Abstract
Concerns have been raised that optimized redistricting of liver allocation areas might have the unintended result of shifting livers from better-performing to poorer-performing OPOs. We used the Liver Simulated Allocation Model to simulate a 5-year period of liver sharing within either 4 or 8 optimized districts. We investigated whether each OPO’s net liver import under redistricting would be correlated with two OPO performance metrics (observed to expected liver yield and liver donor conversion ratio), along with two other potential correlates (eligible deaths and incident listings above MELD 15). We found no evidence that livers would flow from better-performing OPOs to poorer-performing OPOs in either redistricting scenario. Instead, under these optimized redistricting plans, our simulations suggest that livers would flow from OPOs with more-than-expected eligible deaths toward those with fewer-than-expected eligible deaths, and that livers would flow from OPOs with fewer-than-expected incident listings to those with more-than-expected incident listings, the latter a pattern already established in the current allocation system. Redistricting liver distribution to reduce geographic inequity is expected to align liver allocation across the country with the distribution of supply and demand, rather than transferring livers from better-performing OPOs to poorer-performing OPOs.
Keywords: liver, allocation, organ procurement organization performance, liver import
INTRODUCTION
Geographic disparities in the distribution of deceased donor livers have been extensively documented (1–5). Observed disparities in transplant and death rates for liver candidates by ethnicity (6) and socioeconomic status (mediated by traveling to follow the organ supply) (7) have even been attributed to geographic differences in the availability of deceased donor livers. We have described how mathematically optimized redistricting might be applied to design novel liver allocation districts for the purpose of reducing geographic disparity, and redistricting has been predicted to significantly reduce not only overall deaths but also the variation in median MELD at transplant across the country (8, 9). However, concerns have been raised that redistricting might also have the unintended and possibly perverse consequence of shifting livers from better-performing OPOs to poorer-performing OPOs.
Organ procurement organizations (OPOs) educate the public about organ donation and work directly with donor hospitals and donor families to coordinate the donation process. OPO effectiveness at these tasks is of the utmost importance, and significant attention has been focused on increasing donor consent rates (10). The Scientific Registry for Transplant Recipients tracks the performance of OPOs with metrics capturing various aspects of the donation process including consent and donor management. Because better-performing OPOs are those that are more effective at generating donations from the populations they serve, some have speculated that redistricting might reduce geographic disparity in access to liver transplantation by shifting livers from the better-performing OPOs to candidates in poorer-performing OPOs. However, factors other than OPO effectiveness influence the balance of supply and demand for liver transplantation across the country: liver allocation areas span a fourteen-fold variation in incident listings for liver transplantation and a three-fold variation in eligible deaths compared with less than 2-fold difference in OPO performance (11, 12).
The present study examines whether redistricting would shift organs from better-performing to poorer-performing OPOs, using the optimized 8-district and 4-district maps (Figure 1) from the redistricting concept document circulated by the OPTN Liver and Intestinal Transplantation Committee (13). To understand the impact of redistricting on better-performing and poorer-performing OPOs, we considered two metrics of OPO performance as reported by the SRTR: the observed to expected liver yield (O:E liver yield) and the unadjusted liver donor conversion ratio. We also tested whether the flow of livers after redistricting would be correlated with incident listings and/or with eligible deaths.
Figure 1.
Optimized 8-district and 4-district allocation maps for broader sharing of deceased donor livers
METHODS
Simulation and Study Population
The Liver Simulated Allocation Model (LSAM) is a discrete event simulation that models the functioning of the U.S. liver allocation system, including liver offers, acceptance behavior, the evolution of candidate health status over time, death on the waiting list, and post- transplant outcomes. LSAM is designed for comparing allocation outcomes under various allocation schemes. The LSAM simulated population in this study was generated from actual donor and candidate records for the two-year period from January 1, 2010 to Dec 31, 2011. Two optimized redistricting plans were tested in this study: an 8-district plan, and a 4-district plan (13).
In cases where comparisons are drawn between LSAM simulations to the current Share-35 allocation policy, the comparison population included all deceased-donor liver-only transplants from June 18, 2013 to June 17, 2014 (n=5,731), incident listings for liver transplantation from June 18, 2013 to June 17, 2014 (n=12,157), and eligible deaths from 2010 (n=8,982).
Data Sources
This study used data from the Scientific Registry of Transplant Recipients (SRTR). The SRTR data system includes data on all donor, wait-listed candidates, and transplant recipients in the US, submitted by the members of the Organ Procurement and Transplantation Network (OPTN). The Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services provides oversight to the activities of the OPTN and SRTR contractors. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the SRTR or the U.S. Government.
Net Import
Net import was used to measure the direction and magnitude of liver flow, into or out of an OPO. Organs recovered in an OPO other than the recipient’s OPO were considered imports to the recipient OPO and exports from the donor OPO. We defined an OPO’s net import as the difference between imports and exports divided by the organs recovered by the OPO: (import – export) ÷ recovered. Net import might range from −1 to +∞. A negative net import indicated that the OPO exported more livers than were imported; a net import of −1 indicated that all recovered livers were exported. When the net import was 0, the OPO imported as many livers as it exported. When the net import was positive, the OPO imported more livers than it exported.
Potential correlates
Two measures of OPO performance reported by the SRTR were considered in this analysis: O:E liver yield, and liver donor conversion ratio. The other potential correlates, O:E incident listings and O:E eligible deaths, were novel measures designed in the context of this study to reflect disparities in donor and candidate counts per OPO.
O:E Liver Yield
The observed liver yield was calculated, as defined by the SRTR, as the actual number of liver donations per 100 donors reported to SRTR for a given time frame and OPO. The expected liver yield was calculated, also as defined by the SRTR, as a predicted number of liver donations per 100 donors, based on an adjusted linear regression model (14). The O:E liver yield was, as such, the observed to expected ratio for liver that can be found in Table C3 of the SRTR OPO-specific reports. A better-performing OPO would be one with an O:E ratio higher than 1, that is, an OPO that has generated more liver transplants from its donors than expected. Similarly, a poorer-performing OPO would be one with an O:E ratio lower than 1. O:E liver yield data were from 2012–2013.
Liver Donor Conversion Ratio
The liver donor conversion ratio was calculated, as defined by the SRTR, as the proportion of eligible deaths that are converted to liver donors in an OPO. A deceased individual was considered an eligible death if they met certain criteria for age, neurologic death, and other exclusions of infection or malignancy (14). The liver donor conversion ratio was, as such, the unadjusted observed liver-specific donation rate that can be found in Table C2 of the SRTR OPO-specific reports, divided by 100. As an example, if every eligible death in an OPO resulted in a recovered liver, the liver donor conversion ratio would be 1.0; if only half of eligible deaths resulted in liver donations, then the ratio would be 0.5. A better-performing OPO would have a liver donor conversion ratio nearer to 1, indicating that a high proportion of its eligible deaths became liver donors. Liver donor conversion ratio data were from 2012–2013.
O:E of Eligible Deaths
O:E Eligible Deaths was defined for the purposes of this study as: (eligible deaths in OPO/national eligible deaths) ÷ (population in OPO/national population). This metric was designed to measure the prevalence of eligible deaths in each OPO, normalized to the OPO’s population relative to the national population. Population per OPO was calculated from U.S. Census Bureau TIGER/Line shapefiles (15). Because the reporting of eligible deaths is lagged, this analysis used eligible deaths from 2010.
O:E Incident Listings
O:E Incident Listings was defined for the purposes of this study as: (listings in OPO/national listings) ÷ (population in OPO/national population), and included all observed incident listings for liver transplantation in the United States with any lab MELD at the time of listing. This metric was designed to measure how many new registrants are waiting for deceased donor livers in each OPO, normalized to the OPO’s population relative to the national population. Population per OPO was calculated from U.S. Census Bureau TIGER/Line shapefiles (15). This analysis used incident liver-only listings from Jun 18, 2013 to Jun 17, 2014. We also performed a sensitivity analysis, calculating O:E incident listings but excluding incident listings at MELD < 15.
Association between net import and potential correlates
For each of the simulated redistricting scenarios, net import ratios were calculated for 51 OPOs that served local liver transplant programs in 2010. Seven OPOs that did not serve local liver transplant programs in 2010 were excluded from this analysis. In the share-35 era (June 18, 2013 to June 17, 2014), net import ratios were calculated for 52 OPOs that served local liver transplant programs and 6 OPOs that did not serve local liver transplant programs were excluded. Between these two eras, one OPO ceased to serve a local liver transplant program and two OPOs began to serve new local liver transplant programs, so in comparisons between LSAM simulations and the current Share-35 allocation policy, we considered only the set of 50 OPOs that were serving local liver transplant programs in both eras.
For each scenario, a linear model between net import and each of the potential correlates was fitted, weighting by the number of organs recovered in each OPO. The significance of each of the potential correlates in a linear fit, and the correlation coefficients for significant associations, are reported.
Shifts in net import under redistricting
We compared each OPO’s current status as a net exporter or net importer of livers with the predicted net import under redistricting, to determine how many OPOs would change from net importers to net exporters and vice versa. We also considered how redistricting would impact the net import of livers for the set of OPOs in the highest and lowest quartiles of OPO performance. We included only the 50 OPOs that served a local liver transplant program in both eras. We compared net import under redistricting with current net import using the paired Wilcox rank-sum test.
RESULTS
Net importing and net exporting OPOs
With 8 optimized districts, 7 out of 23 OPOs that started as net exporters were predicted to become net importers, and 8 out of 27 OPOs that started as net importers were predicted to become net exporters. The 8 OPOs that became net exporters were predicted to have a median (range) net export of 15 (2–56) livers per year, while the 7 OPOs that became net importers were predicted to have a median (range) net import of 23 (1–67) livers per year.
With 4 optimized districts, 6 out of 23 OPOs that started as net exporters were predicted to become net importers, and 8 out of 27 OPOs that started as net importers were predicted to become net exporters. The 8 OPOs that became net exporters were predicted to have a median (range) net export of 20 (1–58) livers per year, while the 6 OPOs that became net importers were predicted to have a median (range) net import of 26 (3–82) livers per year.
Measuring performance by O:E liver yield, the OPOs that became net exporters were indistinguishable from the OPOs that became net importers, in both the 8-district (p=0.61, Wilcoxon test) and the 4-district (p=0.28) cases. That is, OPOs that became net exporters were not better-performing than OPOs that became net importers.
A summary of the actual counts of livers imported and exported in each scenario appears in Table 1. The median (range) number of exported livers per OPO increased with broader sharing from 28 (4–89) livers/OPO in the Share-35 era to 65 (15–154) livers/OPO in the 8-district simulation, and to 77 (21–188) livers/OPO in the 4-district simulation (linear model, p<0.001).
Table 1.
OPO Characteristics and Liver Transplants
| Share-35 (June 18, 2013 – June 17, 2014) | 8-districts simulation (2010–2011) | 4-districts simulation (2010–2011) | p-value | |
|---|---|---|---|---|
| Transplants per OPO-year, median (range) | 99 (15–313) | 93 (10–364) | 92 (10–374) | p = 0.14 |
| Exported livers per OPO-year, median (range) | 28 (4–89) | 65 (15–154) | 77 (21–188) | p < 0.001 |
| Imported livers per OPO-year, median (range) | 34 (2–166) | 56 (6–248) | 79 (9–292) | p < 0.001 |
| net-imported livers per OPO-year, median (range) | 1.5 (−70 to 86) | 1 (−77 to 158) | 0 (−81 to 170) | p = 0.97 |
| Normalized net-import per OPO-year, median (range) | 0.01 (−0.52 to 1.25) | 0.01 (−0.72 to 1.67) | −0.01 (−0.73 to 1.99) | p = 0.99 |
Between 2010–2011 and Share-35, one OPO ceased to serve a local liver transplant program and two OPOs began to serve new local liver transplant programs; these OPOs are excluded, and only the 50 OPOs common to both eras were included in this summary. For 8 and 4-district simulations, results were averaged from 10 simulation iterations with full district-wide sharing. Net import livers calculated as the difference in the number of livers exported and imported to the same OPO. Normalized net import calculated as the net imported livers divided by the number of recovered livers in the OPO.
Relationship between net import and O:E organ yield in 8 optimized districts
Comparing Share-35 to 8 optimized districts, the change in OPO net import was not correlated with O:E liver yield (p=0.73). That is, redistricting into 8 districts does not shift livers from OPOs with higher liver yield to OPOs with lower liver yield. Further, the net import to OPOs in the top quartile of O:E liver yield was not predicted to change (from a median net import of 0.31 in Share-35 to a median of 0.28 in 8 districts, p = 0.54 by paired Wilcox rank sum test), and OPOs in the lowest quartile of O:E liver yield were actually predicted to export more livers (changing from a median net import of 0.11 in Share-35 to −0.07 in 8 districts, p = 0.02).
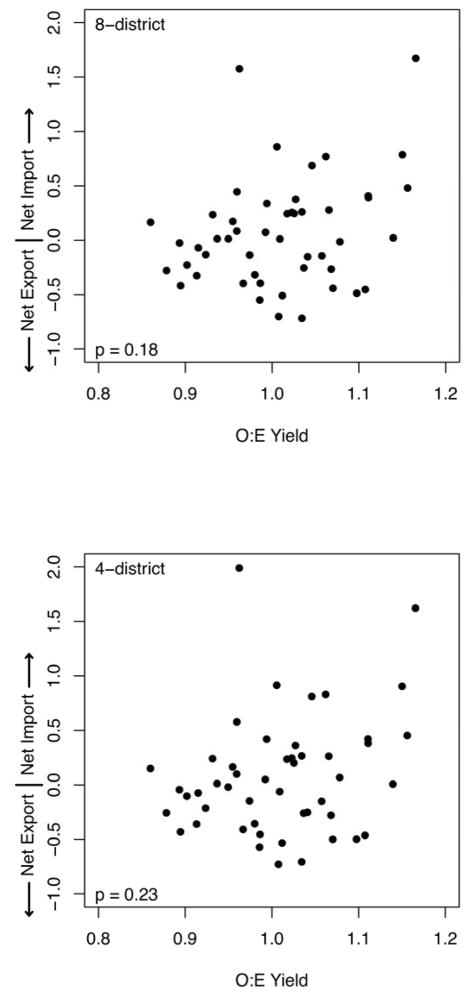
We found no evidence of any association between the O:E liver yield and net import of livers within the 8 district simulations (Figure 2). With 8 optimized districts, 16 out of 27 better-performing OPOs (those with O:E liver yield >1) would be net importers of livers, while only 10 out of 23 poorer-performing OPOs (those with O:E liver yield ≤ 1) would be net importers (p=0.41 by chi-square test). That is, with 8 optimized districts, livers do not flow from OPOs with higher liver yields to OPOs with lower liver yields.
Figure 2.
Net Import versus O:E Liver Yield
Relationship between net import and O:E organ yield in 4 optimized districts
Comparing Share-35 to 4 optimized districts, the change in OPO net import is not correlated with O:E liver yield (p=0.79). That is, redistricting into 4 districts does not shift livers from OPOs with higher liver yield to OPOs with lower liver yield. Further, the net import to OPOs in the top quartile of O:E liver yield was not predicted to change (from a median net import of 0.31 in Share-35 to a median of 0.26 in 4 districts, p = 0.68 by paired Wilcox rank sum test), and OPOs in the lowest quartile of O:E liver yield were actually predicted to export more livers (changing from a median net import of 0.11 in Share-35 to −0.07 in 4 districts, p = 0.013).
We found no evidence of any association between the O:E liver yield and net import of livers within the 4 district simulations (Figure 2). With 4 optimized districts, 16 out of 27 better-performing OPOs (those with O:E liver yield >1) would be net importers of livers, while only 9 out of 23 poorer-performing OPOs (those with O:E liver yield ≤ 1) would be net importers (p=0.26 by chi-square test). That is, with 4 optimized districts, livers do not flow from OPOs with higher liver yields to OPOs with lower liver yields.
Relationship between net import and liver donor conversion ratio in 8 optimized districts
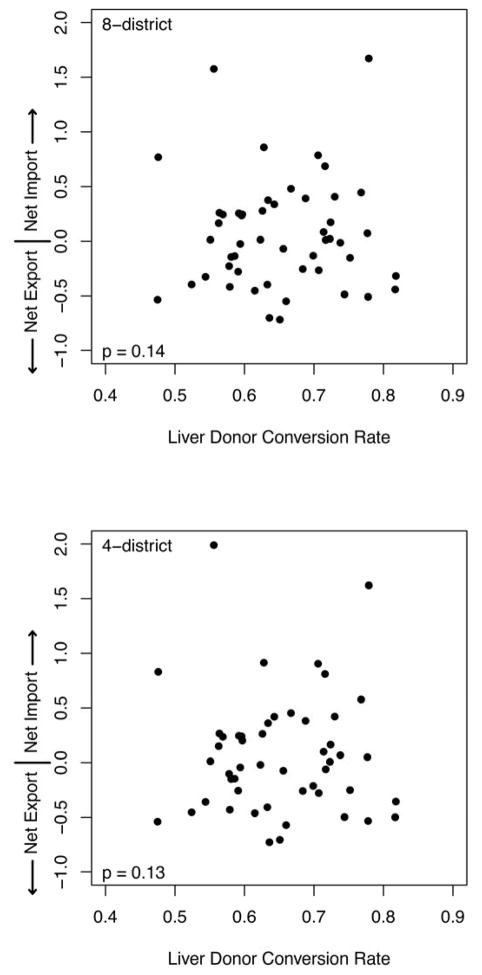
We found no evidence of any association between the liver donor conversion ratio and net import of livers in the 8-district simulations (Figure 3). With 8 optimized districts, 13 out of 25 OPOs with greater-than-median liver donor conversion ratios would be net importers of livers, while 13 out of 25 OPOs with lower-than-median liver donor conversion ratios would be net importers (p>0.99 by chi-square test). That is, redistricting was not predicted to shift livers from OPOs with higher liver donor conversion ratio to OPOs with lower liver donor conversion ratio.
Figure 3.
Net Import versus Liver Donor Conversion Rate
The net import to OPOs in the highest quartile of liver donor conversion ratios was not predicted to change in 8 optimized districts (from a median net import of −0.09 in Share-35 to 0.01 in 8 districts, p=0.95), and net import to the OPOs in the lowest quartile of liver donor conversion ratios was not predicted to change (from a median net import of −0.03 in Share-35 to −0.13 in 8 districts, p=0.68).
Relationship between net import and liver donor conversion ratio in 4 optimized districts
We found no evidence of any association between the liver donor conversion ratio and net import of livers in the 4-district simulations (Figure 3). With 4 optimized districts, 13 of 25 OPOs with greater-than-median liver donor conversion ratios would be net importers of livers, while 12 out of 25 OPOs with lower-than-median liver donor conversion ratios would be net importers (p>0.99 by chi-square test). That is, redistricting was not predicted to shift livers from OPOs with higher liver donor conversion ratio to OPOs with lower liver donor conversion ratio.
Net import to OPOs in the highest quartile of liver donor conversion ratios was not predicted to change in 4 optimized districts (from a median net import of −0.09 in Share-35 to 0.01 in 4 districts, p=0.74), and net import to the OPOs in the lowest quartile of liver donor conversion ratios was not predicted to change (from a median net import of −0.03 in Share-35 to −0.10 in 4 districts, p=0.74).
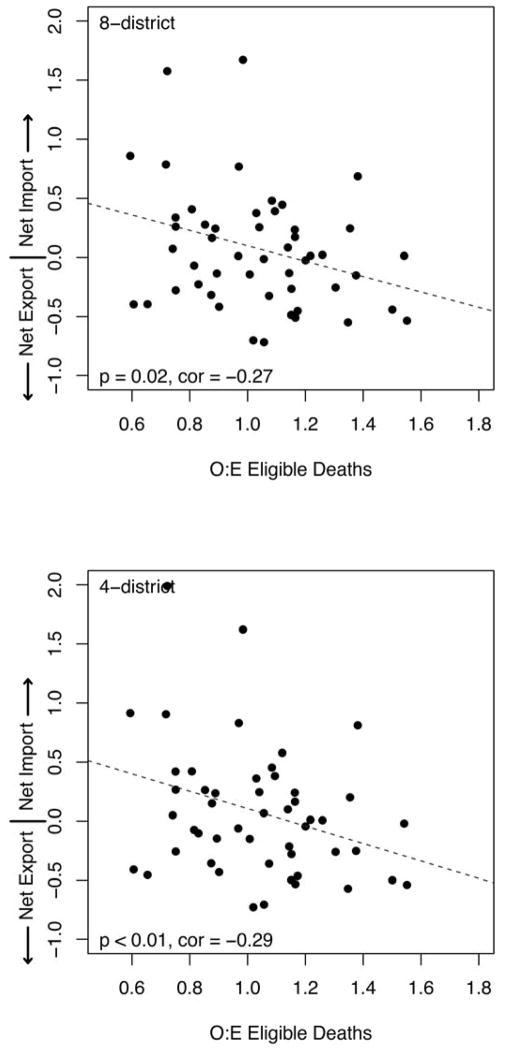
Relationship between net import and eligible deaths in 8 optimized districts
Net import of livers was significantly negatively correlated with O:E eligible deaths in the 8-district simulations, with a correlation coefficient of −0.27 (p=0.02, Figure 4). That is, under redistricting, OPOs that had more-than-expected eligible deaths than expected tended to be net exporters of livers, and OPOs that had fewer-than-expected eligible deaths than expected tended to be net importers of livers.
Figure 4.
Net Import versus O:E Eligible Deaths
Net import to OPOs in the highest quartile of O:E eligible deaths was predicted to decrease in 8 optimized districts (from a median net import of −0.12 in Share-35 to −0.15 in 8 districts, p = 0.003), and net import to the OPOs in the lowest quartile of O:E eligible deaths was not predicted to change (from a median net import of 0.02 in Share-35 to 0.26 in 8 districts, p=0.5).
Relationship between net import and eligible deaths in 4 optimized districts
Net import of livers was significantly negatively correlated with O:E eligible deaths in the 4-district simulations, with a correlation coefficient of −0.29 (p<0.01, Figure 4). That is, under redistricting, OPOs that had more-than-expected eligible deaths than expected tended to be net exporters of livers and OPOs that had fewer-than-expected eligible deaths than expected tended to be net importers of livers.
Net import to OPOs in the highest quartile of O:E eligible deaths was predicted to decrease in 4 optimized districts (from a median net import of −0.12 in Share-35 to −0.25 in 4 districts, p=0.002), and net import to the OPOs in the lowest quartile of O:E eligible deaths was not predicted to change (from a median net import of 0.02 in Share-35 to 0.26 in 4 districts, p=0.34).
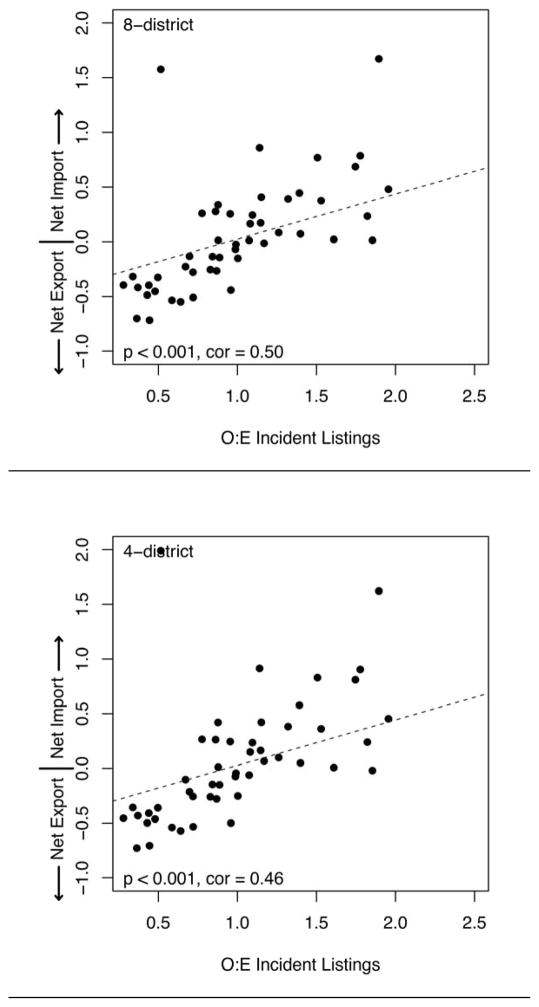
Relationship between net import and incident listings in 8 optimized districts
Net import of livers was significantly positively correlated with O:E incident listings in the 8-district simulations, with a correlation coefficient of 0.50 (p<0.001, Figure 5). With 8 optimized districts, 20 of the 22 OPOs with more-than-expected listings were net importers, while 22 out of the 28 OPOs with fewer-than-expected listings were net exporters (p<0.001 by chi-square test). That is, OPOs that had more-than-expected incident listings for liver transplantation tended to be net importers of livers and OPOs that had fewer-than-expected incident listings for liver transplantation tended to be net exporters of livers.
Figure 5.
Net Import versus O:E Incident Listings
Net import to OPOs in the highest quartile of O:E incident listings was not predicted to change in 8 optimized districts (from a median net import of 0.44 in Share-35 to 0.39 in 8 districts, p = 0.68), and net import to the OPOs in the lowest quartile of O:E incident listings was not predicted to change (from a median net import of −0.29 in Share-35 to −0.42 in 8 districts, p=0.15).
Excluding listings at MELD<15 from the calculation of O:E incident listings did not alter any of the findings reported in this section.
Relationship between net import and incident listings in 4 optimized districts
Net import of livers was significantly positively correlated with O:E incident listings in the 4-district simulations, with a correlation coefficient of 0.46 (p<0.001, Figure 5). With 4 optimized districts, 19 of the 22 OPOs with more-than-expected listings were net importers, while 22 out of the 28 OPOs with fewer-than-expected listings were net exporters (p<0.001 by chi-square test). That is, OPOs that had more-than-expected incident listings for liver transplantation tended to be net importers of livers and OPOs that had fewer-than-expected incident listings for liver transplantation tended to be net exporters of livers.
Net import to OPOs in the highest quartile of O:E incident listings was not predicted to change in 4 optimized districts (from a median net import of 0.44 in Share-35 to 0.38 in 4 districts, p = 0.79), and net import to the OPOs in the lowest quartile of O:E incident listings was not predicted to change (from a median net import of −0.29 in Share-35 to −0.46 in 4 districts, p=0.11).
Excluding listings at MELD<15 from the calculation of O:E incident listings did not alter any of the findings reported in this section.
DISCUSSION
In this national simulation study of the relationship between OPO characteristics and net import, redistricting liver allocation into 8 or 4 optimized districts was not predicted to transfer livers from better-performing OPOs to poorer-performing OPOs. In fact, the effect was quite the opposite: for both the 8 district and 4 district simulations, most (16 out of 27 in the 4 district case) of the better-performing OPOs (with O:E liver yield >1) were predicted to be net importers of livers, while most (13 out of 23 in the 4 district case) of the poorer-performing OPOs (with O:E liver yield ≤ 1) were predicted to be net exporters. As previously reported (12), most of the better-performing OPOs are net importers and most of the poorer-performing OPOs are net exporters under the current allocation system also.
However, consistent with the intent of redistricting, optimized districts were predicted to shift livers based on supply and demand: from OPOs with fewer-than-expected listings and with more-than-expected eligible deaths to OPOs with more-than-expected listings and fewer-than-expected eligible deaths.
Our simulation findings that livers would not shift from better-performing OPOs to worse-performing OPOs were consistent with patterns of organ flow seen since the implementation of broader sharing through Share-35. Although eligible deaths vary nearly four-fold between different donor service areas (11), the current Share-35 allocation has not shifted organs from OPOs with more-than-expected eligible deaths to OPOs with fewer-than-expected eligible deaths (12). Under redistricting, however, optimized plans are specifically designed to reduce geographic disparities in liver availability; not surprisingly, these redistricting plans are predicted to shift livers from OPOs with more-than-expected eligible deaths to OPOs with fewer-than-expected eligible deaths.
Redistricting would align liver distribution with the distribution of eligible deaths, and would not systematically disadvantage better-performing OPOs. Eligible deaths are not an OPO performance measure. Rather, eligible deaths reflect characteristics of the population living within an OPO’s donor service area. We found no correlation between O:E eligible deaths and either of the OPO performance measures discussed here (p=0.72 and p=0.23, O:E liver yield and liver donor conversion ratio, respectively by Pearson product-moment correlation).
Our study has the limitations inherent to any study that uses the Liver Simulated Allocation Model. The LSAM module that determines accept/decline decisions for liver offers is based on observed behavior, but possible behavior changes in response to changes in allocation are not modeled. Furthermore, the inputs for LSAM are from actual donors and candidates from the 2006–2010 era, as these are the most recent input files available.
Another limitation of our study is that it is not clear to what extent the enormous variation in listings for liver transplant reflects differences in the burden of liver disease, versus differences in access to the waitlist (16). It seems unlikely that eligibility for liver transplantation among those who are not currently waitlisted could be determined from available national datasets, given the complexity of determining transplant eligibility. While this is an interesting and frustrating issue, it is not particularly relevant to our findings, as the population served by liver allocation per se is the cohort of patients listed for a transplant. In any case, the current allocation system already shifts livers from OPOs with fewer-than-expected incident listings to OPOs with more-than-expected incident listings (12), so this pattern will continue with or without redistricting.
Finally, measuring OPO performance is a nuanced and possibly controversial endeavor. To address this challenge, we used two quite different performance metrics in the present study. One of these, the O:E liver yield, is a measure of the OPO’s ability to place livers from donors, adjusted for donor characteristics in each OPO. The other, the liver donor conversion ratio, is an unadjusted measure of the OPO’s success at converting eligible deaths to liver donors. We found no evidence of any relationship between either of these OPO performance metrics and the flow of livers under optimized redistricting. The consistency of our results across these two disparate metrics speaks to the robustness of the effect.
In conclusion, the two optimized redistricting plans that we studied are not predicted to transfer livers from better-performing OPOs to poorer-performing OPOs. Redistricting would instead change allocation so as to align liver distribution with the patterns of geographic variation in eligible deaths. Adopting either redistricting plan is predicted to shift livers from areas with fewer-than-expected listings and more-than-expected eligible deaths to areas with more-than-expected listings and fewer-than-expected eligible deaths.
Supplementary Material
Acknowledgments
The Liver Simulated Allocation Model and input data files have been supplied by the Scientific Registry of Transplant Recipients, UNOS, and the Minneapolis Medical Research Foundation under contract with HHS/HRSA. The authors alone are responsible for reporting and interpreting these data; the views expressed herein are those of the authors and not necessarily those of the US Government.
Dr. Segev is supported by grant number K24DK101828 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). This research was supported by an American Recovery and Reinvestment Act grant from the National Institute of Diabetes Digestive and Kidney Diseases, RC1 1RC1DK086450–01, and by Health Resources Services Administration contract #HHSH250201000018C.
Contributor Information
Sommer E. Gentry, Email: gentry@usna.edu.
Eric KH. Chow, Email: echow8@jhmi.edu.
Allan Massie, Email: amassie@jhsph.edu.
Xun Luo, Email: xluo9@jhu.edu.
Eugene Shteyn, Email: eshteyn@cdrg.org.
Joshua Pyke, Email: jpyke@cdrg.org.
David Zaun, Email: dzaun@cdrg.org.
Jon J. Snyder, Email: jsnyder@cdrg.org.
Ajay K. Israni, Email: aisrani@cdrg.org.
Bert Kasiske, Email: bkasiske@cdrg.org.
Dorry L. Segev, Email: dorry@jhmi.edu.
References
- 1.Barshes NR, Becker NS, Washburn WK, Halff GA, Aloia TA, Goss JA. Geographic disparities in deceased donor liver transplantation within a single UNOS region. Liver Transpl. 2007;13(5):747–51. doi: 10.1002/lt.21158. [DOI] [PubMed] [Google Scholar]
- 2.Roberts JP, Dykstra DM, Goodrich NP, Rush SH, Merion RM, Port FK. Geographic differences in event rates by model for end-stage liver disease score. Am J Transplant. 2006;6(10):2470–5. doi: 10.1111/j.1600-6143.2006.01508.x. [DOI] [PubMed] [Google Scholar]
- 3.Ubel PA, Caplan AL. Geographic favoritism in liver transplantation--unfortunate or unfair? N Engl J Med. 1998;339(18):1322–5. doi: 10.1056/NEJM199810293391811. [DOI] [PubMed] [Google Scholar]
- 4.Yeh H, Smoot E, Schoenfeld DA, Markmann JF. Geographic inequity in access to livers for transplantation. Transplantation. 2011;91(4):479–86. doi: 10.1097/TP.0b013e3182066275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Massie AB, Caffo B, Gentry SE, Hall EC, Axelrod DA, Lentine KL, et al. MELD Exceptions and Rates of Waiting List Outcomes. Am J Transplant. 2011;11(11):2362–71. doi: 10.1111/j.1600-6143.2011.03735.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Volk ML, Choi H, Warren GJ, Sonnenday CJ, Marrero JA, Heisler M. Geographic variation in organ availability is responsible for disparities in liver transplantation between Hispanics and Caucasians. Am J Transplant. 2009;9(9):2113–8. doi: 10.1111/j.1600-6143.2009.02744.x. [DOI] [PubMed] [Google Scholar]
- 7.Dzebisashvili N, Massie AB, Lentine KL, Schnitzler MA, Segev D, Tuttle-Newhall J, et al. Following the organ supply: assessing the benefit of inter-DSA travel in liver transplantation. Transplantation. 2013;95(2):361–71. doi: 10.1097/TP.0b013e3182737cfb. [DOI] [PubMed] [Google Scholar]
- 8.Gentry SE, Massie AB, Cheek SW, Lentine KL, Chow EH, Wickliffe CE, et al. Addressing Geographic Disparities in Liver Transplantation Through Redistricting. Am J Transplant. 2013 doi: 10.1111/ajt.12301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gentry S, Chow E, Massie AB, Segev D. Gerrymandering for justice: redistricting U.S. liver allocation (to appear) Interfaces. 2015 doi: 10.1287/inte.2015.0810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sung RS, Galloway J, Tuttle-Newhall JE, Mone T, Laeng R, Freise CE, et al. Organ donation and utilization in the United States, 1997–2006. Am J Transplant. 2008;8(4 Pt 2):922–34. doi: 10.1111/j.1600-6143.2008.02171.x. [DOI] [PubMed] [Google Scholar]
- 11.Sheehy E, O’Connor KJ, Luskin RS, Howard RJ, Cornell D, Finn J, et al. Investigating geographic variation in mortality in the context of organ donation. Am J Transplant. 2012;12(6):1598–602. doi: 10.1111/j.1600-6143.2011.03981.x. [DOI] [PubMed] [Google Scholar]
- 12.Gentry S, Chow E, Massie AB, Luo X, Segev D. Liver Sharing and Organ Procurement Organization Performance. Liver Transplant. 2015;21(3):293–9. doi: 10.1002/lt.24074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liver and Intestinal Transplantation Committee, Organ Procurement and Transplantation Network. Redesigning Liver Distribution to Reduce Variation in Access to Liver Transplantation. 2014 [Google Scholar]
- 14.Scientific Registry of Transplant Recipients. Technical methods for the OPO-specific reports. 2014 available at http://www.srtr.org/csr/current/Centers/201311/all_opo_documentation.pdf.
- 15.United States Census Bureau. 2010 TIGER/Line shapefiles (machine-readable data files) 2010 [Google Scholar]
- 16.Mathur AK, Ashby VB, Fuller DS, Zhang M, Merion RM, Leichtman A, et al. Variation in access to the liver transplant waiting list in the United States. Transplantation. 2014;98(1):94–9. doi: 10.1097/01.TP.0000443223.89831.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.