treated with wider margins or histological control. In table 3, it can be seen that infiltrative and mixed patterns were mostly associated with complete excision (22.42% and 22.08%, respectively). Sexton et al. have identified 30.1% of incomplete excision when these two patterns were associated.47
In this algorithm, superficial BCC was classified as of indolent growth and surgical approach was the only treatment that was considered. Nevertheless, Roozeboom et al.66 have discussed others therapies in a recent review. On the other hand, Mina et al,67 have reviewed 158 purely superficial, primary and recurrent BCCs in the head and neck region, treated with MMS. They have found higher recurrence rates (3,7%) and larger defect sizes than expected.
The correspondence between the histological subtype found in the biopsy and the one found in the subsequent excision ranged from 60.9% to 82% in primary BCCs, and reached 67.1% in recurrent tumors. 52,68-72 The biopsy failed to identify aggressive componentes in up to 11% of primary tumors and in 19% of recurrent tumors.69,72 This fact may be due to the frequent association between different histological types - as there are reports of up to 74% of primary mixed tumors - and to the fact that the accuracy in identifying mixed tumors is quite small (37%) when compared to tumors of a single histological type (83%).68,69 Messina et al.73 have found a correlation between the histological type predominantly found in biopsy material and the one found in the surgical specimen in 78.3% of cases. When the biopsy described the predominant and accessory types, the correlation increased 8.7%, reaching 87%. When BCC was classified as aggressive or non-aggressive, the correlation reached 92.7%. These findings are extremely important because tumor aggressiveness will determine surgical margins. Therefore, prior biopsy is a guiding element routinely used in tumor management.
3. Site
Table 4 is in agreement with most reports in the literature. However, the scalp and other high-risk areas on the face have already been associated with higher recurrence rates.15-22,29,32,37,41,53,55,66 Based on these results, tumor site seems to influence cure rates, although this association is not significant for some authors. Following this reasoning, the recurrence rates in these high-risk areas may be related to the use of smaller safety margins and not to specific tumor characteristics.
Huang and Boyce have divided the body in low-, intermediate- and high-risk areas.64 The trunk and the extremities are low-risk areas; the cheeks, forehead, scalp and neck are intermediate-risk areas; and the central facial area, the nose, jaw, the temples, and the periocular, perioral and periauricular areas are high-risk areas.
In this review, except for the jaw and the temples, the nose, the ears and the periocular regions reached the highest rates of incomplete excision (Table 4). This classification was therefore adopted by our algorithm (Figures 1 and 2).
4. Size
Despite the controversial influence of tumor size on recurrence rates, Breuninger and Dietz5, similarly to Wolf and Ziteli7, have proved that there is a wide variation in subclinical extension, in terms of tumor diameter. Reinforcing this view, Cigna et al. have reported that tumors larger than 5 cm in diameter have poor prognosis.27
Based on these studies, tumor size was adopted as one of the elements to be considered in the algorithm (Figures 1 and 2). As most studies concerning surgical margins have included mostly smaller tumors, the optimal approach for larger tumors still lacks substantial evidence.
CONCLUSION
Despite the broad literature available on the treatment of basal cell carcinoma, there are only a few articles about surgical margins and most of them are limited to analyzing small and primary lesions. A 4-mm excision margin seems to be suitable to eradicate primary BCC lesions smaller than 2 cm in diameter. Nevertheless, even in these tumors histological types, lesion site and previous treatment history must be considered in surgical planning.
Surgical techniques with micrographically controlled margins are more appropriate for recurrent lesions, because conventional surgery often relies on the application of oncological radical resection with three-dimensional margins exceeding 6 mm.
However, limited access to micrographic techniques, especially outside the USA, requires the use of alternative techniques until Mohs' micrographic surgery becomes more widely disseminated. Therefore, the algorithm shown in figures 1 and 2 may be a useful tool in guiding the surgical treatment of basal cell carcinoma.
Footnotes
Financial Support: None.
Conflict of Interest: None.
How to cite this article: Luz FB, Ferron C, Cardoso GP. Surgical treatment of basal cell carcinoma: an algorithm based on the literature. An Bras Dermatol. 2015; 90(3):377-83.
Study conducted at the Private practice - Niterói (RJ), Brazil.
Reference
- 1.Telfer NR, Colver GB, Morton CA, British Association of Dermatologists Guidelines for the management of basal cell carcinoma. Br J Dermatol. 2008;159:35–48. doi: 10.1111/j.1365-2133.2008.08666.x. [DOI] [PubMed] [Google Scholar]
- 2.Gulleth Y, Goldberg N, Silverman RP, Gastman BR. What is the Best Surgical Margin for a Basal Cell Carcinoma: A Meta-Analysis of the Literature. Plast Reconstr Surg. 2010;126:1222–1231. doi: 10.1097/PRS.0b013e3181ea450d. [DOI] [PubMed] [Google Scholar]
- 3.Silverman MK, Kopf AW, Bart RS, Grin CM, Levenstein MS. Recurrence Rates of Treated Basal Cell carcinomas. Part 3: Surgical Excision. J Dermatol Surg Oncol. 1992;18:471–476. doi: 10.1111/j.1524-4725.1992.tb03307.x. [DOI] [PubMed] [Google Scholar]
- 4.Boulinguez S, Grison-Tabone C, Lamant L, Valmary S, Viraben R, Bonnetblanc JM, et al. Histological evolution of recurrent basal cell carcinoma and therapeutic implications for incompletely excised lesions. Br J Dermatol. 2004;151:623–626. doi: 10.1111/j.1365-2133.2004.06135.x. [DOI] [PubMed] [Google Scholar]
- 5.Breuninger H, Dietz K. Prediction of Subclinical Tumor Infiltration in Basal Cell Carcinoma. J Dermatol Surg Oncol. 1991;17:574–578. doi: 10.1111/j.1524-4725.1991.tb03655.x. [DOI] [PubMed] [Google Scholar]
- 6.Kimyai-Asadi A, Alam M, Goldberg LH, Peterson SR, Silapunt S, Jih MH. Efficacy of narrow-margin excision of well-demarcated primary facial basal cell carcinoma. J Am Acad Dermatol. 2005;53:464–468. doi: 10.1016/j.jaad.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 7.Wolf DJ, Zitelli JA. Surgical Margins for basal cell carcinoma. Arch Dermatol. 1987;123:340–344. [PubMed] [Google Scholar]
- 8.Thomas DJ, King AR, Peat BG. Excision margins for nonmelanotic skin cancer. Plast Reconstr Surg. 2003;112:57–63. doi: 10.1097/01.PRS.0000067479.77859.31. [DOI] [PubMed] [Google Scholar]
- 9.Bisson MA, Dunkin CS, Suvarna SK, Griffiths RW. Do plastic surgeons resect basal cell carcinomas too widely? A prospective study comparing surgical and histological margins. Br J Plast Surg. 2002;55:293–297. doi: 10.1054/bjps.2002.3829. [DOI] [PubMed] [Google Scholar]
- 10.Pichardo-Velázquez P, Domínguez-Cherit J, Vega-Memije Ma, Moreno-Coutiño G, Proy H. Surgical option for nonmelanoma skin cancer. Int J Dermatol. 2004;43:148–150. doi: 10.1111/j.1365-4632.2004.02091.x. [DOI] [PubMed] [Google Scholar]
- 11.Wetzig T, Woitek M, Eichhorn K, Simon JC, Paasch U. Surgical excision of basal cell carcinoma with complete margin control: outcome at 5-years follow-up. Dermatology. 2010;220:363–369. doi: 10.1159/000300116. [DOI] [PubMed] [Google Scholar]
- 12.Kumar P, Watson S, Brain AN, Davenport PJ, McWilliam LJ, Banerjee SS, et al. Incomplete excision of basal cell carcinoma: a prospective multicentre audit. Br J Plast Surg. 2002;55:616–622. doi: 10.1054/bjps.2002.3948. [DOI] [PubMed] [Google Scholar]
- 13.Farhi D, Dupin N, Palangié A, Carlotti A, Avril MF. Incomplete Excision of Basal Cell Carcinoma: Rate and Associated Factors among 362 Consecutive Cases. Dermatol Surg. 2007;33:1207–1214. doi: 10.1111/j.1524-4725.2007.33255.x. [DOI] [PubMed] [Google Scholar]
- 14.Kumar P, Orton CI, McWilliam LJ, Watson S. Incidence of incomplete excision in surgically treated basal cell carcinoma: a retrospective clinical audit. Br J Plast Surg. 2000;53:563–566. doi: 10.1054/bjps.2000.3394. [DOI] [PubMed] [Google Scholar]
- 15.Malik V, Goh KS, Leong S, Tan A, Downey D, O'Donovan D. Risk and outcome analysis of 1832 consecutively excised basal cell carcinoma's in a tertiary referral plastic surgery unit. J Plast Reconstr Aesthet Surg. 2010;63:2057–2063. doi: 10.1016/j.bjps.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 16.Dieu T, Macleod AM. Incomplete excision of basal cell carcinomas: a retrospective audit. ANZ J Surg. 2002;72:219–221. doi: 10.1046/j.1445-2197.2002.02351.x. [DOI] [PubMed] [Google Scholar]
- 17.Nagore E, Grau C, Molinero J, Fortea JM. Positive margins in basal cell carcinoma: relationship to clinical features and recurrence risk. A retrospective study of 248 patients. J Eur Acad Dermatol Venereol. 2003;17:167–170. doi: 10.1046/j.1468-3083.2003.00535.x. [DOI] [PubMed] [Google Scholar]
- 18.Sherry KR, Reid LA, Wilmshurst AD. A five year review of basal cell carcinoma excisions. J Eur Acad Dermatol Venereol. 2003;17:167–170. doi: 10.1016/j.bjps.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 19.Hansen C, Wilkinson D, Hansen M, Soyer HP. Factors contributing to incomplete excision of nonmelanoma skin cancer by Australian general practitioners. Arch Dermatol Arch Dermatol. 2009;145:1253–1260. doi: 10.1001/archdermatol.2009.270. [DOI] [PubMed] [Google Scholar]
- 20.Bogdanov-Berezovsky A, Cohen AD, Glesinger R, Cagnano E, Krieger Y, Rosenberg L. Risk Factors for Incomplete Excision of Basal Cell Carcinomas. Acta Derm Venereol. 2004;84:44–47. doi: 10.1080/00015550310020585. [DOI] [PubMed] [Google Scholar]
- 21.Goh BK, Ang P, Wu YJ, Goh CL. Characteristics of basal cell carcinoma amongst Asians in Singapore and a comparison between completely and incompletely excised tumors. Int J Dermatol. 2006;45:561–564. doi: 10.1111/j.1365-4632.2004.02515.x. [DOI] [PubMed] [Google Scholar]
- 22.Griffiths RW. Audit of histologically incompletely excised basal cell carcinomas: recommendations for management by re-excision. Br J Plast Surg. 1999;52:24–28. doi: 10.1054/bjps.1998.3018. [DOI] [PubMed] [Google Scholar]
- 23.Hussain M, Earley MJ. The incidence of incomplete excision in surgically treated basal cell carcinoma: a retrospective clinical audit. Ir Med J. 2003;96:18–20. [PubMed] [Google Scholar]
- 24.Foo CL, Tan SH, Tan KC. Basal cell carcinoma of the head and neck region - a five-year study (1984-88) Ann Acad Med Singapore. 1990;19:182–185. [PubMed] [Google Scholar]
- 25.Rippey JJ, Rippey E. Characteristics of incompletely excised basal cell carcinoma of the skin. Med J Aust. 1997;166:581–583. doi: 10.5694/j.1326-5377.1997.tb123268.x. [DOI] [PubMed] [Google Scholar]
- 26.Tiftikcioglu YO, Karaaslan O, Aksoy HM, Aksoy B, Koçer U. Basal cell carcinoma in Turkey. J Dermatol. 2006;33:91–95. doi: 10.1111/j.1346-8138.2006.00019.x. [DOI] [PubMed] [Google Scholar]
- 27.Cigna E, Tarallo M, Maruccia M, Sorvillo V, Pollastrini A, Scuderi N. Basal cell carcinoma: 10 years of experience. J Skin Cancer. 2011;2011:476362–476362. doi: 10.1155/2011/476362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Friedman HI, Williams T, Zamora S, Al-Assaad ZA. Recurrent basal cell carcinoma in margin-positive tumors. Ann Plast Surg. 1997;38:232–235. doi: 10.1097/00000637-199703000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Bariani RL, Nahas FX, Barbosa MV, Farah AB, Ferreira LM. Basal cell carcinoma: an updated epidemiological and therapeutically profile of an urban population. Acta Cir Bras. 2006;21:66–73. doi: 10.1590/s0102-86502006000200003. [DOI] [PubMed] [Google Scholar]
- 30.Schreuder F, Powell BW. Incomplete excsion of basal cell carcinomas: na audit. Clin Perform Qual Health Care. 1999;7:119–120. doi: 10.1108/14664109910306712. [DOI] [PubMed] [Google Scholar]
- 31.Babaye-Nazhad S, Amirnia M, Alikhah H, Khodaeyani E, Atapour N. Safety margin in excision of basal cell carcinoma. Pak J Biol Sci. 2009;12:1408–1414. doi: 10.3923/pjbs.2009.1408.1414. [DOI] [PubMed] [Google Scholar]
- 32.Santiago F, Serra D, Vieira R, Figueiredo A. Incidence and factors associated with recurrence after incomplete excision of basal cell carcinomas: a study of 90 cases. J Eur Acad Dermatol Venereol. 2010;24:1421–1424. doi: 10.1111/j.1468-3083.2010.03662.x. [DOI] [PubMed] [Google Scholar]
- 33.Wilson AW, Howsam G, Santhanam V, Macpherson D, Grant J, Pratt CA, et al. Surgical management of incompletely excised basal cell carcinoma of the head and neck. Br J Oral Maxillofac Surg. 2004;42:311–314. doi: 10.1016/j.bjoms.2004.02.030. [DOI] [PubMed] [Google Scholar]
- 34.Pua VS1, Huilgol S, Hill D. Evaluation of the treatment of non-melanoma skin cancers by surgical excision. Australas J Dermatol. 2009;50:171–175. doi: 10.1111/j.1440-0960.2009.00531.x. [DOI] [PubMed] [Google Scholar]
- 35.Fleischer AB, Jr, Feldman SR, Barlow JO, Zheng B, Hahn HB, Chuang TY, et al. The specialty of the treating physician affects the likehood of tumor-free resection margins for basal cell carcinoma: results from a multi-institutional retrospective study. J Am Acad Dermatol. 2001;44:224–230. doi: 10.1067/mjd.2001.110396. [DOI] [PubMed] [Google Scholar]
- 36.Asif M, Mamoon N, Ali Z, Akhtar F. Epidemiological and excision margin status of basal cell carcinoma- three years armed forces institute of pathology experience in Pakistan. Asian Pac J Cancer Prev. 2010;11:1421–1423. [PubMed] [Google Scholar]
- 37.Hakverdi S, Balci DD, Dogramaci CA, Toprak S, Yaldiz M. Retrospective analysis of basal cell carcinoma. Indian J Dermatol Venereol Leprol. 2011;77:251–251. doi: 10.4103/0378-6323.77483. [DOI] [PubMed] [Google Scholar]
- 38.Griffiths RW, Suvarna SK, Stone J. Basal cell carcinoma histological clearance margins: an analysis of 1539 conventionally excised tumours. Wider still and deeper? J Plast Reconstr Aesthet Surg. 2007;60:41–47. doi: 10.1016/j.bjps.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 39.Richmond JD, Davie RM. The significance of incomplete excision in patients with basal cell carcinoma. Br J Plast Surg. 1987;40:63–67. doi: 10.1016/0007-1226(87)90013-0. [DOI] [PubMed] [Google Scholar]
- 40.Palmer VM, Wilson PR. Incompletely Excised Basal Cell Carcinoma: Residual Tumor Rates at Mohs Re-Excision. Dermatol Surg. 2013;39:706–718. doi: 10.1111/dsu.12113. [DOI] [PubMed] [Google Scholar]
- 41.Bart RS, Schrager D, Kopf AW, Bromberg J, Dubin N. Scalpel excision of basal cell carcinoma. Arch Dermatol. 1978;114:739–742. [PubMed] [Google Scholar]
- 42.Rigel DS, Robins P, Friedman RJ. Predicting recurrence of basal-cell carcinomas treated by microscopically controlled excision. A recurrence index score. J Dermatol Surg Oncol. 1981;7:807–810. doi: 10.1111/j.1524-4725.1981.tb00171.x. [DOI] [PubMed] [Google Scholar]
- 43.Cataldo PA, Stoddard PB, Reed WP. Use frozen section analysis in the treatment of basal cell carcinoma. Am J Surg. 1990;159:561–563. doi: 10.1016/s0002-9610(06)80066-8. [DOI] [PubMed] [Google Scholar]
- 44.Niederhagen B, von Lindern JJ, Bergé S, Appel T, Reich RH, Krüger E. Staged operations for basal cell carcinoma of the face. Br J Oral Maxillofac Surg. 2000;38:477–479. doi: 10.1054/bjom.2000.0322. [DOI] [PubMed] [Google Scholar]
- 45.Chow VL, Chan JY, Chan RC, Chung JH, Wei WI. Basal Cell Carcinoma of the Head and Neck Region in Ethnic Chinese. Int J Surg Oncol. 2011;2011:890908–890908. doi: 10.1155/2011/890908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Longhi P, Serra MP, Robotti E. Incompletely excised basal cell carcinomas: our guidelines. Onco Targets Ther. 2008;1:1–4. doi: 10.2147/ott.s3540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sexton M, Jones DB, Maloney ME. Histologic pattern analysis of basal cell carcinoma. Study of a series of 1039 consecutive neoplasms. J Am Acad Dermatol. 1990;23:1118–1126. doi: 10.1016/0190-9622(90)70344-h. [DOI] [PubMed] [Google Scholar]
- 48.Crowson AN. Basal cell carcinoma: biology, morphology and clinical implications. Mod Pathol. 2006;19:S127–S147. doi: 10.1038/modpathol.3800512. [DOI] [PubMed] [Google Scholar]
- 49.Salasche SJ, Amonette RA. Morpheaform basal cell epithelioma. A study of subclinical extensions series of 51 cases. J Dermatol Surg Oncol. 1981;7:387–394. doi: 10.1111/j.1524-4725.1981.tb00662.x. [DOI] [PubMed] [Google Scholar]
- 50.Lang PG, Jr, Maize JC. Histologic evolution of recurrent basal cell carcinoma and treatment implications. J Am Acad Dermatol. 1986;14:186–196. doi: 10.1016/s0190-9622(86)70020-0. [DOI] [PubMed] [Google Scholar]
- 51.Lee KC, Higgins HW, 2nd, Cruz AP, Dufresne RG., Jr Characteristics of Basal Cell carcinoma of the Lip Treated Using Mohs Micrographic Surgery. Dermatol Surg. 2012;38:1956–1961. doi: 10.1111/j.1524-4725.2012.02580.x. [DOI] [PubMed] [Google Scholar]
- 52.Welsch MJ, Troiani BM, Hale L, DelTondo J, Helm KF, Clarke LE. Basal cell carcinoma characteristics as predictors of depth of invasion. J Am Acad Dermatol. 2012;67:47–53. doi: 10.1016/j.jaad.2011.02.035. [DOI] [PubMed] [Google Scholar]
- 53.Bøgelund FS, Philipsen PA, Gniadecki R. Factors affecting the recurrence rate of basal cell carcinoma. Acta Derm Venereol. 2007;87:330–334. doi: 10.2340/00015555-0236. [DOI] [PubMed] [Google Scholar]
- 54.Kyrgidis A, Vahtsevanos K, Tzellos TG, Xirou P, Kitikidou K, Antoniades K, et al. Clinical, histological and demographic predictors for recurrence and second primary tumours of head and neck basal cell carcinoma. A 1062 patient-cohort study from a tertiary cancer referral hospital. Eur J Dermatol. 2010;20:276–282. doi: 10.1684/ejd.2010.0903. [DOI] [PubMed] [Google Scholar]
- 55.Bumpous JM, Padhya TA, Barnett SN. Basal cell carcinoma oh the head and neck: identification of predictors of recurrence. Ear Nose Throat J. 2000;79:200-2, 204. [PubMed] [Google Scholar]
- 56.Carducci M, Bozzetti M, Foscolo AM, Betti R. Margin detection using digital dermatoscopy improves the performace of traditional surgical excsion of basal cell carcinomas oh the head and neck. Dermatol Surg. 2011;37:280–285. doi: 10.1111/j.1524-4725.2010.01870.x. [DOI] [PubMed] [Google Scholar]
- 57.Barcaui C. Análise pré-operatória de tumores cutâneos. Surg Cosmet Dermatol. 2011;3:77–79. [Google Scholar]
- 58.Carducci M, Bozzetti M, De Marco G, Foscolo AM, Betti R. Usefulness of margin detection by digital dermoscopy in the traditional surgical excision of basal cell carcinomas of the headand neck including infiltrative/morpheaform type. J Dermatol. 2012;39:326–330. doi: 10.1111/j.1346-8138.2011.01449.x. [DOI] [PubMed] [Google Scholar]
- 59.Caresana G, Giardini R. Dermoscopy-guided surgery in basal cell carcinoma. J Eur Acad Dermatol Venereol. 2010;24:1395–1399. doi: 10.1111/j.1468-3083.2010.03652.x. [DOI] [PubMed] [Google Scholar]
- 60.American Academy of Dermatology. American College of Mohs Surgery. American Society for Dermatologic Surgery Association. American Society for Mohs Surgery. Ad Hoc Task Force. Connolly SM, et al. AAD/ACMS/ASDA/ASMS 2012 Appropriate use criteria for Mohs Micrographic Surgery: a report of the American Academy of dermatology, American College of Mohs Surgery, American Society for dermatologic Surgery Association, and the American Society for Mohs Surgery. Dermatol Surg. 2012;38:1582–1603. doi: 10.1111/j.1524-4725.2012.02574.x. [DOI] [PubMed] [Google Scholar]
- 61.Silverman MK, Kopf AW, Grin CM, Bart RS, Levenstein MJ. Recurrence rates of basal cell carcinomas. Part 1: Overview. J Dermatol Surg Oncol. 1991;17:713–718. doi: 10.1111/j.1524-4725.1991.tb03424.x. [DOI] [PubMed] [Google Scholar]
- 62.Rowe DE, Carroll RJ, Day CL., Jr Long-term recurrence rates in previously untreated (primary) basal cell carcinoma: implications for patient follow-up. J Dermatol Surg Oncol. 1989;15:315–328. doi: 10.1111/j.1524-4725.1989.tb03166.x. [DOI] [PubMed] [Google Scholar]
- 63.Hendrix JD, Jr, Parlette HL. Duplicitous growth of infiltrative basal cell carcinoma. Analysis of clinically undetected tumor extent in a paired case-control sutdy. Dermatol Surg. 1996;22:535–539. [PubMed] [Google Scholar]
- 64.Huang CC, Boyce SM. Surgical Margins of excision for basal cell carcinoma and squamous cell carcinoma. Semin Cutan Med Surg. 2004;23:167–173. doi: 10.1016/j.sder.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 65.Betti R, Radaelli G, Crosti C, Ghiozzi S, Moneghini L, Menni S. Margin involvement and clinical pattern of basal cell carcinoma with mixed histology. J Eur Acad Dermatol Venereol. 2012;26:483–487. doi: 10.1111/j.1468-3083.2011.04104.x. [DOI] [PubMed] [Google Scholar]
- 66.Roozeboom MH, Arits AH, Nelemans PJ, Kelleners-Smeets NW. Overall treatment success after treatment of primary superficial basal cell carcinoma: a systematic review and meta-analysis of randomized and nonrandomized trials. Br J Dermatol. 2012;167:733–756. doi: 10.1111/j.1365-2133.2012.11061.x. [DOI] [PubMed] [Google Scholar]
- 67.Mina MA, Picariello A, Fewkes JL. Superficial Basal Cell Carcinomas of the Head and Neck. Dermatol Surg. 2013;39:1003–1008. doi: 10.1111/dsu.12178. [DOI] [PubMed] [Google Scholar]
- 68.Roozeboom MH, Mosterd K, Winnepenninckx VJ, Nelemans PJ, Kelleners-Smeets NW. Agreement between histological subtype on punch biopsy and surgical excision in primary basal cell carcinoma. J Eur Acad Dermatol Venereol. 2013;27:894–898. doi: 10.1111/j.1468-3083.2012.04608.x. [DOI] [PubMed] [Google Scholar]
- 69.Wolberink EA, Pasch MC, Zeiler M, van Erp PE, Gerritsen MJ. High discordance between punch biopsy and excision in establishing basal cell carcinoma subtype: analysis of 500 cases. J Eur Acad Dermatol Venereol. 2013;27:985–989. doi: 10.1111/j.1468-3083.2012.04628.x. [DOI] [PubMed] [Google Scholar]
- 70.Russell EB, Carrington PR, Smoller BR. Basal cell carcinoma: A comparison of shave biopsy versus punch biopsy techniques in subtype diagnosis. J Am Acad Dermatol. 1999;41:69–71. doi: 10.1016/s0190-9622(99)70409-3. [DOI] [PubMed] [Google Scholar]
- 71.Haws AL, Rojano R, Tahan SR, Phung TL. Accuracy of biopsy sampling for subtyping basal cell carcinoma. J Am Acad Dermatol. 2012;66:106–111. doi: 10.1016/j.jaad.2011.02.042. [DOI] [PubMed] [Google Scholar]
- 72.Mosterd K, Thissen MR, van Marion AM, Nelemans PJ, Lohman BG, Steijlen PM, et al. Correlation between histological findings on punch biopsy specimens and subsequent excision specimens in recurrent BCC. J Am Acad Dermatol. 2011;64:323–327. doi: 10.1016/j.jaad.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 73.Messina MCL, Valente NYS, Castro LGM. Is incisional biopsy helpful in the histopathological classification of basal cell carcinoma. An Bras Dermatol. 2006;81:443–448. [Google Scholar]