Abstract
As globalization progressively connects and impacts the health of people across the world, collaborative research partnerships provide mutual advantages by sharing knowledge and resources to address locally and globally relevant scientific and public health questions. Partnerships undertaken for scientific research are similar to business collaborations in that they require attention to partner systems, whether local, international, political, academic, or non-academic. Scientists, like diplomats or entrepreneurs, are representatives of their field, culture, and country and become obligatory agents in health diplomacy. This role significantly influences current and future collaborations with not only the immediate partner but with other in country partners as well. Research partnerships need continuous evaluation of the collaboration’s productivity, perspectives of all partners, and desired outcomes for success to avoid engaging in “research tourism”, particularly in developing regions. International engagement is a cornerstone in addressing the impact of infectious diseases globally. Global partnerships are strategically aligned with national, partner and global health priorities and may be based on specific requests for assistance from the partnering country governments. Here we share experiences from select research collaborations to highlight principles that we have found key in building long-term relationships with collaborators and in meeting the aim to address scientific questions relevant to the host country and strategic global health initiatives.
Keywords: Collaboration, Clinical research, Research diplomacy, International, Partnership, Stakeholder
Introduction
Collaborative research relationships and international diplomacy
A strong consensus of shared goals and values is critical to international engagement. This has been at the core of successful international development programs, which have enabled host country priorities, engagement and ownership to be at the forefront [1,2]. When these projects are poorly implemented, the legacies often build negative precedents and do harm to future country to country collaborations. It is therefore necessary for researchers to consider a country’s culture and public health context as they embark upon a research partnership. For example, the informed consent process may require different strategies in more versus less developed settings. One of our collaborators has noted that in developing countries, the initial decision-making for informed consent is typically vested in the community rather than the individual and that illiteracy is common, which limits the value of written documents and signatures [3]. Without context, approaches that are appropriate in one setting may be inappropriately applied in another.
Due to the global nature of emerging infectious diseases, it has become increasingly important for the scientific arms of governments to conduct research on diseases of international importance at sites throughout the world. Herein we share our experiences based on our engagement in a government-to-government context while incorporating lessons from the business sector. Our partnerships are unique in engaging higher levels of the government at initiation and challenging in terms of how best to engage within the context of the country with collaborators chosen based on their position in the government. We focus on four key principles that, though not necessarily scientific in nature, are essential to building successful relationships in this context and conducting meaningful research.
Principle 1: Assess Needs and Build Sustainable Capacity
Learn from them. Start with what they know. Build with what they have. [With the best leaders], when the work is done, the task accomplished, the people will say, “We have done this ourselves.” Lao Tzu.
Collaborative scientific research requires skills and equipment that depend on the nature and scope of the project. While infrastructure strengthening will be needed in most cases, this must be done with the goal of leaving tangible benefits and not just creating a dependency on external resources. It is critical not to have preconceived notions of what will be best for others or to consider one’s own motivations as the only standard to work from. Understanding collaborators’ decision-making paradigms will facilitate project feasibility [4].
The assumption that people choose to conduct research to investigate interesting questions or improve community health is common, but may be incorrect. Partners may perceive training needs, revenue, or infrastructure establishment as the primary goal. In the developing world where individuals face significant financial hardship, monetary benefit may be a stimulus to work on an international project; the job may pay better or perhaps other work is not available. Still, not all capacity building endeavors require extensive financial commitment. In many cases, the rationale is altruism or enhanced career opportunities. Capacity building can take the form of teaching and training in research principles, practice and ethics, language skills, or mentoring. Such engagement is ultimately more meaningful and results in greater sustainable benefits. It is important to understand motivations and monitor them from the beginning of the project to maintain progress.
Strategic planning, discussed further below, can facilitate the development of Key Performance indicators (KPI’s). These could be based on effective transfer of technology, career development, or functional relationships with local disease control programs. The impact of these should include increased research capacity, better governance, more publications, increased scientific collaborations, and decreased outsourcing of skills. Assessment of the collaboration’s sustainability should address these diverse relevant parameters.
Illustration of principle 1
Despite the acute realization that research is needed, it continues to be a “want” in many middle and lower income regions because it is of lower priority than immediate clinical care provision. Furthermore, there is minimal access to adequate training to independently conduct research. In one partnership we faced challenges in developing mutually aligned goals due to the issues mentioned above. An internal review highlighted that while the project was considered beneficial it was felt that it primarily helped boost the portfolios of US scientists, did not have an immediate impact on public health and did not engage with national health care programs. Through strategic planning sessions, and discussions with the leaders of health care programs we developed mechanisms to make data of concern to the programs accessible to them, developed clear publication and mentoring policies and worked with junior scientists to develop career plans. A better understanding of the underlying concerns of our collaborators allowed us to work towards common goals, address specific partner priorities and develop operational transparency and alignment.
Principle 2: Engage Stakeholders
“It used to be the case that the value of a gold mine was based on three variables: the amount of gold in the ground, the cost of extraction and the world price of gold. Today, I can show you two mines, identical [in terms of] these three variables that differ in their valuation by an order of magnitude. Why? Because one has local support and the other doesn’t [5]”.
Edward Freeman defined stakeholders as individuals who have a vested interest in the project or work [6]. These individuals may be Internal, those who are an integral part in the execution of the project, or External, those who have some relationship, influence or impact on the project and on whom the project usually has some impact (Figure 1).
Figure 1.
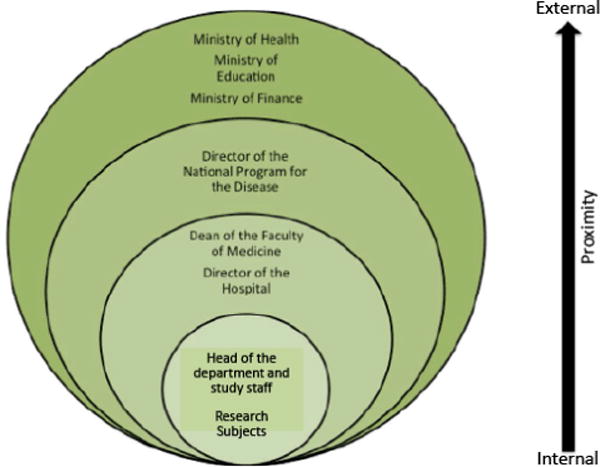
Example of different stakeholders and their distance from a project. Distance from a project is represented by size of the circle. In this example, head of the department and staff and research subjects are the most internal stakeholders.
Regardless of the proximity or distance of the stakeholders to the project, it is important to identify them, their values and interests and understand their relationship to and impact on the project’s success. Project partners may not represent the diverse stakeholders that can influence outcomes. Similarly, local entities involved directly or tangentially often have questions about the research. Since changes at policy or operational leadership levels can heavily influence the approach to research operations and decision-making, acknowledgement of and discussions with external stakeholders early and on a continuing basis provides the basis for the collaboration well beyond the immediate partners. This investment for the future establishes alliances and trust and becomes invaluable especially if support from these individuals or groups may be needed later [7]. It also helps ensure that the research is relevant to and appropriate for the involved communities.
A stakeholder analysis should be done early on to identify internal and external stakeholders, as well as understand their level of interest, their potential impact and how to effectively engage them to ensure optimal support and buy in. The analysis should take into account that stakeholder characteristics vary by country and type of research. Many different strategies for stakeholder analyses have been used successfully in diverse settings, including commercially available tools, interviews, focus groups, online and paper questionnaires, or a combination of these [8–12]. In our projects, the stakeholder analysis has usually been done by a working group of the partners to initially identify key stakeholders, followed by reaching out to them to introduce the research or project and obtain feedback. This is done on an individual level as well as through organizing facilitated stakeholder meetings. It is important to keep in mind that stakeholders change over time and new entities may have to be considered with organizational or governmental changes. The stakeholder list and engagement strategies should be periodically reviewed in conjunction with the strategic plan. Structured monitoring and evaluation strategies provide useful feedback and inform evolution of stakeholders and their roles [13].
Illustration of principle 2
In one project, both partners had good research experience. However, access to health care facilities, agreement from the heads of the hospital system, the national disease control program, and leadership of the local center for disease control and science and technology ministry was crucial to recruiting patients, implementing research and securing resources, community engagement and political support to conduct the studies. To accomplish this, a high level Advisory board comprising of key governmental officials was developed. This advisory board was part of the governance structure and provided leadership engagement that was crucial to negotiating for various resources and other facilities to enable and conduct research. Additionally representatives of relevant health care programs were included in the team when protocols for their specific areas were being developed so that they could provide program specific input. In another project this same concept was applied in the form of targeted regular update meetings with stakeholders and invitations to project meetings so they were aware of the progress and understood the objectives of the program.
Principle 3: Invest in Leadership and Strategic Planning
“Planning is the organization of hope”. Stephen Blum.
Effective leadership and governance are as essential to good planning as they are to maintaining realism and hope. While some individuals may inherently possess leadership skills that enable them to be decisive, innovative and fair while being good managers, these skills may not come as naturally to others. This may create a vacuum of direction, vision and mentoring that is essential in collaborative science. To mitigate this it is most helpful if key collaborators are chosen based on prior track record, but this may not always be possible. Collaborators may be “assigned” or come only from a pool of non-optimal candidates. Leadership development and careful planning should be given high priority under such circumstances. Governance plans, Memoranda of Understanding (MOU) or Principles of Partnership documents are extremely helpful in defining the parameters of the collaboration and establishing realistic expectations for both parties.
Strategic planning is a tool that we have employed in several of our projects. While direction setting is not a substitute for good leadership, it helps leaders to understand gaps and bridge them with effective planning. It forces a project to set mutual goals with measurable success outcomes so that tasks can be defined to enable projects to attain desired operational results. This process should include the anticipation and management of current and changing priorities and a clear statement of both parties’ intent and contributions in order to optimize the productivity of the relationship [14]. Partner conflicts do however arise and may not be evident early in the process when everyone is engaged in relationship building. Usually the beginnings of these conflicts can be traced to the original negotiations of the partnership [15]. Therefore these early discussions need to be as transparent as possible. Clear and frequent communication is the most effective way of preventing misunderstandings. This allows development of mutual trust; open, collaborative communication between partners; and establishment of realistic expectations for reaching mutually aligned goals.
Illustration of principle 3
Collaborations can be adversely affected by differing agendas and influenced by either partner’s leadership priorities. These underlying concerns or issues may not always come up in the initial phases of a project and may arise with change in leadership or at the end of the project. In one of our projects, we faced immense challenges in developing mutually aligned goals. Though the initial agreed-upon goals appeared to be mutually beneficial to both partners, differing background agendas emerged when changes at executive operational levels engendered different goals that were not initially considered. Assessment of the partners’ interest and capacity to do research, resources to sustain efforts beyond the agreement, better alignment with national research programs to sustain efforts, and continuous awareness of the government leadership priorities was needed to achieve success. Developing a better understanding of the motivations of our collaborators allowed us to work towards common goals while addressing specific partner needs and priorities.
Having the touchstone of a written agreement and the backing of the highest levels of government allowed the project to proceed and accomplish many of the initial goals despite increasingly aggressive opposition from local senior leadership. Three key lessons from this experience were to always have jointly developed goals in writing, to ensure the support at the highest levels of the collaborative entities, and to have an agreed upon “conflict resolution” process. This will allow a collaboration to endure storms of management change.
Principle 4: Practice Cultural Awareness
In 1991 the National Football League (NFL) tried to once more introduce American football to Europe. After spending countless dollars in promotion, the NFL closed its European franchise in 2007. Major reasons cited for failure to succeed in Europe included influence of ancient cultural pastimes like bullfights known for artistry and passion and the love for European football (soccer). “Europeans view the sport as a perversion of soccer. It represents the American headstrong attitude with an emphasis on violent conflict” [16].
Culture refers to the learned, shared and enduring orientation patterns in society [16]. National heritage, religious beliefs, contemporary pressures and workplace expectations influence culture. In any collaboration there are cross-cultural risks that can be exacerbated by “ethnocentric orientation”, a tendency to judge others by one’s own cultural standards [15]. These create some of the biggest challenges in engagement in international settings. In most environments only the tip of the cultural iceberg is apparent. However, many factors that impact work and relationships lie below the surface (Figure 2). A deliberate effort is needed to understand deeper cultural aspects and their implications so that relationships can progress from being tolerated to those of mutual respect. Developing such an understanding is crucial for all collaborators though the host country culture and attitudes towards health research usually drives the context.
Figure 2.

The Cultural Iceberg. Factors below the threshold of awareness can have tremendous impact on relationships amongst collaborators and consequently impact the research. Adapted from Cavusgil, Knight and Riesenberger [16].
As collaborators become more comfortable with each other, they may advise on culturally appropriate and inappropriate behaviour. A salient example from one of the networks occurred when there was concern about lack of engagement from members of the network governing body. We had suggested assigning or “nominating” people for specific roles. However, a local leader in the network informed us that people would be insulted by such assignment; it would be more acceptable to wait for a volunteer. Furthermore, asking someone to do something obligates him or her to agree. However, they will never get around to the task if they don’t actually want to do it, which is the culturally appropriate way of passively declining and avoiding dissonance.
While “cultural competence” can be honed with study [17], appreciation of these factors should not compromise scientific integrity or productivity. Nor should it hold the relationship hostage [18]. A two-way exchange must be maintained to encourage transparent dialogue within the accepted boundaries of engagement so that emotional stress from these pressures is minimized in negotiations and discussions. Andrew Molinsky describes the skill of “cultural code–switching” as essential to success in these environments [19]. This is the act of deliberately changing behaviour sometimes against one’s own culture or instincts and beliefs to be more aligned with the partner’s culture. While this may lead to some feelings of being “inauthentic” or “incompetent”, some adjustments to behaviour help with achieving better communication, more effective mentoring, and ultimately achieving the common goals.
Illustration of principle 4
Hiring in international settings can be very challenging as processes normal in one culture may be unfamiliar in others. In one setting, screening candidates prior to presenting them to the partner’s leadership team was perceived as not giving everyone a fair chance and excluding the partners from access to all candidates. However, the screeners felt it would be against their values to forward unqualified candidates. Though eventually the best candidate was chosen, “cultural code switching” to accommodate the partners could have helped build trust even though it meant deviating from the operational method familiar to the screeners. It would also have achieved a similar outcome in terms of selecting the right person, the goal of the interviews.
Conclusions
Developing international clinical research collaborations is costly, time-consuming, and fraught with barriers that must be overcome by commitment and engagement by all partners. Nonetheless, the responsibilities of living in an increasingly global community require their development to address scientific issues that may occur regionally but have significant global impact. Attention to regional, health care, and cultural differences in the context of global standards for the ethical conduct of such research will increase the likelihood of successful execution and completion of collaborative projects. Although the formula for a healthy collaborative research relationship is amorphous and constantly evolving, it ultimately depends upon the commitment of all parties to mutually pursue the project objectives. Successful engagement by all collaborative partners contributes to greater global understanding of disease processes, builds in-country sustainable capacity and scientific expertise, and forges relationships for further health partnership endeavours.
Application of the four principles outlined in this paper can help collaborators successfully conduct meaningful international research while avoiding some common pitfalls. Understanding and sensitively addressing a community’s needs in a sustainable manner will improve project feasibility and relevance, and engender a healthier partnership. This will help prevent engagement in research tourism, in which research conducted in a less developed country is used to the advantage of a more developed country and the less developed country does not realize a benefit, and which contradicts ethical standards necessitating that clinical trials should not exploit their research subjects [20]. In line with the first principle of developing local capacity, the most appropriate research for a community may not avail itself to the best globally available methodology due to local limitations. In such cases, requirements to use the worldwide best methods should not prevent research that can benefit host communities [2].
The outlined principles will also help partner countries to engage in productive health diplomacy, which some have argued is the moral responsibility of non-local governments [21]. Health issues have played an increasing role in the development of foreign policy [22,23] and military medical researchers are being trained in practical diplomacy to help them successfully plan and implement public health surveillance, research, and capacity building programs with partner nation governments and organizations [24]. While such interactions can engender tremendous health benefits, health diplomacy can be complicated by ulterior motives [25]. For example, international military health and research programs may also serve training needs or foreign policy interests [26].
In a government-to-government context there are additional nuances of diplomatic repercussions, alignment with country and national priorities and full engagement and buy in of the appropriate government agencies that may oversee parts or all of the project. Regardless of the context in which research partnerships are developed the issues we highlight here are often overlooked, considered too late or just by chance rather than being addressed during initial engagement. We encourage early incorporation of these considerations in partnerships and utilization of tools that outline partner contributions. These would stimulate an effort to understand partner motivations and set common goals.
Political climates and priorities are dynamic and evolving. Being able to weather these changes effectively ultimately determines the sustainability of collaborations. There is no magic formula that makes all collaborations successful; however, these principles and considerations, which if practiced conscientiously and consistently can achieve lasting collaborations built on transparency, trust and clear communication. While it may be time consuming to implement these and may delay the commencement of scientific work, taking the time to have meaningful early strategic discussions may ensure that a project is completed well and sets the right precedents for all that comes after.
Key Messages.
Cross-cultural research collaborations are becoming more common.
Early engagement of all stakeholders, identification of appropriate leaders, strategic planning and cultural awareness are critical to development of successful collaborative relationships.
Capacity established during research collaboration should result in sustainable benefits for the partners, host country, and strategic global health initiatives.
Acknowledgments
The authors wish to thank their collaborators, the study participants who make research possible and the National Institute of Allergy and Infectious Diseases Office of Planning and Operations Support.
Footnotes
Disclaimer
Research reported in this publication was supported by the National Institute of Allergy and Infectious Disease of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributors and Sources
CL, SO, MP, ET, OK and SS have worked on local and international multi-partner clinical research projects. CW is a medical student focusing on global health. All authors contributed to conceptualization and development of the manuscript. CL serves as guarantor of this article and affirms that the manuscript is an honest, accurate, and transparent account of the information reported.
References
- 1.National Institute of Allergy and Infectious Disease NIH. NIAID Strategic Plan 2013. Bethesda, MD, USA: 2013. [Google Scholar]
- 2.Emanuel EJ, Wendler D, Killen J, Grady C. What makes clinical research in developing countries ethical? The benchmarks of ethical research. J Infect Dis. 2004;189:930–937. doi: 10.1086/381709. [DOI] [PubMed] [Google Scholar]
- 3.Krogstad DJ, Diop S, Diallo A, Mzayek F, Keating J, et al. Informed consent in international research: the rationale for different approaches. Am J Trop Med Hyg. 2010;83:743–747. doi: 10.4269/ajtmh.2010.10-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solter S, Solter C. Providing technical assistance to ministries of health: lessons learned over 30 years. Glob Health Sci Pract. 2013;1:302–307. doi: 10.9745/GHSP-D-13-00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henisz WJ, Dorobantu S, Nartey LJ. Spinning gold: The financial returns to stakeholder engagement. Strategic Management Journal. 2013;35:1727–1748. [Google Scholar]
- 6.Freeman RE. Strategic Management: A Stakeholder Approach. Cambridge University Press; New York, USA: 2010. [Google Scholar]
- 7.Sequeira D, Warner M. Stakeholder Engagement: A Good Practice Handbook for Companies Doing Business in Emerging Markets. International Finance Corporation; Washington, DC, USA: 2007. [Google Scholar]
- 8.Deverka PA, Lavallee DC, Desai PJ, Armstrong J, Gorman M, et al. Facilitating comparative effectiveness research in cancer genomics: evaluating stakeholder perceptions of the engagement process. Journal of comparative effectiveness research. 2012;1:359–370. doi: 10.2217/cer.12.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitropoulou C, Mai Y, van Schaik RH, Vozikis A, Patrinos GP. Stakeholder Analysis in Pharmacogenomics and Genomic Medicine in Greece. Public Health Genomics. 2014 doi: 10.1159/000365896. [DOI] [PubMed] [Google Scholar]
- 10.Namazzi G, N KS, Peter W, John B, Olico O, et al. Stakeholder analysis for a maternal and newborn health project in Eastern Uganda. BMC Pregnancy Childbirth. 2013;13:58. doi: 10.1186/1471-2393-13-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Okui O, Ayebare E, Chalo RN, Pariyo GW, Groves S, et al. Building partnerships towards strengthening Makerere University College of Health Sciences: a stakeholder and sustainability analysis. BMC international health and human rights. 2011;11:S14. doi: 10.1186/1472-698X-11-S1-S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bruner DW, Hanisch LJ, Reeve BB, Trotti AM, Schrag D, et al. Stakeholder perspectives on implementing the National Cancer Institute’s patient-reported outcomes version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE) Transl behav med. 2011;1:110–122. doi: 10.1007/s13142-011-0025-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guerra-Lopez I, Hicks K. The participatory design of a performance oriented monitoring and evaluation system in an international development environment. Eval program plann. 2014;48:21–30. doi: 10.1016/j.evalprogplan.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Motumi N, Emery S, Lane HC. Project Phidisa: development of clinical research capacity within the South African National Defence Force. Curr Opin HIV AIDS. 2007;2:69–76. doi: 10.1097/COH.0b013e328011e9c0. [DOI] [PubMed] [Google Scholar]
- 15.Gage D. The Partnership Charter: How To Start Out Right With Your New Business Partnership. Basic Books; New York, USA: 2004. [Google Scholar]
- 16.Cavusgil ST, Knight G, Riesenberger J. International Business: Strategy, Management and the New Realities. Prentice Hall; New Jersey, USA: 2013. [Google Scholar]
- 17.Sue S. Cultural Competency: From philosophy to research and practice. Journal of Community Psychology. 2006;34:237–245. [Google Scholar]
- 18.Bryson J. Strategic Planning for Public and Nonprofit Organizations: A Guide to Strengthening and Sustaining Organizational Achievement. Jossey-Bass; New Jersey, USA: 2011. [Google Scholar]
- 19.Molinsky AL. Code switching between cultures. Harv Bus Rev. 2012;90:140–141. [PubMed] [Google Scholar]
- 20.Shapiro HT, Meslin EM. Ethical issues in the design and conduct of clinical trials in developing countries. N Engl J Med. 2001;345:139–142. doi: 10.1056/NEJM200107123450212. [DOI] [PubMed] [Google Scholar]
- 21.Novotny TE. US Department of Health and Human Services: a need for global health leadership in preparedness and health diplomacy. Am J Public Health. 2006;96:11–13. doi: 10.2105/AJPH.2005.076885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gagnon ML, Labonté R. Understanding how and why health is integrated into foreign policy – a case study of health is global, a UK Government Strategy 2008–2013. Global Health. 2013;9:24. doi: 10.1186/1744-8603-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Labonté R, Gagnon ML. Framing health and foreign policy: lessons for global health diplomacy. Global Health. 2010;6:14. doi: 10.1186/1744-8603-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katz R, Blazes D, Bae J, Puntambekar N, Perdue CL, et al. Global health diplomacy training for military medical researchers. Mil Med. 2014;179:364–369. doi: 10.7205/MILMED-D-13-00389. [DOI] [PubMed] [Google Scholar]
- 25.Feldbaum H, Lee K, Michaud J. Global health and foreign policy. Epidemiologic reviews. 2010;32:82–92. doi: 10.1093/epirev/mxq006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vanderwagen W. Health diplomacy: winning hearts and minds through the use of health interventions. Mil Med. 2006;171:3–4. doi: 10.7205/milmed.171.1s.3. [DOI] [PubMed] [Google Scholar]


