Abstract
Brachioradial pruritus is a chronic sensory neuropathy of unknown etiology which affects the skin of the shoulders, arms and forearms on the insertion of the brachioradialis muscle. We describe the case of a 60-yearold woman recently diagnosed with multiple myeloma who refers paresis, severe pruritus and itching lesions on the right arm with 6 months of evolution. Investigation led to a diagnosis of Brachioradial pruritus consequent to the presence of cervical disc herniation and Parsonage-Turner syndrome. The patient started gabapentin 900mg/day with good control of itching. Corticosteroids and antihistamines are often ineffective in the treatment of BP. Gabapentin has been used with encouraging results. All patients with Brachioradial pruritus should be evaluated for cervical spine injuries.
Keywords: Brachial plexus neuritis, Intervertebral disc displacement, Pruritus
INTRODUCTION
Brachioradial pruritus (BP) is a chronic sensory neuropathy which affects the skin of the shoulders, arms and forearms on the insertion of the brachioradialis muscle. The etiology is unknown, although some authors emphasize an association with sun exposure and/or cervical spine injuries.1,2
In 1968, Waisman first described cases of patients with very intense and persistent itch of the skin over the insertion of the brachioradialis muscle, having this pathology related to intense sun exposure. 3 The skin in the affected region was normal and the pruritus was resistant to treatment with systemic or topical corticosteroids, oral antihistamines, or anxiolytics.
Additionally, in 1983, Heyl associated BP with cervical spine disorders such as osteoarthritis, trauma or disc herniations.4 Some authors have suggested that cutaneous nerves can be simultaneously damaged by solar radiation and cervical spine injuries.
This case report describes an example of BP not associated with sun exposure.
CASE REPORT
A 60-year-old woman with multiple myeloma was referred to dermatology consultation for an intense pruritus on her right arm with six months evolution and no worsening after sun exposure. On physical examination we observed excoriations on the lateral side of the right arm (Figure 1). The patient also complained of right brachial paresis. Computed tomography of the cervical spine, magnetic resonance imaging and electromyography of the brachial plexus showed right cervical disc herniation with nerve root compression of C6-C7 and right brachial plexus inflamation (Parsonage-Turner syndrome) attributed to neoplastic infiltration of multiple myeloma. A skin biopsy on the right arm demonstrated a nonspecific superficial dermatitis (Figure 2).
FIGURE 1.

Ulcerated erythematous papules on the lateral aspect of the right arm suggestive of scratching
FIGURE 2.
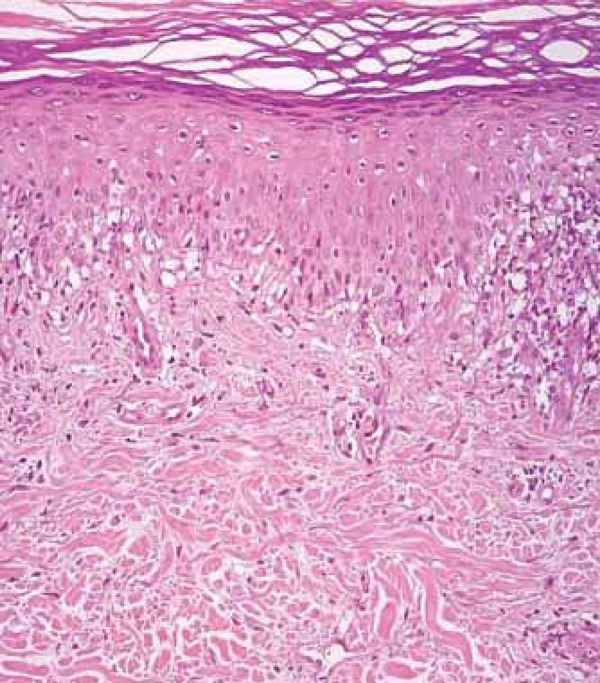
Superficial lymphocytic non-specific dermatitis (H&E, 10x)
In this context, we assumed the diagnosis of BP consequent to the described nerve lesions (cervical disc herniation and Parsonage-Turner syndrome).
The patient was treated with methylprednisolone aceponate cream 0.1% and oral hydroxyzine 25mg every 8 hours, which resulted in little improvement of the pruritus. Consequently, gabapentin was introduced at 900 mg/day, achieving optimal control after 3 months of follow-up. The patient was also referred to neurosurgery and oncology consultation for additional therapeutic orientation.
DISCUSSION
BP has multifactorial etiology and its pathophysiological mechanism remains unknown. A decrease of intraepithelial nerve fibers was observed in patients with intense brachioradial pruritus in the context of prolonged exposure to sunlight and / or disorders of the cervical innervation.5.6
Corticosteroids and antihistamines are often ineffective. Capsaicin cream 0.025% can be effective, but with frequent relapses. Oral gabapentin (900 mg to 3600mg) has been used with encouraging results.7.8 Other treatments include mirtazapine, selective serotonin reuptake inhibitors and thalidomide with variable degrees of response.9
In the presented case, the investigation of BP led to a diagnosis of two different entities with specific therapeutic orientation (cervical disc herniation with nerve root compression requiring neurosurgical intervention and Parsonage-Turner syndrome with neoplastic infiltration of multiple myeloma for oncological treatment). The authors suggest cervical spine lesion be ruled out in all patients with BP.
Footnotes
Financial Support: None.
Conflict of Interest: None.
How to cite this article: Carvalho S, Sanches M, Alves R, Selores M. Brachioradial pruritus in a patient with cervical disc herniation and Parsonage-Turner syndrome. An Bras Dermatol. 2015; 90(3):401-2.
Work performed at the Dermatology and Venereology Service, Centro Hospitalar do Porto, Portugal
Reference
- 1.Oaklander AL. Neuropathic itch. Semin Cutan Med Surg. 2011;30:87–89. doi: 10.1016/j.sder.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oaklander AL. Common Neuropathic itch syndromes. Acta Derm Venereol. 2012;92:118–125. doi: 10.2340/00015555-1318. [DOI] [PubMed] [Google Scholar]
- 3.Waisman M. Solar pruritus of the elbows (brachioradial summer pruritus) Arch Dermatol. 1968;98:481–485. [PubMed] [Google Scholar]
- 4.Heyl T. Brachioradial pruritus. Arch Dermatol. 1983;119:115–116. [PubMed] [Google Scholar]
- 5.Veien NK, Laurberg G. Brachioradial pruritus: a follow-up of 76 patients. Acta Derm Venereol. 2011;91:183–185. doi: 10.2340/00015555-1006. [DOI] [PubMed] [Google Scholar]
- 6.Goodkin R, Wingard E, Bernhard JD. Brachioradial pruritus: cervical spine disease and neurogenic pruritus. J Am Acad Dermatol. 2003;48:521–524. doi: 10.1067/mjd.2003.203. [DOI] [PubMed] [Google Scholar]
- 7.Greaves MW. Recent advances in pathophysiology and current management of itch. Ann Acad Med Singapore. 2007;36:788–792. [PubMed] [Google Scholar]
- 8.Steinhoff M, Cevikbas F, Ikoma A, Berger TG. Pruritus: Management, Algorithms and Experimental Therapies. Semin Cutan Med Surg. 2011;30:127–137. doi: 10.1016/j.sder.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pereira JM. Brachioradial pruritus treated with thalidomide. An Bras Dermatol. 2005;80:295–296. [Google Scholar]


