Abstract
Kidney paired exchanges (KPE) have increased, yet are still underutilized. This study aimed to develop tools for assessing KPE concerns, identify predictors of KPE concerns, and describe common KPE concerns among potential living donors (LDs) and intended recipients. Incompatible former potential LDs (n=135) and intended recipients (n=83) retrospectively completed questionnaires to assess KPE concerns. Healthcare system distrust also was assessed. A minority (n=48 or 36.5% of potential LDs; n=25 or 30.1% of intended recipients) had pursued KPE participation. Of those who pursued KPE participation, 11 (22.9%) and 6 (24.0%) completed KPE donation or transplantation, respectively. The questionnaires for potential LDs and recipients showed good internal consistency and preliminary convergent validity. LDs and patients less willing to pursue KPE reported more KPE concerns. Common KPE concerns for both potential LDs and recipients were related to perceived distrust/inequity and inconvenience/cost. Multivariate predictors of more KPE concerns were: male gender (t=4.5, p<0.001) and more health care system distrust (t=2.5, p=0.01) for potential LDs; black race (t=2.1, p=0.04) and more healthcare system distrust (t=2.3, p=0.03) for intended recipients. These findings underscore the importance of addressing concerns potential LDs and patients have about KPE if the true potential of KPE is to be realized.
Keywords: living donation, kidney exchange, incompatible, paired kidney donation
INTRODUCTION
Approximately one-third of potential living donors (LDs) will be blood type incompatible or human leukocyte antigen (HLA) crossmatch-positive with their intended recipient.[1] The innovation of kidney paired exchanges (KPE), in which computer-generated algorithms are used to facilitate transplantation between incompatible donor-recipient pairs, has allowed more patients to benefit from the many advantages of live donor kidney transplantation (LDKT).[2–5] Indeed, while general trends show a decline in living kidney donation in the United States,[6] KPE has increased 10-fold in the last decade.[7]
Despite its success, however, programmatic inefficiencies, inadequate resources, and prohibitive costs contribute to KPE underutilization by transplant programs.[8–13] Also, favorable attitudes notwithstanding,[14–17] not all incompatible pairs are willing to pursue KPE. Although the true KPE uptake rate is unknown, anecdotal accounts discussed during the 2012 Consensus Conference on Kidney Paired Donation (Herndon, Virginia) suggest that the KPE participation rate among incompatible pairs may be considerably lower than 50%. Waterman et al.[15], for instance, reported that one-third of incompatible potential LDs were not willing to consider KPE; however, this study was done in an era when KPE was not offered to incompatible LDs at the two study sites. Regardless of the true KPE uptake rate, there are minimal data describing the reasons for KPE refusal among incompatible LDs or patients. The decision-making process may be influenced by certain practical and psychological considerations, including an undefined and possibly prolonged waiting period, additional costs that may be incurred by LDs, and feelings of potential inequity (e.g., other LD may “back out” or kidney graft received in the exchange may be of lower quality than the one given).[15] Identifying the KPE concerns of incompatible potential LDs and their intended recipients may help guide interventions to remove barriers and boost KPE participation.
In the current study, we sought to develop and evaluate tools for assessing KPE concerns, identify predictors of KPE concerns and their association with KPE willingness, and describe common KPE concerns among potential LDs and intended recipients. We hypothesized that more KPE concerns would be associated with lower KPE willingness. Additionally, since medical distrust is associated with LD willingness,[18] we hypothesized that medical distrust would be strongly associated with more KPE concerns.
METHODS
Study Design, Setting, and Participants
Potential LDs and their intended recipients at our center (Beth Israel Deaconess Medical Center, Boston MA) are (a) informed by their nurse coordinator about the need for compatibility testing and the opportunity for participation in KPE if testing reveals incompatibility, (b) given a brochure and referred to our website, both providing information about the KPE process, and (c) informed about compatibility testing results and, if incompatible, again presented with the opportunity to pursue further evaluation for possible KPE participation. From October 2004 to December 2011 our program participated in the New England Paired Kidney Exchange (NEPKE) program [19] and in October 2010 we joined the Kidney Paired Donation (KPD) National Pilot Program administered by the United Network for Organ Sharing (UNOS).
Using the Organ Transplant Tracking Record (OTTR), we identified former potential LDs and their intended recipients who were tested between January 1, 2006 and December 31, 2012 and invited them to take part in a retrospective questionnaire assessment. Study inclusion criteria were: ≥18 years old, ABO incompatibility or crossmatch-positive with potential LD/recipient, and confirmation via OTTR entry that both the potential LD and intended recipient were informed about KPE at the time of compatibility testing. Those who did not speak/read English were excluded from the study. An introductory letter, questionnaire packet, and prepaid return envelope were mailed to former potential LDs and intended recipients who met study criteria between July and October 2013. Key elements of informed participation were present in the study invitation letter i.e., that we were conducting research, the purpose of the research and what was being requested for participation, whom to contact with questions, and that participation was voluntary and anonymous. If a packet was returned as undeliverable, we re-searched transplant center and BIDMC databases as well as online resources for current addresses. If we did not find a primary and secondary source of identity verification, we did not mail out another questionnaire packet to ensure that the LD/recipient identity was protected. This strategy yielded few additional completed questionnaires.
Study procedures were approved by the BIDMC Institutional Review Board (Protocol #2013P-000216). Because identifiable information was not obtained from survey respondents and risk was considered minimal, the study was approved under exemption number 2 of the Code of Federal Regulations (45 CFR 46.101(b)).
KPE Concerns
Two questionnaires were developed to assess KPE concerns – Kidney Exchange Concerns – Donors (KEC-D) and Kidney Exchange Concerns–Recipients (KEC-R). To generate items for the KEC-D and KEC-R questionnaires, we reviewed qualitative and quantitative publications in which KPE experiences at the individual LD/recipient or programmatic level were described. Additionally, we asked professionals experienced in KPE (4 nephrologists, 2 surgeons, 5 LD/transplant nurse coordinators, 2 social workers, 1 psychologist, and 1 KPE program director) to identify any KPE concerns reflected in their interactions with incompatible LDs and/or intended recipients. We then generated concern statements for the KEC-D and KEC-R, respectively, with the following response options: strongly disagree (1), disagree (2), agree (3), and strongly agree (4). Our expert panel reviewed each questionnaire for clarity, readability, and redundancy, which led to several items being reworded or removed. Higher scores indicated more KPE concern. The final KEC-D and KEC-R questionnaires comprised 22 and 23 concern statements, respectively. For both measures, statements were conceptually grouped into three subscales: Distrust/Inequity, Uncertainty/Worry, and Inconvenience/Cost.(Table 1)
Table 1.
KEC-D (potential donor) and KEC-R (intended recipient) domains, number of items, means (sd), internal consistency, and sample items
| Version | Domain | Items | Mean (sd) | Cronbach’s α | Sample items |
|---|---|---|---|---|---|
| KEC-D | 22 | 49.8 (11.8) | 0.89 | ||
| Distrust / Inequity | 6 | 14.6 (4.5) | 0.83 | I was concerned that the person who I wanted to donate to might end up with a kidney that was not as good as mine. | |
| Uncertainty / Worry | 8 | 16.8 (4.2) | 0.76 | I was concerned that I would become too anxious not knowing if we would ever find a suitable match. | |
| Inconvenience / Cost | 8 | 18.4 (4.6) | 0.79 | I was concerned that waiting too long in a swap program would be disruptive to my life. | |
| KEC-R | 23 | 54.4 (10.9) | 0.86 | ||
| Distrust / Inequity | 6 | 15.3 (4.1) | 0.78 | I was concerned that the other donor in the swap would back out of it and then I would not get a transplant. | |
| Uncertainty / Worry | 9 | 20.1 (4.5) | 0.69 | I was concerned that my donor would feel more pressure to go through with donation if it was part of a swap. | |
| Inconvenience / Cost | 8 | 18.9 (4.1) | 0.75 | I was concerned that my donor’s costs in a swap program would be too high. |
KPE Willingness, Registration, and Donation/Transplantation
Participants were asked to indicate whether they (a) were willing (yes, no) to pursue further evaluation for possible KPE participation at the time they learned of incompatibility, (b) formally enrolled in KPE (i.e., registration), and (c) eventually donated or received a transplant via KPE.
Medical Distrust and Sociodemographic Characteristics
The Revised Health Care System Distrust (HCSD) Scale [20] was used to assess medical distrust. Participants indicated their level of agreement with 9 items, reflecting two domains of distrust in the health care system: values distrust (5 items; e.g., “The health care system puts making money above patients’ needs.”) and competence distrust (4 items; e.g., “The health care system makes too many mistakes.”). Total scores range from 9 to 45, with higher scores reflecting more distrust. The HCSD is used extensively in healthcare research and has been shown to be valid and reliable.[20–23] Also, we gathered basic sociodemographic information and assessed perceived emotional closeness in the donor-recipient relationship (1=not at all close, 2=somewhat close, 3=moderately close, 4=very close) from all participants.
Statistical Analyses
First, potential LD and intended recipient characteristics are presented as means and standard deviations, or frequencies and percentages, as appropriate. Fisher exact tests or t tests were used to determine whether LDs and recipients differed significantly on any variables. Second, Cronbach’s alpha coefficients were calculated to evaluate internal consistency for the KEC-D and KEC-R overall and for subscales. Third, to assess convergent and discriminant validity, Pearson correlation coefficients were calculated to measure the association between KEC and HCSD scores. Fourth, univariate analyses were conducted to examine whether KPE concerns were associated with sociodemographic characteristics and perceived relationship closeness. Fifth, linear regression was used to examine multivariable predictors of KEC total score (i.e., more concern), following standard diagnostic procedures to validate assumptions of linearity (scatterplot), absence of outliers (scatterplot, case-wise analysis), normal distribution of residuals (Normal P-P Plot), independence (Durbin-Watson test), and homoscedasticity (boxplot, Levene test). Finally, for descriptive purposes, the most commonly endorsed KPE concerns were identified (score ≥3) using frequencies and percentages. PASW Statistics (Version 17.0) software were used for statistical analyses.
RESULTS
Potential LD and Recipient Characteristics
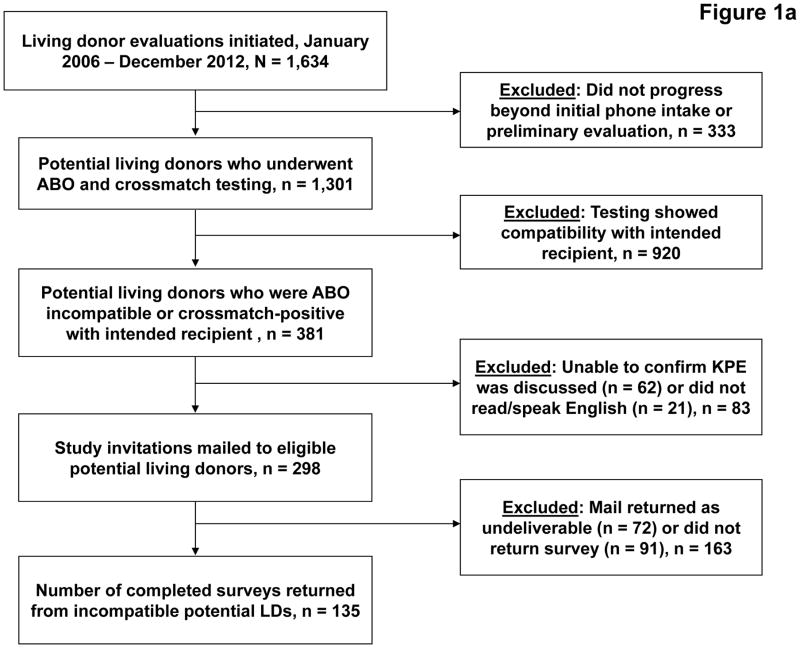
Between January 2006 and December 2012, 1,634 adults initiated LD evaluation (Figure 1a). Of the 1,301 who progressed to compatibility testing, 381 were incompatible with their intended recipient and had reached a final donation disposition prior to study initiation. Of these, 298 met study inclusion criteria and were mailed study information packets, and 135 (45%) returned completed surveys. Mean age was 50.1±12 yrs and the majority were female, white, employed, insured, college graduates, registered organ donors, and biologically related to the intended recipient.(Table 2)
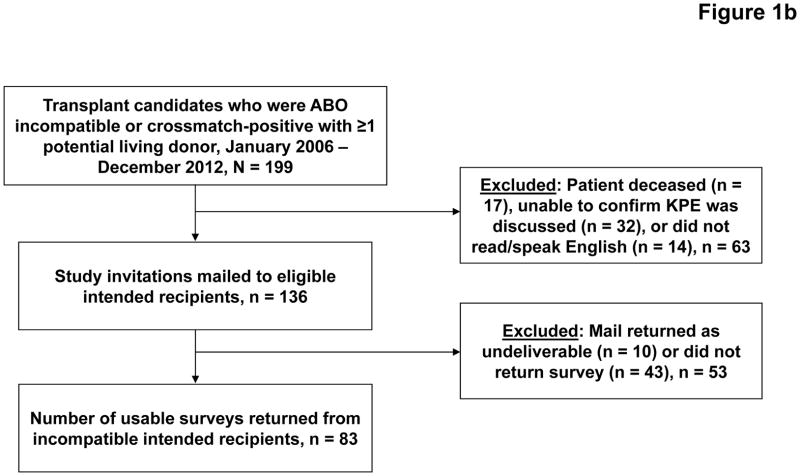
Figure 1.
Recruitment and enrollment of potential living donors (Figure 1a) and intended recipients (Figure 1b).
Table 2.
Sociodemographic characteristics of potential living donors and intended recipients
| Characteristic | Potential Living Donor (n=135) | Intended Recipient (n=83) |
|---|---|---|
| Age, mean (sd) | 50.1 (11.8) | 54.2 (11.4) |
| Sex, % (n) female | 71.9 (97) | 43.4 (36) |
| Race, % (n) | ||
| Non-Hispanic white | 62.2 (84) | 68.7 (57) |
| Black | 23.7 (32) | 16.9 (14) |
| Hispanic | 11.1 (15) | 8.4 (7) |
| Asian | 3.0 (4) | 2.4 (2) |
| Other | 0 (0) | 3.6 (3) |
| Employment, % (n) working | 85.2 (115) | 41.0 (34) |
| Education, % (n) some college | 75.6 (102) | 60.2 (50) |
| Potential donor’s relationship to intended recipient, % (n) | ||
| Parent | 5.9 (8) | 3.6 (3) |
| Child | 14.1 (19) | 15.7 (13) |
| Sibling | 14.8 (20) | 12.0 (10) |
| Other relative | 16.3 (22) | 16.9 (14) |
| Spouse | 21.5 (29) | 28.9 (24) |
| Friend or acquaintance | 27.4 (37) | 22.9 (19) |
| Health insurance, % (n) insured† | 88.9 (120) | |
| Registered organ donor, % (n) yes† | 52.6 (71) | |
| Medical distrust, mean (sd) | ||
| Total distrust | 26.8 (7.2) | 22.8 (6.9) |
| Values distrust | 14.2 (4.7) | 13.5 (4.1) |
| Competence distrust | 10.6 (3.7) | 10.0 (3.4) |
Only potential living donors were asked about their organ donor registration status and health insurance status at time they were considering donation.
The pool of former potential LDs (n=381) were incompatible with 199 intended recipients, of whom 136 met inclusion criteria and were mailed study information packets (Figure 1b). We received completed surveys from 83 intended recipients (61%), the majority of whom were male, white, not working, and had at least some college education.(Table 2) Thirty-three patients had received a transplant by the time of the survey, including 16 (16/33=49%) who underwent LDKT.
KPE Willingness, Registration, and Donation/Transplantation
A minority of former potential LDs (n=48, 36.5%) and intended recipients (n=25, 30.1%) retrospectively reported being willing to pursue KPE at the time of learning about incompatibility. Of the former potential LDs who were willing, 19 (39.6%) were registered into KPE and 11 (22.9%) donated via KPE. Six former potential LDs were withdrawn from KPE by the program (e.g., recipient no longer eligible) and two withdrew for personal reasons. Ten (40.0%) intended recipients were registered in KPE and 6 (24.0%) received a transplant via KPE.
Kidney Exchange Concerns: Internal Consistency and Validity
Table 1 shows the subscales, number of items, means (standard deviations), Cronbach’s alpha, and sample items for the KEC-D and KEC-R.
Pearson correlation coefficients between the subscales for each measure were statistically significant and ranged from 0.34 to 0.62 and 0.47 to 0.71, respectively. Both questionnaires and their subscales showed good internal consistency (α>0.70), with the exception of the KEC-R Uncertainty/Worry subscale (α>0.69).(Table 1) Convergent and discriminant validity were explored by testing relationships between the KEC questionnaires and the HCSD Scale,[20] which showed significant correlations in the expected direction. Total HCSD score was positively correlated with more KPE Distrust/Inequity (KEC-D: r=0.20, p=0.02; KEC-R: r=0.32, p=0.003) and KPE Uncertainty/Worry (KEC-D: r=0.27, p=0.013; KEC-R: r=0.30, p=0.01), but not significantly associated with KPE Inconvenience/Cost (KEC-D: r=0.14, p=0.14; KEC-R: r=0.15, p=0.19).
Relationship Between KPE Concerns, Willingness, and Participation
The relationships between KEC scores and KPE willingness were significant and in the expected direction.(Table 3) Former potential LDs and intended recipients with higher Uncertainty/Worry and Inconvenience/Cost scores were less willing to pursue KPE. Also, potential LDs with higher Distrust/Inequity scores were less willing to pursue KPE. While cell sizes for KPE registration and actual donation/transplantation were small, we also found that potential LDs and intended recipients who registered in a KPE program and those who subsequently donated or received a KPE transplant had lower mean scores on all KEC scales compared to those who did not pursue KPE registration (all P values <0.05; data not shown).
Table 3.
Differences in mean KEC-D and KEC-R scores between respondents who were willing to pursue KPE versus those who were not, by potential living donors and intended recipients
| KEC | Potential Living Donors
|
t test | Intended Recipients
|
t test | ||
|---|---|---|---|---|---|---|
| KPE Willing (n = 48) | KPE Not Willing (n = 87) | KPE Willing (n = 25) | KPE Not Willing (n = 58) | |||
|
|
|
|||||
| Total score | 46.6 (13.1) | 51.6 (10.8) | 2.4(133), p=0.02 | 50.0 (13.7) | 56.3 (9.0) | 2.5(81), p=0.02 |
| Distrust/Inequity | 13.4 (4.5) | 15.2 (4.3) | 2.2(133), p=0.03 | 14.1 (4.7) | 15.7 (3.7) | 1.4(81), p=0.17 |
| Uncertainty/Worry | 15.7 (5.0) | 17.4 (3.7) | 2.2(133), p=0.03 | 18.6 (5.5) | 20.7 (3.8) | 2.1(81), p=0.04 |
| Inconvenience/Cost | 17.2 (5.1) | 19.0 (4.2) | 2.1(133), p=0.04 | 17.0 (5.0) | 19.8 (3.4) | 2.9(81), p=0.004 |
All data expressed as means (standard deviations). Statistical tests include t test value (degrees of freedom) and p value.
Relationship Between KPE Concerns and Sociodemographic Characteristics
Former potential LDs who were male (t=4.5, df=133,P<0.001), black (t=2.6, df=133, P=0.03), and unemployed (t=2.2, df=133, P=0.04) had higher KEC-D total scores than those who were female, white, and employed. Black intended recipients had higher KEC-R total scores than white patients (t=2.4, df=81, P=0.02). Age, education, insurance type, donor registration status (LDs only), relationship type, and level of emotional closeness were not significantly associated with KEC scores.
Multivariate Predictors of KPE Concerns
Results of the multivariable regression model indicate that male gender (unstandardized coefficient B=−9.71, t=4.5, P<0.001) and more health care system distrust (higher HCSD total score) (unstandardized coefficient B=0.30, t=2.5, p=0.01) were significant predictors of more KPE concerns for former potential LDs, accounting for 18% of the variance in KPE concerns. For intended recipients, black race (unstandardized coefficient B=4.82, t=2.1, P=0.04) and higher HCSD total score (unstandardized coefficient B=0.31, t=2.3, P=0.03) predicted more KPE concerns, accounting for 16% of the variance in KEC-R scores.
Common KPE Concerns
Former potential LDs and intended recipients shared several common KPE concerns.(Table 4) These concerns included waiting too long for KPE to occur, the intended recipient not receiving a transplant after their LD donates, life disruption caused by uncertain waiting period, kidney quality inequity, and financial burden for the LD, among others.
Table 4.
Most common KPE concerns† endorsed by potential living donors and intended recipients.
| Potential Living Donors (n = 135) | Intended Recipients (n = 83) | ||
|---|---|---|---|
| I was concerned that it would take too long before a swap would occur. (Inconvenience/Cost) | 60.7 (82) | I was concerned that I might end up not receiving a kidney transplant after my donor had donated their kidney. (Distrust/Inequity) | 57.8 (48) |
| I was concerned the person I wanted to donate to might end up not receiving a kidney after I donated. (Distrust/Inequity) | 55.6 (75) | I was concerned that I might end up with a kidney that was not as good as my donor’s kidney. (Distrust/Inequity) | 53.0 (44) |
| I was concerned that the person who I wanted to donate to might end up with a kidney that was not as good as mine. (Distrust/Inequity) | 51.9 (70) | I was concerned that I didn’t know anything about the person who would be giving me the kidney in the swap. (Distrust/Inequity) | 53.0 (44) |
| I was concerned that waiting too long in a swap program would be disruptive to my life. (Inconvenience/Cost) | 47.3 (64) | I was concerned that waiting too long in a swap program would be disruptive to my donor’s life. (Inconvenience/Cost) | 51.8 (43) |
| I was concerned that my costs as a kidney donor in a swap program would be too high. (Inconvenience/Cost) | 45.9 (62) | I was concerned that my donor would be uncomfortable with the idea that his/her kidney would go to someone other than me. (Uncertainty/Worry) | 49.4 (41) |
| I was concerned that the other donor in the swap would back out of it and then my family member or friend would not get a transplant. (Distrust/Inequity) | 45.2 (61) | I was concerned that my donor’s costs in a swap program would be too high. (Inconvenience/Cost) | 45.8 (38) |
| I was uncomfortable with the idea that my kidney would go to someone other than the person I wanted to donate to. (Uncertainty/Worry) | 40.7 (55) | I was concerned that my donor would feel more pressure to go through with donation if it was part of a swap. (Uncertainty/Worry) | 45.8 (38) |
| I was concerned that I would have to travel to a different transplant center for my surgery. (Inconvenience/Cost) | 39.3 (53) | I was concerned that the other donor in the swap would back out of it and then I would not get a transplant. (Distrust/Inequity) | 45.8 (38) |
| I was concerned that I didn’t know anything about the person who would be getting my kidney in the swap. (Distrust/Inequity) | 39.3 (53) | I was concerned that the person who would be getting my donor’s kidney in the swap would not take good care of it. (Distrust/Inequity) | 45.8 (38) |
| I was willing to accept the risks of donation for someone I know, but not for a stranger. (Distrust/Inequity) | 39.3 (53) | I was concerned that my donor would not approve of taking part in a kidney swap program. (Uncertainty/Worry) | 43.4 (36) |
Data are expressed as percentage (n) of potential living donors and intended recipients who agreed or strongly agreed with the concern on the KEC-D and KEC-R, respectively. Corresponding subscale is noted in parentheses.
DISCUSSION
Despite the emergence of several multi-center registries, a national program facilitated by UNOS, and a few large single-center programs,[4,5,8,9,11,24] KPE adoption rates remain low and little is known about the specific concerns that may influence KPE willingness by incompatible donor-recipient pairs. The present study contributes three primary findings to the extant KPE literature: (1) the development of two questionnaires that can be used to quantitatively measure KPE concerns, one for potential LDs and one for intended recipients, (2) KPE concerns may be more prevalent in certain subgroups of LDs and patients, including men, blacks, and those with more distrust of the health care system, and (3) the most common KPE concerns endorsed by former incompatible potential LDs and recipients are characterized by distrust, inequity, inconvenience, and cost. Collectively, these findings lay the foundation for further scientific inquiry and the development of targeted interventions to more effectively engage incompatible donor-recipient pairs in the KPE process.
Two-thirds of former potential LDs and intended recipients in this study were unwilling to pursue possible KPE after learning of incompatibility. These individuals had more concerns about various aspects of the KPE process, relative to those who were willing to pursue KPE. This level of KPE unwillingness is much higher than what has been reported by others [14–17,25], yet it is generally consistent with our program’s experience over the last several years. We have a small to moderate size transplant program (average of 63 kidney transplants annually) that enrolls only a few incompatible donor-recipient pairs into the UNOS KPD Program each year, despite having a multi-modal approach to KPE educational (i.e., KPE discussions pre- and post-compatibility testing, written materials, opportunity to speak to former KPE recipients/LDs, etc.). Our LD nurse coordinator estimates that two-thirds of potential LDs express interest in KPE upon being informed of incompatibility, but few follow through with additional donor testing. Learning of one’s incompatibility with the intended recipient may be a disappointment to many potential LDs, but others may be privately relieved to learn they are not a compatible match. This is supported by our finding that 24% and 25% of potential LDs and intended recipients, respectively, indicated on the KEC questionnaire that they were relieved not to be a compatible match with the recipient/donor (data not shown). The KPE option may cause some incompatible potential LDs to feel that they can no longer “back out” of donation, a concern that is not lost on intended recipients in our study. Nearly half of them expressed concern about their potential LD feeling more pressure to go through with donation if part of KPE.
Distrust, potential inequities, and inconvenience were prominent concerns expressed by both former potential LDs and intended recipients. This finding should not be surprising to the transplant community. KPE is very complex and characterized by many moving parts, which require exquisite coordination for seamless and successful execution. It is challenging even for transplant professionals, let alone incompatible donor-recipient pairs, to have unwavering trust and faith in the process. Waterman et al.[15] reported that one-third (34%) of ruled-out LDs were unwilling to participate in KPE because they were concerned that the intended recipient might not receive a kidney in exchange for their donation. We found an even higher rate of concern, from both potential LDs (56%) and intended recipients (58%), about the intended recipient not receiving a kidney in a KPE. Additionally, there was a high level of concern about disparate kidney quality in an exchange, something not assessed as part of the Waterman et al.[15] study. The inconvenience of not being able to plan when donation will occur and the disruption this may cause in the potential LD’s life appear to be of high concern for both the LD and intended recipient.
Proper KPE education of potential LDs and patients requires not only a description of the process, but also a discussion of how the transplant community has addressed issues of inequity, established guidelines on the evaluation and selection of LDs, and made changes in KPE process to enhance convenience and reduce cost for LDs (e.g., shipping kidneys, setting parameters regarding travel, etc.).[8,11,24] Failure to adequately address these concerns and to enhance transparency, particularly as KPE increases in complexity, is likely to place additional downward pressure on rates of KPE participation among those with general distrust of the health care system, minorities, and men – subgroups Segev et al.[14] found to be less willing to participate in KPE and that we found to have more KPE-specific concerns.
Interestingly, neither donor-recipient relationship type nor perceived emotional closeness was associated with KPE willingness or concerns. This differs from some earlier findings, in which close family members were more willing to pursue KPE.[15] However, all but one of the KPEs reflected in our sample were completed by a LD who was a biological relative or spouse of the intended recipient. Thus, it is possible that relatives and spouses have the same level of KPE concern as friends and other non-relatives, yet they may engage in a process that helps to remove these concerns as barriers to KPE participation. For instance, Ratner et al.[25] found that most LDs and recipients felt that the decision to participate in KPE should be made together and that each was more willing to engage in the KPE process if they knew the other was enthusiastic about it. Perhaps potential LDs and intended recipients are more likely to discuss KPE with each other if they are related or spouses, thus enabling them to evaluate each other’s KPE interest and willingness. The donor-recipient communication processes surrounding KPE represents a potentially important focus of future study.
Study findings should be evaluated in the context of several important limitations. Data were collected at a single center that performs a small number of KPE transplants annually. Our KPE-related processes may differ from other centers, particularly those with higher volume and greater KPE participation, which limits the generalizability of the findings. Also, KPE concerns were assessed retrospectively, several months or years after initial evaluation and a final donation disposition. Thus, it is possible that memory and decision justification biases influenced responses. Since we did not ask respondents to indicate when they were initially evaluated, we were not able to examine the association between KPE concerns and passage of time. While study participation rates were moderately high for survey-based research, there is inherent selection bias in a survey study, i.e., the KPE concerns of study participants may differ systematically from those who chose not to take part in the study. Since the data were anonymous, we were unable to compare survey responders and non-responders. We examined the relationship between KPE concerns and sociodemographic characteristics, but there are other factors we did not assess that may be related to KPE willingness and concerns, including the intended recipient’s time on the waiting list and quality of life, the potential LD’s financial resources and understanding of the allocation system, and whether the potential LD and/or intended recipient participated in other studies designed to increase LDKT rates at our center.[26] While these instruments show preliminary evidence of convergent and discriminant validity and acceptable internal consistency, further study with larger, more diverse samples is necessary. Larger samples would allow researchers to assess (e.g., using factor analysis) the empirical validation of the three conceptually-derived subscales reported in this study. Finally, this study focused on the more traditional 2-way simultaneous KPE. More research is needed to determine whether similar concerns exist in the context of altruistic unbalanced KPE, compatible pair exchanges, and large cycle exchanges.[8,16,17]
In conclusion, we identified KPE concerns that may adversely impact KPE participation rates among potential LDs and intended recipients. Particularly noteworthy are common concerns associated with distrust, inequity, inconvenience, and cost. Future studies are needed to further quantify the relative significance of these concerns in KPE willingness, using larger and more diverse samples across multiple centers. The two questionnaires developed for this study may be useful in assessing KPE concerns in potential donor-recipient pairs. Quantification of the KPE uptake rate nationally, exploration of the relationship between KPE willingness and actual KPE enrollment, and further description of KPE concerns that may affect participation is essential to help guide the development and evaluation of targeted educational interventions designed to optimize KPE willingness and participation. Even a modest incremental increase in KPE participation of 10% to 15% would allow for more LDKTs to be performed.
Acknowledgments
We are thankful for the assistance provided by Tracy Brann, Betsy Gray-Chrzan, Jodi Dattadeen, Aaron Fleishman, Alexa Hiley, Maeve Moore, Suchie Ravindran, Hongying Tang, Denny Tsai, and Linda Walsh in the conduct of this study.
This study was supported by Award No. R01DK085185 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health. Preparation of this manuscript was also supported, in part, by the Julie Henry Research Fund and the Center for Transplant Outcomes and Quality Improvement, The Transplant Institute, Beth Israel Deaconess Medical Center, Boston, MA.
Abbreviations
- HCSD
Revised Health Care System Distrust
- HLA
Human Leukocyte Antigen
- KEC-D
Kidney Exchange Concerns – Donor
- KEC-R
Kidney Exchange Concerns – Recipient
- KPD
Kidney Paired Donation
- KPE
Kidney Paired Exchange
- LD
Living Donor
- LDKT
Live Donor Kidney Transplantation
- NEPKE
New England Paired Kidney Exchange
- OTTR
Organ Transplant Tracking Record
Footnotes
Authorship: Study design: JR, RL, TV, AE, DM, Measurement development: JR, RL, TV, AE, DM, Study oversight: JR, TV, Study implementation/data collection: JR, TV, Data analysis/interpretation: JR, RL, TV, DM, Manuscript preparation: JR, RL, TV, AE, DM
Conflicts: The authors have no conflicts of interest to disclose.
Copies of the two Kidney Exchange Concerns questionnaires are available from the first author upon request.
References
- 1.Zenios SA, Woodle ES, Ross LF. Primum non nocere: avoiding harm to vulnerable wait list candidates in an indirect kidney exchange. Transplantation. 2001;72:648. doi: 10.1097/00007890-200108270-00015. [DOI] [PubMed] [Google Scholar]
- 2.Kaplan I, Houp JA, Montgomery RA, et al. A computer match program for paired and unconventional kidney exchanges. Am J Transplant. 2005;5:2306. doi: 10.1111/j.1600-6143.2005.00991.x. erratum in: Am J Transplant 2005; 5: 2597. [DOI] [PubMed] [Google Scholar]
- 3.Saidman SL, Roth AE, Sönmez T, et al. Increasing the opportunity of live kidney donation by matching for two- and three-way exchanges. Transplantation. 2006;81:773. doi: 10.1097/01.tp.0000195775.77081.25. [DOI] [PubMed] [Google Scholar]
- 4.Aull MJ, Kapur S. Kidney paired donation and its potential impact on transplantation. Surg Clin North Am. 2013;93:1407. doi: 10.1016/j.suc.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Gentry S, Segev DL. Living donor kidney exchange. Clin Transpl. 2011:279. [PubMed] [Google Scholar]
- 6.Rodrigue JR, Schold JD, Mandelbrot DA. The decline in living kidney donation in the United States: random variation or cause for concern? Transplantation. 2013;96:767. doi: 10.1097/TP.0b013e318298fa61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Organ Procurement and Transplantation Network (OPTN) [Data accessed April 14, 2014]; http://optn.transplant.hrsa.gov/latestData/rptData.asp.
- 8.Gentry SE, Montgomery RA, Segev DL. Kidney paired donation: fundamentals, limitations, and expansions. Am J Kidney Dis. 2011;57:144. doi: 10.1053/j.ajkd.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Massie AB, Gentry SE, Montgomery RA, Bingaman AA, Segev DL. Center-level utilization of kidney paired donation. Am J Transplant. 2013;13:1317. doi: 10.1111/ajt.12189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clark E, Hanto R, Rodrigue JR. Barriers to implementing protocols for kidney paired donation and desensitization: survey of U.S transplant programs. Prog Transplant. 2010;20:357. doi: 10.1177/152692481002000409. [DOI] [PubMed] [Google Scholar]
- 11.Melcher ML, Blosser CD, Baxter-Lowe LA, et al. Dynamic challenges inhibiting optimal adoption of kidney paired donation: findings of a consensus conference. Am J Transplant. 2013;13:851. doi: 10.1111/ajt.12140. [DOI] [PubMed] [Google Scholar]
- 12.Mast DA, Vaughan W, Busque S, et al. Managing finances of shipping living donor kidneys for donor exchanges. Am J Transplant. 2011;11:1810. doi: 10.1111/j.1600-6143.2011.03690.x. [DOI] [PubMed] [Google Scholar]
- 13.Rees MA, Schnitzler MA, Zavala EY, et al. Call to develop a standard acquisition charge model for kidney paired donation. Am J Transplant. 2012;12:1392. doi: 10.1111/j.1600-6143.2012.04034.x. [DOI] [PubMed] [Google Scholar]
- 14.Segev DL, Powe NR, Troll MU, et al. Willingness of the United States general public to participate in kidney paired donation. Clin Transplant. 2012;26:714. doi: 10.1111/j.1399-0012.2012.01596.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waterman AD, Schenk EA, Barrett AC, et al. Incompatible kidney donor candidates’ willingness to participate in donor-exchange and non-directed donation. Am J Transplant. 2006;6:1631. doi: 10.1111/j.1600-6143.2006.01350.x. [DOI] [PubMed] [Google Scholar]
- 16.Ackerman PD, Thistlethwaite JR, Jr, Ross LF. Attitudes of minority patients with end-stage renal disease regarding ABO-incompatible list-paired exchanges. Am J Transplant. 2006;6:83. doi: 10.1111/j.1600-6143.2005.01122.x. [DOI] [PubMed] [Google Scholar]
- 17.Kranenburg LW, Zuidema W, Weimar W, et al. One donor, two transplants: Willingness to participate in altruistically unbalanced exchange donation. Transpl Int. 2006;19:995. doi: 10.1111/j.1432-2277.2006.00378.x. [DOI] [PubMed] [Google Scholar]
- 18.Purnell TS, Powe NR, Troll MU, et al. Measuring and explaining racial and ethnic differences in willingness to donate live kidneys in the United States. Clin Transplant. 2013;27:673. doi: 10.1111/ctr.12196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hanto RL, Reitsma W, Delmonico FL. The development of a successful multiregional kidney paired donation program. Transplantation. 2008;86:1744. doi: 10.1097/TP.0b013e3181909035. [DOI] [PubMed] [Google Scholar]
- 20.Shea JA, Micco E, Dean LT, McMurphy S, Schwartz JS, Armstrong K. Development of a revised Health Care System Distrust scale. J Gen Intern Med. 2008;23:727. doi: 10.1007/s11606-008-0575-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schenker Y, White DB, Asch DA, Kahn JM. Health-care system distrust in the intensive care unit. J Crit Care. 2012;27:3. doi: 10.1016/j.jcrc.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang TC, Matthews SA, Hillemeier MM. Effect of health care system distrust on breast and cervical cancer screening in Philadelphia, Pennsylvania. Am J Public Health. 2011;101:1297. doi: 10.2105/AJPH.2010.300061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ozawa S, Sripad P. How do you measure trust in the health system? A systematic review of the literature. Soc Sci Med. 2013;91:10. doi: 10.1016/j.socscimed.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 24.Wallis CB, Samy KP, Roth AE, Rees MA. Kidney paired donation. Nephrol Dial Transplant. 2011;26:2091. doi: 10.1093/ndt/gfr155. [DOI] [PubMed] [Google Scholar]
- 25.Ratner LE, Rana A, Ratner ER, et al. The altruistic unbalanced paired kidney exchange: proof of concept and survey of potential donor and recipient attitudes. Transplantation. 2010;89:15. doi: 10.1097/TP.0b013e3181c626e1. [DOI] [PubMed] [Google Scholar]
- 26.Rodrigue JR, Pavlakis M, Egbuna O, Paek M, Waterman AD, Mandelbrot DA. The “house calls” trial: a randomized controlled trial to reduce racial disparities in live donor kidney transplantation: rationale and design. Contemp Clin Trials. 2012;33:811. doi: 10.1016/j.cct.2012.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]