Abstract
Objective
Isolated Iliac artery aneurysms are rare, but potentially fatal. The impact of recent trends in the utilization of endovascular iliac aneurysm repair (EVIR) on isolated iliac artery aneurysm-associated mortality is unknown.
Methods
We identified all patients with a primary diagnosis of iliac artery aneurysm in the NIS from 1988 to 2011. We examined trends in management (open vs. EVIR, elective and urgent) and overall isolated iliac artery aneurysm related deaths (with or without repair). We compared in-hospital mortality and complications for the subgroup of patients undergoing elective open and EVIR from 2000-2011.
Results
We identified 33,161 patients undergoing isolated iliac artery aneurysm repair from 1988-2011: of which there were 9,016 EVIR and 4,933 open elective repairs from 2000-2011. Total repairs increased after introduction of EVIR from 28 to 71 per 10M US population (P<.001). EVIR surpassed open repair in 2003. Total isolated iliac artery aneurysm-related deaths, due to rupture or elective repair, decreased after the introduction of EVIR (4.4 to 2.3 per 10M US population, P<.001). However, urgent admissions have not decreased over this time period (15 to 15 procedures per 10M US population, P=0.30). Among elective repairs after 2000, EVIR patients were older (72.4 vs. 69.4 years, P=0.002) and were more likely to have a history of prior MI (14.0% vs. 11.3%, P<.001) and renal failure (7.2% vs. 3.6%, P<.001). Open repair had significantly higher in-hospital mortality (1.8% vs. 0.5%, P<0.001) and complications (17.9% vs. 6.7%, P<0.001), and a longer length of stay (6.7 vs. 2.3 days, P<0.001).
Conclusions
Treatment of isolated iliac artery aneurysm has increased since the introduction of EVIR and is associated with lower perioperative mortality, despite a higher burden of comorbid illness. Decreasing iliac artery aneurysm-attributable in-hospital deaths are likely related primarily to lower elective mortality with EVIR rather than rupture prevention.
Introduction
Comprising approximately 2% of all abdominal aneurysms,1-4 isolated iliac artery aneurysms are uncommon, are frequently asymptomatic, and are most often discovered incidentally.2, 5, 6 When ruptured, however, these aneurysms carry significant risk of mortality.2, 3, 7
Historically, open repair has been the primary treatment, however, given the pelvic location, this may be technically challenging and lead to complications. 2, 3 Therefore, treatment with endovascular techniques has become particularly appealing with good early- and mid-term results.1, 2, 8-12 Reported operative mortality rates with elective open and endovascular repair are 3-6% and 0-1%, respectively.1-4, 6, 9, 13, 14 However, the majority of these studies are from single institutions with small sample sizes The purpose of this national study is to identify epidemiologic trends in management and mortality for isolated iliac artery aneurysm and to evaluate the impact of the introduction of endovascular iliac aneurysm repair (EVIR) in the United States.
Methods
Dataset
All patients with an isolated iliac artery aneurysm from 1988 through 2011 were extracted from the Nationwide Inpatient Sample (NIS) database. NIS is the largest US all-payer inpatient database and has been assembled as part of the Healthcare Cost and Utilization Project (HCUP). NIS represents a 20% stratified sample of all payer (insured and uninsured) hospitalizations and represents approximately eight million hospitalizations per year. These data contain sampling weights to approximate U.S. population estimates. All of our analyses were performed using weighted data. This study contained de-identified data only without any protected health information and is therefore not subject to patient consent or Institutional Review Board approval.
Patients
Using International Classification of Diseases, edition 9 (ICD9) diagnosis code 442.2, we identified all patients with a primary diagnosis (reason for admission) of iliac artery aneurysm undergoing open surgical repair (ICD9 procedure codes 38.06, 38.16, 38.36, 38.46, 38.66, 38.86, 39.25, 39.52) or EVIR (39.71, 39.79, 39.90) in the Nationwide Inpatient Sample from 1988-2011. We excluded patients with concomitant diagnoses of aortic aneurysms (ICD9 diagnosis codes 441.3, 441.4, 441.9) as well as those with thoracic aneurysm and/or aortic dissection (ICD9 diagnosis codes 441.0, 441.1, 441.2, 441.5, 441.6, 441.7). Age, sex, race, and co-morbid conditions were documented, including diabetes mellitus (ICD9 diagnosis code 250.*), chronic obstructive pulmonary disease (ICD9 diagnosis codes 491.*, 492.*, 496.), congestive heart failure (ICD9 diagnosis code 428.*), prior myocardial infarction (ICD9 diagnosis code 412.), and hypertension (ICD9 diagnosis codes 401.*, 402.*, 403.*, 404.*, 405.*). Procedures were categorized as either elective or urgent. A specific ICD 9 code for ruptured iliac aneurysm does not exist.
Outcomes
We examined trends in total repairs and overall isolated iliac artery aneurysm related deaths per ten million citizens of the Unites States, including the percentage of EVIR vs. open repairs. We analyzed elective repairs, urgent repairs, and hospitalizations for isolated iliac artery aneurysm without repairs resulting in death. We compared in-hospital deaths and postoperative complications after elective open repair and EVIR from 2000-2011, to create contemporaneous, comparable cohorts. Our primary outcome was mortality. We also examined post-operative complications, including cardiac complications, respiratory complications, postoperative wound infection, and hematoma. We also analyzed discharge status, and length of stay.
Statistical Analysis
Statistical analysis was completed with SPSS statistical software (version 20; IBM Corp, Armonk, NY). When appropriate, continuous variables were compared using two-tailed independent samples t-test and categorical variable were compared using Chi-squared. A Cochran-Armitage test for linear trend was performed to assess for changes in death and repairs over time. Statistical significance was defined as p < 0.05.
Results
EPIDEMIOLOGIC TRENDS
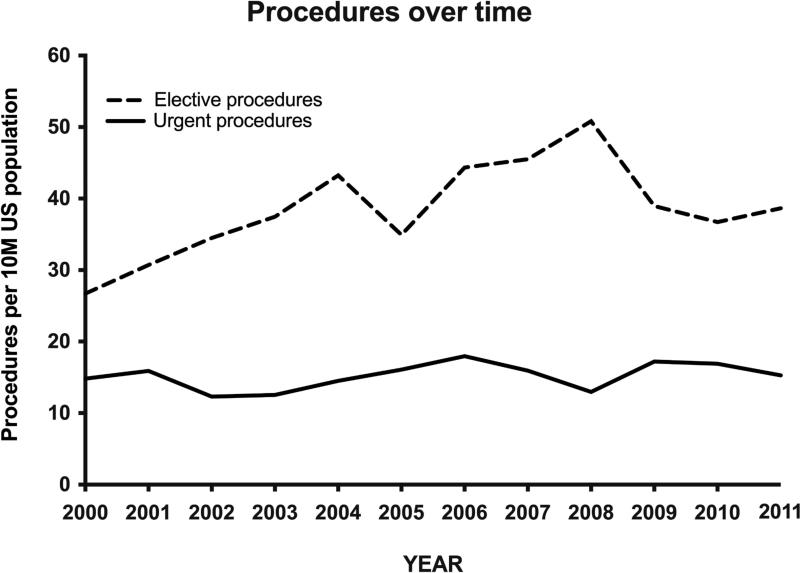
We identified 33,161 patients undergoing isolated iliac artery aneurysm repair, including elective and urgent procedures, from 1988 to 2011. Endovascular repairs increased steadily over time and surpassed open repair in 2003. (Figure 1) The overall rate of repair increased after introduction of EVIR from 28 to 71 repairs per 10 million of the US population (P<.001). Total deaths, including non-operative deaths, decreased after the introduction of EVIR, from 4.4 to 2.3 deaths per 10 million of the US population (P<.001). Deaths due to isolated iliac artery aneurysm over time are demonstrated in Figure 2. Of all deaths in 2011, 73% were after open repair, despite the fact that open repair only made up only 20% of total isolated iliac artery aneurysm repairs in 2011. In-hospital mortality with open surgery and EVIR over time is shown in Figure 3. Operative mortality, for elective and urgent repairs, decreased from 13.4% to 2.4%, with an overall death rate of 1.8% in 2011. The number of urgent procedures, shown in Figure 4, has remained stable over time (from 15 to 15 procedures per 10 million of the US population, P=0.30).
Figure 1.
Elective and urgent procedures over time, per 10 million U.S. population.
Figure 2.
Elective and urgent deaths over time, per 10 million US population.
Figure 3.
In-hospital mortality for all isolated iliac aneurysm repairs (elective and urgent) over time.
Figure 4.
Elective and urgent procedures over time, per 10 million US population.
ELECTIVE EVIR VS. OPEN REPAIR 2000-2011
We identified 13,949 patients who underwent elective repair from 2000 to 2011 after excluding 5,426 patients who underwent urgent repair; there were 4,933 (35%) open surgical repairs and 9,016 (65%) EVIR. For elective repairs, EVIR patients were older (72.4 vs. 69.4 years, P=.002), and were more likely to have a history of MI (14.0% vs. 11.3%, P<.001) and CRF (7.2% vs. 3.6%, P<.001) than patients undergoing open repair. (Table 1)
Table I.
Baseline characteristics for elective endovascular and open isolated Iliac Artery Aneurysm Repair from 2000-2011
| Pre-operative Comorbidities | EVIR N=9016 | Open repair N=4933 | P-value |
|---|---|---|---|
| Age | 72 | 69 | 0.002 |
| Coronary Artery Disease | 43% | 37% | <.001 |
| Hypertension | 64% | 57% | <.001 |
| Dysrhythmia | 4.3% | 7.2% | <.001 |
| Prior MI | 14% | 11% | <.001 |
| Heart Failure | 8.8% | 7.3% | 0.003 |
| COPD | 19% | 22% | 0.002 |
| Afib | 13% | 13% | 0.111 |
| Acute Renal Failure | 1.8% | 4.8% | <.001 |
| Chronic Renal Failure | 7.2% | 3.6% | <.001 |
| CVD | 2.1% | 2.5% | 0.202 |
| PVD | 24% | 24% | 0.722 |
| Hyperlipidemia | 39% | 31% | <.001 |
Patients undergoing elective open repair had higher in-hospital mortality than EVIR (1.8% vs. 0.5%, P<.001). (Table 2) For urgent procedures from 2000 to 2011 the in-hospital mortality was 7.5% for open repair vs. 1.1% for EVIR (P<.001) In addition, elective open repair had higher rates of overall postoperative complications (17.9% vs. 6.7%, P<.001): including cardiac complications (3.3% vs. 1.2%, P<.001), respiratory complications (9.2% vs. 1.4%, P<.001), wound dehiscence (0.8% vs. 0.2%, P<.001 ), and wound infections (10.% vs. 0.3%, P<.001). Patients undergoing open repair had a median length of stay of 6.7 days versus 2.3 days (P<.001) in the EVIR group.
Table II.
Post-operative Outcomes following elective endovascular and open repair of isolated Iliac artery aneurysms from 2000-2011.
| Post-operative Outcomes | EVIR N=9016 | Open repair N=4933 | P-value |
|---|---|---|---|
| In-hospital Mortality | 0.5% | 1.8% | <.001 |
| Cardiac complications | 1.2% | 3.3% | <.001 |
| Respiratory complications | 1.4% | 9.2% | <.001 |
| Peripheral vascular complications | 1.0% | 1.4% | 0.022 |
| Wound dehiscence | 0.2% | 0.8% | <.001 |
| Bleeding complications | 3.2% | 5.7% | <.001 |
| Infection | 0.3% | 1.0% | <.001 |
| Post-operative complications | 6.7% | 17.9% | <.001 |
| Length of Stay (days) | 2.3 | 6.7 | <.001 |
Discussion
We studied trends over the period 1988-2011 and found that the treatment of isolated iliac artery aneurysm has dramatically increased over time since the introduction of EVIR. EVIR is currently the dominant treatment method for isolated iliac artery aneurysm and is associated with lower morbidity, mortality and shorter length of stay, despite more comorbid illness. Deaths from isolated iliac artery aneurysm have decreased over time, despite the increase in total repairs. Similar to the trend seen in abdominal aortic aneurysm (AAA) repair,15, 16 treatment of isolated IAA has shifted away from open surgical repair towards a less invasive endovascular technique. The total number of isolated iliac artery aneurysm repairs has increased with the introduction of EVIR, likely in part due to increased detection related to increased utilization of abdominal imaging over time.17 However, unlike what was seen with AAA, the increase in elective procedures may not have lead to a decrease in urgent procedures over time. This suggests that the increase in elective procedures may be primarily related to a lower threshold for intervention with availability of a less invasive treatment. The decrease in isolated iliac artery aneurysm inhospital deaths over time is likely related to the reduction in elective mortality, similar to trends observed in AAA treatment.15, 16 However, there may not be a reduction in deaths due to rupture prevention. Unfortunately, unlike AAA, there is no specific ICD9 code for rupture and we can only extrapolate from the number of emergent admissions.
Currently, the existing guidelines recommend intervention at a diameter of >3cm for iliac artery aneurysms.18 A study by Santilli et al and a recent survey study by Williams et al. suggest that it is safe to wait until the common iliac diameter is 4cm before intervention.19, 20 However, our data do not include diameter nor do they distinguish the common iliac artery from the hypogastric iliac artery. Therefore they do not support treatment of smaller iliac aneurysms. They simply reflect the impact of current utilization trends.
Prior studies have demonstrated 30-day mortality-rates ranging between 4-6% for open repair and 0-2% for endovascular repair.1, 2, 4, 21 We found comparable mortality-rates of 1.8% for open repair and 0.5% for endovascular repair; however, the NIS contains data for only in-hospital mortality instead of 30-day mortality, which was reported in the prior publications. In a study of abdominal aneurysm repair using Medicare data we found an in-hospital mortality of 4.6% and 1.1% and a 30-day mortality of 4.8% and 1.6% for open and endovascular repair respectively. Thus, 96% of 30-day deaths after open repair occurred during the initial inpatient stay compared to only 69% of EVAR deaths. We expect this overestimation of the benefit of endovascular repair using inpatient mortality alone to be present to a similar extent in isolated iliac artery aneurysm patients.22 Prior literature shows hospital stays of 2-3 days for endovascular patients, and 5-9 days for open repair patients similar to our findings.2, 3, 9
An important caveat is that our study is not a randomized controlled trial, but an observational study of administrative data, which is subject to coding errors and selection bias. To improve the comparison of open surgery and EVIR for the more recent years (2000-2011), we excluded all patients who underwent an urgent procedure since these patients were more likely to have an open repair and were more likely to have adverse outcomes. Administrative studies lack anatomic and clinical details, which could impact patient selection and outcomes. As noted, our study lacks data regarding iliac artery diameters, and we cannot distinguish hypogastric from common iliac arteries. We were unable to distinguish the precise type of endovascular repair due to a lack of specificity of ICD9 codes. Additionally, this database lacks long-term follow-up data including reinterventions, late rupture, and buttock claudication. However, late ruptures that present to the hospital would potentially be captured as another admission. Despite these limitations the strengths of this database are the large numbers with national representation and the ability to demonstrate national trends in utilization and mortality.
Conclusions
This study demonstrates that repair of isolated iliac artery aneurysm across the U.S. is increasing. Overall deaths due to isolated iliac artery aneurysms are decreasing, despite the increase in repair rates, related to the increased use of EVIR with its lower operative mortality. It remains to be seen whether there has been any decrease in deaths due to rupture prevention.
Acknowledgments
Supported by grant 5R01HL105453-03 from the NHLBI and the NIH T32 Harvard-Longwood Research Training in Vascular Surgery grant HL007734.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the SVS 2014 Vascular Annual Meeting held on June 4-7 in Boston, MA.
References
- 1.Huang Y, Gloviczki P, Duncan AA, Kalra M, Hoskin TL, Oderich GS, et al. Common iliac artery aneurysm: expansion rate and results of open surgical and endovascular repair. J Vasc Surg. 2008;47(6):1203–10. doi: 10.1016/j.jvs.2008.01.050. discussion 10-1. [DOI] [PubMed] [Google Scholar]
- 2.Patel NV, Long GW, Cheema ZF, Rimar K, Brown OW, Shanley CJ. Open vs. endovascular repair of isolated iliac artery aneurysms: A 12-year experience. J Vasc Surg. 2009;49(5):1147–53. doi: 10.1016/j.jvs.2008.11.101. [DOI] [PubMed] [Google Scholar]
- 3.Chaer RA, Barbato JE, Lin SC, Zenati M, Kent KC, McKinsey JF. Isolated iliac artery aneurysms: a contemporary comparison of endovascular and open repair. J Vasc Surg. 2008;47(4):708–13. doi: 10.1016/j.jvs.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 4.Sandhu RS, Pipinos II. Isolated iliac artery aneurysms. Seminars in vascular surgery. 2005;18(4):209–15. doi: 10.1053/j.semvascsurg.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 5.Scheinert D, Schroder M, Steinkamp H, Ludwig J, Biamino G. Treatment of iliac artery aneurysms by percutaneous implantation of stent grafts. Circulation. 2000;102(19 Suppl 3):III253–8. doi: 10.1161/01.cir.102.suppl_3.iii-253. [DOI] [PubMed] [Google Scholar]
- 6.Chemelli A, Hugl B, Klocker J, Thauerer M, Strasak A, Jaschke W, et al. Endovascular repair of isolated iliac artery aneurysms. J Endovasc Ther. 2010;17(4):492–503. doi: 10.1583/10-3047.1. [DOI] [PubMed] [Google Scholar]
- 7.Uberoi R, Tsetis D, Shrivastava V, Morgan R, Belli AM, Subcommittee on Reporting Standards for Arterial Aneurysms of The Society for Vascular S Standard of practice for the interventional management of isolated iliac artery aneurysms. Cardiovascular and interventional radiology. 2011;34(1):3–13. doi: 10.1007/s00270-010-0055-0. [DOI] [PubMed] [Google Scholar]
- 8.Boules TN, Selzer F, Stanziale SF, Chomic A, Marone LK, Dillavou ED, et al. Endovascular management of isolated iliac artery aneurysms. J Vasc Surg. 2006;44(1):29–37. doi: 10.1016/j.jvs.2006.02.055. [DOI] [PubMed] [Google Scholar]
- 9.Pitoulias GA, Donas KP, Schulte S, Horsch S, Papadimitriou DK. Isolated iliac artery aneurysms: endovascular versus open elective repair. J Vasc Surg. 2007;46(4):648–54. doi: 10.1016/j.jvs.2007.05.047. [DOI] [PubMed] [Google Scholar]
- 10.Stroumpouli E, Nassef A, Loosemore T, Thompson M, Morgan R, Belli AM. The endovascular management of iliac artery aneurysms. Cardiovascular and interventional radiology. 2007;30(6):1099–104. doi: 10.1007/s00270-007-9133-3. [DOI] [PubMed] [Google Scholar]
- 11.Kim MD, Lee DY, Lee M, Won JY, Lee SJ, Kim IJ, et al. Single-center experience in the endovascular management of isolated iliac artery aneurysm. Acta radiologica. 2013 doi: 10.1177/0284185113496553. [DOI] [PubMed] [Google Scholar]
- 12.Fossaceca R, Guzzardi G, Di Terlizzi M, Divenuto I, Cerini P, Malatesta E, et al. Long-term efficacy of endovascular treatment of isolated iliac artery aneurysms. La Radiologia medica. 2013;118(1):62–73. doi: 10.1007/s11547-012-0813-1. [DOI] [PubMed] [Google Scholar]
- 13.Dorigo W, Pulli R, Troisi N, Alessi Innocenti A, Pratesi G, Azas L, et al. The treatment of isolated iliac artery aneurysm in patients with non-aneurysmal aorta. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2008;35(5):585–9. doi: 10.1016/j.ejvs.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 14.Ferreira J, Canedo A, Brandao D, Maia M, Braga S, Chaparro M, et al. Isolated iliac artery aneurysms: six-year experience. Interactive cardiovascular and thoracic surgery. 2010;10(2):245–8. doi: 10.1510/icvts.2009.218305. [DOI] [PubMed] [Google Scholar]
- 15.Giles KA, Pomposelli F, Hamdan A, Wyers M, Jhaveri A, Schermerhorn ML. Decrease in total aneurysm-related deaths in the era of endovascular aneurysm repair. J Vasc Surg. 2009;49(3):543–50. doi: 10.1016/j.jvs.2008.09.067. discussion 50-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schermerhorn ML, Bensley RP, Giles KA, Hurks R, O'Malley A J, Cotterill P, et al. Changes in abdominal aortic aneurysm rupture and short-term mortality, 1995-2008: a retrospective observational study. Annals of surgery. 2012;256(4):651–8. doi: 10.1097/SLA.0b013e31826b4f91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kocher KE, Meurer WJ, Fazel R, Scott PA, Krumholz HM, Nallamothu BK. National trends in use of computed tomography in the emergency department. Annals of emergency medicine. 2011;58(5):452–62. e3. doi: 10.1016/j.annemergmed.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 18.Moll FL, Powell JT, Fraedrich G, Verzini F, Haulon S, Waltham M, et al. Management of abdominal aortic aneurysms clinical practice guidelines of the European society for vascular surgery. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2011;41(Suppl 1):S1–S58. doi: 10.1016/j.ejvs.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Williams SK, Campbell WB, Earnshaw JJ. Survey of management of common iliac artery aneurysms by members of the Vascular Society of Great Britain and Ireland. Annals of the Royal College of Surgeons of England. 2014;96(2):116–20. doi: 10.1308/003588414X13814021676512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santilli SM, Wernsing SE, Lee ES. Expansion rates and outcomes for iliac artery aneurysms. J Vasc Surg. 2000;31(1 Pt 1):114–21. doi: 10.1016/s0741-5214(00)70073-5. [DOI] [PubMed] [Google Scholar]
- 21.Antoniou GA, Nassef AH, Antoniou SA, Loh CY, Turner DR, Beard JD. Endovascular treatment of isolated internal iliac artery aneurysms. Vascular. 2011;19(6):291–300. doi: 10.1258/vasc.2011.ra0050. [DOI] [PubMed] [Google Scholar]
- 22.Schermerhorn ML, Giles KA, Sachs T, Bensley RP, O'Malley AJ, Cotterill P, et al. Defining perioperative mortality after open and endovascular aortic aneurysm repair in the US Medicare population. Journal of the American College of Surgeons. 2011;212(3):349–55. doi: 10.1016/j.jamcollsurg.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]