Abstract
Objective
Manifestations of instability in knee OA include low overall knee confidence, low confidence that the knees will not buckle, buckling, and excessive motion during gait. Confidence and buckling may particularly influence activity choices, contributing to events leading to disability. Buckling is more likely to affect advanced than basic functional tasks. In this prospective, longitudinal study, we tested the hypotheses: overall knee confidence, buckling confidence, buckling, and frontal plane motion during gait are associated with advanced 2-year function outcome in persons with knee OA.
Methods
Persons with knee OA were queried about overall knee confidence (higher worse), buckling confidence, and knee buckling, and underwent quantitative gait analysis to quantify varus-valgus excursion and angular velocity. Physical function was assessed using the LLFDI Basic and Advanced Lower Extremity Domain scores. Logistic regression was used to evaluate the relationship between baseline instability measures and baseline-to-2-year function outcome, adjusting for potential confounders.
Results
212 persons (mean age 64.6 years, 76.9% women) comprised the sample. Buckling was significantly associated with poor advanced (adjusted OR 2.08, 95% CI: 1.03–4.20) but not basic function outcome. Overall knee confidence was significantly associated with advanced outcome (adjusted OR 1.65, 95% CI: 1.01–2.70), while associations between buckling confidence and both outcomes approached significance. Neither varus-valgus excursion nor angular velocity during gait was associated with either outcome.
Conclusion
Knee buckling and confidence were each associated with poor 2-year advanced function outcome. Current treatment does not address these modifiable factors; interventions to address them may improve outcome in knee OA.
INTRODUCTION
Knee instability in the setting of osteoarthritis (OA) encompasses a spectrum of symptoms and phenomena, including a feeling of low overall confidence in the knees (1), low confidence that the knees will not buckle (which we name buckling confidence), actual buckling [defined as the sudden loss of postural support across the weightbearing knee (2)], and excessive frontal plane motion objectively measured during weightbearing activity.
Given the central role of the knee in activity, instability may influence what an individual perceives she/he can do and chooses to do. Such choices may in turn influence which skills are maintained, aerobic capacity and conditioning, and ultimately the risk of disability. Via such paths, knee instability may impact quality of life in knee OA. Because lack of confidence may cause people with knee OA to alter activity to avoid buckling, evaluation of knee confidence provides an additional approach to capture buckling impact. Notably, self-reported knee instability and greater varus-valgus joint motion during gait were both associated with worse knee confidence in a recent study (3). In the instability spectrum, confidence and the memory of a buckling experience may particularly influence nature and intensity of activity. It is not known whether these variables are more important to outcome than instability measured during gait.
Whether buckling is associated with physical function decline is not known. An association between buckling and function has been described previously in cross-sectional studies (2, 4–7), precluding inferences about causal direction. These studies thus leave open the possibility that poor function and its consequences cause knee joint environment changes that lead to buckling. Whether buckling contributes to or is a consequence of function decline is important to elucidate: recent studies suggest it is frequent [e.g., as high as 67% in an OA sample (8)]; and current treatment for knee OA does little to address it or other aspects of instability (9, 10).
An optimal function measure to evaluate buckling impact must include tasks that have a reasonable likelihood of being limited by buckling. Basic tasks are emphasized in most knee OA function measures, e.g., in WOMAC (11): rising from sitting; standing; bending to floor; walking on flat ground; getting in/out of a car; putting on socks/stockings; rising from bed; lying in bed, etc. Buckling is unlikely to limit many of these tasks; it is possible that buckling impacts aspects of function that measures like WOMAC do not incorporate. In other words, buckling may have more impact on advanced (e.g., taking a 1-mile walk, hiking on uneven surfaces, going up and down stairs without a handrail) than basic functional tasks. To investigate this, we used the Late-Life Function and Disability Instrument (LLFDI), which uniquely enables scoring basic and advanced lower extremity function separately (see Appendix A for individual items) (12, 13).
The goals of this prospective, longitudinal study were to test the hypotheses that: overall knee confidence, buckling confidence, buckling, and excessive frontal plane motion during gait are each associated with advanced physical function outcome in persons with knee OA over a 2-year follow-up interval.
METHODS
Sample
Participants in this cohort study, the MAK-3 Study (Mechanical Factors in Arthritis of the Knee-Study 3), were recruited from the community via periodicals targeting older persons, neighborhood organizations, the Northwestern Buehler Center on Aging, Health, and Society registry, and medical center referrals. Inclusion criteria were: definite osteophyte presence [Kellgren/Lawrence (K/L) radiographic grade ≥ 2] in one or both knees; and Likert category of at least “a little difficulty” for 2 or more items in the WOMAC physical function scale. Exclusion criteria were: corticosteroid injection within the previous 3 months; history of avascular necrosis, rheumatoid or other inflammatory arthritis, periarticular fracture, Paget’s disease, villonodular synovitis, joint infection, ochronosis, neuropathic arthropathy, acromegaly, hemochromatosis, gout, pseudogout, osteopetrosis, or meniscectomy; or exclusion criteria for MRI. Approval was obtained from the Institutional Review Boards of Northwestern University and NorthShore University HealthSystem Evanston Hospital. Written consent was obtained from all participants.
Measurement of Overall Knee Confidence, Buckling Confidence, Buckling, and Frontal Plane Motion during Gait
Knee confidence was assessed using the KOOS quality of life subscale question: “How much are you troubled with lack of confidence in your knees?” (14) The KOOS is a valid, reliable, and responsive self-administered instrument, developed to evaluate short- and long-term symptoms and function in persons with knee injury and OA (14). In our previous pilot testing of this question, participants had difficulty distinguishing “severely” from “extremely”; therefore, we collapsed these responses into a single category: score 0 = not at all; 1 = mildly; 2 = moderately, 3 = severely or extremely (labeled “extremely” below) (higher score worse).
Buckling confidence was assessed separately for right and left knees using the question: “How confident are you that your knee will not buckle or give way?” Possible responses included not at all, mildly confident, moderately confident, and extremely confident (score 0–3, higher score better). Both for this question and the ascertainment of buckling (see below), the following definitions, adapted from those in the Cincinnati Knee Rating Scale (15), were provided within standardized instructions: “by knee buckling or giving way, we mean a partial knee collapse with no fall to the ground or a knee collapse with actual falling to the ground.” Buckling confidence was analyzed as a person-level variable, using the worse score of the 2 knees.
To assess reliability, prior to this study, we interviewed 26 MAK-3 cohort members on 2 occasions, one week apart, asking all KOOS quality of life subscale questions and the buckling confidence question. For inter-session reliability, we analyzed responses on the two occasions using weighted kappa coefficients with quadratic weights. The coefficients were 0.84 for knee confidence and 0.81 for buckling confidence, suggesting excellent agreement for each.
To ascertain buckling, we used questions developed for the Framingham Osteoarthritis Study (2): “Has your knee buckled or given way at least once in the past 3 months (yes or no)? Which knee buckled or gave way at least once (right, left, both, don’t know)?” We analyzed buckling as a person-level variable, i.e., defined by occurrence in one or both knees.
Frontal plane knee instability was assessed at self-selected speed with personal gym shoes. An eight camera Eagle Digital Real-Time motion measurement system (Motion Analysis Corporation, Santa Rosa, CA) was used to capture three-dimensional motion data at a sampling rate of 120 Hz. Six AMTI (Advanced Mechanical Technology Inc., Watertown, MA, USA) force platforms flush with the floor were used to measure ground reaction forces at a sampling rate of 960 Hz. At least five trials with clean foot strikes on the platforms for the left and right feet were collected and averaged. External passive reflective markers were placed bilaterally by an experienced examiner [modified Helen Hayes full-body marker set (16)]. OrthoTrak gait analysis software was used. Knee angular velocity was computed as the time derivative of the frontal plane knee angle; maximal velocity in either varus or valgus direction, higher of the 2 knees, was used in analysis. Knee varus-valgus excursion was measured as distance between peak varus and peak valgus angles during stance; higher of the 2 knees was analyzed. To assess reliability, the examiner placed markers on ten persons, five with knee OA, collected data for five trials at self-selected speed, removed markers, gave a rest period, reapplied markers, and collected data for another five trials. A two-way mixed model ANOVA with repeated measures and the ICC for single measures revealed excellent reliability: right and left heel strike varus/valgus angle ICCs 0.99 and 0.98; right and left maximum varus ICCs 0.99 and 0.99; right and left maximum valgus ICCs 0.98 and 0.99.
Measurement of Covariables
Body mass index (BMI) was calculated as weight in kg divided by height in meters squared. Function self-efficacy was assessed using the Arthritis Self-Efficacy Scale function subscale (self-rating of certainty in one’s ability to walk 100 feet in 20 seconds, walk 10 steps downstairs in 7 seconds, and get out of an armless chair without using hands for support) (higher better) (17). Construct and concurrent validity and test–retest reliability for the subscales have been demonstrated in persons with arthritis (17). Depressive symptoms were assessed using the 15-item version of the Geriatric Depression Scale with demonstrated strong psychometric properties (18). Knee extensor strength during movement (average peak torque corrected for body weight, N-M/kg) was assessed isokinetically at 120°/second, using a computer-driven isokinetic dynamometer (Biodex System 3, Biodex Corporation, Shirley, NY) by a single tester. The value for the knee with worse buckling confidence was used in analysis. Participants underwent bilateral, anteroposterior, weightbearing knee radiographs in the semi-flexed position with fluoroscopic confirmation of anterior and posterior tibial plateau line superimposition and tibial spine centering within the femoral notch (19). Disease severity was assessed using the K/L system: 0 = normal; 1 = possible osteophytes; 2 = definite osteophytes, possible joint space narrowing; 3 = moderate osteophytes, definite joint space narrowing, some sclerosis, possible attrition; and 4 = large osteophytes, marked joint space narrowing, severe sclerosis, and definite attrition. The value for the more diseased knee was used in analysis. Knee pain severity was measured using the Intermittent and Constant Osteoarthritis Pain (ICOAP) instrument, a valid and reliable multidimensional measure designed to comprehensively evaluate the pain experience in persons with knee or hip OA (20, 21).
Assessment of Outcome
Physical function was assessed at baseline and 2 years later using the LLFDI Advanced Lower Extremity Domain scaled score and the LLFDI Basic Lower Extremity Domain scaled score (12, 13, 22). The function component of the Late-Life Function and Disability Instrument assesses difficulty in completing specific physical tasks or actions, both basic and more advanced (Appendix A). The instrument was constructed using factor analysis and Rasch analytic techniques, and its validity and test-retest reliability have been evaluated in ethnically and racially diverse older adults who had a range of functional limitations and chronic health conditions (12, 13).
To characterize the baseline to 2-year function experience of each participant, quintile-defined groups were used. For the basic function outcome, participants were categorized by LLFI Basic Lower Extremity Domain scaled score quintile derived from the cohort at baseline, ranging from worst to best function, as follows: first quintile (<60.92); second quintile (≥60.92 and <67.24); third quintile (≥67.24 and <74.31); fourth quintile (≥74.31 and <81.17); and fifth quintile (≥81.17). For the advanced function outcome, participants were categorized by LLFI Advanced Lower Extremity Domain scaled score quintile derived from the cohort at baseline, ranging from worst to best function: first quintile (<42.81); second quintile (≥42.81 and <51.68); third quintile (≥51.68 and <58.18); fourth quintile (≥58.18 and <67.07); and fifth quintile (≥67.07). For both outcomes, poor outcome was defined as remaining within the same low functioning group (the two worst groups) or moving into a worse function group at 2-year follow-up.
Statistical Analysis
All analyses were based on person-level variables (see above for definition of covariables). Baseline covariables were evaluated initially for pairwise associations using Spearman’s correlation coefficients to rule out potential troublesome collinearity among variables to be included in the statistical models for the 2-year outcomes. Univariate and multivariable logistic regression models were used to evaluate the relationships between baseline variables buckling, overall knee confidence, buckling confidence, varus-valgus excursion during gait, and maximum varus-valgus angular velocity during gait, and each of the outcomes: basic function outcome and advanced function outcome. Separate models were used for each outcome variable. The final multivariable models adjusted for baseline age, gender, BMI, knee pain severity, function self-efficacy, depressive symptoms, disease severity (K/L grade), knee extensor strength, each as a continuous variable (other than gender). Results are summarized as unadjusted and adjusted odds ratios (ORs) and 95% confidence intervals (CIs); ORs with 95% Cis that exclude the value of 1.0 are considered to be statistically significant.
RESULTS
Among 250 participants, 212 completed the 2-year follow-up evaluation. Reasons for not completing included: unreachable (12 persons); serious medical condition (6 persons); too busy (5 persons); could not miss work (5 persons); other (10 persons). As shown in Table 1, the 212 participants had a mean (SD) age of 64.6 (10.1) years and a mean BMI of 28.5 (5.7) kg/m2; 163 (76.9%) were women. Baseline characteristics for the full sample and by buckling status are shown in Table 1. As compared to the attributes of the 212 persons (shown in first column of Table 1), participants who did not complete the study differed only slightly for baseline age [mean 66.9 years (11.1)], gender (68% women), BMI [mean 28.6 kg/m2 (4.7)], overall knee confidence [2 persons (5.3%) with score 0, 20 (52.6%) with score 1, 16 (42.1%) with score 2, 0 with score 3], buckling confidence [8 persons (21.1%) with score 0, 9 (23.7%) with score 1, 19 (50.0%) with score 2, 2 (5.3%) with score 3], varus-valgus excursion during gait [mean 6.9° (2.3)] maximum varus-valgus angular velocity during gait [mean 33.0°/second (16.0)], basic function [mean 66.1 (10.7)], or advanced function [mean 50.5 (10.7)], but more frequently reported buckling [25 persons (65.8%)].
Table 1. Baseline Characteristics for the Full Sample and by Buckling Status.
Mean (SD) is shown unless otherwise specified.
| Full sample (212 persons) | No buckling (136 persons) | Yes buckling (76 persons) | ||
|---|---|---|---|---|
| Overall knee confidence, higher score worse, number (%) | 0 | 38 (17.9%) | 35 (25.7%) | 3 (3.9%) |
| 1 | 96 (45.3) | 62 (45.6) | 34 (44.7) | |
| 2 | 63 (29.7) | 36 (26.5) | 27 (35.5) | |
| 3 | 15 (7.1) | 3 (2.2) | 12 (15.8) | |
| Buckling confidence, higher score better, number (%) | 0 | 29 (13.7%) | 6 (4.4%) | 23 (30.3%) |
| 1 | 71 (33.5) | 38 (27.9) | 33 (43.4) | |
| 2 | 71 (33.5) | 51 (37.5) | 20 (26.3) | |
| 3 | 41 (19.3) | 41 (30.1) | 0 (0) | |
| Varus-valgus excursion during gait, ° | 7.1 (2.6) | 7.2 (2.6) | 6.9 (2.5) | |
| Maximum varus-valgus angular velocity during gait, °/second | 31.9 (17.1) | 33.3 (18.6) | 29.6 (13.7) | |
| Age, years | 64.6 (10.1) | 65.8 (9.7) | 62.6 (10.6) | |
| Women, number (%) | 163 (76.9%) | 106 (77.9%) | 57 (75.0%) | |
| BMI, kg/m2 | 28.5 (5.7) | 28.3 (5.8) | 29.0 (6.0) | |
| Self-efficacy, higher score better | 25.5 (5.2) | 26.7 (3.9) | 23.4 (6.5) | |
| Depressive symptoms | 1.6 (1.3) | 1.4 (1.1) | 1.8 (1.6) | |
| Knee extensor strength, N-M/kg (of knee with worse buckling confidence) | 92.9 (30.6) | 95.9 (29.1) | 87.4 (32.7) | |
| K/L grade, worse of R and L, number (%) | 0 | 2 (0.9%) | 2 (1.5%) | 9 (0.0%) |
| 1 | 21 (9.9) | 12 (8.8) | 9 (11.8) | |
| 2 | 103 (48.6) | 64 (47.1) | 39 (51.3) | |
| 3 | 34 (16.0) | 24 (17.7) | 10 (13.2) | |
| 4 | 52 (24.5) | 34 (25.0) | 18 (23.7) | |
| Knee pain | 9.2 (7.7) | 7.1 (6.5) | 12.9 (8.1) | |
| Basic function, higher score better | 71.5 (13.2) | 74.8 (12.7) | 65.7 (12.2) | |
| Advanced function, higher score better | 54.5 (13.2) | 57.1 (11.9) | 49.9 (14.3) | |
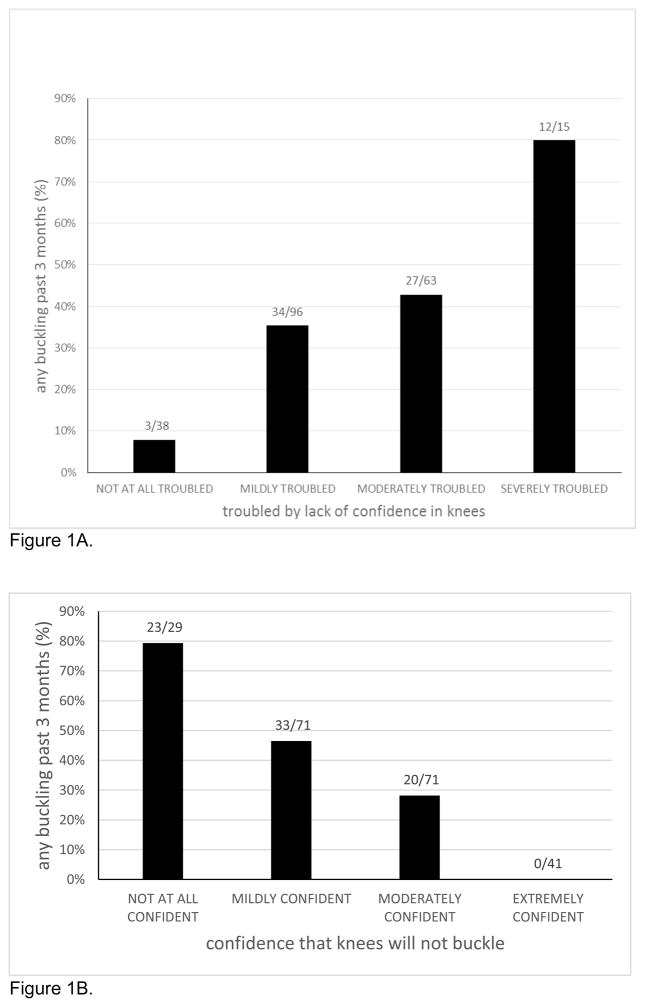
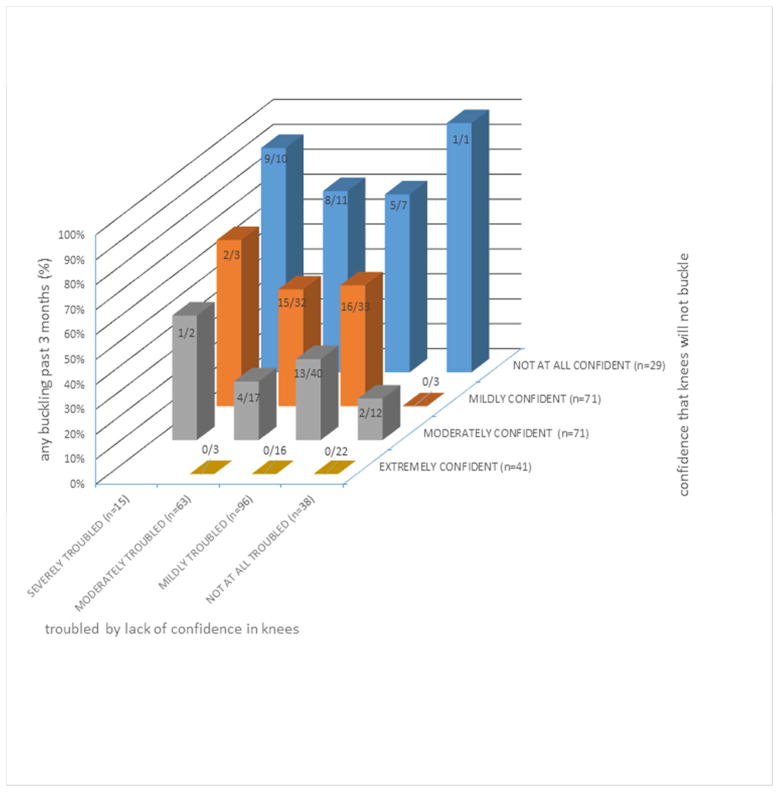
Spearman correlation coefficients for baseline variables are shown in Table 2. In graphs summarizing the relationships between confidence and buckling, the percentage of persons with buckling in the past 3 months was higher with successively worse overall knee confidence (Figure 1A) and buckling confidence (Figure 1B) categories. Figure 2 shows the percentage of persons with buckling within groups defined by both confidence variables jointly.
Table 2. Pairwise Correlations between Baseline Variables (n = 212 persons).
The table shows Spearman’s correlation coefficients for baseline covariables.
| Overall knee confidence (higher worse) |
Buckling confidence (higher better) |
Varus- valgus excursion during gait |
Varus- valgus angular velocity during gait |
Age | BMI | Self- efficacy (higher better) |
Depressive symptoms |
Knee extensor strength |
K/L grade |
Knee pain severity |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall knee confidence (higher worse) | 1.00 | −0.47 | −0.05 | −0.04 | −0.24 | 0.22 | −0.39 | 0.19 | −0.23 | 0.12 | 0.62 |
| Buckling confidence (higher better) | 1.00 | 0.10 | 0.05 | 0.26 | −0.23 | 0.31 | −0.13 | 0.27 | −0.12 | −0.51 | |
| Varus-valgus excursion during gait | 1.00 | 0.11 | 0.08 | −0.38 | 0.20 | −0.13 | 0.14 | 0.14 | −0.05 | ||
| Varus-valgus angular velocity during gait | 1.00 | 0.02 | 0.09 | 0.03 | −0.12 | −0.12 | 0.19 | −0.03 | |||
| Age | 1.00 | −0.15 | −0.01 | −0.24 | −0.22 | 0.19 | −0.26 | ||||
| BMI | 1.00 | −0.28 | 0.02 | −0.30 | 0.17 | 0.28 | |||||
| Self-efficacy (higher better) | 1.00 | −0.18 | 0.48 | −0.08 | −0.44 | ||||||
| Depressive symptoms | 1.00 | 0.00 | −0.15 | 0.17 | |||||||
| Knee extensor strength | 1.00 | −0.19 | −0.28 | ||||||||
| K/L grade | 1.00 | 0.04 | |||||||||
| Knee pain severity | 1.00 |
Figure 1.
Figure 1A. Percentage of Persons with Buckling within Overall Knee Confidence Categories.
Figure 1B. Percentage of Persons with Buckling within Buckling Confidence Categories
Figure 1A and 1B. The bars show the percentage of persons who reported buckling within categories based on responses to the overall knee confidence (Figure 1A) and buckling confidence (Figure 1B) queries.
Figure 2. Percentage of Persons with Buckling within Groups Defined by Both Confidence Variables.
The height of each bar in the figure corresponds to the percentage of persons who had buckling within groups defined by the values of both confidence variables shown on the axes. The fractions at the top of each bar show the actual number with buckling divided by the number who had the specified value for each of the confidence variables.
As shown in Table 3, in adjusted analyses, buckling was significantly associated with advanced function outcome, but not basic function outcome. Each of the confidence variables was significantly associated with each outcome in unadjusted analyses. A significant association persisted for overall knee confidence and advanced function outcome, while the association approached significance for buckling confidence and both outcomes. Neither varus-valgus excursion nor angular velocity during gait was associated with risk of either outcome in unadjusted or adjusted analyses. Further adjustment for knee injury, knee surgery, self-reported physical activity, or hip abductor muscle strength minimally altered these findings (data not shown).
Table 3. Results from Logistic Regression Models to Evaluate Associations of Each Instability Variable with Odds of a Poor Basic Function Outcome and Poor Advanced Function Outcome.
The table shows the association between each instability variable at baseline and poor basic function outcome (dependent variable) and poor advanced function outcome (dependent variable), as odds ratios (ORs) and associated 95% confidence intervals (CIs) unadjusted and then adjusted for age, gender, BMI, knee pain severity, function self-efficacy, depressive symptoms, disease severity (K/L, worse of 2 knees), and knee extensor strength (of the knee with worse buckling confidence). 95% CIs that exclude 1 are statistically significant.
| Poor basic function outcome 101/212 persons (47.6%) | Poor advanced function outcome 98/212 persons (46.2%) | |||
|---|---|---|---|---|
| Instability variable (baseline) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
| Buckling, past 3 months (yes/no) | 1.66 (0.94, 2.93) | 1.18 (0.59, 2.35) | 2.27 (1.28, 4.03) | 2.08 (1.03, 4.20) |
| Confidence knees will not buckle (higher better, continuous) | 0.61 (0.46, 0.83) | 0.74 (0.51, 1.09) | 0.63 (0.47, 0.85) | 0.69 (0.47, 1.02) |
| Overall knee confidence (higher worse, continuous) | 1.52 (1.09, 2.13) | 1.05 (0.65, 1.68) | 1.80 (1.27, 2.56) | 1.65 (1.01, 2.70) |
| Varus-valgus excursion during gait, per 1° | 0.91 (0.81, 1.01) | 0.99 (0.87, 1.12) | 0.95 (0.85, 1.06) | 1.01 (0.89, 1.15) |
| Maximum varus-valgus angular velocity during gait, per 1°/sec | 1.00 (0.98, 1.02) | 1.00 (0.98, 1.02) | 0.99 (0.98, 1.01) | 0.99 (0.97, 1.01) |
In secondary adjusted analyses, we explored the association between buckling and specific task performance. Among basic tasks, buckling was significantly associated with impaired performance (defined as a response of “cannot do, quite a lot, or some” to “How much difficulty do you have…”, persisting or newly present at the 2-year evaluation), for bending over from a standing position to pick up a piece of clothing from the floor, and stepping on and off a bus. Among advanced tasks, buckling was significantly associated with impaired performance (defined as “cannot do or quite a lot” persisting or newly present at the 2-year evaluation) for running ½ mile or more, going up and down 3 flights of stairs using a handrail, carrying something in both arms while climbing a flight of stairs, and taking a 3 mile brisk walk without stopping to rest.
DISCUSSION
In summary, buckling was significantly associated with greater risk of 2-year advanced but not basic function outcome. Overall knee confidence was significantly associated with advanced function outcome in adjusted analyses. The associations between buckling confidence and both outcomes approached significance in adjusted analyses. There was no evidence of an association between either of the quantitative gait measures of frontal plane instability and either basic or advanced function outcome.
Fitzgerald et al originally described self-reported instability including giving way, buckling, or shifting of the knee during functional activity as potentially having an effect in OA that could not be accounted for by knee pain or strength (4). Three previous studies used the same question as we did to ascertain buckling: two of these had a lower frequency [11.8% in the Framingham Osteoarthritis Study (2) and 18.0% in MOST (7)] than we found (35.8%), most likely because our cohort all had knee OA while the two previous studies included individuals without OA; the third study described a higher frequency (67%, Amsterdam OA cohort), perhaps due to differences in distribution of disease severity (8). Previous studies have described a cross-sectional association between buckling and self-reported function, in persons: with knee OA (4, 6); with and without knee OA (2); and with knee OA and without knee OA but at higher risk to develop it (7).
To our knowledge, ours is the first longitudinal report of the buckling/function association and is also unique in concurrently evaluating confidence and reporting specifically on advanced and basic function outcome. In contrast to buckling, overall knee confidence has been evaluated longitudinally, within our previous Osteoarthritis Initiative report: worse knee confidence was associated with a greater risk of poor 3-year self-reported function outcome, with trend tests supporting a graded response (1). Our current findings (Table 2) suggest that the two confidence measures are correlated but distinguishable. Overall knee confidence, queried using an item from an established instrument as in our previous report (1), is very likely a broader construct than the more specific worry about buckling. We prospectively studied these confidence measures to address the possibility that an individual might alter activity to minimize buckling; in this scenario, solely asking about recent buckling would not capture its impact on function. We did not include buckling and confidence in the same model given the likelihood that they share causal pathways. We found (Table 2) that confidence is also related to self-efficacy, defined by Bandura as the belief in one’s capacities to mobilize the internal resources and course of action needed to meet given situational demands (23). The findings of the current report were all independent of self-efficacy which was included in each model.
Measurement of function outcomes over time is necessary to better understand the impact of knee OA. However, the best way to evaluate function outcomes in knee OA has not been established. As we previously described (24), a focus on change ignores those with persistently high or low function, effectively collapsing them into the same group, and reducing the ability to detect the effects of factors responsible for an individual’s state of function. In a disease that is slow to evolve, such as knee OA, factors related to persistent low- or high-function states are particularly important. We (1, 24) and others (25) have used the outcome approach of the current manuscript to address this issue. Buckling was associated only with advanced function outcome, supporting the possibility that buckling may not affect the nature of tasks included in a basic function measure. It is important to identify factors associated with advanced function decline, given the likelihood that high level function decline leads to reduction in activity.
There are limitations to this study that need to be recognized. As noted above, persons not included had a higher frequency of buckling on average; it is difficult to estimate the impact that this difference may have had on our findings. We did not measure anxiety or pain- or movement-related fear which may influence the relationship between the instability variables and outcome. Despite the technological sophistication of quantitative gait analysis, quantification of frontal plane motion during gait has its limitations. Surface skin markers may not accurately reflect knee joint kinematics, especially in obese individuals. We found no relationship between frontal plane instability during gait as we measured it and function outcome; it remains possible that frontal plane instability during activity quantified using other approaches may be associated with outcome. Of note, previously we found that static varus-valgus laxity, a more direct measure of motion at the knee, albeit not weightbearing, was associated with 3-year function outcome (24).
These findings support intervention development to target buckling and confidence. Recent treatment guidelines and systematic reviews do not include such interventions or the need to develop them (9, 10). For buckling, such therapy might ultimately include neuromuscular training during task performance, taping, or bracing. Interventions including neuromuscular exercise are showing some promise (26–28) although recent studies are not as yet specifically evaluating buckling or confidence outcomes. Knee confidence could be addressed using principles of Bandura’s social cognitive theory (29, 30), including: reproduction of modalities learned within physical therapy (vicarious reinforcement); anticipation of future events and planning for consequences of actions (forethought activity); short-term goal setting to connect current actions and future outcomes (self-regulatory capabilities); self-evaluations to appraise goal attainment (self-reflecting capability); and social and intrinsic rewards to motivate performance and help individuals persist through setbacks (self-reinforcement). Specific strategies could incorporate education concerning risk of poor outcome and benefits associated with its prevention, recognize and address impediments to improving confidence, tailor to the individual’s self-management capabilities, and use telephone counseling and/or linkage to supportive social networks. Skou et al suggest that knee confidence might be improved by targeting self-reported knee instability, lower muscle strength, and greater dynamic varus-valgus motion (3). Future studies should continue this important work to identify the sources of confidence (3) and buckling (31); these parameters could then become the target of additional strategies.
In conclusion, knee buckling and overall knee confidence were each associated with poor 2-year advanced function outcome. Current treatment does not address these modifiable factors; interventions to address them may improve outcome in knee OA.
SIGNIFICANCE AND INNOVATIONS.
This is the first longitudinal report of the association between knee buckling and physical function outcome in persons with knee OA. Whether buckling contributes to or is a result of poor function and its consequence on the knee joint environment is important to elucidate: current treatment guidelines for knee OA do not target buckling or other aspects of instability.
This study evaluates knee instability broadly, i.e., knee buckling, overall knee confidence, buckling confidence, and instability measured during quantitative gait analysis. Because lack of confidence may cause people with knee OA to alter activity to avoid buckling, evaluation of knee confidence provides an additional approach to capture buckling impact. In the instability spectrum, confidence and the memory of a buckling experience may particularly influence nature and intensity of activity; it is not known whether these variables are more important to outcome than instability measured during gait.
An optimal function measure to evaluate buckling impact must include tasks that have a reasonable likelihood of being limited by buckling. Basic tasks are emphasized in most knee OA function measures, e.g., in WOMAC: rising from sitting; standing; bending to floor; walking on flat ground; getting in/out of a car; putting on socks/stockings; rising from bed; lying in bed, etc. Buckling is unlikely to limit many of these tasks; it is possible that buckling impacts aspects of function that measures like WOMAC do not incorporate. This study used the Late-Life Function and Disability Instrument to specifically evaluate basic and advanced function outcome.
Acknowledgments
Support: NIH/NIAMS P60 AR064464, R01 AR054806, R01 AR048748
APPENDIX A. Items of the Late-Life Function instrument are shown, with basic lower extremity items highlighted in grey and advanced lower extremity items in purple
| LATE-LIFE FUNCTION -BASIC LOWER EXTREMITY ITEMS: 14 ITEMS - F2, F10, F11, F12, F14, F15, F18, F21, F22, F23, F25, F26, F28, F31 | |
| LATE-LIFE FUNCTION -ADVANCED LOWER ITEMS: 11 ITEMS - F4, F7, F8, F9, F19, F20, F24, F27, F29, F30, F32 | |
| F1 | HOW MUCH DIFFICULTY DO YOU HAVE… UNSCREWING THE LID OFF A PREVIOUSLY UNOPENED JAR WITHOUT USING ANY DEVICES |
| F2 | HOW MUCH DIFFICULTY DO YOU HAVE… GOING UP AND DOWN A FLIGHT OF STAIRS INSIDE, USING A HANDRAIL |
| F3 | HOW MUCH DIFFICULTY DO YOU HAVE… PUTTING ON AND TAKING OFF LONG PANTS (INCLUDING MANAGING FASTENERS) |
| F4 | HOW MUCH DIFFICULTY DO YOU HAVE… RUNNING 1/2 MILE OR MORE |
| F5 | HOW MUCH DIFFICULTY DO YOU HAVE… USING COMMON UNTENSILS FOR PREPARING MEALS (CAN OPENER, POTATO PEELER, OR SHARP KNIFE) |
| F6 | HOW MUCH DIFFICULTY DO YOU HAVE…HOLDING A FULL GLASS OF WATER IN ONE HAND |
| F7 | HOW MUCH DIFFICULTY DO YOU HAVE… WALKING A MILE, TAKING RESTS AS NECESSARY |
| F8 | HOW MUCH DIFFICULTY DO YOU HAVE… GOING UP AND DOWN A FLIGHT OF STAIRS OUTSIDE, WITHOUT USING A HANDRAIL |
| F9 | HOW MUCH DIFFICULTY DO YOU HAVE… RUNNING A SHORT DISTANCE, SUCH AS TO CATCH A BUS |
| F10 | HOW MUCH DIFFICULTY DO YOU HAVE… REACHING OVERHEAD WHILE STANDING, AS IF TO PULL A LIGHT CORD |
| F11 | HOW MUCH DIFFICULTY DO YOU HAVE…SITTING DOWN IN AND STANDING UP FROM A LOW, SOFT COUCH |
| F12 | HOW MUCH DIFFICULTY DO YOU HAVE… PUTTING ON AND TAKING OFF A COAT OR JACKET |
| F13 | HOW MUCH DIFFICULTY DO YOU HAVE…REACHING BEHIND YOUR BACK AS IF TO PUT A BELT THROUGH A BELT LOOP |
| F14 | HOW MUCH DIFFICULTY DO YOU HAVE… STEPPING UP AND DOWN FROM A CURB |
| F15 | HOW MUCH DIFFICULTY DO YOU HAVE… OPENING A HEAVY, OUTSIDE DOOR |
| F16 | HOW MUCH DIFFICULTY DO YOU HAVE…RIP OPEN A PACKAGE OF SNACK FOOD (E.G. CELLOPHANE WRAPPING ON CRACKERS) USING ONLY YOUR HANDS |
| F17 | HOW MUCH DIFFICULTY DO YOU HAVE… POURING FROM A LARGE PITCHER |
| F18 | HOW MUCH DIFFICULTY DO YOU HAVE… GETTING INTO AND OUT OF A CAR/TAXI (SEDAN) |
| F19 | HOW MUCH DIFFICULTY DO YOU HAVE… HIKING A COUPLE OF MILES ON UNEVEN SURFACES, INCLUDING HILLS |
| F20 | HOW MUCH DIFFICULTY DO YOU HAVE… GOING UP AND DOWN 3 FLIGHTS OF STAIRS INSIDE, USING A HANDRAIL |
| F21 | HOW MUCH DIFFICULTY DO YOU HAVE… PICKING UP A KITCHEN CHAIR AND MOVING IT, IN ORDER TO CLEAN |
| F22 | HOW MUCH DIFFICULTY DO YOU HAVE… USING A STEP STOOL TO REACH INTO A HIGH CABINET |
| F23 | HOW MUCH DIFFICULTY DO YOU HAVE… MAKING A BED, INCLUDING SPREADING AND TUCKING IN BED SHEETS |
| F24 | HOW MUCH DIFFICULTY DO YOU HAVE… CARRYING SOMETHING IN BOTH ARMS WHILE CLIMBING A FLIGHT OF STAIRS (E.G. LAUNDRY BASKET) |
| F25 | HOW MUCH DIFFICULTY DO YOU HAVE… BENDING OVER FROM A STANDING POSITION TO PICK UP A PIECE OF CLOTHING FROM THE FLOOR |
| F26 | HOW MUCH DIFFICULTY DO YOU HAVE… WALKING AROUND ONE FLOOR OF YOUR HOME, TAKING INTO CONSIDERATION THRESHOLDS, DOORS, FURNITURE, AND A VARIETY OF FLOOR COVERINGS |
| F27 | HOW MUCH DIFFICULTY DO YOU HAVE… GETTING UP FROM THE FLOOR (AS IF YOU WERE LAYING ON THE GROUND) |
| F28 | HOW MUCH DIFFICULTY DO YOU HAVE… WASHING DISHES, POTS, AND UTENSILS BY HAND WHILE STANDING AT SINK |
| F29 | HOW MUCH DIFFICULTY DO YOU HAVE…WALKING SEVERAL BLOCKS |
| F30 | HOW MUCH DIFFICULTY DO YOU HAVE… TAKING A 1 MILE, BRISK WALK WITHOUT STOPPING TO REST |
| F31 | HOW MUCH DIFFICULTY DO YOU HAVE… STEPPING ON AND OFF A BUS |
| F32 | HOW MUCH DIFFICULTY DO YOU HAVE… WALKING ON A SLIPPERY SURFACE OUTDOORS |
Footnotes
Financial Support Information: There has been no financial support or other benefits from commercial sources for the work reported on in the manuscript, or any other financial interests that any of the authors may have, which could create a potential conflict of interest or the appearance of a conflict of interest with regard to the work.
References
- 1.Colbert CJ, Song J, Dunlop D, Chmiel JS, Hayes KW, Cahue S, et al. Knee confidence as it relates to physical function outcome in persons with or at high risk of knee osteoarthritis in the osteoarthritis initiative. Arthritis Rheum. 2012;64(5):1437–46. doi: 10.1002/art.33505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Felson DT, Niu J, McClennan C, Sack B, Aliabadi P, Hunter DJ, et al. Knee buckling: prevalence, risk factors, and associated limitations in function. Ann Intern Med. 2007;147(8):534–40. doi: 10.7326/0003-4819-147-8-200710160-00005. [DOI] [PubMed] [Google Scholar]
- 3.Skou ST, Wrigley TV, Metcalf BR, Hinman RS, Bennell KL. Association of knee confidence with pain, knee instability, muscle strength, and dynamic varus-valgus joint motion in knee osteoarthritis. Arthritis Care Res (Hoboken) 2014;66(5):695–701. doi: 10.1002/acr.22208. [DOI] [PubMed] [Google Scholar]
- 4.Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. 2004;51(6):941–6. doi: 10.1002/art.20825. [DOI] [PubMed] [Google Scholar]
- 5.Schmitt LC, Fitzgerald GK, Reisman AS, Rudolph KS. Instability, laxity, and physical function in patients with medial knee osteoarthritis. Phys Ther. 2008;88(12):1506–16. doi: 10.2522/ptj.20060223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van der Esch M, Knoop J, van der Leeden M, Voorneman R, Gerritsen M, Reiding D, et al. Self-reported knee instability and activity limitations in patients with knee osteoarthritis: results of the Amsterdam osteoarthritis cohort. Clin Rheumatol. 2012;31(10):1505–10. doi: 10.1007/s10067-012-2025-1. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen US, Felson DT, Niu J, White DK, Segal NA, Lewis CE, et al. The impact of knee instability with and without buckling on balance confidence, fear of falling and physical function: the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage. 2014;22(4):527–34. doi: 10.1016/j.joca.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knoop J, van der Leeden M, van der Esch M, Thorstensson CA, Gerritsen M, Voorneman RE, et al. Association of lower muscle strength with self-reported knee instability in osteoarthritis of the knee: results from the Amsterdam Osteoarthritis cohort. Arthritis Care Res (Hoboken) 2012;64(1):38–45. doi: 10.1002/acr.20597. [DOI] [PubMed] [Google Scholar]
- 9.McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(3):363–88. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Juhl C, Christensen R, Roos EM, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol. 2014;66(3):622–36. doi: 10.1002/art.38290. [DOI] [PubMed] [Google Scholar]
- 11.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40. [PubMed] [Google Scholar]
- 12.Jette AM, Haley SM, Coster WJ, Kooyoomjian JT, Levenson S, Heeren T, et al. Late life function and disability instrument: I. Development and evaluation of the disability component. J Gerontol A Biol Sci Med Sci. 2002;57(4):M209–16. doi: 10.1093/gerona/57.4.m209. [DOI] [PubMed] [Google Scholar]
- 13.Haley SM, Jette AM, Coster WJ, Kooyoomjian JT, Levenson S, Heeren T, et al. Late Life Function and Disability Instrument: II. Development and evaluation of the function component. J Gerontol A Biol Sci Med Sci. 2002;57(4):M217–22. doi: 10.1093/gerona/57.4.m217. [DOI] [PubMed] [Google Scholar]
- 14.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 15.Barber-Westin SD, Noyes FR, McCloskey JW. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati knee rating system in 350 subjects with uninjured, injured, or anterior cruciate ligament-reconstructed knees. Am J Sports Med. 1999;27(4):402–16. doi: 10.1177/03635465990270040201. [DOI] [PubMed] [Google Scholar]
- 16.Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. Journal of Orthopaedic Research. 1990;8(3):383–92. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 17.Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989;32(1):37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- 18.Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9) Arthritis Care Res (Hoboken) 2011;63 (Suppl 11):S454–66. doi: 10.1002/acr.20556. [DOI] [PubMed] [Google Scholar]
- 19.Buckland-Wright C. Protocols for precise radio-anatomical positioning of the tibiofemoral and patellofemoral compartments of the knee. Osteoarthritis Cartilage. 1995;3 (Suppl A):71–80. [PubMed] [Google Scholar]
- 20.Hawker GA, Davis AM, French MR, Cibere J, Jordan JM, March L, et al. Development and preliminary psychometric testing of a new OA pain measure--an OARSI/OMERACT initiative. Osteoarthritis Cartilage. 2008;16(4):409–14. doi: 10.1016/j.joca.2007.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP) Arthritis Care Res (Hoboken) 2011;63 (Suppl 11):S240–52. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 22.Gignac MA, Cao X, McAlpine J, Badley EM. Measures of disability: Arthritis Impact Measurement Scales 2 (AIMS2), Arthritis Impact Measurement Scales 2-Short Form (AIMS2-SF), The Organization for Economic Cooperation and Development (OECD) Long-Term Disability (LTD) Questionnaire, EQ-5D, World Health Organization Disability Assessment Schedule II (WHODASII), Late-Life Function and Disability Instrument (LLFDI), and Late-Life Function and Disability Instrument-Abbreviated Version (LLFDI-Abbreviated) Arthritis Care Res (Hoboken) 2011;63 (Suppl 11):S308–24. doi: 10.1002/acr.20640. [DOI] [PubMed] [Google Scholar]
- 23.Bandura A. Self-efficacy mechanism in physiological activation and health-promoting behavior. In: Madden J, editor. Neurobiology of Learning, Emotion, and Affect. New York: Raven Press; 1991. p. 229. [Google Scholar]
- 24.Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48(12):3359–70. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 25.Mallen CD, Peat G, Thomas E, Lacey R, Croft P. Predicting poor functional outcome in community-dwelling older adults with knee pain: prognostic value of generic indicators. Ann Rheum Dis. 2007;66(11):1456–61. doi: 10.1136/ard.2006.067975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Villadsen A, Overgaard S, Holsgaard-Larsen A, Christensen R, Roos EM. Immediate efficacy of neuromuscular exercise in patients with severe osteoarthritis of the hip or knee: a secondary analysis from a randomized controlled trial. J Rheumatol. 2014;41(7):1385–94. doi: 10.3899/jrheum.130642. [DOI] [PubMed] [Google Scholar]
- 27.Knoop J, van der Leeden M, Roorda LD, Thorstensson CA, van der Esch M, Peter WF, et al. Knee joint stabilization therapy in patients with osteoarthritis of the knee and knee instability: Subgroup analyses in a randomized, controlled trial. J Rehabil Med. 2014;46(7):703–7. doi: 10.2340/16501977-1809. [DOI] [PubMed] [Google Scholar]
- 28.Bennell KL, Kyriakides M, Metcalf B, Egerton T, Wrigley TV, Hodges PW, et al. Neuromuscular versus quadriceps strengthening exercise in patients with medial knee osteoarthritis and varus malalignment: a randomized controlled trial. Arthritis Rheumatol. 2014;66(4):950–9. doi: 10.1002/art.38317. [DOI] [PubMed] [Google Scholar]
- 29.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 30.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 31.Chang AH, Lee SJ, Zhao H, Ren Y, Zhang LQ. Impaired varus-valgus proprioception and neuromuscular stabilization in medial knee osteoarthritis. J Biomech. 2014;47(2):360–6. doi: 10.1016/j.jbiomech.2013.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]