Abstract
Objective
Women with breast cancer (BCa) report elevated distress post-surgery. Group-based cognitive-behavioral stress management (CBSM) following surgery improves psychological adaptation, though its key mechanisms remain speculative. This randomized controlled dismantling trial compared two interventions featuring elements thought to drive CBSM effects: a 5-week Cognitive-Behavioral Training (CBT) and 5-week Relaxation Training (RT) vs. a 5-week Health Education (HE) control group.
Method
Women with stage 0-III BCa (N = 183) were randomized to CBT, RT, or HE condition 2–10 weeks post-surgery. Psychosocial measures were collected at baseline (T1) and post-intervention (T2). Repeated-measures ANOVAs tested whether CBT and RT treatments improved primary measures of psychological adaptation and secondary measures of stress management resource perceptions from pre- to post-intervention relative to HE.
Results
Both CBT and RT groups reported reduced depressive affect. The CBT group reported improved emotional well-being/quality of life and less cancer-specific thought intrusions. The RT group reported improvements on illness-related social disruption. Regarding stress management resources, the CBT group reported increased reliability of social support networks, while the RT group reported increased confidence in relaxation skills. Psychological adaptation and stress management resource constructs were unchanged in the HE control group.
Conclusions
Non-metastatic breast cancer patients participating in two forms of brief, 5-week group-based stress management intervention after surgery showed improvements in psychological adaptation and stress management resources compared to an attention-matched control group. Findings provide preliminary support suggesting that using brief group-based stress management interventions may promote adaptation among non-metastatic breast cancer patients.
Keywords: breast cancer, cognitive-behavioral therapy, relaxation therapy, distress
A breast cancer (BCa) diagnosis is a major life stressor compounded by surgery, chemotherapy, radiation, and hormonal treatments that impose significant physical and psychological challenges (Carlson et al., 2004). Women with BCa are among the most distressed of cancer subgroups, and those with non-metastatic BCa report distress related to fear of disease progression and recurrence (Herschbach et al., 2004). This distress can be manifested as depressed mood and elevated anxiety (Montanzer, 2008), disrupted quality of life and emotional well-being (Reich et al., 2008), and withdrawal from social activities during BCa treatment (Carver, Lehman, & Antoni, 2003). Further, cancer-specific distress in the form of cognitive intrusions about illness, prognosis, recurrence, death, and disability may occur (Tatrow & Montgomery, 2006) and are associated with worse quality of life (QOL) later in treatment (Golden-Kruetz et al., 2005).
Conversely, stress management interventions have the potential to ameliorate many of the negative psychosocial effects of cancer. Despite controversy regarding their effectiveness for all cancer patients (Coyne, Lepore, & Palmer, 2006), stress management interventions have been shown to improve QOL and decrease distress during cancer treatment (Jacobsen & Jim, 2008). The components of these interventions that generate improvements are underexplored (Phillips et al., 2012) and may provide insight into the ways to fine-tune interventions to maximize benefit.
One such intervention is group-based cognitive-behavioral stress management (CBSM), which combines cognitive-behavioral techniques and relaxation training. This intervention improves psychological adaptation during active treatment among women with non-metastatic BCa (Antoni et al., 2006b). Correlational evidence points to the role of perceived efficacy in using cognitive-behavioral processes and relaxation skills to explain its effects in women with BCa (Antoni et al., 2006a), and recent work has tested the effects of focused CBT interventions (Schnur et al., 2009), but no study has tested CBSM processes in a dismantling design.
Prior CBT-oriented interventions during primary treatment for breast cancer have ranged from 9–20 weeks, with 1.5–2 hour sessions each week (Fors et al., 2011), but this intensity may not be feasible in clinical oncology services. Studies of brief “clinic ready” interventions are needed in view of the limited time and resources for providing psychological support in the oncology setting (Stanton, Lueken, MacKinnon, & Thompson, 2013). Prior work suggests that the effects of a 10-week CBSM intervention may be observed in persons who attend as few as 5 weekly sessions (Antoni et al., 2006a), and 5-week CBSM interventions have also shown some positive effects in women with BCa (Groarke, Curtis, & Kerin, 2013). However, prior trials have not employed an attention-time matched control design to rule out the possibility that effects were driven by non-CBSM-specific group intervention processes (Cohen & Fried, 2007).
The current randomized controlled trial (RCT) addressed these limitations. It explored specific components of traditional CBSM by dismantling the intervention into two active 5-week treatment groups (i.e., Cognitive-Behavioral Training [CBT] and Relaxation Training [RT]) and examining changes in primary indicators of psychological adaptation and intermediary stress management resources as compared to an attention-matched Health Education (HE) control condition. We hypothesized that women assigned to the active intervention conditions would show improvements in psychological adaptation indicators, including general affect, cancer-specific distress, interpersonal disruption, and emotional well-being/QOL compared to the control condition at post-intervention follow-up. We further hypothesized that the CBT group, which focused on cognitive-behavioral and interpersonal skills training, would show differential increases in perceived social support resources, while the RT group would show differential increases in perceived efficacy for using relaxation skills to deal with stress at post-intervention follow-up. Although true mediation tests could not be conducted because the present study involves concurrent outcome measures, intervention-specific stress management resources were further examined as provisional mediators of intervention effects on psychological adaptation.
Method
Participants
Women age 21 or older with stage 0 – III BCa were recruited within 10 weeks of primary surgery from community clinics and cancer centers in the Miami area between 2006 and 2013. Consecutive cases from these sites were referred by surgical oncologists and provided consent to be contacted by our team, and were mailed informational pamphlets and pre-screened via phone. A total of 739 women were approached, and 183 women (25%) entered the study (see Results for detailed information on participation). Potential participants were excluded if they had prior cancer or neo-adjuvant treatment, severe psychiatric illness, acute or chronic medical conditions, or were not fluent in English. These exclusion criteria were established to ensure participants’ ability to participate in the intervention trial and to form a homogenous sample.
Procedures
The study was a single-center, single-blind, randomized controlled trial conducted within the Psychology Department at the University of Miami and approved by the Institutional Review Board (National Institutes of Health Clinical Trial NCT02103387). Women who met criteria provided written informed consent, completed a baseline (T1) psychological questionnaire packet within 2–10 weeks after surgery, and were compensated $50. Demographic data were collected via self-report at baseline, and medical data were collected via self-report and medical chart review. Participants were then randomized into groups of 3–7 women to receive either 5 weeks of CBT intervention (N = 55), RT intervention (N = 70), or HE control (N = 58). A project coordinator not involved in intervention administration or assessment generated the random allocation sequence, enrolled participants, and assigned participants to groups. The sequence of the groups was pre-determined by a drawing. After the 5 weekly sessions, approximately 2 months post-baseline, women completed a second questionnaire packet (T2), which was similar to the baseline questionnaire. Research assistants who were blinded to the condition mailed or administered the T2 questionnaire. Women were compensated $25 for the completion of the T2 assessment. A number of other secondary measures of interest were collected at both T1 and T2 to provide insights into mediator and moderator variables. The trial was considered complete when the study end date was reached and funding stopped.
Intervention Conditions
All conditions were administered across a 5-week span based on previous findings from a 10-week group-based CBSM trial (Antoni et al., 2006b) showing that women who attended 5 sessions experienced improved psychological adaptation that did not differ from those attending 8–10 sessions. Groups met weekly at the University of Miami for 1.5-hour sessions and were co-led by Master’s level students in a clinical psychology doctoral program who were trained in the protocols for each condition. There were six interventionists involved in the trial. Women were compensated $10 per session to offset the costs of travel and parking. Fidelity was monitored by two licensed psychologists who viewed the videotaped sessions for all three conditions, and drift was minimized by weekly supervision with interventionists to provide feedback on competence and adherence to protocol. No study-related adverse events were reported.
Cognitive-behavioral training condition
The CBT group was modeled after the cognitive-behavioral components of a structured, manualized group intervention (Antoni, 2003) used previously for post-surgical BCa patients (Antoni et al., 2006a). The intervention taught women adaptive coping skills to manage daily stressors and encouraged utilization of social resources, with a special emphasis on issues related to cancer and treatment. The intervention involved in-session experiential exercises to teach CBT techniques as well as out-of-session assignments for at-home practice of CBT skills (e.g., thought monitoring). Specific intervention content was condensed to a 5-week protocol covering awareness of stressors, cognitive restructuring (Beck & Emery, 1985), coping skills training (Folkman & Greer, 2000), and skills for social support utilization, anger management to promote conflict resolution, and assertiveness training (Fensterheim & Baer, 1975) to promote support seeking and emotional expression.
Relaxation training condition
The RT group was also modeled after the structured, manualized group intervention (Antoni, 2003) used in the previous 10-week CBSM intervention (Antoni et al., 2006a) but utilized only the relaxation components. The aim of the intervention was to teach relaxation techniques to promote anxiety reduction (via relaxing imagery and muscle relaxation; Bernstein & Borkovec, 1973). This involved in-session experiential exercises to teach RT techniques and out-of-session assignments for at-home practice of RT skills. Group members were provided with audio recordings of the group leader reciting relaxation exercises and were encouraged to practice these exercises daily. Selection of specific RT content for the 5-week intervention was based partly on feedback obtained from women following the 10-week CBSM group intervention (Antoni et al., 2006a). RT modules included abdominal breathing, progressive muscle relaxation, guided imagery, and meditation.
Health education condition
HE served as an attention and time-matched control group with educational content derived primarily from the American Cancer Society (2006) as well as the National Cancer Institute, Susan G. Komen, Dr. Susan Love Research Foundation, and the Livestrong Foundation. The 5-week FIE group included information related to BCa diagnosis and treatment, available resources, side-effect management, recurrence, healthy lifestyle behaviors (i.e., physical activity, nutrition, and sleep), and QOL after BCa. By providing pertinent information related to BCa, the HE condition reduced the risk of attrition often associated with treatment-as-usual control groups. This control condition was unique in that it was conducted in a group format, providing women with opportunities for positive social comparisons and group support. The HE condition lacked the active ingredients of the intervention groups, including opportunities to learn coping strategies and relaxation techniques as well as weekly home practice. This creates a strong test of the different interventions’ specific content. One drawback of the HE group is that it contains many influential intervention ingredients (e.g., information and social support), potentially hindering the ability to detect differences from the active intervention conditions tested in this trial.
Measures
Four primary outcome variables were examined to assess intervention effects on psychological adaptation. Together, this battery provides an assessment of general affect as well as illness-specific thought intrusions, social disruption, and emotional well-being.
Depressive affect
Depressive affect was assessed using the depression subscale of the 40-item Affects Balance Scale (ABS; Derogatis, 1975), which has been previously used in research on BCa patients (e.g., Antoni et al., 2006a). Respondents are provided with a list of adjectives and asked to indicate the degree to which they felt each emotion during the past week. Response options range from Never (1) to Always (5). The ABS-depressive affect subscale score was calculated as the mean response score of five items: sad, hopeless, worthless, miserable, unhappy. Reliability of this subscale was high, α> .90.
Cancer-specific distress
Intrusion of cancer-related thoughts was assessed using the Intrusions subscale of the Impact of Event Scale – Revised (IES-R; Weiss, 2007). Intrusions are unwanted thoughts about cancer, its treatment, recurrence, and implications for one’s life. This scale was chosen because it was shown to be affected by the 10-week CBSM intervention in this population (Antoni et al., 2006b). The seven items from the IES-Intrusion (IES-I) subscale ask participants to consider difficulties they may be experiencing with respect to BCa, such as “having dreams about it,” and to indicate how distressing these difficulties have been during the past week. Response options range from Not at all (0) to Extremely (4). The IES-I subscale score was calculated as the mean score of these seven item responses. The internal consistency of the IES-I in the current sample was high, α = .92.
Social disruption
The tendency to disengage from social activities is an important aspect of life disruption in BCa patients (Antoni, 2003; Carver et al., 2003). In the current sample, disruption in social interactions was measured with the 11-item Sickness Impact Profile – Social Interaction subscale (SIP-SI; Bergner, Bobbitt, Carter, & Gilson, 1981). Improvements in the SIP-SI were found in a 10-week CBSM intervention in BCa patients (Antoni et al., 2006a). Participants are asked to determine how 11 statements apply to their activities over the “past few weeks,” such as “I am going out less to visit people” or “I am avoiding social visits from others.” Two response options are provided: No (1) or Yes, this applies to me (2). Scores on this measure were calculated by a weighted formula (Bergner et al., 1981), with higher scores representing higher levels of disruption. The internal consistency of the SIP-SI subscale was high, □α = .90.
FACT emotional well-being
Because the current study specifically targeted psychological adaptation to BCa, emotional adjustment was measured using the Emotional Well-being (EWB) subscale of the Functional Assessment of Cancer Therapy – Breast (FACT-B; Brady et al., 1997). The FACT-B is an extension of the FACT-General (FACT-G; Cella et al., 1993) developed for and validated in BCa samples. The FACT-EWB subscale assesses the extent to which participants experience aspects of emotional well-being, such as “I worry about dying,” “I am satisfied with how I am coping with my illness,” and “I am losing hope in the fight against my illness” over the past week. Response options range from Not at all (1) to Very much (5). The FACT-EWB subscale was calculated as the mean score of six such item responses. The internal consistency of the FACT-EWB subscale in the current sample was high, α = .87.
Stress management resources
Two intermediary variables were assessed to reflect the proximal effects of the specific interventions tested—one focused on interpersonal resources and one on perceived relaxation skills. Previous work has shown that social support can mediate CBSM intervention effects on mood among HIV-infected individuals (Lutgendorf et al., 1998). In the current study, perceived social support was conceptualized as an interpersonal resource for managing stress and was assessed using the Social Provisions Scale (SPS; Cutrona & Russell, 1987). The CBT condition focused, among other targets, on teaching interpersonal skills, such as identifying sources of support within one’s support network, assertiveness skills, and anger management, in order to identify, utilize, and maintain social resources for managing stress (Antoni, 2003). We hypothesized that CBT participants would show increases in the Reliable Alliance (SPS-RA) subscale (e.g., having people to depend on if needed). Participants described the extent to which such statements as “there are people I can depend on in an emergency” apply to their current relationships with others. Response options range from I agree a lot (1) to I disagree a lot (5). The SPS-RA subscale was calculated as the mean score of four such item responses. The internal consistency of the SPS-RA subscale was adequate, α > .71.
A subset of the Measure of Current Status – Part A (MOCS-A; Carver, 2006) assessed women’s perceived ability to utilize skills targeted by the intervention. Previous work utilized principal component analysis to identify four factors (Antoni et al., 2006a) of the MOCS-A. Of these four factors, the MOCS-relaxation subscale was chosen for the current study to test the hypothesized effect of the RT intervention on perceived relaxation skills. The MOCS-relaxation subscale assesses one’s perceived ability to relax at will using two response items: “I am able to use mental imagery to reduce any tension I experience” and “I am able to use muscle relaxation techniques to reduce any tension I experience.” Response options range from I cannot do this at all (1) to I can do this extremely well (5). The MOCS-relaxation subscale score was calculated as the mean score of these two item responses. The internal consistency of the MOCS-relaxation subscale in the current sample was adequate, α = .81.
Covariates
Theory and previous empirical data have highlighted important relations between medical variables and the psychological variables of interest. Specifically, previous literature suggests that women’s disease stage and the amount of time between surgery and initial psychological assessment may influence self-reported psychological adaptation (e.g., Montazeri, 2008). Therefore, these variables were collected by medical chart review at the women’s surgical oncologists’ offices. Disease stage was coded as 0,I, II, or III. Time since surgery was calculated as the number of days from date of surgery to T1 assessment.
Analytic Approach
A priori power analysis using the NQuery Program indicated that a sample size of 60 participants per condition (180 total) would provide 75% power to detect a medium effect size (d = 0.5; Cohen, 1988) at p < .05. Data were examined for outliers, skewness, and kurtosis. Variables with outliers greater than 3 standard deviations from the mean were winsorized (Wilcox, 1993). Intervention effects were tested using 3-group (CBT, RT, HE) x 2 time-point (T1, T2) repeated-measures analysis of variance (ANOVA) in SPSS-version 21, which uses list-wise deletion for cases with missing values. Unfortunately, the use of only two timepoints in the present study precludes the use of some of the more recent approaches to repeated measures, such as Latent Growth Modeling (LGM), because LGM requires ‘a continuous dependent variable measured on at least three different occasions’ (Kline, 2011, p.304). Follow-up interaction contrasts testing T1 to T2 changes between pairs of groups were conducted using the error term from the overall analysis. Analyses included all participants for whom T2 post-intervention data were available, even if participants did not attend all sessions, and all ANOVAs controlled for stage, time since surgery, and income. Cohen’s d (Cohen, 1988), widely accepted as a measure of clinically meaningful change after psychological intervention (Eisen, Ranganathan, Seal, & Spiro, 2007), was used to assess the clinical significance of intervention effects in interaction contrasts between intervention groups and HE control with the conventional benchmarks suggested by Cohen (1988): small (d = 0.2), medium (d = 0.5), and large (d = 0.8). Cohen’s (1988) benchmarks for partial η2 were used for omnibus ANOVA tests: small (η2 = 0.01), medium (η2 = 0.06), and large (η2 = 0.14) effects.
Results
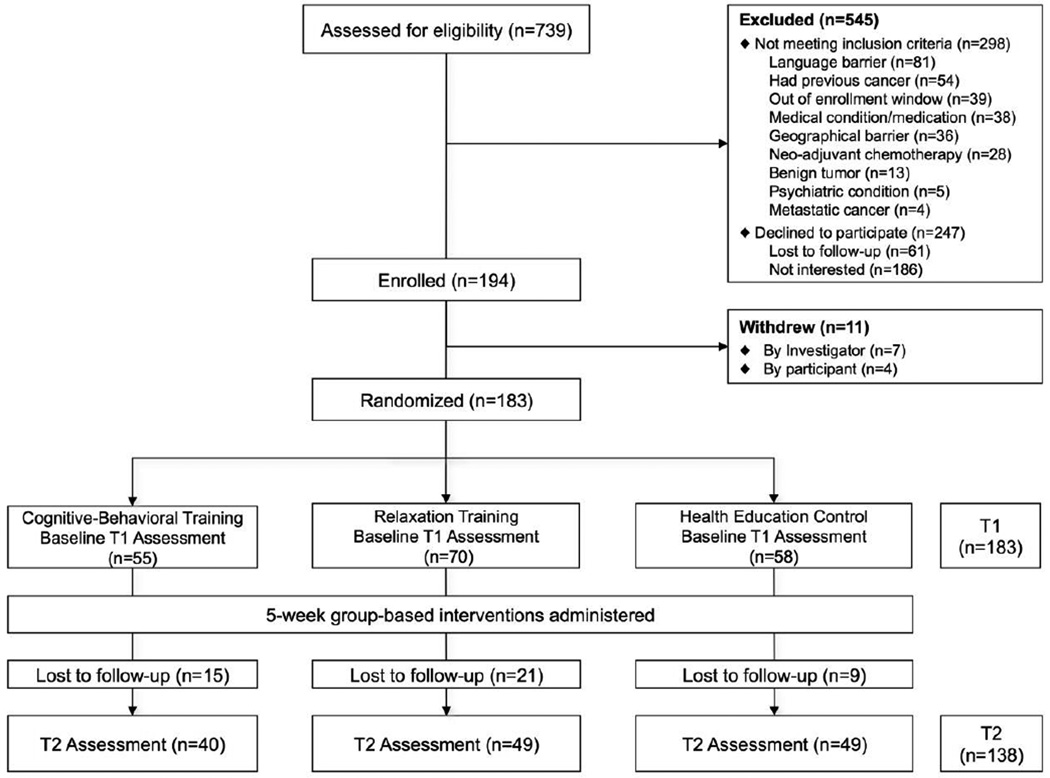
See Figure 1 for CONSORT diagram of study enrollment. Of the 739 women screened between 2006 and 2013, 298 did not meet inclusion criteria; 247 declined participation due to lack of time, transportation difficulties, or lack of interest. A total of 194 women gave informed consent; however, 11 of them withdrew prior to T1 assessment and randomization. A total of 183 women completed a Tl assessment and were randomly assigned to one of the 3 study groups. Fifty-five women were randomized to CBT, 70 to RT, and 58 HE. A total of 138 women completed the T2 post-intervention follow-up assessment, approximately 2 months post-baseline.
Figure 1.
CONSORT flow diagram.
Sample Demographics
Women in the sample ranged in age from 28 to 80 years, with an average age of 54.28 (SD = 10.06). Chart reviews revealed that 19.1% of these women were diagnosed with stage 0 ductal carcinoma in-situ (DCIS), 51.4% had stage I BCa, 24.0% had stage II BCa, 4.9% had stage III BCa. The majority of women were estrogen-receptor (ER) positive (72.7%) and progesterone-receptor (PR) positive (65.0%), and 16.4% had positive lymph nodes. Women underwent either a lumpectomy (48.6%) or a mastectomy (51.4%). Women enrolled in the study an average of 37.42 days following surgery (SD = 22.30). The majority of women self-identified as either Hispanic (41.5%) or non-Hispanic White (41.5%) with an additional 8.7% self-identifying as Black/African-American, and 6.6% representing other ethnic categories. Most women were partnered (63.9%). Median annual household income was $100,000 per year; median years of education was 16 years.
Group differences on demographic characteristics, medical and treatment-related factors, and psychotropic medication usage were assessed with chi-square tests and one-way ANOVAs (Table 1). The study conditions differed significantly only on reported income, with women in HE reporting the greatest income. Thus, income was included as a covariate in all analyses. The number of sessions attended did not significantly differ across the study conditions (CBT M = 3.98, SD = 1.47; RT M = 3.61, SD = 1.58; HE M = 4.29, SD = 1.08) (p > .05). Session attendance was not significantly associated with the magnitude of T1 – T2 changes in most outcomes within any of the three study conditions. The one exception was that attendance correlated positively with change in SPS-RA from T1 to T2 among women in the CBT group (r = 0.49, p = .003). From the T1 assessment to the post-intervention assessment, retention rates did not significantly differ as a function of group assignment (χ2(2) = 3.87, p = .144).
Table 1.
Means, Standard Deviations, and Frequencies for Demographic and Medical Variables by Group
| Variable | CBT (n = 55) |
RT (n = 70) |
HE (n = 58) |
Statistic | P |
|---|---|---|---|---|---|
| Age (yrs), 23–80 | 54.62 (9.2) | 53.69(11.5) | 54.67(9.1) | F(2,180) = 0.20 | .823 |
| Race/Ethnicity | χ2(6) = 4.08 | .665 | |||
| Non-Hispanic White | 25 (45.5%) | 24 (34.3%) | 27 (46.6%) | ||
| Hispanic | 20 (36.4%) | 33 (47.1%) | 23 (39.7%) | ||
| African-American | 4 (7.3%) | 6 (8.6%) | 6 (10.3%) | ||
| Other | 5(9.1%) | 5(7.1%) | 2(3.4%) | ||
| Income (thousands) | 103.11 (62.0) | 87.02 (57.9) | 116.62(78.5) | F(2,180) = 3.20 | .043 |
| Education (years) | 16.15(2.6) | 17.41 (14.6) | 15.60(3.2) | F(2,176) = 0.62 | .533 |
| Married/partnered | 39 (70.9%) | 40(57.1%) | 38 (65.5%) | χ2(2) = 2.39 | .303 |
| Stage | χ2(6) = 2.36 | .883 | |||
| 0 | 11 (20.0%) | 12(17.1%) | 12 (20.7%) | ||
| I | 31 (56.4%) | 34 (48.6%) | 29 (50.0%) | ||
| II | 11 (20.0%) | 20 (28.6%) | 13 (22.4%) | ||
| III | 2(3.6%) | 3 (4.3%) | 4 (6.9%) | ||
| Positive Nodes | 5(9.1%) | 13 (18.6%) | 12 (20.7%) | χ2(2) = 2.81 | .245 |
| Hormonal Status | |||||
| ER Positive | 40 (72.7%) | 55 (78.6%) | 38 (65.5%) | χ2(2) = 3.56 | .169 |
| PR Positive | 35 (63.6%) | 48 (68.6%) | 36(62.1%) | χ2(2) = 0.43 | .806 |
| Surgical Procedure | χ2(2) = 0.82 | .662 | |||
| Lumpectomy | 24(43.6%) | 35 (50.0%) | 30(51.7%) | ||
| Mastectomy | 31 (56.4%) | 35 (50.0%) | 28 (48.3%) | ||
| Days Since Surgery | 36.73 (25.0) | 39.36 (22.8) | 35.72(18.9) | F(2,180) = 0.46 | .635 |
| Adjuvant Treatment | |||||
| Chemotherapy | 9 (16.4%) | 16 (22.9%) | 14(24.1%) | χ2(2)=1.12 | .570 |
| Radiation | 7 (12.7%) | 10 (14.3%) | 15 (25.9%) | χ2(2) = 2.68 | .263 |
| Anti-hormonal | 11 (20.0%) | 16 (22.9%) | 11 (19.0%) | χ2(2)=1.28 | .528 |
| Baseline Medication | |||||
| Anti-depressant | 11 (20.0%) | 7 (10.0%) | 3 (5.2%) | χ2(4) = 7.18 | .127 |
| Anti-anxiety | 11 (20.0%) | 11 (15.7%) | 7(12.1%) | χ2(4) = 3.09 | .543 |
| Sleep | 11 (20.0%) | 12(17.1%) | 10 (17.2%) | χ2(4)=1.86 | .762 |
| Pain | 12(21.8%) | 14 (20.0%) | 9(15.5%) | χ2(4)=1.71 | .788 |
Mean (SD) or Frequency (%)
CBT = Cognitive-Behavioral Training; RT = Relaxation Training; HE = Health Education; NHW = Non-Hispanic White; ER = Estrogen Receptor; PR = Progesterone Receptor; T1 = Baseline Assessment; T2 = Post-intervention Assessment
We also compared outcome and intermediary variables for group differences at T1. Unexpectedly, we found significant differences in ABS-depressive affect (F[2,178] = 4.33, p = .015, η2 = .05), IES-I (F[2,176] = 4.35, p = .014, η2 = .05), and SIP-SI (F[2,177] = 3.45, p = .034, η2 = .04). Specifically, baseline ABS-depressive affect scores were significantly lower in the HE group than in the CBT (p = .005) or RT group (p = .040), baseline IES-I scores were significantly higher in the CBT group than in the RT (p = .023) or HE group (p = .006), and baseline SIP-SI scores were significantly lower in the HE group than in the RT group (p = .010). Results must be interpreted with these baseline differences in mind.1
Psychological Adaptation Indicators
Depressive affect
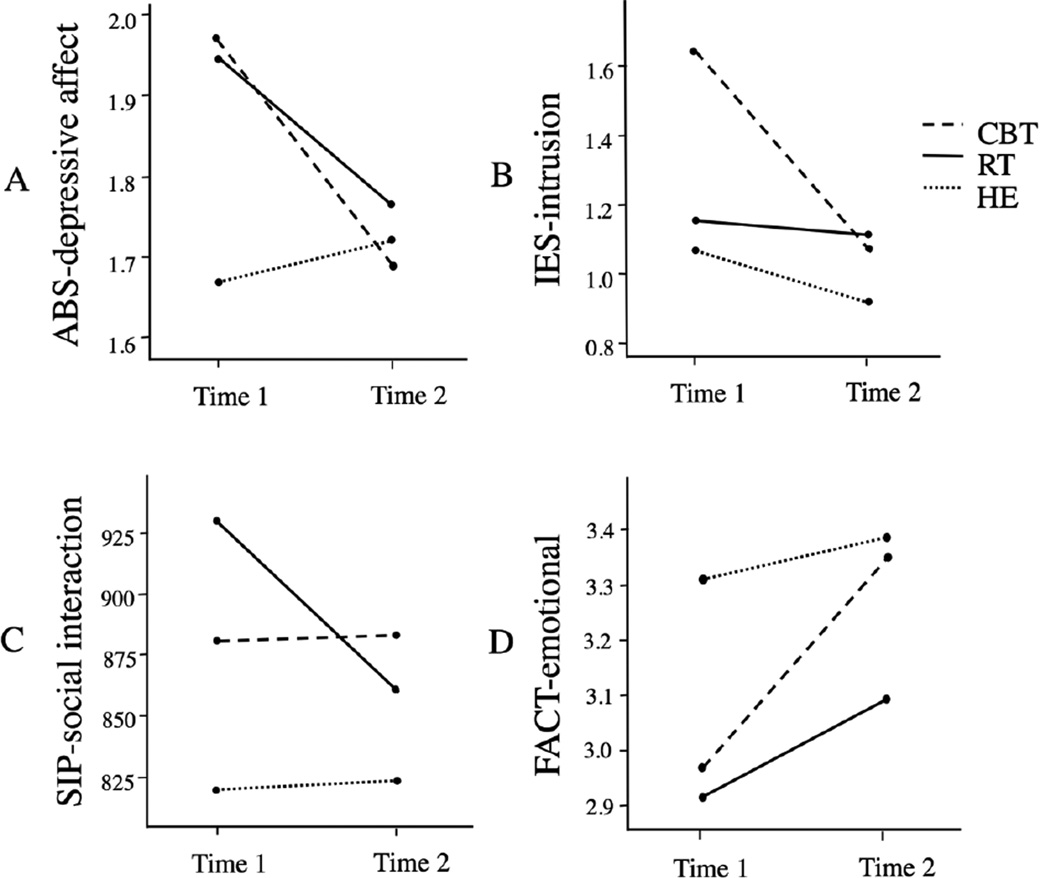
A 3×2 repeated-measures ANOVA revealed a significant group by time effect on ABS-depressive affect, F(2,131) = 5.61, p = .005, η2 = .08. An interaction contrast (2×2, repeated-measures by pair of groups) found that women in CBT showed significantly greater improvement in ABS-depressive affect scores compared to those in HE, F(1,131) = 10.51, p = .002, d = 0.69, 95% CI [0.64, 0.73]. Women in RT also showed significantly greater improvements in ABS-depressive affect than those in HE, F(1,131) = 4.91, p = .028, d = 0.48, 95% CI [0.43, 0.52]. An interaction contrast comparing CBT with RT showed no significant differences in ABS-depressive affect scores over time, F(1,131) = 0.50, p = .479. Within-condition simple effect tests showed significant decrease in ABS-depressive affect in CBT (t[136] = −3.74, p < .001, d = 0.46, 95% CI [0.41, 0.50]) and RT (t[136] = −2.64, p = .009, d = 0.29, 95% CI [0.25, 0.33]) but no change in HE (t[136] = 0.75, p = .454; see Figure 2a).
Figure 2.
Four indices of psychological adaptation indicators among women in the three study conditions (CBT vs. RT vs. HE) at baseline (Time 1) and post-intervention (Time 2). Means are adjusted for the following covariates: disease stage, time since surgery, and baseline income. Note: ABS is Affects Balance Scale; IES is Impact of Event Scale; SIP is Sickness Impact Profile; FACT is Functional Assessment of Cancer Therapy; CBT is Cognitive Behavioral Training; RT is Relaxation Training; HE is Health Education.
Cancer-specific distress
A3×2 repeated-measures ANOVA yielded a significant group by time effect on IES-I, F(2,131) = 7.20, p = .001, η2 = . 10. An interaction contrast showed that women in CBT showed significantly greater improvements in IES-I than those in HE, F(1,131) = 8.65, p = .004, d = 0.62, 95% CI [0.58, 0.67]. Changes in IES-I also differed significantly between CBT and RT groups, F(1, 131) = 11.85,p < .001, d = 0.78, 95% CI [0.73, 0.82], such that improvements in cancer-specific distress were greater among women in the CBT group than among those in the RT group. IES-I changes for women in RT did not differ from those in HE, F(1,131) = 0.72, p = .399. Within-condition simple effect tests showed that IES-I scores significantly decreased for women in CBT (t[136] = −5.45, p < .001, d = 0.69, 95% CI [0.64, 0.74]), but remained unchanged for women in RT (t[136] = −0.43, p = .668) and HE (t[136] = − 1.61, p = .109; see Figure 2b).
Social disruption
A 3×2 ANOVA yielded a significant group by time effect on SIP-Social Interactions (SI), F(2,131) = 3.82, p = .024, η2 = .06. An interaction contrast showed that women in RT showed significantly greater reductions in SIP-SI than those in HE, F(1,131) = 4.39, p = .038, d = 0.50, 95% CI [0.46, 0.54]. Another interaction contrast showed that changes in SIP-SI differed significantly between CBT and RT, F(1,131) = 6.53, p = .012, d = 0.51, 95% CI [0.46, 0.55], such that social disruption decreased among women in RT but increased among those in CBT. SIP-SI changes for women in CBT did not differ from those in HE, F(1,131) = 0.01, p = .915. Within-condition simple effect tests showed that SIP-SI scores significantly decreased for women in RT (t[136] = −2.24, p = .027, d = 0.27, 95% CI [0.23, 0.31]) but were unchanged for women in either CBT (t[ 136] = 1.27, p =.206) or HE (t[136] = 1.34, p = .184; see Figure 2c).
FACT emotional well-being
A 3×2 ANOVA revealed a significant group by time effect on FACT-EWB, F(2,131) = 3.08, p = .049, η2 = .05. An interaction contrast showed that women in CBT showed significantly greater improvement in FACT-EWB scores than those in HE, F(1,131) = 6.98, p = .009, d = 0.52, 95% CI [0.47, 0.56]. FACT-EWB change among women in RT did not differ significantly from those in HE, F(1,131) = 0.08, p = .777. Changes in FACT-EWB did not differ between CBT and RT, F(1, 131) = 0.72, p = .399. Within-condition simple effect ANOVAs showed FACT-EWB scores significantly increased among women in both CBT (t[136] = 4.11,p < 0.001, d = 0.58, 95% CI [0.53, 0.63]) and RT (t[136] = 2.07, p =.040, d = 0.26, 95% CI [0.22, 0.30]), but were unchanged among women in HE (t[136] = 0.93, p = .356; see Figure 2d).
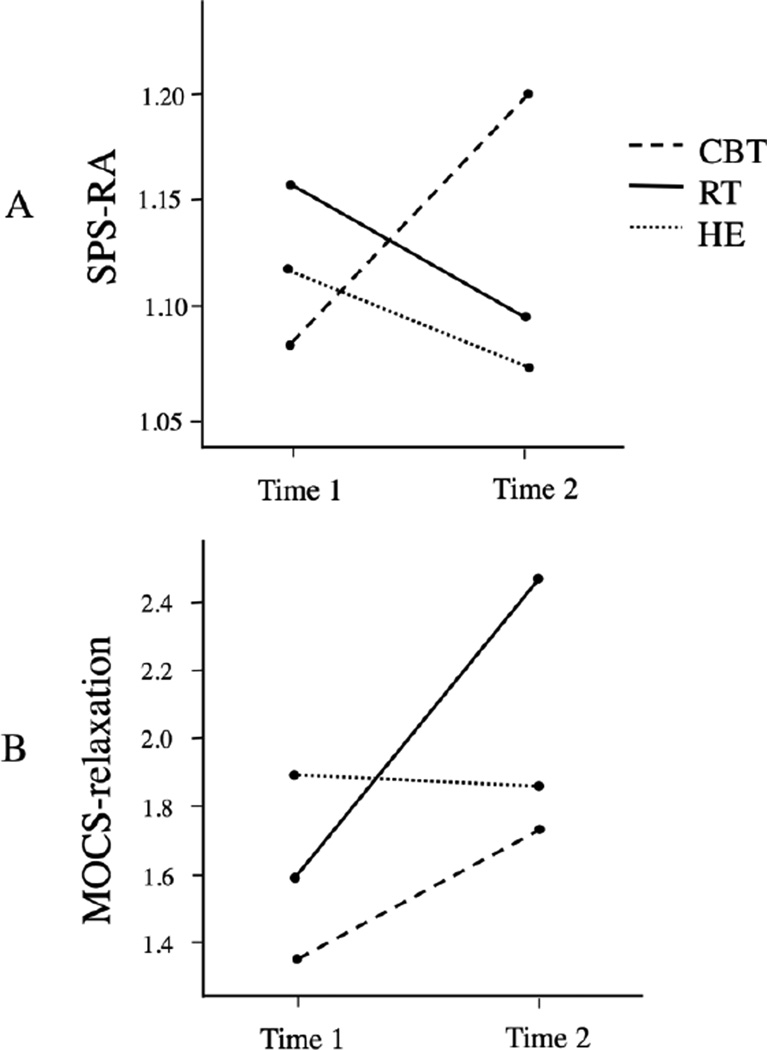
Stress Management Resources
Interpersonal resources
A 3×2 repeated-measures ANOVA yielded a significant group by time effect on SPS-RA, F(2,130) = 5.85, p = .004, η2 = .08. An interaction contrast showed that women in CBT had significantly greater improvements in SPS-RA scores than those in HE, as predicted, F(1,130) = 8.32, p = .005, d = 0.61, 95% CI [0.57, 0.66]. SPS-RA also improved significantly more among women in the CBT group than among women in the RT group, F(1,130) = 10.65, p = .001, d = 0.67, 95% CI [0.62, 0.71]. SPS-RA changes among women in RT did not differ from those among women in HE, F(1,130) < 0.01, p = .999. Within-condition simple effect tests showed that SPS-RA scores significantly increased among women in CBT (t[135] = 2.83, p =.005, d = 0.48, 95% CI [0.43, 0.53], but were unchanged for women in either RT (t[135] = −1.60, p = .112) or HE (t[135] = −125, p = .214; see Figure 3a).
Figure 3.
Two indices of stress management resources among women in the three study conditions (CBT vs. RT vs. HE) at baseline (Time 1) and post-intervention (Time 2). Means are adjusted for the following covariates: disease stage, time since surgery, and baseline income. Note: SPS-RA is Social Provisions Scale Reliable Alliance; MOCS is Measure of Current Status; CBT is Cognitive Behavioral Training; RT is Relaxation Training; HE is Health Education.
Perceived relaxation skills
In a 3×2 repeated-measures ANOVA, there was a significant group by time effect on MOCS-relaxation skills, F(2,131) = 10.01, p < .001, η2 = .13. An interaction contrast showed that women in RT showed significantly greater improvement in MOCS-relaxation scores relative to those in HE, as predicted, F(1,131) = 20.81, p < .001, d = 0.92, 95% CI [0.88, 0.96]. Change in MOCS-relaxation also differed significantly between RT and CBT groups, F(1,131) = 6.41, p = .013, d = 0.51, 95% CI [0.46, 0.55]. Women in CBT showed marginally better improvement in MOCS-relaxation relative to HE, F(1,131) = 3.29, p = .072, d = 0.42, 95% CI [0.38, 0.47]. Within-condition simple effect ANOVAs showed significant increases in MOCS-relaxation scores in both RT (t[136] = 6.35, p <.001, d = 0.82, 95% CI [0.77, 0.86]) and CBT (t[136] = 2.46, p = .015, d = 0.36, 95% CI [0.31, 0.41]), with no change observed in HE (t[136] = −0.20, p = .841; see Figure 3b).
Commonalities
The design of this study does not permit a test of true mediation. However, we conducted one more set of analyses to assess the plausibility of such a relationship. These tests involved repeating the analyses in which a treatment group experienced a benefit over time compared to the control group, but with an additional control for change in the stress management resource that was also affected by that treatment (i.e., interpersonal resources for CBT, relaxation skills for both RT and CBT).
Interaction contrasts adding this control for change in interpersonal resources found that the interaction contrasting CBT and HE remained significant for ABS-depressive affect (F(1,131) = 12.41, p < .001), IES-I (F(1,131) = 8.06, p = .005), and FACT-EWB (F(1,131) =9.64, p = .002). Similarly, adding a control for change in MOCS-relaxation found that the same interactions remained significant: for ABS-depressive affect (F(1,131) = 7.23, p = .008), IES-I (F(1,131) = 7.43, p = .007), and FACT-EWB (F(1,131) = 4.71, p = .032). These subsidiary analyses indicated that a mediational relationship here is implausible. However, interaction contrasts also showed that when controlling for change in MOCS-relaxation from T1 to T2, differences over time between RT and HE were no longer significant for either ABS-depressive affect (F(1,131) = 0.81, p = .369) or SIP-SI (F(1,131) = 0.68, p = .412). This pattern suggests mediation in this case may be plausible.
Discussion
Group-based CBSM is beneficial during active treatment for women with non-metastatic BCa (e.g., Antoni et al., 2006b). However, less is known about which components of CBSM are responsible for its effects on psychological adaptation. The current RCT tested two components of CBSM by dismantling the intervention into two active 5-week treatment groups (i.e., CBT and RT) and comparing them to an attention-matched Health Education control condition (HE). Both CBT and RT groups significantly improved on primary indicators of adaptation, as well as hypothesized intervention-targeted stress management factors from pre-to post-intervention, while the HE group did not change. These findings control for theoretically and empirically-based medical covariates. Overall, average effect sizes from the current study were medium (d = 0.57–0.78) and would be considered clinically meaningful (Hayes & Woolley, 2000).
This study is the first to our knowledge to compare two active components of an evidence-based psychosocial intervention to each other and to an attention-matched control condition in a sample of BCa patients undergoing active treatment. A somewhat comparable study was conducted by Cohen and Fried (2007), who compared a 9-session 90-minute cognitive-behavioral group with a 9-session relaxation/guided imagery group in women with BCa who were 2–12 months post-surgery. However, the two active intervention groups were compared to a wait-list control group, which does not account for potential beneficial effects of group support and therapist attention on these outcomes.
We must note explicitly, however, that the study reported here suffered from a failure of random assignment to equate the groups on their initial levels of some aspects of well-being. Specifically, the HE control group had better initial levels on three of the adjustment measures: depressive affect, thought intrusion, and social disruption. Because of this, there is ambiguity about whether the differential improvement of the treatment groups compared to the HE group on these measures represents true benefits of the treatment as opposed to regression to the mean or a natural course of improvement in well-being over time in the CBT and RT groups. As levels of distress in the HE group were relatively low at baseline, there may not have been as much room for improvement as there were in the treatment condition groups. However, natural improvement in well-being is unlikely in the current study given the brief time-frame (approximately 2 months from T1 to T2) and the fact that women were moving from a non-intensive period of treatment at T1 prior to beginning adjuvant treatment to a more intensive period at T2 in the midst of active adjuvant treatment. Subsidiary analyses using an archival data set suggested that the anomalous levels occurred in the control group, but those analyses can only be considered suggestive.
Psychological Adaptation
Distress and emotional well-being
The finding that both 5-week intervention groups had reduced depressive affect compared to the HE control fits with previous findings of longer group-based CBSM effects on depressive symptoms (Antoni et al., 2001; Antoni et al., 2006b) as well as reductions in total mood disturbance achieved with other group-based cognitive-behavioral interventions (Andersen et al., 2004; Fukui et al., 2000). Improvement in the FACT emotional well-being scale for women in the CBT group is also very much in line with previous studies (e.g., Dirksen & Epstein, 2008), systematic reviews (e.g., Jassim, Whitford, & Grey, 2010), and meta-analyses (e.g., Tatrow & Montgomery, 2006) of psychosocial and cognitive-behavioral interventions for BCa, which were based largely on longer interventions. Women in the CBT group, but not the RT group, also had significant reductions in cancer-related thought intrusions. This finding is consistent with a previous trial, which found that a 10-week CBSM intervention reduced thought intrusion (Antoni et al., 2006b). Another trial of a shortened (5 weeks, 3-hour sessions) CBSM intervention did not find significant effects on cancer-specific distress (Groarke et al., 2013). The fact that thought intrusions were improved in the CBT but not the RT condition here suggests that CBT techniques may be more valuable for targeting this aspect of psychological adaptation to BCa.
Social disruption
Interestingly, only the RT group showed significant improvement in social disruption. This is consistent with the previous finding that a 10-week CBSM group reduced disruption of social interactions (Antoni et al., 2006a), but it adds to this previous finding by differentiating between effects of relaxation and cognitive techniques. Few studies have investigated how psychosocial interventions can lessen illness-related social withdrawal reported by women undergoing primary BCa treatment (Carver et al., 2003). The current result suggests that some aspect of relaxation may help mobilize women to rejoin their social activities.
Stress Management Resources
Interpersonal resources
The CBT group reported feeling more assured that they could count on social support networks in times of stress, one of the main targets of that intervention (Antoni, 2003). One CBT module teaches anger management skills, helping to prevent the erosion of social support, a phenomenon previously documented during cancer treatment (Dukes Holland & Holahan, 2003). Another module focuses assertiveness in approaching support sources and expressing emotions, which has been previously found to increase perceived social support from family (Andersen et al., 2004). Thus, this study is among the few to focus on teaching interpersonal strategies to enhance BCa patients’ perceived social support.
Despite work indicating that social support plays an important role in explaining CBSM intervention effects on mood among HIV-infected individuals (Lutgendorf et al., 1998), the present findings do not support this mediation in women with BCa; controlling for changes in reliable social support (as indicated by increases in SPS-RA) did not affect differences between the CBT and HE groups in ABS-depressive affect or FACT-EWB. However, it is possible that social support changes may have an impact over a longer period of follow-up. Also, other mediators may be driving the observed group differences, especially over the short term. For example, the CBT modules uniquely focused on interpersonal skills and assertiveness as well as cognitive restructuring skills, and these skills were not addressed in the HE group. It is possible that improvements in these domains may mediate the observed group differences (Antoni, Carver, & Lechner, 2009). Without validated measures of these constructs, these potential mediators cannot be fully explored in the present study. Future studies may benefit from considering such potential mediators and including measures of constructs like irrational beliefs, such as the Shortened General Attitude and Belief Scale, which assesses various dimensions of irrationality such as need for comfort and demand for fairness (Lindner, Kirkby, Wertheim, & Birch, 1999).
Perceived relaxation skills
As hypothesized, we found that women in the RT group reported increased confidence in their ability to engage in relaxation skills, the main target of the RT intervention. Findings are similar to other studies showing that longer stress management interventions can improve confidence in the ability to relax (Andersen, Shelby, & Golden-Kreutz, 2007). This study adds to this literature by demonstrating that briefer (i.e., 5-week) interventions can produce similar results in increasing perceived relaxation skills (Phillips et al., 2012).
Previous work found that confidence in one’s ability to engage relaxation skills (i.e., perceived relaxation skills on the MOCS) mediated the effect of a broader intervention on illness-related disruption of social and interpersonal interactions (Antoni et al., 2006a). The current study provides additional suggestive support for this relationship in showing parallel improvements in relaxation confidence and reductions in social disruption in the RT condition. However, since these changes were measured over the same period in the present study, mediation effects could not be tested here. Taken together these findings suggest that both basic elements of a 10-week group-based CBSM intervention—RT and CBT—when parsed into 5-week formats, can improve adaptation during primary treatment for non-metastatic BCa. The specific change processes underlying each of these interventions require further exploration.
Strengths and Limitations
Strengths
Analyses were conducted with an intention-to-treat method and an adequate sample size, with sufficient power to detect medium-sized effects. The study addresses a gap in the literature by focusing on the distinct elements of the manualized CBSM to examine how stress management interventions influence psychological adaptation (Stanton et al., 2013). It is one of very few studies examining the effects of a brief psychosocial intervention in BCa (Fukui et al., 2000, Groarke et al., 2013). The use of an attention-matched control is an improvement in study design over previous CBT research in BCa, by keeping the non-specific effects of group support on psychosocial well-being constant across all conditions.
Most BCa intervention studies have enrolled predominantly white middle class women, which is problematic since minority women experience poorer QOL (Giedzinska, Meyerowitz, Ganz, & Rowland, 2004). In the current sample, 57% were of an ethnic minority, which allows for greater generalizability of the findings. Additionally, participants were enrolled in the study 2–10 weeks post-surgery, a time when women struggle with anticipatory anxiety about adjuvant treatment and side effects from surgical recovery (Spencer et al., 1999). Intervening at this point in treatment may capitalize on a “window of opportunity” for teaching stress management skills that may be useful throughout survivorship.
Limitations
As is true of most psychological intervention trials conducted in university settings, many eligible women declined to participate in the study and the sample is composed of women who are motivated to participate in research. They may not reflect the clinical settings where these types of interventions might ultimately be delivered. Future studies should seek to address potential barriers to participation, such as transportation limitations and lack of fluency in English. There was no entry criterion of a minimal level of cancer-related distress in this study. Given the focus on stress management, it is plausible that effects would have been larger in a more distressed sample, and future work should target this population using cancer distress screening measures (Carlson & Bultz, 2004). These factors together may limit generalizability of the findings.
Although the study did enroll a large proportion of Hispanic women, it should be noted that English fluency was an inclusion criterion. Future work could translate measures and study materials in ways that are culturally appropriate to enable inclusion of non-English speaking women. The sample also included only a small number of African-American women. Future work should target African-American populations, given known disparities in cancer morbidity (Siegel, Naishadham, & Jemal, 2012). Additionally, while women with metastatic BCa were excluded to increase group homogeneity, this exclusion may further limit generalizability of the present findings.
Given that all measures were self-report, there is the potential for self-report bias. Study conditions were similar on nearly all sociodemographic and medical characteristics. However, we did find baseline differences on income, and there is the previously mentioned failure of random assignment to equate the study groups at baseline. This creates an ambiguity concerning the meaning of the results that cannot be entirely discounted.
Clinical Relevance
Despite limitations, the current findings add to literature indicating that group-based stress-reducing interventions may be efficacious for women with non-metastatic BCa. However, some of the methodological limitations in the present study temper any firm conclusions. Patients who have greater confidence in stress management skills prior to chemotherapy have less negative mood and better QOL (Faul, Jim, Williams, Loftus, & Jacobsen, 2010). Others have suggested that psychological therapy should be considered part of the “adjuvant” treatment plan alongside chemotherapy or radiation therapy (Cunningham, 2000). The present study suggests that a brief (5 weeks of 90 minutes per week) psychosocial intervention could be of help, especially during the early period of adjuvant treatment. Follow-up studies are needed to determine whether intervention effects are sustained in the long-term. A follow-up of the current cohort of breast cancer patients is in progress. Given the positive effect of both CBT and RT interventions on primary indicators of adaptation as well as the unique contributions of CBT and RT intervention components, the combination of these two brief interventions in the form of Cognitive-Behavioral Stress Management may be recommended. Present findings suggest that 5 weeks of any combination of CBT and RT components could be used, confirming prior observations that women attending 5 of 10 CBSM sessions showed comparable results to those attending a greater number of sessions. The interventions were implemented by Master’s level graduate students in clinical psychology, under the supervision of licensed psychologists. While psychiatrists and psychologists should continue to be called on for treatment of more serious psychological problems, allied healthcare professionals such as advanced oncology nurses and social workers could be trained to deliver these brief, manualized psychosocial interventions to target general distress. Thus, this work joins other efforts to develop effective strategies that can be employed with the limited time and resources in oncology settings (Stanton et al., 2013).
Table 2.
Descriptive Data for Study Dependent Variables by Group
| Tl |
T2 |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT | RT | HE | CBT | RT | HE | ||||||||
| Dependent Variable |
Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| ABS-dep | M | 1.96 | 1.97 | 1.96 | 1.95 | 1.67 | 1.67 | 1.66 | 1.69 | 1.80 | 1.76 | 1.71 | 1.72 |
| SD | 0.61 | 0.65 | 0.65 | 0.60 | 0.65 | 0.64 | 0.48 | 0.64 | 0.63 | 0.61 | 0.63 | 0.60 | |
| IES-I | M | 1.63 | 1.64 | 1.15 | 1.15 | 1.09 | 1.07 | 1.08 | 1.07 | 1.07 | 1.11 | 0.93 | 0.92 |
| SD | 0.81 | 0.82 | 0.73 | 0.77 | 0.90 | 0.82 | 0.77 | 0.91 | 0.84 | 0.86 | 0.83 | 0.84 | |
| SIP-SI | M | 880.20 | 880.94 | 929.45 | 930.35 | 818.84 | 818.71 | 879.95 | 883.21 | 860.90 | 860.58 | 826.04 | 823.65 |
| SD | 138.26 | 161.61 | 204.58 | 149.15 | 113.24 | 164.85 | 184.95 | 173.39 | 161.22 | 158.38 | 118.68 | 158.16 | |
| FACT- EWB |
M | 2.97 | 2.97 | 2.97 | 2.91 | 3.26 | 3.31 | 3.37 | 3.35 | 3.11 | 3.09 | 3.37 | 3.39 |
| SD | 0.85 | 0.72 | 0.76 | 0.68 | 0.66 | 0.72 | 0.49 | 0.69 | 0.79 | 0.66 | 0.55 | 0.64 | |
| SPS-RA | M | 1.08 | 1.08 | 1.17 | 1.16 | 1.10 | 1.12 | 1.19 | 1.20 | 1.11 | 1.09 | 1.05 | 1.07 |
| SD | 0.23 | 0.27 | 0.34 | 0.26 | 0.24 | 0.27 | 0.32 | 0.26 | 0.25 | 0.25 | 0.15 | 0.24 | |
| MOCS- relax |
M | 1.32 | 1.34 | 1.62 | 1.58 | 1.87 | 1.89 | 1.71 | 1.73 | 2.45 | 2.47 | 1.86 | 1.86 |
| SD | 0.98 | 1.06 | 1.15 | 0.97 | 1.00 | 1.07 | 1.02 | 1.19 | 0.90 | 1.09 | 1.21 | 1.07 | |
Note: Adjusted means are adjusted for the following covariates: Disease stage, time since surgery, and baseline income.
Public Health Significance.
The present study suggests that brief stress management group interventions may be helpful in promoting stress management skills and improving psychological adaptation among women with non-metastatic breast cancer, especially during the early period of adjuvant treatment. These brief stress management interventions may be easier to incorporate into clinical settings than previously validated longer interventions and may therefore be able to be offered to a broader population.
Acknowledgments
This study was funded by the National Cancer Institute of the National Institutes of Health 2R01-CA-064710, the Sylvester Comprehensive Cancer Center, and the Non-Therapeutic Research Support Core of the Sylvester Comprehensive Cancer Center
Footnotes
In an effort to assess which of these conditions is atypical, we compared these baselines against an archival data set (Antoni et al., 2006b), in which two of the same measures had been collected at baseline. The HE baseline on depressive affect proved to be significantly lower than the archival mean (1.97, SD = 0.64), which did not differ from the CBT or RT baselines. The HE baseline on SIP-SI was also lower than the archival mean, which did not differ from the CBT or RT baselines. The IES in the form used here was not included in the earlier sample.
References
- American Cancer Society. Learn about breast cancer. 2006 Retrieved from http://www.cancer.org/cancer/breastcancer/
- Andersen B, Farrar W, Golden-Kreutz D, Emery C, Glaser R, Crespin T, Carson III W. Distress reduction from a psychological intervention contributes to improved health for cancer patients. Brain Behav Immun. 2007;21(7):953–961. doi: 10.1016/j.bbi.2007.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen B, Farrar W, Golden-Kreutz D, Glaser R, Emery C, Crespin T, Carson W., 3rd Psychological, behavioral, and immune changes after a psychological intervention: A clinical trial. J Clin Oncol. 2004;22(17):3570–3580. doi: 10.1200/JCO.2004.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen B, Shelby R, Golden-Kreutz D. RCT of a psychological intervention for patients with cancer: I. mechanisms of change. J Consult Clin Psych. 2007;75(6):927. doi: 10.1037/0022-006X.75.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoni M. Stress management intervention for women with breast cancer. Washington, DC US: American Psychological Association; 2003. [Google Scholar]
- Antoni M, Carver C, Lechner S. Enhancing positive adaptation: Example intervention during treatment for breast cancer. In: Park CL, Lechner SC, Antoni MH, Stanton AL, editors. Medical illness and positive life change: Can crisis lead to personal transformation? Washington, DC: American Psychological Association; 2009. pp. 197–214. [Google Scholar]
- Antoni M, Lechner S, Kazi A, Wimberly S, Sifre T, Urcuyo K, Carver C. How stress management improves quality of life after treatment for breast cancer. J Consult Clin Psych. 2006(a);74(6):1143–1152. doi: 10.1037/0022-006X.74.6.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoni M, Lehman J, Kilbourn K, Boyers A, Culver J, Alferi S, Carver C. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol. 2001;20(1):20. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- Antoni M, Wimberly S, Lechner S, Kazi A, Sifre T, Urcuyo K, Carver C. Reduction of cancer-specific thought intrusions and anxiety symptoms with a stress management intervention among women undergoing treatment for breast cancer. Am J Psychiat. 2006(b);163(10):1791–1797. doi: 10.1176/ajp.2006.163.10.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A, Emery G. Anxiety disorders and phobias: A cognitive perspective. New York: Basic Books; 1985. [Google Scholar]
- Bergner M, Bobbitt R, Carter W, Gilson B. The Sickness Impact Profile: Development and final revision of a health status measure. Medical Care. 1981;19:787–806. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- Bernstein B, Borkovec T. Progressive muscle relaxation training: A manual for the helping professions. Champaign, IL: Research Press; 1973. [Google Scholar]
- Brady M, Cella D, Mo F, Bonomi A, Tulsky D, Lloyd S, Shiomoto G. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol. 1997;15(3):974–986. doi: 10.1200/JCO.1997.15.3.974. [DOI] [PubMed] [Google Scholar]
- Carlson L, Angen M, Cullum J, Goodey E, Koopmans J, Lamont L, Bultz B. High levels of untreated distress and fatigue in cancer patients. Brit J Cancer. 2004;90(12):2297–2304. doi: 10.1038/sj.bjc.6601887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson L, Bultz B. Efficacy and medical cost offset of psychosocial interventions in cancer care: making the case for economic analyses. Psycho-Oncol. 2004;13(12):837–849. doi: 10.1002/pon.832. [DOI] [PubMed] [Google Scholar]
- Carver C. Measure of Current Status. 2006 Retrieved January 17, 2014, from Department of Psychology, University of Miami Web site: http://www.psy.miami.edu/faculty/ccarver/
- Carver C, Lehman J, Antoni M. Dispositional pessimism predicts illness-related disruption of social and recreational activities among breast cancer patients. J Pers Soc Psychol. 2003;84(4):813. doi: 10.1037/0022-3514.84.4.813. [DOI] [PubMed] [Google Scholar]
- Cella D, Tulsky D, Gray G, Sarafian B, Lloyd S, Linn E, Brannon J. The Functional Assessment of Cancer Therapy (FACT) Scale: Development and validation of the general measure. J Clin Oncol. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. NY: Academic Press; 1988. [Google Scholar]
- Cohen M, Fried G. Comparing relaxation training and cognitive-behavioral group therapy for women with breast cancer. Res Soc Work Prac. 2007;17(3):313–323. [Google Scholar]
- Coyne J, Lepore S, Palmer S. Efficacy of psychosocial interventions in cancer care: Evidence is weaker than it first looks. Ann Behav Med. 2006;32:104–110. doi: 10.1207/s15324796abm3202_5. [DOI] [PubMed] [Google Scholar]
- Cunningham A. Adjuvant psychological therapy for cancer patients: putting it on the same footing as adjunctive medical therapies. Psycho-Oncol. 2000;9(5):367–371. doi: 10.1002/1099-1611(200009/10)9:5<367::aid-pon473>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Cutrona C, Russell D. Advances in Personal Relationships. 1 ed. Greenwich: JAI Press; 1987. The provisions of social relationships adaptation to stress; pp. 37–67. [Google Scholar]
- Derogatis L. The Affects Balance Scale. Baltimore: Clinical Psychometric Research; 1975. [Google Scholar]
- Dirksen S, Epstein D. Efficacy of an insomnia intervention on fatigue, mood and quality of life in breast cancer survivors. J Adv Nurs. 2008;61(6):664–675. doi: 10.1111/j.1365-2648.2007.04560.x. [DOI] [PubMed] [Google Scholar]
- Dukes Holland K, Holahan C. The relation of social support and coping to positive adaptation to breast cancer. Psychol Health. 2003;18(1):15–29. [Google Scholar]
- Eisen S, Ranganathan G, Seal P, Spiro A., III Measuring clinically meaningful change following mental health treatment. J Behav Health Ser R. 2007;34(3):272–289. doi: 10.1007/s11414-007-9066-2. [DOI] [PubMed] [Google Scholar]
- Faul L, Jim H, Williams C, Loftus L, Jacobsen P. Relationship of stress management skill to psychological distress and quality of life in adults with cancer. Psycho-Oncol. 2010;19(1):102–109. doi: 10.1002/pon.1547. [DOI] [PubMed] [Google Scholar]
- Fensterheim H, Baer J. Don’t say yes when you want to say no. New York: McKay; 1975. [Google Scholar]
- Fors E, Bertheussen G, Thune I, Juvet L, Elvsaas I, Oldervoll L, Leivseth G. Psychosocial interventions as part of breast cancer rehabilitation programs? Results from a systematic review. Psycho-Oncol. 2011;20(9):909–918. doi: 10.1002/pon.1844. [DOI] [PubMed] [Google Scholar]
- Fukui S, Kugaya A, Okamura H, Kamiya M, Koike M, Nakanishi T, Uchitomi Y. A psychosocial group intervention for Japanese women with primary breast carcinoma. Cancer. 2000;89(5):1026–1036. doi: 10.1002/1097-0142(20000901)89:5<1026::aid-cncr12>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- Giedzinska A, Meyerowitz B, Ganz P, Rowland J. Health-related quality of life in a multiethnic sample of breast cancer survivors. Ann Behav Med. 2004;28(1):39–51. doi: 10.1207/s15324796abm2801_6. [DOI] [PubMed] [Google Scholar]
- Golden-Kreutz D, Thornton L, Wells-Di Gregorio S, Frierson G, Jim H, Carpenter K, Andersen B. Traumatic stress, perceived global stress, and life events: Prospectively predicting quality of life in breast cancer patients. Health Psychol. 2005;24(3):288. doi: 10.1037/0278-6133.24.3.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groarke A, Curtis R, Kerin M. Cognitive-behavioural stress management enhances adjustment in women with breast cancer. Brit J Health Psych. 2013;18(3):623–641. doi: 10.1111/bjhp.12009. [DOI] [PubMed] [Google Scholar]
- Hays R, Woolley J. The concept of clinically meaningful difference in health-related quality-of-life research. Pharmacoeconomics. 2000;18(5):419–423. doi: 10.2165/00019053-200018050-00001. [DOI] [PubMed] [Google Scholar]
- Herschbach P, Keller M, Knight L, Brandl T, Huber B, Henrich G, Marten-Mittag B. Psychological problems of cancer patients: A cancer distress screening with a cancer-specific questionnaire. Brit J Cancer. 2004;91(3):504–511. doi: 10.1038/sj.bjc.6601986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen P, Jim H. Psychosocial interventions for anxiety and depression in adult cancer patients: Achievements and challenges. CA: A Cancer Journal for Clinicians. 2008;58(4):214–230. doi: 10.3322/CA.2008.0003. [DOI] [PubMed] [Google Scholar]
- Jassim G, Whitford D, Grey I. Psychological interventions for women with non-metastatic breast cancer. The Cochrane Library. 2010 [Google Scholar]
- Kline R. Principles and practice of structural equation modeling. 3rd ed. New York, NY: The Guilford Press; 2011. [Google Scholar]
- Lindner H, Kirkby R, Wertheim E, Birch P. A brief assessment of irrational thinking: The Shortened General Attitude and Belief Scale. Cognitive Ther Res. 1999;23:651–663. [Google Scholar]
- Lutgendorf S, Antoni M, Ironson G, Starr K, Costello N, Zuckerman M, Schneiderman N. Changes in cognitive coping skills and social support during cognitive behavioral stress management intervention and distress outcomes in symptomatic human immunodeficiency virus (HlV)-seropositive gay men. Psychosom Med. 1998;60(2):204–214. doi: 10.1097/00006842-199803000-00017. [DOI] [PubMed] [Google Scholar]
- Montazeri A. Health-related quality of life in breast cancer patients: A bibliographic review of the literature from 1974 to 2007. J Exp Clin Canc Res. 2008;27(1):32. doi: 10.1186/1756-9966-27-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips K, Jim H, Small B, Tanvetyanon T, Roberts W, Jacobsen P. Effects of self-directed stress management training and home-based exercise on stress management skills in cancer patients receiving chemotherapy. Stress and Health. 2012;28(5):368–375. doi: 10.1002/smi.2450. [DOI] [PubMed] [Google Scholar]
- Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: Meta analysis of 37 published controlled outcome studies. Patient Educ Couns. 2003;50(2):179–186. doi: 10.1016/s0738-3991(02)00149-0. [DOI] [PubMed] [Google Scholar]
- Reich M, Lesur A, Perdrizet-Chevallier C. Depression, quality of life and breast cancer: A review of the literature. Breast Cancer Res TR. 2008;110(1):9–17. doi: 10.1007/s10549-007-9706-5. [DOI] [PubMed] [Google Scholar]
- Schnur J, David D, Kangas M, Green S, Bovbjerg D, Montgomery G. A Randomized trial of a cognitive-behavioral therapy and hypnosis intervention on positive and negative affect during breast cancer radiotherapy. J Clin Psychol. 2009;65(4):443–455. doi: 10.1002/jclp.20559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: A Cancer Journal for Clinicians. 2012;62(1):10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- Spencer S, Lehman J, Wynings C, Arena P, Carver C, Antoni M, Love N. Concerns about breast cancer and relations to psychosocial well-being in a multiethnic sample of early-stage patients. Health Psychol. 1999;18(2):159–168. doi: 10.1037//0278-6133.18.2.159. [DOI] [PubMed] [Google Scholar]
- Stanton A, Luecken L, MacKinnon D, Thompson E. Mechanisms in psychosocial interventions for adults living with cancer: Opportunity for integration of theory, research, and practice. J Consult Clin Psych. 2013;81(2):318. doi: 10.1037/a0028833. [DOI] [PubMed] [Google Scholar]
- Tatrow K, Montgomery G. Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: A meta-analysis. J Behav Med. 2006;29(1):17–27. doi: 10.1007/s10865-005-9036-1. [DOI] [PubMed] [Google Scholar]
- Weiss D. The impact of event scale: Revised. Cross-cultural assessment of psychological trauma and PTSD. 2007 Springer:219–238. [Google Scholar]
- Wilcox R. Some results on a winsorized correlation-coefficient. Brit J Math Stat Psy. 1993;46:339–349. [Google Scholar]