Abstract
Objective
To compare academic outcomes between children with orofacial cleft (OFC) and children without major birth defects.
Design and Setting
In 2007–2008, we mailed questionnaires to a random sample of mothers of school-aged children with OFC and mothers of children without major birth defects (comparison group). The questionnaire included Likert-scale, closed-ended, and open-ended questions from validated instruments. We conducted bivariate and multivariable analyses on parent-reported educational outcomes and bivariate analyses on parent-reported presence of related medical conditions between children with isolated OFC and unaffected children.
Patients/Participants
A random sample of 504 parents of children with OFCs born 1996–2002 (age 5–12 years) were identified by the North Carolina Birth Defects Monitoring Program. A random sample of 504 parents of children without birth defects born 1996–2002 was selected from North Carolina birth certificates. Of the 289 (28.7%) respondents, we analyzed 112 children with isolated OFC and 138 unaffected children.
Main Outcome Measures
Letter grades, school days missed, and grade retention.
Results
Parents of children with isolated OFC reported more developmental disabilities and hearing and speech problems among their children than comparison parents. Children with isolated OFC were more likely to receive lower grades and miss more school days than unaffected children. Because of the low response rate, results should be interpreted cautiously.
Conclusion
Children with isolated OFC may have poorer academic outcomes during elementary school than their unaffected peers. Future studies are needed to confirm these results and determine whether these differences persist in later grades.
Keywords: academic outcomes, cleft lip, cleft palate, orofacial clefts
Orofacial clefts (OFCs) are among the most common birth defects (Parker et al., 2010). Each year in the United States, an estimated 1 in 940 infants are born with cleft lip with or without cleft palate, and another 1 in 1,574 infants are born with cleft palate alone (Parker et al., 2010). OFCs can be classified as isolated or nonisolated. Nonisolated or syndromic OFC are characterized by the presence of least one other major birth defect, associated syndrome, or associated sequence whereas isolated or nonsyndromic clefts occur in the absence of other major congenital anomalies (Rasmussen et al., 2003).
Previous findings suggest that children with isolated OFC may experience differences in cognitive functioning (Jocelyn et al., 1996; Kapp-Simon and Krueckeberg, 2000; Speltz et al., 2000), behavior (Wehby et al., 2012), and speech (Estes and Morris, 1970) compared with their peers without OFC. Children with OFC also have lower achievement and increased special needs in academic settings (Goodstein, 1961; Strauss and Broder, 1993; Broder et al., 1998; Persson et al., 2012; Richman et al., 2012). Intelligence quotient (IQ) studies have shown that children with isolated OFC have lower mean scores than children without OFC, and this trend is apparent at young ages (12–24 months old) and early adulthood (Jocelyn et al., 1996; Eide et al., 2006; Persson et al., 2008). Evaluation of specific cognitive functions shows that the greatest deficit is in verbal IQ, and children with OFC may experience increased reading and language problems (Kommers and Sullivan, 1979; Richman et al., 1988; Collett et al., 2010a; Collett et al., 2010b). Children with OFC are also at higher risk for frequent ear infections, hearing difficulties, and speech problems (Fox et al., 1978; Jocelyn et al., 1996; Broen et al., 1998; Collett et al., 2010b). In fact, children with OFC, both isolated and nonisolated, are more than three times as likely to receive services for a speech or language disorder than children without birth defects (Yazdy et al., 2008). Cognition, reading, language, hearing, speech, developmental, and behavioral problems in school settings may result in challenges in academic achievement for children with any of these conditions and may be magnified for children with OFC.
Understanding academic performance in children with OFC is important for development of interventions and services to improve the short- and long-term outcomes of this population. Previous studies focusing on academic outcomes in children with OFC in the United States have mostly been clinic based with small sample sizes, and some studies have not included an unaffected comparison group (Richman, 1976; Broder et al., 1998; Broen et al., 1998; Collet et al. 2010a).
No previously published studies have assessed academic outcomes on a population-based level using birth defects registries in the United States. The purpose of this study was to examine the academic achievement of 5- to 12-year-old children with isolated OFC compared with that of children without a major birth defect using a population-based, statewide sample. We hypothesized that children with isolated OFC (i.e., children with no other major birth defects) would have lower letter grades, miss more school days, and have higher grade retention rates than children without a major birth defect even after adjusting for selected maternal and child characteristics.
Methods
Participants and Study Design
A total of 1,232 children with OFC, including isolated and nonisolated OFC, were born in North Carolina between 1996 and 2002 and ascertained by the North Carolina Birth Defects Monitoring Program (NCBDMP). From this total, we used the survey select procedure in SAS software version 9.3 (SAS Institute, Cary, NC) to identify a random sample of mothers of school-aged (5–12 years old) children with OFC (n = 504). The NCBDMP is a population-based, statewide birth defects surveillance system that gathers information from all hospitals, except military hospitals, in the state. The NCBDMP ascertains information on all live-born infants, fetal deaths at or after 20 weeks’ gestation, and pregnancy terminations that are associated with one or more major birth defects diagnosed in the first year of life and in which the mother is a North Carolina resident. For infants with major birth defects, the NCBDMP collects information from health services databases, Medicaid-paid claims information, and vital statistics data (National Birth Defects Prevention Network, 2011). Major birth defects are defined as conditions present at birth that cause structural changes in one or more parts of the body and can have a serious, adverse effect on health, development, or functional ability (Parker et al., 2010).
This study included children with cleft lip only, cleft palate only, and cleft lip with cleft palate. Children with a nonisolated OFC were identified through the NCBDMP by the presence of at least one other major birth defect, using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and British Pediatric Association Classification of Diseases (BPA) diagnostic codes. Children with a nonisolated OFC were excluded from our analysis because their academic success may have been affected by the additional birth defect(s) instead of the OFC alone. This exclusion also allowed for a more homogenous group and direct comparability with previous studies.
The control group was a random sample of mothers of children without a major birth defect born during the same time period, between 1996 and 2002, and selected from North Carolina birth certificates (n = 504). Mothers who were unable to speak or read English or Spanish, whose child had died before the survey, or whose child was born out of state were excluded from both groups of children.
Between May 2007 and April 2008, questionnaires were mailed to mothers in our study sample. The survey included Likert-scale and closed-ended and open-ended questions from validated quality-of-life instruments, including the Pediatric Quality of Life Inventory 4.0, Youth Quality of Life Instrument-Research Version, and Youth Quality of Life Instrument-Facial Differences Module (Strauss et al., 1995; Patrick et al., 2002; Edwards et al., 2005; Topolski et al., 2005; Varni et al., 2005; Varni et al., 2006;). Survey domains included demographics, outcomes, family life, dental health, diagnostic experiences, and other quality-of-life aspects, but only the results related to academic outcomes are described in this study. If potential participants did not respond to the initial mailing, up to three subsequent mailings were attempted in order to contact the mothers. Most participants responded to the first mailing. For successful completion and return of the survey, respondents were sent a $20 gift card.
The academic outcomes measured included overall letter grades, number of school days missed, and grade retention from maternal report in the questionnaire. For overall letter grades, mothers selected the grade (A through F) that their child had received most frequently in the recent grading period. Because of the small numbers, letter-grade categories were collapsed into mostly As and Bs (typically above average) and mostly Cs, Ds, or Fs (below average). Mothers could also answer “not in school” or “other,” followed by an open-ended question to allow for further explanation. Children indicated as “not in school” or “other” whose response could not be reassigned a letter-grade category were excluded from all the letter-grade analyses.
Number of school days missed in the past 12 months was a free-response question that also included the option “not in school.” The number of school days missed was collapsed into categories of 5 or fewer days (1 school week or less) missed and 6 or more days (more than 1 school week) missed based on consultation with clinical and public health experts in cleft and craniofacial conditions and developmental disabilities. Children whose mothers responded “not in school” were excluded from the school days missed analyses. Grade retention was measured by asking, “Starting since kindergarten, has your child repeated any grades?” Grade retention was analyzed as a binary variable (yes/no).
Maternal and child characteristics thought to be associated with academic outcomes were considered for the multivariable analyses. The child's sex, race/ethnicity, age, and primary health insurance; mother's age at delivery; respondent's relationship to the child; marital status; household income; and maternal education were obtained from the survey. Preterm birth and child's birth weight were obtained from vital statistics data. If information on the child's age or race/ethnicity or the mother's age was missing or illogical from the survey responses, we used demographic data from vital statistics.
A socioeconomic status (SES) variable was created from the mother's education level, household income level, and child's primary insurance. Each of these three components was categorized as “low” or “high” for each child. “Low” was equal to mother's education ≤high school degree, household income <$25,000, and public or no insurance for the child. “High” was equal to mother's education >high school degree, household income ≥$25,000, and private insurance for the child. A child was given one point for each characteristic classified as low for an SES score ranging from zero to three with zero representing the highest SES (high SES or no low categories) and three the lowest SES category (all categories were low). This SES method was derived from a similar study involving children with OFC and academic outcomes and another study involving other birth defects (Yang et al., 2008; Wehby et al., 2012). These categorizations were evaluated using a correlation matrix.
The presence of other medical conditions was obtained from maternal report on the questionnaire. The questions used to ascertain this information were validated, standardized questions used in the 2003 National Survey of Children's Health to collect information on the presence of medical conditions. The wording of these questions was as follows: “Has a doctor or medical professional ever told you that your child has_________” (Maternal and Child Health Bureau, 2013). The 10 conditions included in the survey were mental retardation, attention deficit disorder (ADD) or attention deficit hyperactivity disorder (ADHD), depression or anxiety, behavior or conduct problems, problems with shyness, developmental delay or physical impairment, hearing problems, speech problems, and three or more ear infections in the past 12 months. The term “mental retardation” was used in the survey instrument, but a more acceptable term, “intellectual disability,” will be used throughout the remainder of this article to represent this developmental disability (Schalock et al., 2007).
Statistical Analysis
We compared the selected maternal and child characteristics and the presence of the selected medical conditions between children with OFC and children without a major birth defect using chi-square tests, Fisher exact tests, and t tests where appropriate to calculate P values. A P value < .05 was considered statistically significant.
Multivariable regression models were developed for each of the three academic outcomes with presence of OFC as the independent variable of interest. The adjusted model included child's sex, race/ethnicity, and age; whether the birth was preterm; SES; and maternal age and marital status. The selected medical conditions were not included in the multivariable analyses because we could not differentiate if these conditions resulted from the OFC itself or developed along a causal pathway distinct from the OFC. Low birth weight was not included in the adjusted models because it was correlated with preterm birth, and preterm birth is more often associated with cognitive function. Crude odds ratios (cORs), adjusted odds ratios (aORs), and 95% confidence intervals (CIs) were determined for the three academic outcomes.
To examine the effects of nonresponse, a sensitivity analysis was conducted for each of the three adjusted models. First, a propensity score was calculated for the probability of each mother responding to the questionnaire using maternal race, education, age, and marital status from the birth certificate. Deciles were created from the propensity scores, and within each group, the responders were weighted to represent the proportion of children from the underlying population in that group (responders and nonresponders). The weights were scaled and used in the adjusted logistic regression models for the three outcomes to estimate adjusted odds ratios.
All analyses were conducted using SAS software 9.3. This study was approved by the institutional review boards of the North Carolina Division of Public Health, the University of North Carolina at Chapel Hill, and Emory University.
Results
Of the 1,008 questionnaires mailed, 289 were completed and returned for an overall response rate of 28.7%. Among surveys completed, 150 were from mothers of children with OFC and 139 from mothers of children without a major birth defect, for response rates of 29.8% and 27.6%, respectively. We excluded nine children (eight children with OFC and one child without a major birth defect) because the mother reported that the child had been diagnosed with an intellectual disability, which we assumed would confound the relationship between academic outcomes and having an OFC. Another 30 of the children with OFC (21.1%) were excluded from our analysis because they had a nonisolated OFC. The final sample size for analysis was 112 children with isolated OFC and 138 children without a major birth defect.
Among the eight children with OFC excluded for intellectual disability, five had cleft palate only and three had cleft lip and palate. At the time of the survey, one was six years old, two were seven, two were eight, two were 10, and one was 11 years old. The child without OFC who was excluded for intellectual disability was nine years old at the time of the survey.
In both groups, mothers who did not respond to the survey were more likely to be non-Hispanic black compared with mothers who responded. Mothers of unaffected children who did not respond were younger at the time of their child's birth than mothers of unaffected children who responded (Table 1).
TABLE 1.
Selected Maternal and Child Characteristics Compared Between Children With Isolated Orofacial Cleft (OFC) and Children Without a Major Birth Defect and Characteristics Compared Between These Children in Both Groups (Responders) and Those Whose Mother Did Not Respond to the Survey (Nonresponders)*
| Responders |
Nonresponders |
|||
|---|---|---|---|---|
| Characteristics | Children With Isolated OFC (N = 112) N(%†) | Children Without a Major Birth Defect (N = 138) N (%†) | Children With Isolated OFC (N = 251) N(%†) | Children Without a Major Birth Defect (N = 365) N (%†) |
| Child | ||||
| Sex | ||||
| Male | 73 (65.2%) | 69 (50.0%) | 140 (55.8%) | 188 (51.5%) |
| Female | 39 (34.8%) | 69 (50.0%) | 111 (44.2%) | 177 (48.5%) |
| Race/ethnicity | ||||
| Non-Hispanic White | 93 (83.0%) | 96 (69.6%) | 202 (80.5%) | 243 (66.5%) |
| Non-Hispanic Black | 3 (2.7%) | 23 (16.7%) | 42 (16.7%) | 107 (29.3%) |
| Multiracial‡ | 5 (4.5%) | 9 (6.5%) | 0 (0.0%) | 0 (0.0%) |
| Other§ | 11 (9.8%) | 10 (7.3%) | 7 (2.8%) | 15 (4.1%) |
| Cleft type | ||||
| Cleft lip only | 31 (27.7%) | NA | 50 (19.9%) | NA |
| Cleft lip with cleft palate | 45 (40.2%) | NA | 125 (49.8%) | NA |
| Cleft palate only | 36 (32.1%) | NA | 76 (30.3%) | NA |
| Preterm birth | ||||
| <37 weeks' gestation | 16 (14.3%) | 16 (11.6%) | 38 (15.1%) | 37 (10.1%) |
| ≥37 weeks' gestation | 96 (85.7%) | 122 (88.4%) | 213 (84.9%) | 328 (89.9%) |
| Birth weight | ||||
| Low or very low (<2,500 g) | 14 (12.5%) | 10 (7.3%) | 37 (14.7%) | 30 (8.2%) |
| Normal (≥2,500 g) | 98 (87.5%) | 128 (92.8%) | 214 (85.3%) | 335 (91.8%) |
| Age at survey | ||||
| 5–6 years | 32 (28.6%) | 27 (19.6%) | 49 (19.5%) | 82 (22.5%) |
| 7–8 years | 34 (30.4%) | 41 (29.7%) | 72 (28.7%) | 101 (27.7%) |
| 9–10 years | 29 (25.9%) | 33 (23.9%) | 72 (28.7%) | 106 (29.0%) |
| 11–12 years | 17 (15.2%) | 37 (26.8%) | 58 (23.1%) | 76 (20.8%) |
| Socioeconomic status¥ | ||||
| 0 (High) | 55 (49.1%) | 82 (59.4%) | NA | NA |
| 1 | 20 (17.9%) | 25 (18.1%) | NA | NA |
| 2 | 16 (14.3%) | 12 (8.7%) | NA | NA |
| 3 (Low) | 14 (12.5%) | 14 (10.1%) | NA | NA |
| Mother | ||||
| Relationship to child | ||||
| Biological mother | 107 (95.5%) | 138 (100.0%) | NA | NA |
| Other | 2 (1.8%) | 0 (0.0%) | NA | NA |
| Marital status | ||||
| Married | 85 (75.9%) | 102 (73.9%) | NA | NA |
| Other# | 25 (22.3%) | 34 (24.6%) | NA | NA |
| Age at child's birth | ||||
| ≤20 years | 17 (15.2%) | 16 (11.6%) | 50 (19.9%) | 76 (20.8%) |
| 21–25 years | 29 (25.9%) | 21 (15.2%) | 77 (30.7%) | 106 (29.0%) |
| 26–30 years | 30 (26.8%) | 50 (36.2%) | 67 (26.7%) | 105 (28.8%) |
| 31–35 years | 27 (24.1%) | 37 (26.8%) | 35 (13.9%) | 55 (15.1%) |
| ≥36 years | 9 (8.0%) | 14 (10.1%) | 22 (8.8%) | 23 (6.3%) |
Characteristic values in bold are statistically significant (P < .05). Among responders, children with isolated OFC are compared with children without a major birth defect. Among nonresponders, children with isolated OFC are compared with responders of children with isolated OFC. Nonresponders for children without a major birth defect are compared with responders of children without a major birth defect.
Percentages may not add to 100% due to missing values.
The multiracial category was created to include mothers who reported their child's race as more than one race category.
Other races included American Indian, Alaska native, Asian, Native Hawaiian, Pacific Islander, Hispanic, multiracial, or other.
Socioeconomic status included household income, maternal education, and child's insurance status. Low indicated a low response in all three of these characteristics (mother's education ≤high school degree; household income <$25,000; and the child had public or no insurance). In comparison, high socioeconomic status indicated that the child had the opposite of these characteristics (mother's education >high school degree; household income ≥$25,000, and the child had private insurance).
Other respondent relationship included biological father and grandmother.
Other marital status included divorced, widowed, separated, never married, and unmarried couple.
Overall, of those who responded, most children were non-Hispanic white and of higher SES, and most mothers were married (Table 1). Cleft lip with cleft palate was the most frequent diagnosis among the children with OFC (n = 45; 40.2%), followed by children with cleft palate only (n = 36; 32.1%), and cleft lip only (n = 31; 27.7%). Children with OFC were significantly more likely than their peers without a major birth defect to be male (65.2% versus 50.0%) and non-Hispanic white (83.0% versus 69.6%). All other comparisons of selected maternal and child characteristics were similar between these groups.
We excluded 33 children with OFC and 29 unaffected children from the letter-grade analysis for the following reasons: 12 (10.7%) children with OFC and eight (5.8%) unaffected children were not in school; 19 (17.0%) children with OFC and 19 (13.8%) unaffected children did not receive grades at all or were not on a standard letter-grade scale; and two (1.8%) children with OFC and two (1.4%) unaffected children had missing data for letter grades. Among children with OFC, 99 (88.4%) had complete responses for school days missed and 103 (92.0%) had complete responses for grade retention. For both school days missed and grade retention, 129 (93.5%) children without a major birth defect had analyzable responses.
Among mothers of children with OFC whose child received standard letter grades, 11 (13.9%) reported receiving mostly Cs and Ds compared with eight (7.3%) children without a major birth defect (cOR, 2.0; 95% CI, 0.8–5.3). No mothers in either group reported that their child received mostly Fs, and only four mothers in the groups combined reported mostly Ds.
Comparing school days missed, 38 (38.4%) children with OFC reported missing more than five school days compared with 32 (25.4%) children without a major birth defect (cOR, 1.9; 95% CI, 1.1–3.3). Among mothers of children with OFC, eight (7.8%) reported that their child repeated a grade compared with 11 (8.5%) children without a major birth defect (cOR, 0.9; 95% CI, 0.3–2.3) (Table 2). Among children with OFC, 16.1% with cleft lip and palate, 13.3% with cleft palate only, and 11.1% with cleft lip only had mothers who reported mostly Cs or Ds. Forty-four percent of children with cleft lip and palate, 29.0% with cleft palate only, and 40.7% with cleft lip only missed more than five days of school. Seven percent of children with cleft lip and palate, 6.1% with cleft palate only, and 10.7% with cleft lip only had repeated a grade.
TABLE 2.
Academic Outcomes Among Children With Isolated Orofacial Clefts and Children Without a Major Birth Defect*
| Children With Isolated Orofacial Cleft (N = 112)‡ |
Children Without a Major Birth Defect (N = 138)‡ |
Unadjusted Model |
Adjusted Model† |
|||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | Crude Odds Ratio | 95% Confidence Interval | Adjusted Odds Ratio | 95% Confidence Interval | |
| Letter grades | 79 | 70.5% | 109 | 79.0% | ||||
| Mostly As and Bs | 68 | 86.1% | 101 | 92.7% | Referent | Referent | ||
| Mostly Cs and Ds | 11 | 13.9% | 8 | 7.3% | 2.0 | 0.8–5.3 | 2.6 | 0.9–8.2 |
| School days missed | 99 | 88.4% | 129 | 93.5% | ||||
| 0–5 | 61 | 59 8% | 97 | 74.6% | Referent | Referent | ||
| <5 | 38 | 38.4% | 32 | 25.4% | 1.9 | 1.1–3.3 | 1.7 | 0.9–3.1 |
| Grade retention | 103 | 92.0% | 129 | 93.5% | ||||
| No | 95 | 92.2% | 118 | 91.5% | Referent | Referent | ||
| Yes | 8 | 7.8% | 11 | 8.5% | 0.9 | 0.3–2.3 | 0.8 | 0.3–2.6 |
Odds ratios in bold are statistically significant at α = 0.05.
Fully adjusted model included child's sex, race/ethnicity, and age; preterm birth; socioeconomic status; maternal age; and marital status.
Number of children evaluated for each outcome <100% of total study sample in each group because of not applicable or missing data.
Adjusting for maternal and child characteristics, children with OFC were 2.6 times more likely to receive mostly Cs or Ds than children without a major birth defect (aOR, 2.6; 95% CI, 0.9–8.2). Adjustment slightly attenuated the odds ratio comparing school days missed between these groups. Compared with unaffected children, children with OFC were 1.7 times more likely to miss more than five school days (aOR, 1.7; 95% CI, 0.9–3.1). Children with OFC were 20% less likely to repeat a grade than children without a major birth defect (aOR, 0.8; 95% CI, 0.3–2.6) (Table 2). Using the propensity score to weight the responders, children with OFC had an adjusted odds of receiving mostly Cs or Ds 2.1 times greater than for children without OFC (95% CI, 0.8–5.6). OFC had no effect on grade retention (aOR, 1.0; 0.3–3.0), and children with OFC had 1.8 times greater odds of missing more than five days of school (95% CI, 0.9–3.3) after weighting.
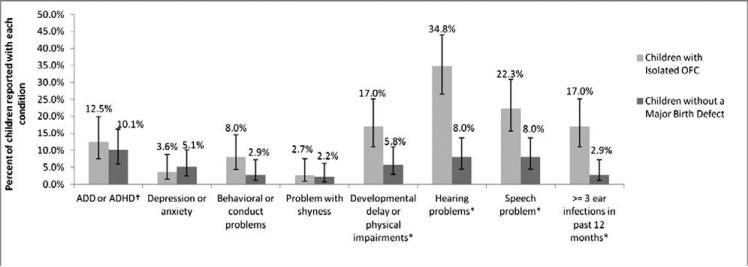
The responses on co-occurring medical conditions were assessed separately, and a number of conditions could be reported for the same child. Among children with OFC, the most common conditions reported were hearing problems (34.8%) and speech difficulties (22.3%). ADD or ADHD was the most commonly reported condition among the children without a major birth defect (10.1%). Compared with children without a major birth defect, children with OFC were significantly more likely to have developmental delay or physical impairment, hearing problems, speech problems, and three or more ear infections in the past 12 months (Figure 1).
FIGURE 1.
Prevalence and 95% confidence intervals of selected medical conditions among children with isolated orofacial cleft (OFC) and children without major birth defect (a child could have more than one medical condition; these categories are not mutually exclusive)* The prevalence of the following conditions was statistically significantly different (P <.05) between children with isolated OFC (n = 112) and children without a major birth defect (n = 138): developmental delay or physical impairments, hearing problems, speech problems, and three or more ear infections in the past 12 months.† Attention deficit disorder (ADD) and attention deficit hyperactivity disorder (ADHD).
Discussion
This study found that children with isolated OFC were more likely to receive mostly Cs and Ds and were more likely to miss more than a week of school than children without a major birth defect, even after adjusting for selected maternal and child characteristics. However, some of the CI estimates were imprecise and thus need to be interpreted with caution. Our study is congruent with a large population-based study conducted among Swedish children that found higher odds of receiving lower grades among children with OFC compared with the general population of Swedish students (Persson et al., 2012).
Despite the differences found between the two groups in our study, academic deficits among children with OFC were not as common as suggested by previous studies (Richman, 1976; Broder et al., 1998; Persson et al., 2012). We found that only 7.8% of children with OFC had repeated a grade. These results are much less than the 27% found in a 1998 clinic-based study that included 84 children with a nonsyndromic OFC (Broder et al., 1998). Like our study, the 1998 study excluded children with intellectual disability, but the 1998 study also excluded those with “giftedness.” Part of the higher rate in the 1998 study may be a result of the older age range of children and the clinic-based population. Furthermore, improvements in health care, insurance, early intervention services, and education of children with special health care needs have occurred between 1998 and 2008. These changes may have led to the increased academic success of children with OFC over time, but further research is needed to verify this conclusion.
A recent study in the United Kingdom evaluated subject-area academic achievement in seven-year-old children with cleft lip with or without cleft palate and a comparison group of children without OFC matched on sex, birth weight, and gestational age from the same region. The authors excluded children with other abnormalities or health problems. Unlike our findings, the authors did not find differences between the groups, but they assessed subject-specific areas and controlled for IQ. Because 32% of the children with OFC were identified as having special education needs compared with about 9% in the comparison group in the United Kingdom study, the researchers hypothesized that children with OFC had benefited from special needs services (Hentges et al., 2011). In our study, no information was gathered on special education and early intervention services; thus, the effect of these services on our results cannot be determined.
Our study showed children with OFC had more hearing problems, speech problems, and recurrent ear infections than unaffected children. These results concur with findings of previous studies (Fox et al., 1978; Jocelyn et al., 1996; Broen et al., 1998; Collett et al., 2010b). In our study, mothers of children with OFC also reported a higher prevalence of developmental delay or physical impairment compared with mothers of children without a major birth defect. The presence of these co-occurring conditions may explain some of the differences in letter grades and school absences between the two groups in our study. Because of an insufficient sample size, we were not able to stratify our results by the presence of these co-occurring conditions to examine this further.
Limitations
The main limitation of this study was the low response rate. The major reason for nonresponse was our inability to locate potential participants, especially older children. Similar studies using birth-defect registries have also had difficulty contacting families of older children. One study of parents of children with OFC in North Carolina had a 51.6% response rate. In that study, 89.1% of the eligible participants that did not respond to the survey were lost to follow-up (Cassell et al., 2012; Cassell et al., 2013). That response rate was higher than that of our current study because participants were able to complete the survey by mail or phone, and the children were younger (2–6 years old) so contact information in the NCBDMP was not as out-of-date as was potentially the situation with our study (Cassell et al., 2012; Cassell et al., 2013). Another telephone survey administered to families of children with spina bifida (0–17 years old) had a response rate of 47%. This higher response rate was also likely due to the phone survey administration (Tilford et al., 2009). Unfortunately, our study lacked the resources to contact potential participants by telephone.
It is encouraging that we did not find differences between responders and nonresponders with respect to several birth characteristics that are known risk factors for developmental disabilities, such as low birth weight or gestational age. Nevertheless, the low response rate increases the likelihood for bias in our results, although the extent and direction of such biases are unclear. There was a difference in the distribution of child's race between responders and nonresponders. However, the percent of children without a major birth defect who were non-Hispanic white in our study, 69.6%, was similar to this percentage in all infants born in North Carolina during the same time, 71.5% (North Carolina State Center for Health Statistics, 2013a). Our study included a larger proportion of non-Hispanic white children with OFC, 83.3%, compared with all children with OFC in North Carolina born between 1998 and 2002, 69.1% (North Carolina State Center for Health Statistics, 2013b). Among children without a birth defect whose mother responded, 19.4% had a household income less than $25,000 which is less than the 21.2% of children under the age of 19 in North Carolina in 2007 who had a household income less than $20,650 (North Carolina Institute of Medicine, 2009).
Our sensitivity analysis suggested some evidence of potential bias because of the low response rate; specifically, the survey results may have overstated the magnitude of the difference between the OFC and comparison group with respect to reported letter grades. However, correction for nonresponse still resulted in at least a twofold difference in reported letter grades between the two groups, so the interpretation of the effect remained similar. Moreover, there was no appreciable difference in the other outcomes after adjustment, which suggests that there may not be substantial bias overall from the low response rate. However, because we had limited data available to use in the propensity score, the potential for residual bias cannot be excluded. The response rate also resulted in a relatively small sample size, which led to some imprecision in our results, the categorization of outcomes, and precluded further analyses.
Our reliance on maternal reporting to assess academic performance was another limitation. First, not all children received letter grades on the traditional A–F letter-grade scale. For example, kindergarteners and older children enrolled in alternative schooling, such as private schools or Montessori schools, or those who were home-schooled, were not on a standard letter-grade system. No data were available regarding the reason for enrollment in various school types, so it is unclear whether children were in alternative schools because of previous academic difficulties or by parental choice. It is also unclear whether mothers used a previous report card or relied on memory to report their child's grades, and we were unable to validate and compare their reported responses with official grade reports. This leads to the potential for recall bias, especially if mothers of children with OFC are more concerned about academic difficulties than mothers of children without this condition. Because mothers also answered the questions about the presence of co-occurring conditions, we cannot be certain how they interpreted the questions, which may have been especially problematic for the question about developmental delay or physical impairment as this is a broad categorization. Nevertheless, we believe this indication does not include intellectual disability because we excluded children with indicated “mental retardation.” At the time this study was conducted, regulations made it impractical to ascertain school records for use in this study.
In this study, the classification of children with OFC as having isolated or nonisolated birth defects was primarily based on the ICD-9-CM and BPA codes in the NCBDMP. Ideally, such classification should be carried out by a clinical geneticist and based on a detailed, verbatim clinical description of the child's phenotype. In this study, it is possible that some of the children who were excluded as having nonisolated OFC had birth defects that were relatively minor and, thus, should have been retained in the analysis. In addition, the NCBDMP only includes infants diagnosed with a birth defect in the first year of life, which makes it possible that some children with OFC had another birth defect that had not yet been detected. We also lacked data on timeliness of cleft surgical repair, which could affect short- and long-term outcomes, such as speech impediments, stigmatization, and quality of life.
For children who repeated a grade, no rationale was available indicating whether the child failed academically or was held back a year for medical or behavioral problems or other reasons, such as a family emergency. We did not have data on the use of special education services or the presence of an individualized education program, which may affect the criteria for grade promotion and receipt of letter grades for children with certain exceptionalities. Similarly, we could not discern the reason why children missed school days and whether it was related or unrelated to the OFC (e.g., the child was sick, had medical appointments, went on family vacation, or missed school to avoid bullying or stigmatization). Additional surgeries to correct the OFC are common in this age group and likely a reason for some children's absences but we are unable to verify this with our data. Information was not available from teachers or about school characteristics that may affect a child's academic achievement, such as the size, location, and student-teacher ratio of the school attended.
Strengths
The major advantages of this study were that we used a population-based, statewide sample that included a randomly selected, representative comparison group of children without major birth defects. The population-based, statewide sample likely better represents the range of severity in OFC compared with other study samples, which were based on convenience samples from hospitals and cleft and craniofacial centers (Broder et al., 1998; Hentges et al., 2011). Having a more representative sample is important because children with OFC seen regularly at a cleft and craniofacial center may be those children who require more management and treatment, are of a higher SES, and/or differ on other characteristics that affect academic outcomes. Including a population-based comparison group is preferable to the method of previous studies that did not because the children without a major birth defect represent the baseline academic achievement of children from the same source population.
Another strength of our study was that the questionnaire was derived from previously validated quality-of-life instruments. In addition, we were able to assess the academic outcomes while controlling for SES, using a composite SES measure based on maternal education, household income, and child's health insurance type. These types of variables were not consistently collected in previous studies. Also, previous studies on quality of life in this population did not have the benefit of linking with a statewide birth defects registry.
Finally, the survey captured information on number of school days missed, which had not been previously evaluated. Therefore, this study provided a better understanding of the overall school experience of children with OFC compared with children without birth defects.
Conclusions
Our results indicate children with OFC may be more likely to have poorer academic outcomes than their peers without a major birth defect, but the magnitude of this association is uncertain because of the small sample size. Nevertheless, the percentage of children with poor academic outcomes was small in both groups, suggesting that even though a comparatively higher proportion of children with OFC perform poorly than unaffected children, most children with OFC are successful in school. This study is important for its assessment of these academic outcomes and related co-occurring conditions because of its use of a population-based, statewide birth defects registry, which can more accurately reflect the variability of difficulties experienced by children with OFC. Similar population-based studies are needed to replicate these findings and identify characteristics that determine academic achievement among children with this type of birth defect, including the presence of different cleft types along with associated syndromes or co-occurring medical conditions.
Our study also identified difficulties and areas of improvement for future studies that use birth defect registries to assess academic outcomes. These studies should try to link vital statistics, birth defects registry, early intervention, health insurance, medical records, and school record information to recruit a larger population-based sample of children and to compare school records to parent reports for better accuracy of academic outcomes. Additional information to collect includes reasons for special education placement and the type of school attended (e.g., private, public, or Montessori). Additional studies should evaluate academic achievement in older children because many of the younger children in our study did not have meaningful academic values. Public school standardized tests and standard letter grades are typically initiated by third grade, which may be the youngest meaningful age to include in academic outcome studies. As older children face more academic challenges, older children with OFC may diverge further from their peers without OFC. Furthermore, school-aged children with OFC may continue to be treated and be further exposed to factors already mentioned, including ear infections and social stigmatization. Optimal studies would also include linked longitudinal academic and medical record data to further evaluate maternal and child characteristics that potentially predict academic success.
Acknowledgments
We would like to thank the survey respondents for their participation and thoughtful feedback. We acknowledge the NCBDMP staff for obtaining and linking data for this project. We also thank Eleanor Howell, with the North Carolina State Center for Health Statistics, for assistance in data cleaning and analysis; Michele Marcus, with the Rollins School of Public Health, Emory University, for input on methodologic approaches and support; and Amelia Drake, with the University of North Carolina Craniofacial Center, for sharing her clinical expertise on speech, hearing, and ear infections in children with OFC. Lastly, we acknowledge Margaret Honein with the CDC's National Center on Birth Defects and Developmental Disabilities for her helpful comments on previous drafts and support of this project.
This work was supported by the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention (grant number U50/CCU422096).
Footnotes
Parts of this manuscript were presented at the National Birth Defects Prevention Network meeting, February 27–29, 2012, Arlington, Virginia, and the American Cleft Palate-Craniofacial Association annual meeting, April 17–21, 2012, San Jose, California.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors had no financial relationships relevant to this article to disclose.
REFERENCES
- Broder HL, Richman LC, Matheson PB. Learning disability, school achievement, and grade retention among children with cleft: a two-center study. Cleft Palate Craniofac J. 1998;35:127–131. doi: 10.1597/1545-1569_1998_035_0127_ldsaag_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- Broen PA, Devers MC, Doyle SS, Prouty JM, Moller KT. Acquisition of linguistic and cognitive skills by children with cleft palate. J Speech Lang Hear Res. 1998;41:676–687. doi: 10.1044/jslhr.4103.676. [DOI] [PubMed] [Google Scholar]
- Cassell CH, Krohmer A, Mendez DD, Strauss RP, Meyer RE. Factors associated with distance and time traveled to cleft and craniofacial care. Birth Defects Res A Clin Mol Teratol. 2013;97:685–695. doi: 10.1002/bdra.23173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassell CH, Mendez DD, Strauss RP. Maternal perspectives: qualitative responses about perceived barriers to care among children with orofacial clefts in North Carolina. Cleft Palate Craniofac J. 2012;49:262–269. doi: 10.1597/09-235. [DOI] [PubMed] [Google Scholar]
- Collett BR, Leroux B, Speltz ML. Language and early reading among children with orofacial clefts. Cleft Palate Craniofac J. 2010a;47:284–292. doi: 10.1597/08-172.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collett BR, Stott-Miller M, Kapp-Simon KA, Cunningham ML, Speltz ML. Reading in children with orofacial clefts versus controls. J Pediatr Psychol. 2010b;35:199–208. doi: 10.1093/jpepsy/jsp047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards TC, Patrick DL, Topolski TD, Aspinall CL, Mouradian WE, Speltz ML. Approaches to craniofacial-specific quality of life assessment in adolescents. Cleft Palate Craniofac J. 2005;42:19–24. doi: 10.1597/03-097.2.1. [DOI] [PubMed] [Google Scholar]
- Eide MG, Skjaerven R, Irgens LM, Bjerkedal T, Oyen N. Associations of birth defects with adult intellectual performance, disability and mortality: population-based cohort study. Pediatr Res. 2006;59:848–853. doi: 10.1203/01.pdr.0000219172.16638.f9. [DOI] [PubMed] [Google Scholar]
- Estes RE, Morris HL. Relationships among intelligence, speech proficiency, and hearing sensitivity in children with cleft palates. Cleft Palate J. 1970;7:763–773. [PubMed] [Google Scholar]
- Fox D, Lynch J, Brookshire B. Selected developmental factors of cleft palate children between two and thirty-three months of age. Cleft Palate J. 1978;15:239–245. [PubMed] [Google Scholar]
- Goodstein LD. Intellectual impairment in children with cleft palates. J Speech Hear Res. 1961;4:287–294. doi: 10.1044/jshr.0403.287. [DOI] [PubMed] [Google Scholar]
- Hentges F, Hill J, Bishop DV, Goodacre T, Moss T, Murray L. The effect of cleft lip on cognitive development in school-aged children: a paradigm for examining sensitive period effects. J Child Psychol Psychiatr. 2011;52:704–712. doi: 10.1111/j.1469-7610.2011.02375.x. [DOI] [PubMed] [Google Scholar]
- Jocelyn LJ, Penko MA, Rode HL. Cognition, communication, and hearing in young children with cleft lip and palate and in control children: a longitudinal study. Pediatrics. 1996;97:529–534. [PubMed] [Google Scholar]
- Kapp-Simon KA, Krueckeberg S. Mental development in infants with cleft lip and/or palate. Cleft Palate Craniofac J. 2000;37:65–70. doi: 10.1597/1545-1569_2000_037_0065_mdiiwc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- Kommers MS, Sullivan MD. Written language skills of children with cleft palate. Cleft Palate J. 1979;16:81–85. [PubMed] [Google Scholar]
- Maternal and Child Health Bureau [March 15, 2013];National Survey of Children’s Health, 2007. Available at http://www.cdc.gov/nchs/data/slaits/ NSCH_Questionnaire.pdf.
- National Birth Defects Prevention Network (NBDPN) State birth defects surveillance program directory. Birth Defects Res A Clin Mol Teratol. 2011;91:1028–1049. [Google Scholar]
- North Carolina Institute of Medicine . Prevention for the Health of North Carolina: Prevention Action Plan. North Carolina Institute of Medicine; Morrisville: 2009. Socioeconomic Determinants of Health. p. 246. Chapter 11. [Google Scholar]
- North Carolina State Center for Health Statistics, DHHS [October 16, 2013a];Selected Vital Statistics for 1996, 1997, 1998, 1999, 2000, 2001, and 2002. Available at http://www.schs.state.nc.us/data/vital.cfm.
- North Carolina State Center for Health Statistics, DHHS [October 16, 2013b];N.C. Birth Defects, Statewide Totals. Available at http://www.schs.state.nc.us/ schs/data/bdefects/defectsbystate.cfm.
- Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE. National Birth Defects Prevention Network. Updated national birth prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin Mol Teratol. 2010;88:1008–1016. doi: 10.1002/bdra.20735. [DOI] [PubMed] [Google Scholar]
- Patrick DL, Edwards TC, Topolski TD. Adolescent quality of life, part II: initial validation of a new instrument. J Adolesc. 2002;25:287–300. doi: 10.1006/jado.2002.0471. [DOI] [PubMed] [Google Scholar]
- Persson M, Becker M, Svensson H. General intellectual capacity of young men with cleft lip with or without cleft palate and cleft palate alone. Scand J Plast Reconstr Surg Hand Surg. 2008;42:14–16. doi: 10.1080/02844310701694472. [DOI] [PubMed] [Google Scholar]
- Persson M, Becker M, Svensson H. Academic achievement in individuals with cleft: a population-based register study. Cleft Palate Craniofac J. 2012;49:153–159. doi: 10.1597/09-047. [DOI] [PubMed] [Google Scholar]
- Rasmussen SA, Olney RS, Holmes LB, Lin AE, Keppler-Noreuil KM, Moore CA. Guidelines for case classification for the National Birth Defects Prevention Study. Birth Defects Res A Clin Mol Teratol. 2003;67:193–201. doi: 10.1002/bdra.10012. [DOI] [PubMed] [Google Scholar]
- Richman LC. Behavior and achievement of cleft palate children. Cleft Palate J. 1976;13:4–10. [PubMed] [Google Scholar]
- Richman LC, Eliason MJ, Lindgren SD. Reading disability in children with clefts. Cleft Palate J. 1988;25:21–25. [PubMed] [Google Scholar]
- Richman LC, McCoy TE, Conrad AL, Nopoulos PC. Neuropsycho-logical, behavioral, and academic sequelae of cleft: early developmental, school age, and adolescent/young adult outcomes. Cleft Palate Craniofac J. 2012;49:387–396. doi: 10.1597/10-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schalock RL, Luckasson RA, Shogren KA, Borthwick-Duffy S, Bradley V, Buntinx WH, Coulter DL, Craig EM, Gomez SC, Lachapelle Y, et al. The renaming of mental retardation: understanding the change to the term intellectual disability. Intellect Dev Disabil. 2007;45:116–124. doi: 10.1352/1934-9556(2007)45[116:TROMRU]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Speltz ML, Endriga MC, Hill S, Maris CL, Jones K, Omnell ML. Cognitive and psychomotor development of infants with orofacial clefts. J Pediatr Psychol. 2000;25:185–190. doi: 10.1093/jpepsy/25.3.185. [DOI] [PubMed] [Google Scholar]
- Strauss RP, Broder H. Children with cleft lip/palate and mental retardation: a subpopulation of cleft-craniofacial team patients. Cleft Palate Craniofac J. 1993;30:548–556. doi: 10.1597/1545-1569_1993_030_0548_cwclpa_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- Strauss RP, Sharp MC, Lorch SC, Kachalia B. Physicians and the communication of “bad news”: parent experiences of being informed of their child's cleft lip and/or palate. Pediatrics. 1995;96:82–89. [PubMed] [Google Scholar]
- Tilford JM, Grosse SD, Goodman AC, Li K. Labor market productivity costs for caregivers of children with spina bifida: a population-based analysis. Med Decis Making. 2009;29:23–32. doi: 10.1177/0272989X08322014. [DOI] [PubMed] [Google Scholar]
- Topolski TD, Edwards TC, Patrick DL. Quality of life: how do adolescents with facial differences compare with other adolescents? Cleft Palate Craniofac J. 2005;42:25–32. doi: 10.1597/03-097.3.1. [DOI] [PubMed] [Google Scholar]
- Varni JW, Burwinkle TM, Seid M. The PedsQL 4.0 as a school population health measure: feasibility, reliability, and validity. Qual Life Res. 2006;15:203–215. doi: 10.1007/s11136-005-1388-z. [DOI] [PubMed] [Google Scholar]
- Varni JW, Burwinkle TM, Sherman SA, Hanna K, Berrin SJ, Malcarne VL, Chambers HG. Health-related quality of life of children and adolescents with cerebral palsy: hearing the voices of the children. Dev Med Child Neurol. 2005;47:592–597. [PubMed] [Google Scholar]
- Wehby GL, Tyler MC, Lindgren S, Romitti P, Robbins J, Damiano P. Oral clefts and behavioral health of young children. Oral Dis. 2012;18:74–84. doi: 10.1111/j.1601-0825.2011.01847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J, Carmichael SL, Canfield M, Song J, Shaw GM, National Birth Defects Prevention Study Socioeconomic status in relation to selected birth defects in a large multicentered US case-control study. Am J Epidemiol. 2008;167:145–154. doi: 10.1093/aje/kwm283. [DOI] [PubMed] [Google Scholar]
- Yazdy MM, Autry AR, Honein MA, Frias JL. Use of special education services by children with orofacial clefts. Birth Defects Res A Clin Mol Teratol. 2008;82:147–154. doi: 10.1002/bdra.20433. [DOI] [PubMed] [Google Scholar]