Abstract
Introduction
Limited data describe the frequency, timing, or indications for endotracheal intubation (ETI) in patients with status epilepticus. A better understanding of the characteristics of patients with status epilepticus requiring airway interventions could inform clinical care. We sought to characterize ETI use in patients with prehospital status epilepticus.
Methods
This study was a secondary analysis of the Rapid Anticonvulsant Medication Prior to Arrival Trial, a multi-center, randomized trial comparing intravenous lorazepam to intramuscular midazolam for prehospital status epilepticus treatment. Subjects received ETI in the prehospital, Emergency Department (ED), or inpatient setting at the discretion of caregivers.
Results
Of 1023 enrollments, 218 (21 %) received ETI. 204 (93.6 %) of the ETIs were performed in the hospital and 14 (6.4 %) in the prehospital setting. Intubated patients were older (52 vs 41 years, p < 0.001), and men underwent ETI more than women (26 vs 21 %, p = 0.047). Patients with ongoing seizures on ED arrival had a higher rate of ETI (32 vs 16 %, p < 0.001), as did those who received rescue anti-seizure medication (29 vs 20 %, p = 0.004). Mortality was higher for intubated patients (7 vs 0.4 %, p < 0.001). Most ETI (n = 133, 62 %) occurred early (prior to or within 30 min after ED arrival), and late ETI was associated with higher mortality (14 vs 3 %, p = 0.002) than early ETI.
Conclusions
ETI is common in patients with status epilepticus, particularly among the elderly or those with refractory seizures. Any ETI and late ETI are both associated with higher mortality.
Keywords: Status epilepticus, Seizures, Endotracheal intubation, Airway management, Respiratory insufficiency, Emergency medical services
Introduction
Status epilepticus is a neurological emergency with approximately 200,000 cases in the United States each year and a mortality of 9–27 % [1, 2]. Respiratory failure is an important complication of status epilepticus [3, 4]. It is usually a consequence of the seizure or an effect of the medications used to treat the seizure.
Patients with respiratory failure may benefit from endotracheal intubation and mechanical ventilation [5–7]. However, the role and benefit of endotracheal intubation to prevent hypoventilation or pulmonary aspiration in status epilepticus is unclear because many patients who are poorly responsive after a seizure will recover quickly without airway and ventilator support. In such patients, endotracheal intubation may pose unnecessary risks and mask clinical signs of recurrent seizure. Previous multicenter studies showed that approximately 15–18 % of patients with status epilepticus received endotracheal intubation [1, 8]. The best practices for airway management in patients with status epilepticus are unclear, and there are few evidence-based guidelines for airway management in status epilepticus [4].
Greater understanding of characteristics and clinical course of status epilepticus patients receiving ETI could inform the care of these patients. We sought to characterize the use of prehospital and hospital ETI in patients with prehospital status epilepticus and compared those patients receiving ETI prior to or within 30 min of emergency department (ED) arrival to those receiving later ETI.
Materials and Methods
Study Setting and Design
This study was a secondary analysis of the Rapid Anticonvulsant Medication Prior to Arrival Trial (RAMPART) [9]. RAMPART was the first study completed by the Neurological Emergencies Treatment Trials (NETT) network. The NETT is a National Institute of Neurological Disorders and Stroke funded clinical research network conducting studies on neurological emergencies that is organized in a hubspoke model with 17 hub sites, each of which has many associated spoke hospitals. RAMPART was conducted by the NETT through 33 emergency medical services (EMS) agencies and 79 receiving hospitals nationwide.
RAMPART was a randomized, double-blind, non-inferiority clinical trial which compared the use of intravenous lorazepam to intramuscular midazolam for the treatment of prehospital status epilepticus [9]. The trial met the requirements for exception from informed consent for emergency research under the 21 CFR §50.24 and was approved by each site's institutional review board. Study teams obtained written informed consent from a subject or legally authorized representative following enrollment to allow continued data collection until completion of follow-up.
Study Subjects
The RAMPART trial included adults and children with an estimated weight of 13 kg or more who required treatment with benzodiazepines for prehospital status epilepticus. Status epilepticus was defined as continuous, convulsive seizures for longer than 5 min or convulsive seizures at the time of treatment after having intermittent seizures without regaining consciousness for longer than 5 min. Exclusion criteria included seizure due to major trauma, hypoglycemia, cardiac arrest, a heart rate less than 40 beats per minute, known allergy to midazolam or lorazepam, pregnancy, prisoners, being enrolled in another study, or wearing a RAMPART declined bracelet.
Study Outcomes
The primary outcome for this analysis was endotracheal intubation. Endotracheal intubation was defined as attempted placement of a definitive tracheal airway (orotracheal, nasotracheal, cricothyroidotomy, or tracheostomy) for support of respirations or protection of airway. The use of a non-definitive and/or non-tracheal airway (oral or nasal airways, laryngeal mask airways, or esophageal obturator airways) was not included unless specifically deemed to have been used in lieu of tracheal intubation. Intubations performed to facilitate surgical interventions were not included. Optimal airway management and the decision to perform endotracheal intubation were left to the treating clinicians. The circumstances surrounding intubation were requested through an adverse event narrative. The predefined indications included respiratory depression and depressed mental status with or without persistent convulsions. Any intubations that described subjective or objective issues with oxygenation or ventilation in the narrative were categorized as respiratory depression. Any intubations that did not include oxygenation or ventilation issues but instead described airway protection, CNS depression, ongoing seizures, or prolonged postictal unresponsiveness were categorized as depressed mental status. Secondary outcomes included timing of endotracheal intubation, mortality, and hospital length of stay. Early endotracheal intubation was defined as intubation prior to arrival or within 30 min after arrival to the ED.
Covariates
Clinical covariates included subjects’ demographics and clinical characteristics such as seizure etiology, need for rescue therapy or high dose treatment, ongoing or recurrent seizures on ED arrival, and reasons for endotracheal intubation. Seizure etiology and the primary reason for intubation were determined by investigators at each enrolling hospital. Rescue therapy was defined as the prehospital administration of rescue medications according to local EMS protocol if the subject was still convulsing 10 min after the last study medication was administered. It did not include additional anticonvulsant medications given in the ED. High dose treatment was administered to children whose estimated body weight was above 40 kg and to all adults and treatment consisted of either 10 mg of intramuscular midazolam or 4 mg of intravenous lorazepam. The low-dose tier included children whose estimated body weight was 13–40 kg and treatment consisted of either 5 mg of intramuscular midazolam or 2 mg of intravenous lorazepam. The primary RAMPART outcome was cessation of status epilepticus upon ED arrival as defined by not having seizures on arrival in the ED and not receiving rescue medications before arrival.
Data Analysis
Univariate analyses compared baseline characteristics and clinical outcomes between intubated and non-intubated groups and early and late intubated groups. Using logistic regression including a random effect to account for repeated intubations within enrollments, we developed two multivariate models to assess the independent association of patient characteristics with the outcomes (1) endotracheal intubation and (2) early intubation. For this, we first considered a full model including all variables preceding outcome and achieving statistical significance (p < 0.05) in univariate models. Then, the least significant variable was removed and the reduced model successively re-fit until all effects were statistically significant at p < 0.05. We also examined variability in intubation rates across NETT hubs using funnel plots, which compared the sitespecific intubation rates to the 95 and 99 % confidence intervals for the overall intubation rate [10]. All analyses were conducted using SAS software (Cary, NC).
Results
There were 1023 RAMPART enrollments encompassing 893 individual subjects. There were 218 (21.3 %) endotracheal intubations among 213 (23.9 %) unique subjects. Of the 218 intubations, 204 (93.6 %) were performed in the hospital and 14 (6.4 %) were performed in the prehospital setting (Fig. 1). There were no cricothyroidectomies performed. The most common primary reasons reported for intubation were respiratory depression (39 %), depressed mental status with or without persistent convulsions (36 %), and recurrent convulsions after initial termination (16 %). The proportion of patients thought to be actively seizing at the time of intubation was 28 %. Duration of intubation ranged from 2 h to 47 days, with a median of 39 h. Forty-two percent were intubated for fewer than 24 h, and 11 % for fewer than 12 h.
Fig. 1.
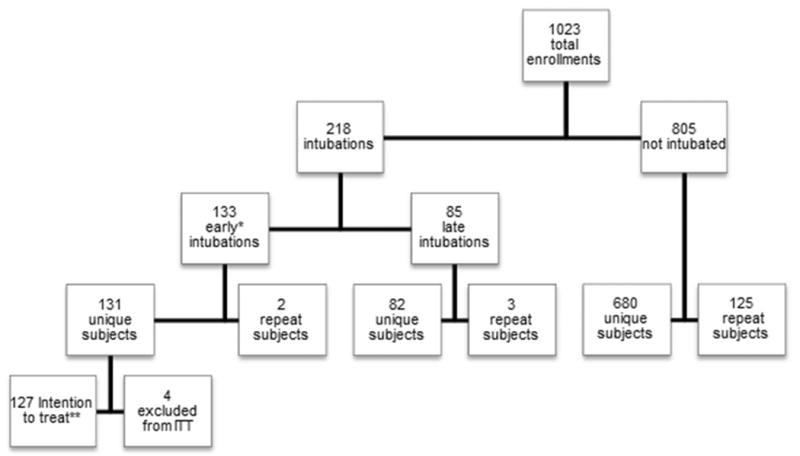
Subjects and enrollments. *Early intubations were performed prior to ED arrival or within 30 min of ED arrival. 14 of the 133 early intubations were prehospital. **Intention to treat includes unique subjects without key eligibility violations
Overall, 893 subjects were included in the intention to treat analysis in RAMPART. There were 63 (14.1 %) intubated in the midazolam group and 64 (14.4 %) intubated in the lorazepam group within 30 min of arrival to the ED [9]. The rate of intubation between these two groups was similar.
Endotracheal intubation was less common among younger patients (<50 years, 14.9 %, vs ≥50 years, 35.5 %, p < .0001; Fig. 2). Women were less likely to be intubated than men (Table 1). Intubation was rare among those ultimately diagnosed with a non-epileptic spell.
Fig. 2. Age distribution of intubated patients.
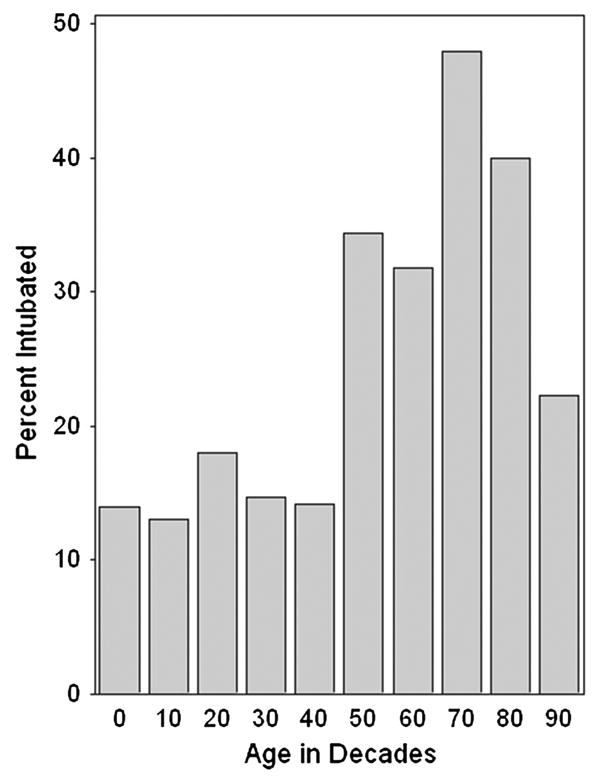
Table 1. Demographics of intubated and not intubated subjects.
| Demographics by subject | No. of subjects | Not intubated (n = 680) | Intubated (n = 213) | p value |
|---|---|---|---|---|
| Age (years) | 893 | 40.88 (21.57) | 51.54 (21.11) | <0.001 |
| Gender | 893 | 0.047 | ||
| Female | 405 | 321 (79.26) | 84 (20.74) | |
| Race | 893 | 0.990 | ||
| Black/African American | 453 | 344 (75.94) | 109 (24.06) | |
| White | 348 | 266 (76.44) | 82 (23.56) | |
| Other | 56 | 43 (76.78) | 13 (23.21) | |
| Unknown/not reported | 36 | 27 (75.00) | 9 (25.00) | |
| Ethnicity | 893 | 0.859 | ||
| Hispanic or Latino | 106 | 80 (75.47) | 26 (24.53) | |
| Not Hispanic or Latino | 599 | 454 (75.79) | 145 (24.21) | |
| Unknown/not reported | 188 | 146 (77.66) | 42 (22.34) |
Those with a prior history of seizures and those with anticonvulsant withdrawal or non-compliance as the etiology of status epilepticus had lower rates of intubation. Those with febrile seizure or idiopathic or breakthrough status epilepticus also showed lower rates of intubation, although the differences were not statistically significant. Patients were more likely to be intubated if their status epilepticus was caused by toxic or metabolic etiologies or by a central nervous system tumor or stroke.
Patients with active seizures on ED arrival were twice as likely to be intubated as those with cessation of seizures. Intubation was also more common in those enrollments in which rescue benzodiazepine medications were given prior to ED arrival (28.8 vs 19.5 %) (Table 2).
Table 2. Clinical characteristics and outcomes of intubated and not intubated enrollments.
| Clinical characteristics by enrollment | No. of enrollments | Not intubated (n = 805) | Intubated (n = 218) | p value |
|---|---|---|---|---|
| Diagnosis at discharge | 1,023 | 805 | 218 | <0.001 |
| Seizure/status epilepticus | 910 | 699 (76.81) | 211 (23.19) | |
| Non-epileptic spell | 83 | 81 (97.59) | 2 (2.41) | |
| Cause unknown | 30 | 25 (83.33) | 5 (16.67) | |
| Prior history | 909 | 698 | 211 | <0.001 |
| No | 215 | 146 (67.91) | 69 (32.09) | |
| Etiology | 903 | 693 | 210 | |
| Febrile seizure | 25 | 22 (88.00) | 3 (12.00) | 0.177 |
| Toxic/metabolic | 100 | 68 (68.00) | 32 (32.00) | 0.028 |
| CNS tumor/stroke | 52 | 28 (53.85) | 24 (46.15) | <0.001 |
| Idiopathic/unknown precipitant without history of seizure | 54 | 40 (74.07) | 14 (25.93) | 0.632 |
| Other identified acute precipitant | 48 | 33 (68.75) | 15 (31.25) | 0.178 |
| Anticonvulsant withdrawal/non-compliance with history of seizure | 336 | 270 (80.36) | 66 (19.64) | 0.048 |
| Idiopathic or breakthrough seizure with history of seizure | 288 | 232 (80.56) | 56 (19.44) | 0.064 |
| Non-epileptic spell | 83 | 81 | 2 | 0.027 |
| Pseudoseizure | 69 | 69 (100.00) | 0 (0.00) | |
| Seizure mimic/non-epileptic coma | 14 | 12 (85.71) | 2 (14.29) | |
| Seizure cessation upon ED arrival | 1,023 | 805 | 218 | <0.001 |
| No | 327 | 222 (67.89) | 105 (32.11) | |
| Dose | 1,023 | 805 | 218 | 0.018 |
| Low | 128 | 111 (86.72) | 17 (13.28) | |
| High | 895 | 694 (77.54) | 201 (22.46) | |
| Received rescue medications | 1,023 | 805 | 218 | 0.004 |
| No | 825 | 664 (80.48) | 161 (19.52) | |
| Yes | 198 | 141 (71.21) | 57 (28.79) | |
| Outcomes by enrollment Hospitalization | 1,015 | 798 | 217 | <0.001 |
| Yes | 612 | 401 (65.52) | 211 (34.48) | |
| ICU admission | 1,015 | 798 | 217 | <0.001 |
| Yes | 304 | 106 (34.87) | 198 (65.13) | |
| Length of stay (days) | 597 | 4.00 (4.15) | 9.67 (11.96) | <0.001 |
| Mortality | 1,023 | 805 | 218 | <0.001 |
| No | 1,004 | 802 (79.88) | 202 (20.12) | |
| Yes | 19 | 3 (15.79) | 16 (84.21) |
CNS central nervous system, ED emergency department, ICU intensive care unit
Among the 218 endotracheal intubation events, 133 (61 %) occurred early and 85 (39 %) occurred late (Fig. 3). There was no difference in baseline demographic characteristics between early and late intubated subjects (Table 3).
Fig. 3.
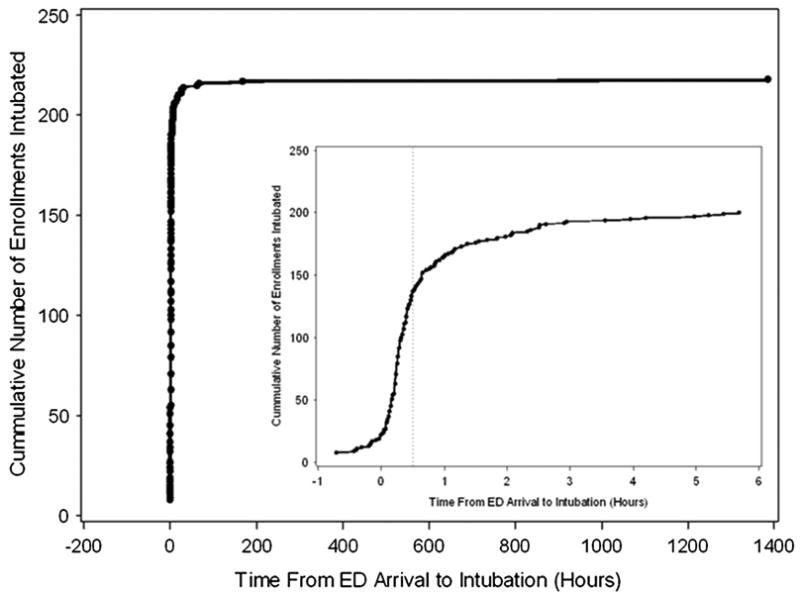
Time to intubation. Seven observations were removed for being listed as occurring in the ED, but also as having negative times from ED arrival to intubation
Table 3. Demographics of early and late intubated subjects.
| Early vs late intubations: demographics by subject | No. of subjects | Intubated early (n = 131) | Intubated late (n = 82) | p value |
|---|---|---|---|---|
| Age (years) | 213 | 52.44 (22.01) | 50.11 (19.62) | 0.435 |
| Gender | 213 | 131 | 82 | 0.179 |
| Female | 84 | 47 (55.95) | 37 (44.05) | |
| Race | 213 | 131 | 82 | 0.467 |
| Black/African American | 109 | 67 (61.47) | 42 (38.53) | |
| White | 82 | 50 (60.98) | 32 (39.02) | |
| Other | 13 | 6 (46.15) | 7 (53.85) | |
| Unknown/not reported | 9 | 8 (88.89) | 1 (11.11) | |
| Ethnicity | 213 | 131 | 82 | 0.671 |
| Hispanic or Latino | 26 | 18 (69.23) | 8 (30.77) | |
| Not Hispanic or Latino | 145 | 87 (60.00) | 58 (40.00) | |
| Unknown/not reported | 42 | 26 (61.90) | 16 (38.10) |
Mortality was higher in intubated than non-intubated patients (7 vs 0.4 %, p < .001; Table 2). Mortality was also higher in patients undergoing late intubation than in those undergoing early intubation (14 vs 3 %, p = .002; Table 4). Intubation was associated with a longer hospital length of stay (Table 2).
Table 4. Clinical characteristics and outcomes of early and late intubations by enrollment.
| Early vs late intubations: clinical characteristics by enrollment | No. of enrollments | Early intubation (n = 133) | Late intubation (n = 85) | p value |
|---|---|---|---|---|
| Diagnosis at discharge | 218 | 133 | 85 | 0.833 |
| Seizure/status epilepticus | 211 | 128 (60.66) | 83 (39.34) | |
| Non-epileptic spell | 2 | 1 (50.00) | 1 (50.00) | |
| Cause unknown | 5 | 4 (80.00) | 1 (20.00) | |
| Prior history | 211 | 128 | 83 | 0.577 |
| No | 69 | 40 (57.97) | 29 (42.03) | |
| Etiology | 210 | 127 | 83 | |
| Febrile seizure | 3 | 3 (100.00) | 0 (0.00) | 0.28 |
| Toxic/metabolic | 32 | 19 (59.38) | 13 (40.62) | 0.89 |
| CNS tumor/stroke | 24 | 7 (29.17) | 17 (70.83) | <0.001 |
| Idiopathic/unknown precipitant without history of seizure | 14 | 11 (78.57) | 3 (21.43) | 0.152 |
| Other identified acute precipitant | 15 | 10 (66.67) | 5 (33.33) | 0.611 |
| Anticonvulsant withdrawal/non-compliance with history of seizure | 66 | 39 (59.09) | 27 (40.91) | 0.781 |
| Idiopathic or breakthrough seizure with history of seizure | 56 | 38 (67.86) | 18 (32.14) | 0.187 |
| Non-epileptic spell | 2 | 1 | 1 | NA |
| Pseudoseizure | 0 | 0 (0.00) | 0 (0.00) | |
| Seizure mimic/non-epileptic coma | 2 | 1 (50.00) | 1 (50.00) | |
| Precipitating adverse event | 218 | 133 | 85 | |
| Convulsion | 35 | 12 (34.29) | 23 (65.71) | <0.001 |
| Depressed level of consciousness | 78 | 58 (74.36) | 20 (25.64) | 0.004 |
| Respiratory depression | 86 | 55 (63.95) | 31 (36.05) | 0.482 |
| Seizure cessation upon ED arrival | 218 | 133 | 85 | 0.099 |
| No | 105 | 70 (66.67) | 35 (33.33) | |
| Dose | 218 | 133 | 85 | 0.399 |
| Low | 17 | 12 (70.59) | 5 (29.41) | |
| High | 201 | 121 (60.20) | 80 (39.80) | |
| Received rescue medications | 218 | 133 | 85 | 0.009 |
| No | 161 | 90 (55.90) | 71 (44.10) | |
| Yes | 57 | 43 (75.44) | 14 (24.56) | |
| Early vs late intubations: outcomes by enrollment | ||||
| Hospitalization | 217 | 132 | 85 | 0.084 |
| Yes | 211 | 126 (59.72) | 85 (40.28) | |
| ICU admission | 217 | 132 | 85 | 0.828 |
| Yes | 198 | 120 (60.61) | 78 (39.39) | |
| Length of stay (days) | 205 | 8.55 (9.24) | 11.31 (15.01) | 0.137 |
| Mortality | 218 | 133 | 85 | 0.002 |
| No | 202 | 129 (63.86) | 73 (36.14) | |
| Yes | 16 | 4 (25.00) | 12 (75.00) | |
CNS central nervous system, ED emergency department, ICU intensive care unit
On multivariate analysis, factors independently inversely associated with endotracheal intubation included non-epileptic spell or unknown cause (odds ratio [OR], 0.20, 95 % CI 0.09–0.43) and those patients not seizing upon ED arrival (OR, 0.39; 95 % CI 0.29–0.53). Factors independently associated with early vs late intubation included patients presenting with status epilepticus caused by tumor or stroke (OR, 0.24; 95 % CI 0.09–0.61) and patients receiving rescue medications (OR, 2.73; 95 % CI 1.31–5.68).
There was variability in rates of intubation by hub, but the rates were randomly distributed about the mean without evidence of systemic bias or frequent statistical outliers (Fig. 4). Similarly, hub-specific rates of intubation without concurrent seizure by enrollments are all within the 99 % CI for the overall proportion, and only 1 hub shows greater than expected variability for intubation with concurrent seizure (Fig. 4).
Fig. 4.
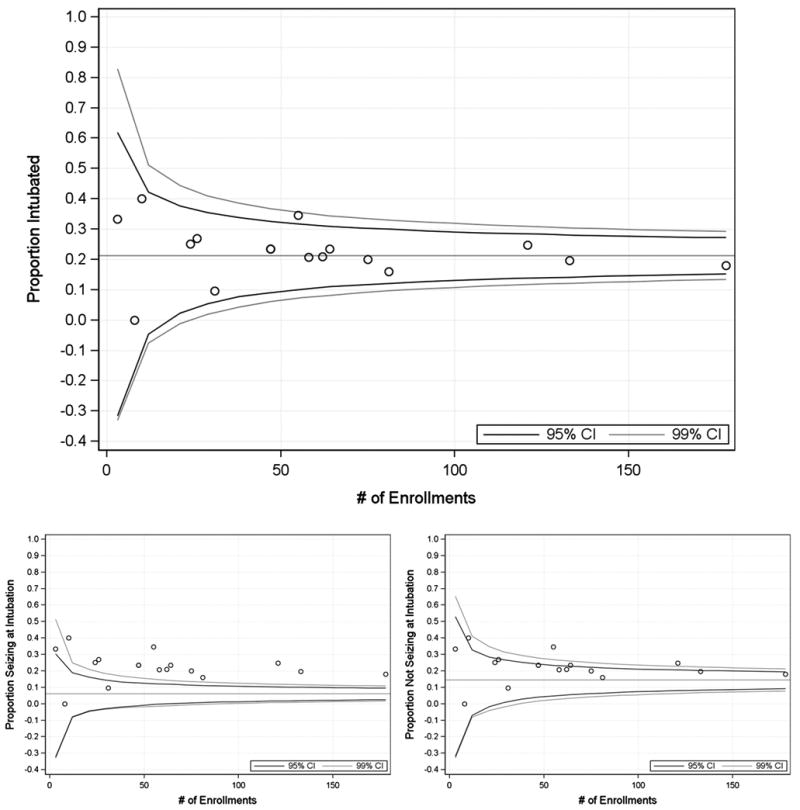
Variation in endotracheal intubation rates by enrolling sites. Proportion intubated (top), proportion seizing during intubation (lower left), and proportion not seizing during intubation (lower right)
Discussion
Despite its frequency and potential importance in clinical practice, the use of endotracheal intubation in patients with status epilepticus is poorly characterized. In this broad- based study involving 79 hospitals and 33 EMS agencies, endotracheal intubation occurred in 1 out of every 5 status epilepticus patients. This is a different rate than previously reported [1, 8, 11].
The most commonly reported primary indications for intubation in status epilepticus patients are respiratory depression, recurrent seizures, or depressed mental status. These indications are not mutually exclusive. An intubation for persistent (rather than recurrent) seizures was coded as respiratory depression or depressed mental status. All 3 indications are consistent with current guidelines for intubation [12]. However, the clinical importance of mechanical ventilation is more obvious in those who are failing to oxygenate or ventilate and in those who have coma induced with general anesthetics to treat their status epilepticus, than in those who are intubated for airway protection.
The overall intubation frequency of 21 % is higher than that in previous studies that enrolled similar out-of-hospital status epilepticus patients, and there is substantial variability in the use of intubation [1]. It may be that the changes in the prevailing attitudes about the use of intubation for airway protection in sedated postictal patients contribute to variability in practice and the increasing use of intubation in this population. This is supported by less variability in intubation rates in the one-third of patients thought to be seizing at the time of intubation than in those with more subjective intubation criteria. Substantial use for short-term airway protection is also suggested by durations of intubation of less than 24 h in 42 % of those intubated.
Intubation as compared to non-intubation and late intubation as compared to early intubation are both markers for patients with more severe pathology and worse mortality. The former finding is consistent with the intubated population having characteristics already associated with increased mortality in refractory status epilepticus, such as being older and not having a known seizure disorder [13]. The latter finding may be due to early intubations occurring more often in clinically undifferentiated patients, while later intubations likely occurred in many patients whose morbidity had become more evident. Alternatively, it is also possible early intubation actually contributes to improved outcomes in some patients if those with later intubations develop more physiologic consequences of status epilepticus or more complications of an unprotected airway, such as aspiration [5–7].
Clinicians caring for patients with status epilepticus in the prehospital or ED setting make rapid airway decisions with limited information. There is often uncertainty in whether a patient's postictal respiratory depression or depressed mental status will quickly improve or linger and put that patient at risk for airway compromise. There are no clinical guidelines to inform clinicians on this matter. Future studies might focus on identifying a cohort of status epilepticus patients who would benefit from early endotracheal intubation, such as refractory status epilepticus or those patients in whom a short period of watchful waiting may be more appropriate than early endotracheal intubation.
Limitations
There are a few limitations to this study. The randomized treatment protocol was limited to the prehospital setting, and this protocol did not include directives for airway management. Hence, all data on airway management are drawn from routine practice patterns across the enrolling sites. There may have been selection or provider bias, with clinicians having different thresholds for performing endotracheal intubation. The prehospital selection of study subjects narrows the scope of this analysis such that the results may not apply to inpatients with status epilepticus. Also the prehospital administration of benzodiazepines does not allow conclusions regarding endotracheal intubation for the vast majority of patients reaching a hospital in status epilepticus without any prehospital pharmacologic treatment, since there was no placebo arm.
Although the study included specific demographic and clinical factors that impact decisions regarding airway management, other important factors may not have been assessed. For example, clinicians may have been more likely to perform endotracheal intubation if a patient was to be transferred to a tertiary care center. Such data were not recorded. Specific rescue medications administered for refractory seizures were not recorded and may have influenced rates of endotracheal intubation. Nevertheless, rates between study sites were comparable. Also, due to the quality of documentation of the narratives and the overlap of the clinical conditions, there may have been misclassification between respiratory depression and depressed mental status as the reason for intubation.
There was also significant variability in the timing of late intubations. Early intubations occurred within the first 30 min of enrollment, but late intubations could have occurred any time from this 30 min time point until hospital discharge. Lastly, because the study is limited by the lack of prospective comparison of airway management in these subjects, it is not possible to establish causal relationship between the characteristics described and endotracheal intubation.
Conclusions
ETI is common in patients with prehospital treatment of status epilepticus, particularly among the elderly or those with refractory seizures. However, the overall duration of intubation is often for a short time period. Any ETI and late ETI are both associated with higher mortality. More selective and appropriately timed use of ETI in the appropriate patients with prehospital status epilepticus may be warranted.
Acknowledgments
Funding This study was supported by awards 5U01NS056975, U01NS059041, and 5U10NS058974-5 from the National Institute of Neurological Disorders and Stroke (NINDS), the Office of the Director, National Institutes of Health (OD), BARDA, and the NIH CounterACT program. The funding source had no role in the design and conduct of this study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Appendix
The Neurological Emergencies Treatment Trials investigators
The Neurological Emergencies Treatment Trials investigators that performed the RAMPART study are listed by center or hub. Hubs are ordered by the number of subjects enrolled. Participating EMS agencies are listed with each hub.
The Neurological Emergencies Treatment Trials investigators are
Clinical Coordinating Center
Robert Silbergleit, MD, Daniel Lowenstein, MD, William Barsan, MD, Arthur Pancioli, MD, Valerie Stevenson, BAS, RRT, CCRP, Erin Zaleski, MA, Deneil Harney, MPH, MSW, Donna Harsh, MS, Joy Pinkerton, BSN, RN, MS, Allison Kade, BA, Nicholas Siewert, BA, Ashley Pinawin, BS, Catherin Ring, Phebe Brenne.
National EMS Coordinator
Kay Vonderschmidt, MPA, MS-EM, NREMT-P
Statistical Data Management Center
Valerie Durkalski, PhD, Yuko Palesch, PhD, Catherine Dillon, Keith Pauls, Qi Wu, Wenle Zhao, PhD
National Institutes of Health
Robin Conwit, MD, Scott Janis, PhD, David Jett, PhD, Brandy Fureman, PhD
Hubs (ordered by number of subjects enrolled)
Wayne State University (178)
Hub Principal Investigator: Robert D. Welch, MD, MS
Primary Study Coordinators: Lynnmarie Mango, MPH, Valerie H. Mika, MS
EMS Director(s)/Coordinator: Jenny Atas, MD
Other Site Investigators: Robert Dunne, MD, Douglas Wheaton, MD, Phillip Levy, MD, MPH, Marc-Anthony Velilla, MD, Robert Sherwin, MD, Brian O’Neil, MD, Angela Groves, MD, Marc Rosenthal, DO, PhD
Participating EMS Service: Detroit EMS
University of Cincinnati (133)
Hub Principal Investigator: Arthur Pancioli, MD
Primary Study Coordinators: Irene Ewing, RN, BSN, Peggy Waymeyer, RN
EMS Director(s)/Coordinator: Jason McMullan, MD, M.
Kay Vonderschmidt, MPA, MS-EM, NREMT-P
Other Site Investigators: Hamilton Schwartz, MD, Brian Stettler, MD, William Knight, MD, Opeolu Adeoye, MD, Rhonda Cadena, MD, Jordan Bonomo, MD, Erin Grise, MD, Laura Heitsch, MD, Nick Gagai, CCRP, Pamela Schmit, RN BSN, Sara Stark, Med, Traci Doellman, RN, David Ficker, MD
Participating EMS Services: Cincinnati Fire Department, BlueAsh Fire Department, Forest Park Fire Department, Green Township Fire Department, Florence Fire Department, Independence Fire Department
University of California San Francisco (121)
Hub Principal Investigator: J. Claude Hemphill, III, MD, MAS
Primary Study Coordinators: Michele Meeker, RN, BSN, Kelley Rosborough, BA
EMS Director(s)/Coordinator: Jeany Duncan EMT-P Other Site Investigators: Karl Sporer, MD, FACEP, FACP, Alan Gelb, MD; Wade Smith, MD, PhD, Prasanthi Ramanujam, MD, Kazuma Nakagawa, MD, Asma Moheet, MD, Hooman Kamel, MD, Bharath Naravetla, MD, Mary Mercer, MD, Christine Wong, MD
Participating EMS Services: San Francisco Fire Department, EMS Division
University of Texas-Houston (81)
Hub Principal Investigator: Elizabeth Jones, MD
Trial Principal Investigator: Truman J. Milling, MD
Primary Study Coordinators: Misty Ottman, RN, BSN, Ben King, Laura LaChance
EMS Directors/Coordinators: Jeff Brockman, RN, Pete Didonato, EMT-P
Other Site Investigator: Paul Hinchey, MD
Participating EMS Service: Austin-Travis County EMS
Emory University (75)
Hub Principal Investigator: David W. Wright, MD
Trial Principal Investigators: Matthew D. Bitner, MD, Gerald W. Beltran, DO
Primary Study Coordinator: Harriet Howlett-Smith, RN, CCRC
EMS Director/Coordinator: Andrea G. McDougal
Other Site Investigators: Jeffrey F. Linzer Sr, MD, Lisa H. Merck, MD MPH, Tamara Espinoza, MD
Participating EMS Service: Grady EMS
Henry Ford Health System (64)
Hub Principal Investigator: Christopher A. Lewandowski, MD
Trial Principal Investigator: Taher T. Vohra, MD
Primary Study Coordinators: Paula L. Crouse, RN, BSN., MA., Anna E. Baker, RN, BSN
EMS Director/Coordinator: Dean R. Creech EMT-P, I/C
Other Site Investigator: Andrew N. Russman, DO, Joseph B. Miller, MD, Jumana Nagarwala, MD, Raymond Fowkes, MD
Participating EMS Services: Detroit EMS, West Bloomfield Fire and EMS Services
Stanford University (62)
Hub Principal Investigator: James V. Quinn, MD, MS
Primary Study Coordinators: Stephanie Casal. RN, CNS, Anke Hebig, Mark Liao
EMS Director/Coordinator: Peter D’Souza, MD
Participating EMS Services: Palo Alto Fire Department, San Jose Fire Department, Redwood City Fire Department, San Mateo Fire Department
University of Arizona (58)
Hub Principal Investigator: Kurt R. Denninghoff, MD
Trial Principal Investigator: Daniel W. Spaite, MD
Primary Study Coordinator: Bruce Barnhart, RN, CEP
EMS Director(s)/Coordinator: Willie Haro, CEP
Other Site Investigator: Bentley J. Bobrow, MD
Participating EMS Service: Glendale Fire Department
Virginia Commonwealth University (55)
Hub Principal Investigator: Joseph P. Ornato, MD
Primary Study Coordinator: Sallie L. Noe, RN
EMS Director/Coordinator: Alan D. Payne, CCEMTP
Other Site Investigators: Alan R. Towne, MD, Michael C. Kurz, MD, John T. Carmack, MD
Participating EMS Service: Richmond Ambulance Authority
University of Minnesota (47)
Hub Principal Investigator: Michelle Biros, MD
Trial Principal Investigator: Brian Mahoney, MD
Primary Study Coordinator: Corey Sargent
Other Site Investigators: David Hildebrandt, Chris Kummer, Doug Gesme
Participating EMS Services: Hennepin County EMS
Medical College of Wisconsin (47)
Hub Principal Investigator: Tom P. Aufderheide, MD
Primary Study Coordinator: Joseph T. Brandt Jr., BS, EMT-P
EMS Director/Coordinator: M. Riccardo Colella, DO
Other Site Investigators: Ron Pirrallo, MD, MHSA, Walter Bialkowski, MS, Benjamin Hermanson, BS, Christopher Sandoval, BS, EMT-P, Kevin Morrow, MFA, Kelly McCormick, BS, MBA, Katherine Burpee, BA, Geri Price, BS, Dawn Kawa, BA
Participating EMS Services: Milwaukee County EMS, Milwaukee Fire Department, Franklin Fire Department, Greenfield Fire Department, North Shore Fire Department, Oak Creek Fire Department, South Milwaukee Fire Department, Wauwatosa Fire Department, West Allis Fire Department
University of Kentucky (31)
Hub Principal Investigator: Roger L. Humphries, MD
Primary Study Coordinator: Linda Dechtenberg, RN, BSN, CCRC
EMS Director/Coordinator: Christofer Sweat
Other Site Investigator: L.Creed Pettigrew, MD,MPH
Participating EMS Service: Lexington-Fayette Urban County Government Division of Fire & Emergency Services
University of Pennsylvania (26)
Hub Principal Investigator: Jill M. Baren, MD, MBE
Trial Principal Investigator: R. Daniel Bledsoe, MD
Primary Study Coordinator: Barbie Stahlman, MS, Katherine Lamond, BA, Pamela G. Nathanson, MBE
Other Site Investigator: Scott E. Kasner, MD, MSCE, Peter D. Le Roux, MD
Participating EMS Services: York Hospital Medic 97, White Rose Ambulance, Grantley Fire Company, Jacobus Lions Ambulance Club, West York Ambulance
Oregon Health & Science University (24)
Hub Principal Investigators: Craig R. Warden, MD, MPH, Robert A. Lowe, MD, MPH
Primary Study Coordinator: Rachel N. Stone, CCRP
Participating EMS Service: Clackamas Fire District #1
New York Presbyterian Hospital (10)
Hub Principal Investigator: Stephan Mayer, MD, FCCM
Trial Principal Investigator: Neal Flomenbaum, MD
Primary Study Coordinators: M. Cristina Falo, PhD, Lisa-Vanessa Magitbay, RN, Chirag Surti
EMS Directors/Coordinators: Heidi Cordi, MD, Daniel Ribaudo
Other Site Investigators: Axel Rosengart, MD, PhD, Matthew Vibbert, MD, Santiago Ortega-Gutierrez, MD, H. Alex Choi, MD, Emily Gilmore, MD, Rishi Malhotra, MD, Lawrence Berger
Participating EMS Services: New York Presbyterian
Temple University (8)
Hub Principal Investigator: Nina T. Gentile, MD
Trial Principal Investigators: Alvin Wang, DO, Christopher Vates, MD, Ben Usatch, MD
Primary Study Coordinators: Brent B. Freeman, Stacey L. Cleary
Participating EMS Services: Volunteer Medical Services Corps of Lower Merion and Narberth (Narberth Ambulance), Life Lion EMS
University of Maryland (3)
Hub Principal Investigator: Barney Stern, MD
Trial Principal Investigators: Tricia Ting, MD, Gregory Krauss, MD
Primary Study Coordinators: Virginia Ganley, RN, Susan Rice, RN, Jennifer Ronald
EMS Director/Coordinator: Michelle Stevens, RN
Other Site Investigators: Brian Browne, MD, Robert Rosenthal, MD, Peter Hill, MD
Participating EMS Services: Maryland Institute for Emergency Medical Services Systems (MIEMSS), Baltimore City EMS
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Taher T. Vohra, Email: tvohra1@hfhs.org, Department of Emergency Medicine, Henry Ford Hospital, CFP 259, 2799 W Grand Blvd, Detroit, MI 48202, USA.
Joseph B. Miller, Department of Emergency Medicine, Henry Ford Hospital, CFP 259, 2799 W Grand Blvd, Detroit, MI 48202, USA
Katherine S. Nicholas, Department of Public Health Sciences, Medical University of South Carolina, Charleston, SC, USA
Panayiotis N. Varelas, Departments of Neurology and Neurosurgery, Wayne State University, Henry Ford Hospital, Detroit, MI, USA
Donna M. Harsh, Department of Emergency Medicine, University of Michigan, Ann Arbor, MI, USA
Valerie Durkalski, Department of Public Health Sciences, Medical University of South Carolina, Charleston, SC, USA.
Robert Silbergleit, Department of Emergency Medicine, University of Michigan, Ann Arbor, MI, USA.
Henry E. Wang, Department of Emergency Medicine, University of Alabama School of Medicine, Birmingham, AL, USA
References
- 1.Alldredge BK, Gelb AM, Isaacs SM, et al. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med. 2001;345:631–7. doi: 10.1056/NEJMoa002141. [DOI] [PubMed] [Google Scholar]
- 2.DeLorenzo RJ, Hauser WA, Towne AR, et al. A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology. 1996;46:1029–35. doi: 10.1212/wnl.46.4.1029. [DOI] [PubMed] [Google Scholar]
- 3.Varelas PN, Mirski MA. Status epilepticus. Curr Neurol Neurosci Rep. 2009;9:469–76. doi: 10.1007/s11910-009-0069-7. [DOI] [PubMed] [Google Scholar]
- 4.Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17:3–23. doi: 10.1007/s12028-012-9695-z. [DOI] [PubMed] [Google Scholar]
- 5.Meldrum BS, Brierley JB. Prolonged epileptic seizures in primates. Ischemic cell change and its relation to ictal physiological events. Arch Neurol. 1973;28:10–7. doi: 10.1001/archneur.1973.00490190028002. [DOI] [PubMed] [Google Scholar]
- 6.Meldrum BS, Horton RW. Physiology of status epilepticus in primates. Arch Neurol. 1973;28:1–9. doi: 10.1001/archneur.1973.00490190019001. [DOI] [PubMed] [Google Scholar]
- 7.Meldrum BS, Vigouroux RA, Brierley JB. Systemic factors and epileptic brain damage. Prolonged seizures in paralyzed, artificially ventilated baboons. Arch Neurol. 1973;29:82–7. doi: 10.1001/archneur.1973.00490260026003. [DOI] [PubMed] [Google Scholar]
- 8.Chamberlain JM, Okada P, Holsti M, et al. Lorazepam vs diazepam for pediatric status epilepticus: a randomized clinical trial. JAMA. 2014;311:1652–60. doi: 10.1001/jama.2014.2625. [DOI] [PubMed] [Google Scholar]
- 9.Silbergleit R, Durkalski V, Lowenstein D, et al. Intramuscular versus intravenous therapy for prehospital status epilepticus. N Engl J Med. 2012;366:591–600. doi: 10.1056/NEJMoa1107494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spiegelhalter DJ. Funnel plots for comparing institutional performance. Stat Med. 2005;24:1185–202. doi: 10.1002/sim.1970. [DOI] [PubMed] [Google Scholar]
- 11.Langer JE, Fountain NB. A retrospective observational study of current treatment for generalized convulsive status epilepticus. Epilepsy Behav. 2014;37:95–9. doi: 10.1016/j.yebeh.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Roppolo LP, Walters K. Airway management in neurological emergencies. Neurocrit Care. 2004;1:405–14. doi: 10.1385/NCC:1:4:405. [DOI] [PubMed] [Google Scholar]
- 13.Rossetti AO, Logroscino G, Milligan TA, Michaelides C, Ruffieux C, Bromfield EB. Status epilepticus severity score (STESS): a tool to orient early treatment strategy. J Neurol. 2008;255:1561–6. doi: 10.1007/s00415-008-0989-1. [DOI] [PubMed] [Google Scholar]


