Abstract
Objective
Type 1 diabetes remains a significant source of premature mortality; however, its burden has not been assessed in the U.S. Virgin Islands (USVI). As such, the objective of this study was to estimate type 1 diabetes mortality in a population-based registry sample in the USVI.
Research Design and Methods
We report overall and 20-year mortality in the USVI Childhood (<19 years old) Diabetes Registry Cohort diagnosed 1979-2005. Recent data for non-Hispanic blacks from the Allegheny County, PA population-based type 1 diabetes registry were used to compare mortality in the USVI to the contiguous US.
Results
As of December 31, 2010, the vital status of 94 of 103 total cases was confirmed (91.3%) with mean diabetes duration 16.8 ± 7.0 years. No deaths were observed in the 2000-2005 cohort. The overall mortality rates for those diagnosed 1979-1989 and 1990-1999 were 1852 and 782 per 100,000 person-years, respectively. Overall cumulative survival for USVI was 98% (95% CI: 97-99) at 10 years, 92% (95% CI: 89-95) at 15 years and 73% (95% CI: 66-80) at 20 years. The overall SMR for non-Hispanic blacks in the USVI was 5.8 (95% CI 2.7-8.8). Overall mortality and cumulative survival for non-Hispanic blacks did not differ between the USVI and Allegheny County, PA.
Conclusions
This study, as the first type 1 diabetes mortality follow-up in the USVI, confirmed previous findings of poor disease outcomes in racial/ethnic minorities with type 1 diabetes.
Introduction
Unlike type 2 diabetes, where prevention is possible, (1) type 1 diabetes is currently a lifelong incurable metabolic disorder. Despite increased access to treatment, improved disease management, and successful reduction of complications through intensive therapy, (2) the major complications of type 1 diabetes (retinopathy, nephropathy, neuropathy, and cardiovascular disease) persist as significant sources of morbidity and early mortality. (3) Prior mortality studies estimate type 1 diabetes mortality in the U.S. to be 5-7 times higher than the general population (4); higher than estimates in other developed nations. (5-6) Recent reports from the Allegheny County population-based registry indicated that type 1 diabetes mortality has improved in recent decades and the proportion of deaths due to often preventable acute complications has greatly decreased. (7-8) Researchers also confirmed that African-Americans with type 1 diabetes were at a nearly 2.5-fold increased risk of premature death compared to Caucasians, as shown in several earlier studies. (9-12) Roy et al also reported long-term type 1 diabetes mortality to be 6-12 times higher in an all-African-American cohort compared to the general population. (13) Thus, further assessment and understanding of the mortality associated with type 1 diabetes in non-Hispanic blacks is critical. The United States Virgin Islands (USVI), a predominantly non-Hispanic black population, provides an ideal population. Diabetes has risen to the fourth leading cause of death in the USVI (14); however, the mortality and survival associated specifically with type 1 diabetes has yet to be evaluated and is of concern as the incidence of type 1 diabetes in the USVI has risen over the past 30 years to levels higher than anticipated based on worldwide estimates. (15-16)
We thus investigated mortality rates in a population-based childhood onset type 1 diabetes cohort in the USVI with a mean follow-up of 16.8 years to assess trends in mortality by race, sex, age of diagnosis, and year of type 1 diabetes diagnosis and to compare rates to the non-Hispanic black cohort of the Allegheny County type 1 diabetes Registry, a U.S. population-based registry.
Methods
Study Population
The USVI Childhood Diabetes Registry cohort includes any individual diagnosed with diabetes before age 19 and living in the territory at the time of diagnosis between January 1, 1979 and December 31, 2005. (17) Cases were ascertained through retrospective review of medical records at all hospitals and community health clinics. Individuals were excluded if pregnant (likely gestational diabetes) or not a USVI resident. Diabetes type was determined by health professional diagnosis. The registry cohort is composed of a total of 103 eligible type 1 diabetes cases from all three islands (St. Croix, St. Thomas, and St. John).
The Allegheny County type 1 diabetes Registry (n=1,075) has been described in detail, (18) and consists of all individuals diagnosed with childhood-onset (age<18 years) type 1 diabetes in Allegheny County, PA between 1 January 1965 and 31 December 1979, and placed on insulin at diagnosis. Individuals were identified via hospital record review and validated by contacting pediatricians throughout the county (ascertainment>95%). (19) Children developing diabetes from a secondary cause (i.e., cystic fibrosis, Down's syndrome, or steroid-induced diabetes) were excluded. This cohort has been part of a comparative international study (Diabetes Epidemiology Research International, DERI) of type 1 diabetes mortality rates and was selected in this study as a proxy for type 1 diabetes mortality in the U.S. (20) Notably, the registry is composed of 7.5% African-Americans.
Vital Status
Vital status for the USVI registry was ascertained as of December 31, 2010, by first contacting all participants via postal mail and telephone to update registry contact information. When participants were not contactable via telephone or mail, attempts were made to contact family members listed in the registry via telephone. Finally, telephone books and internet search engines were used to identify updated contact information for participants.
The USVI Territorial Death Index, the U.S. Social Security Death Index (SSDI), and the National Death Index (NDI) were then searched to confirm possible deaths among non-contacted participants. Death certificates were obtained from the USVI Bureau of Vital Statistics for all deaths occurring within the territory. NDI data was ascertained for all deaths occurring outside of the territory, to determine cause of death.
Vital status for the Allegheny County type 1 diabetes Registry was ascertained as of January 1 2008. Similarly, all participants were contacted initially by letter, then by telephone if necessary, to complete a brief health update questionnaire. The study protocol was approved by the University of Pittsburgh Institutional Review Board.
Statistical Analysis
Student's t-test and one-way ANOVA were used to compare continuous variables across groups (sex, race, and diagnosis cohort), adjusting for multiple comparisons using the Bonferroni correction. The χ2 (or Fisher's exact) test was used to compare categorical variables between groups. Diagnosis year was categorized into three groups, based on decade (1979–1989, 1990–1999, and 2000-2005) to assess temporal trends in overall mortality. Age at diagnosis was categorized as pre-pubertal (<10 yrs), peri-pubertal (10-14 yrs), and post-pubertal (>14 yrs). Race was categorized as non-Hispanic white (NHW), non-Hispanic black (NHB), and Hispanic (H), based on race abstracted from the USVI Childhood Diabetes Registry. Mortality rates were estimated using person-years method, and 95% CIs were determined using the Poisson distribution. Non-Hispanic whites were not included in the analysis, because no deaths have occurred to date. Each individual's person-years contribution was calculated from the date of diagnosis to the December 31, 2010, date of death, of the date of last follow-up. Life-table analyses by the Kaplan-Meier method were performed. Log-rank test was used to determine the statistical difference between survival curves. Age- and sex-adjusted standardized mortality ratios (SMRs) were calculated as the observed divided by the expected number of deaths in each age, and sex category for non-Hispanic Blacks. Expected mortality was calculated using population life tables for USVI, obtained from the USVI Department of Health Bureau of Vital Statistics. (21) Background mortality rates covering the same period were used. SMRs were not calculated for Hispanics due to the lack of population life tables for Hispanics in the USVI. 95% CIs were determined with the Poisson distribution. Mortality rates and SMRs were compared using rate ratio (RR) analyses and calculating 95% CIs. (22) Multivariate Cox proportional hazard models were used to assess the effects of sex, race, age at onset and year of diagnosis on mortality. Twenty (20)-year mortality rates in NHBs in the USVI cohort were compared to all-cause mortality rates in NHBs in the Allegheny County population-based type 1 diabetes registry cohort, as a proxy for the contiguous US. Statistical significance was considered as a p-value less than 0.05. Analyses were completed using SPSS 18.0 (SPSS, Inc.) and SAS 9.2 (SAS, Inc.).
Results
As of December 31, 2010, the vital status of 94 of the 103 total cases was confirmed (91.3%). There were no statistical differences in the proportion of males (46.9% male vs. 50.1% male) or mean age at onset (11.5 ± 4.4 vs. 11.0 ± 2.4) in the unverified sample, compared to the verified sample. Non-Hispanic blacks (94.7%) and Hispanics (90%) had similar proportions traced. However, individuals diagnosed 1979-1989 (80.6%) were less likely to be traced compared to the 1990-1999 (95.6%) and 2000-2005 (100.0%) cohorts (p=.04). Demographic characteristics and overall mortality rates of the USVI type 1 diabetes cohort are shown by sex, race, and year of diagnosis in Table 1.
Table 1. Demographic Characteristics and Overall Mortality of USVI Type 1 Diabetes Registry Cohort (1979-2005) by Sex, Race, and Year of Diagnosis.
| Sex | Race | Year of Diagnosis | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Male* | Female | Non-Hispanic Black* | Non-Hispanic White | Hispanic | 1979-1989* | 1990-1999 | 2000-2005 | ||
| n | 49 | 54 | 77 | 6 | 20 | 36 | 45 | 22 | 103 |
| Follow-up | 89.8 (44) | 92.6 (50) | 94.7 (72) | 50 (3) | 90 (18) | 80.6 (29) | 95.6 (43) | 100.0 (22)† | 91.3 |
| Male | -- | -- | 48.1 (37) | 66.7 (4) | 40.0 (8) | 55.6 (20) | 44.4 (20) | 40.9 (9) | 47.6 (49) |
| Age of diagnosis (years) | 10.9 ± 4.7 | 11.7 ± 4.4 | 11.6 ± 4.7 | 8.8 ± 2.4 | 11.1 ± 4.5 | 10.9 ± 4.4 | 11.2 ± 5.2 | 12.4 ± 3.2 | 11.3 ± 4.5 |
| Mean diabetes duration (years) | 17.5 ± 7.2 | 16.1 ± 6.9 | 16.7 ± 7.0 | 23.8 ± 2.7 | 15.4 ± 7.0 | 24.3 ± 4.2 | 15.2 ± 3.0‡ | 7.5 ± 1.5‡ | 16.8 ± 7.0 |
| Mean Age (years) | 28.4 ± 7.3 | 27.8 ±7.8 | 28.3 ± 7.4 | 32.6 ± 4.5 | 26.5 ± 8.6 | 35.2 ±5.2 | 26.4 ± 5.3† | 19.9 ±3.3‡ | 28.2 ± 7.5 |
| Diagnosis Cohort | |||||||||
| 1979-1989 | 40.8 (20) | 29.6 (16) | 31.2 (24) | 83.3 (5) ‡ | 35.0 (7)† | -- | -- | -- | 35.0 (36) |
| 1990-1999 | 40.8 (20) | 46.3 (25) | 48.1 (37) | 16.7 (1) † | 35.7 (7) | -- | -- | -- | 43.7 (45) |
| 2000-2005 | 18.4 (9) | 24.1 (13) | 20.8 (16) | -- | 30.0 (6) | -- | -- | -- | 21.4 (22) |
| Race | |||||||||
| Non-Hispanic Black | 8.2 (4) | 3.7 (2) | -- | -- | -- | 66.7 (24) | 80.0 (36) | 72.7 (16) | 5.8 (6) |
| Non-Hispanic White | 75.5 (37) | 74.1 (40) | -- | -- | -- | 13.9 (5) | 2.2 (1) | -- | 74.8 (77) |
| Hispanic | 16.3 (8) | 22.2 (12) | -- | -- | -- | 19.4 (7) | 15.6 (7) | 27.3 (6) | 19.4 (20) |
| Deaths | 20.4 (10) | 13.0 (7) | 18.2 (14) | 0 (0) | 15.0 (3) | 33.3 (12) | 11.1 (5) | 0 (0) | 16.5 (17) |
| Person-years of follow-up§ | 693.9 | 758.6 | 1200.0 | -- | 252.5 | 648.5 | 639.0 | 165.0 | 1452.5 |
| Overall Mortality Rate (95% CI) | 1441 (775, 2678) | 922 (440, 1936) | 1167 (691, 1970) | -- | 1188 (383, 3684) | 1852 (976, 3026) | 782 (326, 1879) | -- | 1170 (727, 1883) |
Data are % (n) or means ± SD.
p<0.05;
p<0.01
Denotes reference category
Excludes non-Hispanic whites.
The overall mortality rate was 1170 per 100,000 person-years (95% CI 727, 1883). There were no significant differences in overall mortality by sex, race, diagnosis cohort or age of onset in the USVI.
Results from Cox regression modeling showed that sex, race, and year of diagnosis were not significant and were not included in the final model. Age at onset, categorically and continuously, was the only significant predictor of mortality in the cohort. Individuals diagnosed after the age of 14 had a 9-fold increased risk of mortality compared to those diagnosed prior to age 10 (95% CI 2.0-42.3). The 10-14 age group had a nearly 3-fold increased risk, though not significant (95% CI 0.5-15.8). Each additional year in age at onset increased risk of mortality by 23% (hazard ratio – 1.2, 95% CI 1.1-1.4).
The 20-year mortality rates by sex, diagnosis year, and age of diagnosis for NHBs in the USVI and Allegheny County are shown in Table 2. The 20-year mortality rate in NHBs did not differ between the USVI and Allegheny County cohorts (p=.23). The overall SMRs are also shown in Table 2. The overall SMR for non-Hispanic blacks in USVI was 5.8 (95% CI 2.7-8.8). There were no differences based on sex, diagnosis cohort, or age of diagnosis; however the SMR was highest for the 1979-1989 cohort (8.1, 95% CI 3.1-13.1) and for the >14 diagnosis age group (8.7, 95% CI 2.3-15.1). The SMR seemed to increase gradually by age of diagnosis; however this pattern was not observed in Allegheny County, with the highest SMR occurring in the <10 age group.
Table 2. 20-year Mortality Rates (per 100,000 person-years) and Overall Standardized Mortality Ratios (SMRs) by Gender, Diagnosis Cohort, and Diagnosis Age in Non-Hispanic Blacks in the USVI and Allegheny County (1965-1979).
| USVI (1979-2005) (N=72) | Allegheny County (1965-1979) (N=79) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Deaths % (n) | Follow-up time (person-years) | Mortality Rate (95% CI) | SMR (95% CI) | Deaths % (n) | Follow-up time (person-years) | Mortality Rate (95% CI) | SMR (95% CI) | |
| Overall | 12.5 (9) | 1095.2 | 822 (428, 1579) | 5.8 (2.7, 8.8) | 10.0 (8) | 1522.9 | 525 (263, 1050) | 7.5 (5.2, 9.8) |
| Gender | ||||||||
| Male | 11.8 (4) | 524.9 | 762 (286, 2030) | 6.0 (1.5, 10.4) | 6.1 (2) | 671.8 | 298 (74, 1190) | 4.0 (2.0, 6.0) |
| Female | 13.2 (5) | 570.3 | 877 (365, 2106) | 5.5 (1.4, 9.6) | 13.3 (6) | 851.1 | 705 (316, 1569) | 15.6 (9.5, 21.7) |
| Diagnosis Year | ||||||||
| 1965-1969 | 17.9 (5) | 510.4 | 980 (408, 2354) | 10.0 (5.5, 14.5) | ||||
| 1970-1974 | 4.0 (1) | 498.8 | 201 (28, 1423) | 7.1 (3.1, 11.2) | ||||
| 1975-1979 | 8.7 (2) | 513.7 | 389 (97, 1557) | 5.1 (1.8, 8.4) | ||||
| 1979-1989 | 22.7 (5) | 426.8 | 1171 (487, 2815) | 8.1 (3.1, 13.1) | ||||
| 1990-1999 | 11.8 (4) | 548.1 | 729 (274, 1944) | 3.2 (1.0, 6.3) | ||||
| 2000-2005 | -- (0) | -- | -- | -- | ||||
| Age at Onset | ||||||||
| <10 years | 4.8 (1) | 354.5 | 282 (40, 2003) | 2.6 (0, 5.6) | 13.0 (3) | 427.0 | 703 (227, 2178) | 6.0 (1.8, 10.1) |
| 10-14 years | 6.9 (2) | 404.9 | 494 (124, 1975) | 5.5 (1.1, 10.9) | 6.9 (2) | 629.2 | 318 (79, 1271) | 9.1 (4.9, 13.4) |
| >14 years | 26.0 (6) | 335.8 | 1787 (803, 3977) | 8.7 (2.3, 15.1) | 12.5 (3) | 466.7 | 643 (207, 1993) | 6.9 (3.3, 10.5) |
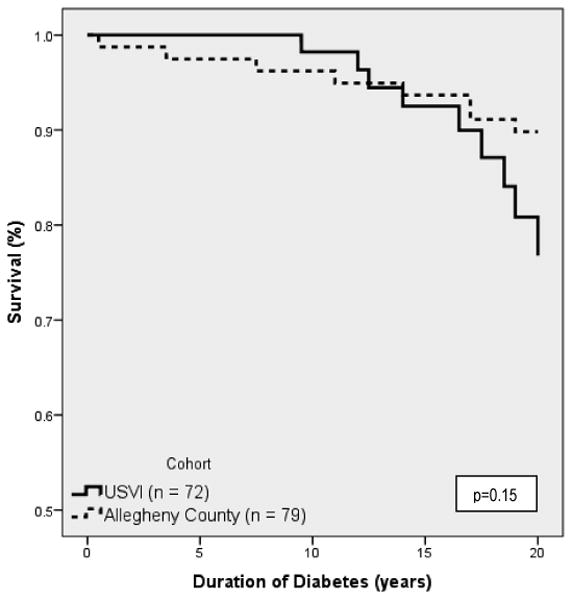
Overall, cumulative survival in the USVI (not shown) was 98% (95% CI: 97-99) at 10 years, 92% (95% CI: 89-95) at 15 years and 73% (95% CI: 66-80) at 20 years. Survival curves up to 20 years duration for the non-Hispanic blacks in USVI and Alleghany County are shown in Figure 1. Cumulative survival for NHBs in USVI was 98% (95% CI: 96-100) at 10 years, 93% (95% CI: 89-97) at 15 years and 77% (95% CI:70-85) at 20 years. Cumulative survival at 20 years was not significantly different between non-Hispanic blacks in Allegheny County (91% 95% CI: 84-98) compared to the USVI cohort.
Figure 1. Life-Table Analysis Overall in Non-Hispanic Blacks in USVI (1979-2005) vs. Allegheny County (1965-1979).
Discussion
This study, for the first time, evaluated mortality in a population-based type 1 diabetes cohort in the USVI and compared the effects of race, sex, age of diagnosis, and calendar year period of diagnosis on survival. These data appear to reveal a major impact of age at onset on mortality, such that a post-pubertal onset increases mortality 9-fold. Recent data from the Allegheny County, Pennsylvania population-based registry cohort were also used to compare the mortality experience in the USVI to that of a county in the contiguous United States. Notably, there were no significant difference in 20-year mortality or survival for non-Hispanic blacks in the USVI cohort compared to non-Hispanic blacks in the Allegheny County, PA cohort, which may suggest a similar mortality experience for non-Hispanic blacks across the different geographic locations. In accordance with reports from Allegheny County cohort (5,7) and other studies (13, 23) that have shown higher mortality in individuals with type 1 diabetes compared to the general population, mortality for non-Hispanic blacks with type 1 diabetes in the USVI was 5.8 (95% C.I. 2.7-8.8) times higher than the general USVI non-Hispanic black population. This SMR was similar to that of non-Hispanic blacks in the Allegheny County cohort (SMR: 7.5 (95% C.I. 5.2-9.8)).
In addition, poorer outcomes in non-Hispanics blacks with type 1 diabetes may also be associated with poor socioeconomic status and other environment factors, including access to care. The SEARCH Study found that non-Hispanic black youth diagnosed with type 1 diabetes had poorer socioeconomic profiles, and were more likely to be uninsured or utilizing public insurance. (24) In concert, the USVI has high rates of poverty and uninsured, coupled with a significantly high cost of living, which results in poor overall socioeconomic conditions. (25) The poor socioeconomic conditions impact the entire population, with and without diabetes, but are likely to still be associated with poor prognosis and increased mortality in type 1 diabetes, (26) and would not be detected in the SMR.
Mortality between non-Hispanic blacks and Hispanics did not differ, but the sample size of the latter precludes further analysis. Regrettably, apart from this study, there is no long-term follow-up of mortality in Hispanics with type 1 diabetes in the literature.
No sex differences in mortality for men and women was observed in the USVI, consistent with several previous studies,(4, 13, 28) but not all (6, 27) In the New Jersey 725 Study there were no significant differences in mortality for men and women; however the SMR for women was significantly higher than for men (10.5 vs 7.0). (13) This difference was not observed in the USVI, as SMRs for men and women were virtually identical (6.0 vs 5.5); however, a difference was seen in the Allegheny County cohort, where females had a nearly 4-fold increased SMR compared to males (4.0 vs. 15.6). This may be attributed to the smaller sex gap in overall mortality seen in the general non-Hispanic black population in the USVI compared to Allegheny County and New Jersey.
In contrast to the overall Allegheny County cohort and other studies abroad (6, 28), no temporal improvement in mortality was observed in the USVI, as there were no significant differences in mortality based on diagnosis cohort. Importantly, follow-up was worse for the earlier diagnosis cohort (80.6% vs 95.6%). As such, we evaluated the mortality and survival, applying the same mortality in the traced individuals to the untraced individuals, as well as estimated mortality assuming that all untraced individuals were deceased, and mortality (p-values: 0.27, 0.21) and survival (p-values: 0.62, 0.41) still did not significantly differ. Notably, in Allegheny County, there was also no significant temporal improvement in mortality for non-Hispanic blacks, as survival did not differ across diagnosis year cohorts. Similarly, overall mortality did not differ between diagnosis cohorts in the USVI. While this may partly be an artifact of the small sample size, it is plausible that there has been no temporal improvement in mortality in the USVI. While disease recognition, care and treatment have improved, there are still major gaps in access to specialized diabetes care and treatment. There are few endocrinologists currently practicing in the territory, and none specializing in pediatrics. (29) There is also minimal access to diabetes educators to provide additional training to patients and families. As a result, families often seek care in neighboring territories or stateside; however, this is limited to those financially advantaged families, as this is often not covered by medical insurance providers and in cases where coverage is provided, travel expenses remain the burden of the individual family.
Age of diagnosis was the only significant predictor of mortality in the USVI. This difference also seemed to occur specifically in non-Hispanic blacks, as 20-year mortality increased by 4.5-fold between the <10 age group and the >14 age group; this difference was significant. The overall SMRs also seemed to follow a similar pattern as the SMR in the <10 age group was 2.6, compared 8.7 in the >14 age group (not significant). This pattern was not observed in non-Hispanic blacks in Allegheny County, where the SMRs did not differ dramatically across diagnosis age groups. Other studies have shown higher mortality rates in individuals diagnosed during and after puberty, compared to those diagnosed before puberty. (4, 6, 27, 30) While the factors associated with this increased risk remain unclear, and it is possible that care-related factors play a role (e.g. resistance to self-management and compliance by maturing adolescents). In addition, there is some evidence that suggests that the earliest years of type 1 diabetes (pre-puberty) are largely free of complications, and as such, the pattern seen may be an effect of age, as opposed to a true difference in mortality.
The major limitation of this present study is the small sample size and as a result no confirmed deaths were seen in non-Hispanic whites. This prohibited racial comparisons between non-Hispanic whites and other race groups in the USVI. However, based on survival estimates for non-Hispanic whites in Allegheny County, PA, we would expect 92% survival at 24-years duration (mean duration of non-Hispanic whites in USVI), which equates to only .48 expected deaths. Another limitation of the study is that the living status of 8.7% of participants was not determined. Nonetheless, the likelihood of death in these individuals is low, as the USVI Territorial Death Index, Social Security Death Index, and National Death Index were all searched for these individuals. The comparison made to the Allegheny County sample has several limitations for consideration, including: 1. Cultural variations between populations (i.e demographics, culture, access to care, etc. 2. Temporal variations between samples (i.e. AC sample was diagnosed 1965-1979, compared to USVI, 1989-2005). A final limitation for consideration is the impact of migration from the USVI to the contiguous US on the interpretation of these results specific to factors in the USVI. Approximately 35% of deaths occurred outside of the USVI; however, some of this is accounted for by individuals seeking ambulatory care stateside.
In conclusion, this is the first population-based type 1 diabetes mortality follow-up in the USVI and Caribbean region. This study confirms previous findings of poor disease outcomes in racial/ethnic minorities with type 1 diabetes, particularly if diagnosed after puberty. Mortality outcome seems comparable to Allegheny County non-Hispanic blacks. Continued follow-up and efforts to improve disease management and access to care in the USVI are critical.
Acknowledgments
REW was supported by a research supplement from the National Institute of Diabetes and Digestive and Kidney Diseases (R37-DK-034818-26W1).
Guarantor: REW
We would like to thank the U.S. Virgin Islands Childhood Diabetes Registry participants and the staff of USVI Bureau of Vital Statistics for their support.
Footnotes
All authors (REW, TJO, VCA, REL, AMS, EST) have no potential conflicts of interest.
REW researched data and wrote the manuscript, TJO contributed to the discussion and reviewed/edited the manuscript, VCA contributed to the data analysis and discussion, and reviewed/edited the manuscript, REL contributed to the discussion and reviewed/edited the manuscript, AMS provided data and analysis for the Allegheny County cohort and reviewed/edited the manuscript, EST researched data, contributed to the discussion and reviewed/edited the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Knowler WC, Barrett-Connor E, Fowler SE. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DCCT Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin dependent diabetes mellitus. N Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 3.Pambianco G, Costacou T, Ellis D, Becker D, Klein R, Orchard T. The 30-Year Natural History of Type 1 diabetes Complications: The Pittsburgh Epidemiology of Diabetes Complications Study Experience. Diabetes. 2005;55:1463–1469. doi: 10.2337/db05-1423. [DOI] [PubMed] [Google Scholar]
- 4.Dorman JS, Tajima N, LaPorte RE, Becker DJ, Cruickshanks KJ, Wagener DK, Orchard TJ, Drash AL. The Pittsburgh insulin-dependent diabetes mellitus (IDDM) morbidity and mortality study. Mortality results. Diabetes. 1984;33(3):271–276. doi: 10.2337/diab.33.3.271. [DOI] [PubMed] [Google Scholar]
- 5.Nishimura R, LaPorte RE, Dorman JS, Tajima N, Becker D, Orchard TJ. Mortality trends in type 1 diabetes. The Allegheny County (Pennsylvania) Registry 1965-1999. Diabetes Care. 2001;24(5):823–827. doi: 10.2337/diacare.24.5.823. [DOI] [PubMed] [Google Scholar]
- 6.Skrivarhaug T, Bangstad HJ, Stene LC, Sandvik L, Hanssen KF, Joner G. Long-term mortality in a nationwide cohort of childhood-onset type 1 diabetic patients in Norway. Diabetologia. 2006;49(2):298–305. doi: 10.1007/s00125-005-0082-6. [DOI] [PubMed] [Google Scholar]
- 7.Secrest AM, Becker DJ, Kelsey SF, LaPorte RE, Orchard TJ. All-cause mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes: the Allegheny County type 1 diabetes registry. Diabetes Care. 2010;33(12):2573–2579. doi: 10.2337/dc10-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Secrest AM, Becker DJ, Kelsey SF, Laporte RE, Orchard TJ. Cause-specific mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes The Allegheny County Type 1 diabetes Registry. Diabetes. 2010 doi: 10.2337/dc10-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tull ES, Barinas E. A twofold excess mortality among black compared with white IDDM patients in Allegheny County, PA. Diabetes Care. 1996;19(12):1344–47. doi: 10.2337/diacare.19.12.1344. [DOI] [PubMed] [Google Scholar]
- 10.Lipton R, Good G, Mikhailov T, Freels S, Donoghue E. Ethnic differences in mortality from insulin-dependent diabetes mellitus among people less than 25 years of age. Pediatrics. 1999;103(5 Pt 1):952–6. doi: 10.1542/peds.103.5.952. [DOI] [PubMed] [Google Scholar]
- 11.Bosnyak Z, Nishimura R, Hagan Hughes M, Tajima N, Becker D, Tuomilehto J, Orchard TJ. Excess mortality in Black compared with White patients with Type 1 diabetes: an examination of underlying causes. Diabet Med. 2005;22(12):1636–41. doi: 10.1111/j.1464-5491.2005.01671.x. [DOI] [PubMed] [Google Scholar]
- 12.Burnet DL, Cooper AJ, Drum ML, Lipton RB. Risk Factors for Mortality in a Diverse Cohort of Patients with Childhood-onset Diabetes in Chicago. Diabetes Care. 2007;30(10):2559–63. doi: 10.2337/dc07-0216. [DOI] [PubMed] [Google Scholar]
- 13.Roy M, Rendas-Baum R, Skurnick J. Mortality in African-Americans with Type 1 diabetes: The New Jersey 725. Diabetic Medicine. 2006;23:698–706. doi: 10.1111/j.1464-5491.2006.01901.x. [DOI] [PubMed] [Google Scholar]
- 14.Cause of Death, 2008. Bureau of Vital Statistics. U.S. Virgin Islands Department of Health, 2011.
- 15.Tull E, Christian V, Roseman J. Epidemiology of Childhood IDDM in the U.S. Virgin Islands from 1979-1988. Evidence of an epidemic in the early 1980s and variation by degree of racial admixture. Diabetes Care. 1991;14(7):558–564. doi: 10.2337/diacare.14.7.558. [DOI] [PubMed] [Google Scholar]
- 16.Karvonen M, Viik-Kajander M, Moltchanova E, Libman I, LaPorte R, Tuomilehto J. Incidence of childhood type 1 diabetes worldwide. Diabetes Care. 2000;23:1516–26. doi: 10.2337/diacare.23.10.1516. [DOI] [PubMed] [Google Scholar]
- 17.Tull ES, Christian CL, Roseman JM. Development of a Registry for diabetes in persons 0-19 years of age in the U. S. Virgin Islands. Bulletin of PAHO. 1991;25(3):218–28. [PubMed] [Google Scholar]
- 18.Major cross-country differences in risk of dying for people with IDDM. Diabetes Epidemiology Research International Mortality Study Group. Diabetes Care. 1991;14:49–54. doi: 10.2337/diacare.14.1.49. [DOI] [PubMed] [Google Scholar]
- 19.LaPorte RE, Fishbein HA, Drash AL, Kuller LH, Schneider BB, Orchard TJ, Wagener DK. The Pittsburgh insulin-dependent diabetes mellitus (IDDM) registry. The incidence of insulin dependent diabetes mellitus in Allegheny County, Pennsylvania (1965-1976) Diabetes. 1981;30:279–284. doi: 10.2337/diab.30.4.279. [DOI] [PubMed] [Google Scholar]
- 20.International analysis of insulin-dependent diabetes mellitus mortality: a preventable mortality perspective. The Diabetes Epidemiology Research International (DERI) Study. Am J Epidemiol. 1995;142:612–618. [PubMed] [Google Scholar]
- 21.Cause of Death, 2007. Bureau of Vital Statistics. U.S. Virgin Islands Department of Health, 2010.
- 22.Armstrong B. Comparing standardized mortality ratios. Ann Epidemiol. 1995;5:60–64. doi: 10.1016/1047-2797(94)00032-o. [DOI] [PubMed] [Google Scholar]
- 23.Laing SP, Swerdlow AJ, Slater SD, Botha JL, Burden AC, Waugh NR, Smith AW, Hill RD, Bingley PJ, Patterson CC, Qiao Z, Keen H. The British Diabetic Association Cohort Study, I: all-cause mortality in patients with insulin-treated diabetes mellitus. Diabet Med. 1999;16(6):459–65. doi: 10.1046/j.1464-5491.1999.00075.x. [DOI] [PubMed] [Google Scholar]
- 24.Mayer-Davis E, Beyer J, Bell R, Dabelea D, D'Agostino R, Imperatore G, Lawrence J, Liese A, Liu L, Marconvina S, Rodriguez B. Diabetes in African-American Youth. Prevalence, incidence, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2009;32(Suppl 2):S112–S122. doi: 10.2337/dc09-S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Virgin Islands Community Survey. Eastern Caribbean Center, University of the Virgin Islands; 2008. [Google Scholar]
- 26.Gutelius B, Songer T, Orchard T. Association between socioeconomic status and diabetes complications in type 1 diabetes. Diabetes. 2006;55(1) Abstract 1150-P, A1270. [Google Scholar]
- 27.Asao K, Sarti C, Forsen T, Hyttinen V, Nishimura R, Matsushima M, Reunanen A, Tuomilehto J, Tajima N Diabetes Epidemiology Research International Mortality Study Group. Long-term mortality in nationwide cohorts of childhood onset type 1 diabetes in Japan and Finland. Diabetes Care. 2003 Jul;26(7):2037–2042. doi: 10.2337/diacare.26.7.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borch-Johnsen K. Improving prognosis of type 1 diabetes. Mortality, accidents, and impact on insurance. Diabetes Care. 1999 Mar;22(Suppl 2):B1–3. [PubMed] [Google Scholar]
- 29.Territorial Licensed Medical Providers. Office of Medical Licensure and Insurance USVI Department of Health; 2010. [Google Scholar]
- 30.Kostraba JN, Dorman JS, LaPorte RE, Kuller LH, Orchard TJ, Becker DJ, Drash AL. The investigation of age at onset as a risk factor for mortality in persons with insulin-dependent diabetes mellitus using Cox proportional hazards models. Am J Epidemiol. 1991;133(1):67–72. doi: 10.1093/oxfordjournals.aje.a115804. [DOI] [PubMed] [Google Scholar]


