Abstract
Milker's nodule is an occupational viral skin disease of universal distribution, caused by the Paravaccinia virus and that occurs in individuals who deal with dairy cattle herds. We describe a case acquired due to lack of use of PPE (Personal Protective Equipment) and perform a literature review.
Keywords: Orf vírus, Parapoxvirus, Pseudocowpox virus
INTRODUCTION
Occupational dermatoses are produced or aggravated by agents present where professional activity is performed. We describe here a dermatosis caused by the Paravaccinia virus, acquired on the job site due to lack of use of PPE.
CASE REPORT
Female patient, 55 years old, dentist, born and raised in Rio de Janeiro, complaining about a "hand lesion". She reported the onset of an erythematous lesion on the side of right hand, of centrifugal growth, asymptomatic, 13 days before. She did not associate any triggering factor, denied local trauma and/or insect bite. She used ketoconazole, betamethasone, mupirocin on her own - without improvement of symptoms. She presented hypothyroidism (using levothyroxine), arrhythmia (using propafenone) and denied other comorbidities/allergies, smoking and/or drinking.
At the dermatological examination we observed a nodular lesion, erythematous-purplish, round, of clear center, depressed and with an erythematous halo of approximately 2.5 cm in diameter (Figures 1 and 2).
FIGURE 1.

Side of right hand. Nodular, erythematous-purplish lesion, with round, clear center and erythematous halo of approximately 2.5 cm in diameter
FIGURE 2.
Milker’s nodule. Evolution of lesion on side of right hand. A) exudative nodule – 13 days of evolution. B) regenerative stage – 24 days of evolution. C) papillomatous stage – 32 days of evolution. D) remission stage, erythematous macule with circular purplish areas (biopsy sites) – 41 days of evolution
After evaluating the lesion we asked the patient again about her hygiene habits and if she had had contact with bovines and ovines. She said she was not practicing the dental profession, but that she worked in her farm where she vaccinated cattle and manipulated cutting/perforating materials without the use of PPE (Personal Protective Equipment).
In view of this picture and the patient's professional history, the hypotheses were: milker's nodule, brown spider bite, pyoderma and cutaneous tuberculosis.
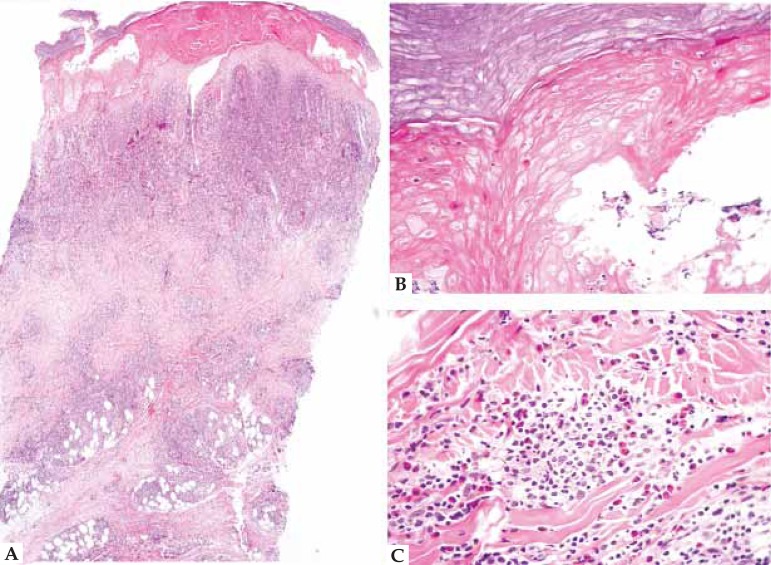
We punctured the lesion and sent the material for culture and direct examination, with a negative result for bacteria and fungi. Biopsies were performed and one fragment was sent for fungi and bacteria culture which also resulted negative; another was sent for histopathological examination, which demonstrated squamous crusts, acanthosis, epidermal necrosis, vesiculae formation, keratinocyte apoptosis and ballooning degeneration, deep and superficial dense dermal inflammatory infiltrate (up to the panicle), mononuclear and rich in eosinophils (Figure 3). Laboratory tests presented no alterations.
FIGURE 3.
Histopathology – Milker’s nodule. A) Squamous crust, acanthosis, deep and superfi cial mononuclear dense dermal infl ammatory infi ltrate (up to panicle). B) necrosis of epidermis, formation of vesiculae and apoptotic keratinocytes. C) Mononuclear diffuse infi ltrate rich in eosinophils
Thus we concluded the diagnosis as Milker's nodule.
Since the disease is self-limited, the conduct was expectant and we gave general guidelines about care that should be taken with infected cattle.
DISCUSSION
Milker's nodule, also called pseudocowpox virus, is the infection caused by the Paravaccinia virus, a DNA virus of the genus Parapoxvirus and poxvirus family. 1-4
It is considered an occupational viral skin disease of universal distribution (occupational dermatoses are the ones produced or aggravated by agents present where professional activity is performed) which occurs in individuals who manage dairy cattle 1,5, whether by touching infected udder or noses of cows, or those who manipulate meat and/or contaminated objects.1,L4
The disease presents a period of incubation from 5 to 15 days and the number of lesions varies from one to five, 1,3,4 involving mainly the hands and forearms, although it may also occur on the face. 1,4 The clinical picture is asymptomatic and rarely presents fever, lymphadenopathy and erythema multiforme. The most common occurrence is secondary bacterial overgrowth.4,5
Through histopathology we observed hyperkeratosis and acanthosis of epidermis, multilocular vesicles, reticular degeneration and ballooning of the upper third cells of epidermis. Eosinophilic and intracytoplasmic inclusion bodies are characteristic but are not present in all evolution phases. In the dermis we have a mononuclear and eosinophils inflammatory infiltrate.1,3,4
The diagnosis is based on the epidemiologic history, dermatological and histopathological examination. It may be more permanently established by the demonstration of viral particles by electron microscopy, by reproduction of virus in tissue culture, PCR technique or by demonstrating neutralizing antibodies for the vaccinia group in the patient's serum.1,3
The differential diagnosis is done with Orf, brown spider bite, anthrax, sporotrichosis, pyoderma, atypical mycobacteriosis and cowpox, among other diseases. 1-5
Milker's nodule and Orf are very similar diseases but caused by different viruses, although from the same family and genus. Furthermore, the host of Milker's nodule is bovine cattle while goats and sheep host Orf (Chart 1). 1,6,7,8
CHART 1.
Differences between Milker's nodule and Orf
| Milker's nodule | ORF | |
|---|---|---|
| Virus | Paravaccinia virus | Orf |
| Genus | Parapoxvirus | |
| Family | Poxvirus | |
| Host | Bovine cattle | Goats, sheep |
Both evolve clinically in six typical stages, lasting an average of six days each. They start with an erythematous maculopapular lesion which evolves to a target lesion with central ulceration and then to a exudative nodule. It goes through a dry regenerative stage with dark spots, a papillomatous stage and finally remiss spontaneously with a dry crust, leaving no scars (Figure 2). 1,3,6-8
Another important differential diagnosis due to biological wars and bioterrorism is anthrax.3
In addition to the fact that the disease is self-limited, follow-up is expectant and sequential until remission of clinical picture. General guidelines should be given regarding dealing with infected cattle. Milker's nodule provides the host with immunity.1,3,4 We believe that the number of cases is greater than found in literature; as the disease is self-limited, many do not seek medical help, making it appear relatively infrequent. It is important to emphasize the importance of a detailed anamnesis and remember that "we only think of what we know".
Footnotes
Financial Support: None.
Conflict of Interest: None.
How to cite this article Adriano AR, Quiroz CD, Acosta ML, Jeunon T, Bonini F. Milker’s nodule - Case report. An Bras Dermatol. 2015; 90(3):407-10.
Work performed at Instituto de Dermatologia Professor Rubem David Azulay - Santa Casa da Misericórdia do Rio de Janeiro (IDPRDA - SCMRJ) – Rio de Janeiro (RJ), Brazil.
Reference
- 1.Paredes O, Garcia R, Figueroa Y. Nódulo de los ordeñadores. Folia Dermatol. 2006;17:133–136. [Google Scholar]
- 2.Slattery WR, Juckett M, Agger WA, Radi CA, Mitchell T, Striker R. Milkers' nodules complicated by erythema multiforme and graft-versus-host disease after allogeneic hematopoietic stem cell transplantation for multiple myeloma. Clin Infect Dis. 2005;40:e63–e66. doi: 10.1086/428619. [DOI] [PubMed] [Google Scholar]
- 3.Werchniak AE, Herfort OP, Farrell TJ, Connolly KS, Baughman RD. Milker's nodule in a healthy young woman. J Am Acad Dermatol. 2003;49:910–911. doi: 10.1016/s0190-9622(03)02115-7. [DOI] [PubMed] [Google Scholar]
- 4.Sartori-Barraviera SRC, Marques AS, Stolf HO, Silvares MRC, Marques MEA. Nódulo dos ordenhadores: relato de dez casos. An Bras Dermatol. 1997;72:477–480. [Google Scholar]
- 5.Batalla A, Álvarez-Argüelles ME, González-Martinéz MB, Curto JR. Nódulo de los ordeñadores complicado com eritema multiforme. Med Clin (Barc) 2013;141: doi: 10.1016/j.medcli.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Human Orf virus infection from household exposures - United States, 2009-2011. MMWR Morb Mortal Wkly Rep. 2012;61:245–248. [PubMed] [Google Scholar]
- 7.Hosie B. Orf: reasons to take an interest in control. Vet Rec. 2012;170:671–672. doi: 10.1136/vr.e4335. [DOI] [PubMed] [Google Scholar]
- 8.Dulcan AG. Milkers' Nodules. Can Med Assoc J. 1957;77:339–342. [PMC free article] [PubMed] [Google Scholar]