Abstract
Objective
To investigate the effects of mild traumatic brain injury (mTBI) in children on symptom ratings of behavior problems across the first year post injury.
Setting
Emergency departments of two regional children’s hospitals.
Participants
Parents of 176 children with mTBI and 90 with orthopedic injury (OI) ages 8–15 years.
Design
Group comparisons of post-injury parent and teacher ratings of child behavior problems controlling for background factors.
Main Measures
Child Behavior Checklist (CBCL) and Teacher’s Report Form (TRF).
Results
For younger but not older children in the sample, children with mTBI compared to those with OI had higher post-injury ratings on the CBCL Total Behavior Problem scale, t (264) = 3.34, p<.001, and higher rates of T-scores ≥ 60 on this scale, OR (CI) = 3.00 (1.33, 6.77), p=.008. For children with mTBI, hospitalization, motor vehicle accidents, loss of consciousness, and MRI abnormality were associated with higher parent or teacher ratings.
Conclusions
School-age children with mTBI are at risk for persistent symptoms of behavior problems, especially if mTBI is more severe or occurs at a younger age. The findings justify monitoring of behavior long after injury and further research to identify risk factors for these symptoms and their association with clinical disorders.
Keywords: Child, Injury, Brain, Traumatic Mild, Neurobehavioral Manifestations
INTRODUCTION
Epidemiological surveys indicate that about half a million US children from birth to 14 years of age visit an emergency department each year for traumatic brain injury (TBI) and that about 40,000 are hospitalized.1 Mild TBI (mTBI) accounts for the vast majority of these injuries.2 Post-concussive symptoms (PCS) are prevalent soon after injury and include reports of headaches, dizziness, fatigue, depressed or anxious mood, sleep disturbance, light sensitivity, forgetfulness, and concentration difficulties.3 Although these symptoms typically resolve within a few months after mTBI,4,5 they can persist for a year or more in some children.6–9
The longer-term consequences of mTBI for behavioral adjustment more generally have been less well researched and findings are inconsistent.10 One study found that children who sustained mTBI at ≤ 14 years had higher rates of psychiatric disorders, most often hyperactivity, than controls without mTBI and that the differences persisted across a 3-year follow-up.11 Another study found higher rates of hyperactivity/inattention and conduct disorder at 10–13 years in children who sustained mTBI prior to age 10 years compared to children without head injuries.12 The negative effects of mTBI were largely confined to children who were hospitalized for their injuries and were more pronounced when injuries were sustained at younger ages. However, other studies have failed to demonstrate persisting effects of mTBI on child behavior.13,14
The purpose of this study was to examine the effects of mTBI on parent and teacher ratings of child behavior problems across the first year post injury. The study was part of a larger project investigating the pattern of recovery in the cognitive and behavioral outcomes of pediatric mTBI in which children were assessed shortly after injury and at 3- and 12-month post-injury follow-ups. To control for the experience of an acute injury and for tendencies for children who sustain injuries to be at heightened risk for pre-injury behavior problems,15 school-age children with mTBI were compared to those with orthopedic injuries (OI). As previously reported, the mTBI group continued to have higher ratings of cognitive PCS than the OI group out to 1 year post injury.7–9 Based on our findings and data indicating associations of PCS with behavior problems in children with mTBI,5,16 we hypothesized that the mTBI group would have higher ratings of behavior problems than the OI group across the first year post injury and that these differences would be more evident for younger children.12,17,18 In view of previous research indicating age differences in the effects of mTBI and evidence for diminishing effects of mTBI with increasing time post injury,7,8 moderating effects of these factors on group differences were also considered. A secondary goal was to determine if higher ratings of behavior problems within the mTBI group were related to markers of more severe mTBI.
METHODS
Sample
Children in both the mTBI and OI groups were 8–15 years at the time of injury and were recruited between September, 2001 and October, 2006 from consecutive admissions to the outpatient emergency departments of two children’s hospitals. The project was approved by the institutional review boards of the hospitals that collaborated on the study, and informed parental consent and child assent were obtained prior to participation.
Consistent with existing definitions,19,20 eligibility for the mTBI group included blunt head trauma and at least one of the following indications of concussion: loss of consciousness (LOC) <30 minutes, a Glasgow Coma Scale (GCS)21 score of 13–14, or at least two of the following acute signs of concussion: persistent post-traumatic amnesia, transient neurological deficits, vomiting, nausea, headache, diplopia, and dizziness. Children were excluded if they had delayed neurological deterioration or medical contraindications to magnetic resonance imaging (MRI) but not if they had brain injuries on clinical CT scans (i.e., cases of complicated mTBI) or were hospitalized following evaluation in the emergency department. Children in the OI group sustained upper or lower extremity fractures associated with a score of 3 or less on the Abbreviated Injury Scale (AIS)22 without evidence of head injury or signs of concussion. Children were excluded from both groups if they or their parents were non-English-speaking or if they had received surgical treatment; sustained injuries that precluded neuropsychological testing conducted as a part of the larger project (e.g., dominant arm fractures) or that were related to drug or alcohol use; or had shock, hypoxia, or hypotension with injury or histories of previous head injury requiring medical intervention, neurological disorder or intellectual disability, abuse, or hospitalization for psychiatric disorder. To increase generalizability, children with prior histories of learning disabilities, attention deficit hyperactive disorder, or other behavior disorders were not excluded from either group.
Participation rates for children who met eligibility criteria were 47% for the mTBI group and 35% for the OI group. Eligible non-participants did not differ significantly from participants in age at injury, sex, race, or census-tract-based demographic measures (e.g., income level, poverty rate).23 Children participating in the initial post-acute (baseline) assessments included 186 in the mTBI group and 99 in the OI group. Nineteen children (10 with mTBI, 9 with OI) who did not return for follow-up visits at 3 and 12 month post injury or had sustained a TBI after the initial assessment (4 from mTBI group, 1 from OI group) were excluded, leaving 176 children with mTBI 90 with OI. The 19 excluded children did not differ significantly from the participants in sex, race, or socioeconomic status (SES) as defined by an average of the sample z-scores for years of maternal education, median family income for census tract, and parent occupational status as measured by the Duncan Socioeconomic Index.24 Analysis also failed to reveal differences between excluded and included children with mTBI on the measures of severity considered in this study (see below) or between the excluded and included in either group on the Injury Severity Scale, which summarizes injury severity on the AIS across the three most affected body regions.22
The mTBI and OI groups did not differ significantly in age at injury, days between injury and the baseline visit, months between subsequent visits, sex, SES, race, or IQ as measured by a short form of the Wechsler Abbreviated Scale of Intelligence25 administered at baseline (Table 1). However, a higher proportion of the mTBI group was injured in motor-vehicle-related accidents and a higher proportion of OI group had “other” injuries such as rough-housing. The subset with teacher ratings (122/176 with mTBI and 66/90 with OI) had higher SES and a lower proportion of non-white children than the subset without teacher ratings (p<.05).
Table 1.
Sample Characteristics.
| Characteristic | mTBI Group (n=176) | OI Group (n=90) |
|---|---|---|
| Age at injury in years, M (SD) | 11.94 (2.23) | 11.73 (2.22) |
| Months between injury and 3-month follow-up, M (SD) | 3.21 (0.39) | 3.21 (0.41) |
| Months between injury and 12-month follow-up, M (SD) | 12.26 (0.50) | 12.23 (0.60) |
| Males, n (%) | 123 (70%) | 59 (66%) |
| White race, n (%) | 125 (71%) | 60 (67%) |
| Socioeconomic status (SES), M (SD) | 0.06 (0.90) | −0.06 (1.18) |
| WASI short form IQ at baseline assessment, M (SD) | 99.95 (13.84) | 100.12 (14.80) |
| Abbreviated Injury Severity Scale, M (SD)* | 4.56 (4.46) | 3.27 (1.52) |
| Injury mechanism:* | ||
| Falls, n (%) | 35 (20%) | 19 (21%) |
| Sports/recreation, n (%) | 99 (56%) | 56 (62%) |
| Motor vehicle, n (%) | 29 (16%) | 3 (3%) |
| Other, n (%) | 13 (7%) | 12 (13%) |
| Injury to other body region in addition to head, n (%) | 44 (25%) | --- |
| Loss of consciousness (LOC), n (%) | 72 (41%) | --- |
| Glasgow Coma Scale score 13–14, n (%) | 23 (13%) | --- |
| Skull fracture, n (%) | 14 (8%) | --- |
| Injury-related abnormality on acute-phase computed tomography (CT) scan, n/122 (%) | 10 (8%) | --- |
| Injury-related abnormality on MRI, n/172 (%) | 28 (16%) | |
| Hospitalized, n (%)* | 55 (31%) | 0 (0%) |
Note: mTBI = mild traumatic brain injury; OI = orthopedic injury; WASI = Wechsler Abbreviated Intelligence Scale. SES defined as average of sample z scores for year of maternal education, median family income based on census data for the neighborhood of residence, and the Duncan Socioeconomic Index (a measure of occupational status). Other injuries comprise those associated with rough-housing and carelessness (e.g., wrestling, tripping, running into objects). CT abnormalities included 6 children with parenchymal lesions or edema and 4 with extra-axial lesions only. MRI abnormalities included 22 with parenchymal lesions, 4 with extra-axial hemorrhages only, and 2 with mild atrophy only.
p<.05.
Procedure and Measures
Parents completed retrospective ratings of pre-injury functioning on the Child Behavior Checklist (CBCL)26 at the baseline assessment. The CBCL was then re-administered at the 3- and 12-month follow-ups to obtain measures of concurrent post-injury behavior. Post-injury teacher ratings were obtained by mailing the Teacher’s Report Form (TRF)26 to teachers immediately after the 12-month visit. The regular classroom teacher was asked to complete the TRF for children attending primary school and a teacher of an academic subject for children with multiple teachers. To insure ratings were made by the current teacher, mailing of the TRFs was delayed until the second month of the next school year for children injured during the summer months. The CBCL and TRF are Likert ratings that assess a broad range of behavior problems and are sensitive to post-injury changes in behavior following pediatric TBI.27 The primary outcome measures were the Total Behavior Problem scales for the CBCL and TRF. Secondary outcomes were subscale ratings for Internalizing and Externalizing problems, Social Problems, Thought Problems, and Attention Problems. Scores for corresponding scales from the CBCL and TRF at the 12-month follow-up were only modestly correlated (r’s .22–.50, all p’s<.01), suggesting that they captured different perspectives on children’s behavior.
CT scans were conducted as part of acute clinical care and MRIs as a component of the baseline assessment (in most cases within 3 weeks of injury) for children with mTBI. MRIs included sagittal T1-weighted spin echo, axial T2-weighted and proton density fast spin echo, coronal gradient echo, coronal fluid attenuated inversion recovery (FLAIR), and axial diffusion-weighted echo planar images.
Data Analysis
Raw scores from the CBCL and TRF used to maximize sensitivity to age-related change and cube root transformations were applied prior to analysis to correct for non-normality in the raw score distributions. Group comparisons of CBCL ratings at the 3- and 12-month follow-ups were conducted using general linear mixed model analysis.28 Factors in the analysis were group (mTBI vs. OI), age at injury, time since injury (3 and 12 months), and the interactions of these factors. Covariates were SES, race, and sex. Analysis of scores on each CBCL scale also controlled for the corresponding pre-injury rating. Similar analysis was conducted on TRF scores but did not include time since injury or pre-injury ratings as factors. Preliminary analysis of the total sample revealed associations of higher pre-injury ratings, younger age at injury, and lower SES with higher post-injury ratings on multiple CBCL and TRF scales. To reduce risks of overfitting and enhance the interpretability of findings,29,30 initial models were trimmed by deleting non-significant higher- and then lower-order interactions.
Additional analyses were conducted using χ2 analysis and General Estimating Equations (GEE)31 to determine if group differences on rating scores were accompanied by differences in rates (or odds) of elevated T-scores. Because few children received ratings in the clinical range, elevations were defined as T-scores falling ≥1 standard deviation above the normative mean (i.e., ≥60). The use of this cut-off was justified by the utility of similar cut-offs to identify clinical “caseness” in previous research and by evidence that such less stringent cut-offs provide a more optimal balance of sensitivity and specificity in predicting future behavior disorders.32,33 GEE analyses included the same factors as the mixed models. Mixed model and GEE analyses were also conducted within the mTBI to determine if any of several indicators of more severe mTBI were related to ratings of behavior problems, including LOC, motor-vehicle-related mechanism of injury, hospital admission, accompanying non-head injuries, and neuroimaging abnormalities.7–9,12,34 These factors were examined in analyses that paralleled those described above, with the presence vs. absence of each severity indicator examined separately in place of group membership.
Effects sizes were estimated in terms of Cohen’s d35 for group differences in dimensional ratings (i.e., standardized mean differences), standardized regression coefficients for differential change (slopes) over time post-injury, and odds ratios (95% confidence intervals) for T-score elevations. Small, medium, and large effect sizes, respectively, are 0.2, 0.5, and 0.8 for d and 0.1, 0.3, and 0.5 for standardized regression coefficients. The alpha level for significance was .05 for the two primary measures and .01 for each of the five subscale scores from the CBCL and TRF.
RESULTS
Differences Between the mTBI and OI Groups in Behavior Outcomes
Analysis of CBCL ratings revealed age at injury x group interactions for the Total Behavior Problem scale, F (1,267) = 7.42, p<.007; Externalizing, F (1,266) = 14.89, p<.001; and Social Problems, F (1,264) = 8.87, p<.003. To examine the interaction, younger and older ages were defined as ages that were 1 SD below and 1 SD above the sample mean, corresponding to mean ages of 10 and 14 years respectively. Group differences in model estimates were significant only at the younger age level for the Total Behavior Problem scale, estimate (standard error) [est. (se)] = 0.29 (0.09), p<.001, d = .29, and Externalizing, est. (se) = 0.29 (0.08), p<.001, d = .29. A similar trend was found for Social Problems, est. (se) = 0.22 (0.09), p=.013, d = .30. To illustrate these differences, Figure 1 graphs model estimates of mean scores on the Total Behavior Problem scale for younger and older children in the two groups at the 3- and 12-month follow-ups.
Figure 1.
Model estimates of mean ratings on the CBCL Total Behavior Problems scale (cube root transformation) at 3- and 12-month follow-up assessments for mild traumatic brain injury (mTBI) and orthopedic injury (OI) groups at younger and older age levels. Mean scores are estimates from mixed model analysis that control for the pre-injury rating on this measure as well as SES (see text for definition), race, sex, and age at injury. Error bars designate values within 1 standard error of the means. The group difference across the two assessments is significant only at the younger age level.
Group comparisons of T-scores ≥ 60 using GEE revealed similar findings, with group x age at injury interactions for the CBCL Total Behavior Problem scale, χ2 (1) = 4.61, p=.032; Externalizing, χ2 (1) = 10.91, p=.001; and Social Problems, χ2 (1) = 7.10, p=.008. Follow-up analyses indicated higher rates of covariate-adjusted proportions of T-score elevations on the Total Behavior Problems scale for the mTBI group compared to the OI group for younger children only, 14% vs. 5%, odds ratio (95% confidence interval) [OR (CI)] = 3.00 (1.33, 6.77), p=.008. Similar trends were found for Externalizing, 13% vs. 4%, OR (CI) = 3.76 (1.32, 10.71), p=.013, and Social Problems, 13% vs. 6%, OR (CI) = 2.57 (1.09, 6.08), p=.032. Analysis also revealed an unexpected and potentially spurious trend for higher Externalizing scores for the older children with OI compared to those with mTBI, 13% vs. 5%, OR (CI) = 0.32 (0.12, 0.84), p=.022. Analysis of the TRF failed to reveal any group differences (data not shown).
The ranges of the T-scores for the two groups, covariate-adjusted mean T-scores, and frequencies of T-scores at or above specific cut-offs for the CBCL and TRF scales are presented in Tables 2 for descriptive purposes. Mean T-scores were similar for the two groups and well within the average range, with few T-scores at clinically significant levels. As evident in Table 2, rates of elevated T-scores tended to be lower in the mTBI group than in the OI group. However, this same trend was found for most of the pre-injury CBCL ratings. The mTBI group had significantly lower rates of pre-injury T-scores ≥60 than the OI group for the Total Problem scale, χ2 (1, N=221) = 7.22, p=.007, and Social Problems, χ2 (1, N=216) = 7.19, p=.007, with similar but non-significant differences in rates of T-score elevations on other scales and in pre-injury raw score ratings. These pre-injury differences may help to account for the disparities between the unadjusted data presented in Table 2 and findings from the adjusted group comparisons. Table 2, moreover, describes overall group differences rather than the more subtle differences revealed by analysis, which accounted for background factors and varied by age at injury. Because pre-injury behavior problems were not rated by teachers and thus could not be controlled in analysis of the TRF, any tendency for the mTBI group to have fewer symptoms prior to injury than the OI group also would have made it more difficult to detect group differences on the teacher ratings.
Table 2.
Descriptive data on ranges, covariate adjusted T-scores, and frequencies (%) of elevated T-scores for the mild traumatic brain injury (mTBI) and orthopedic injury (OI) groups for the Child Behavior Checklist (CBCL) and Teacher Rating Form (TRF).
| 3-month CBCL | 12-month CBCL | 12-month TRF | ||||
|---|---|---|---|---|---|---|
| Scale | mTBI | OI | mTBI | OI | mTBI | OI |
| Total Behavior Problem: | ||||||
| Range | 23–74 | 23–77 | 23–75 | 23–80 | 31–75 | 31–82 |
| Adjusted mean (se) | 48.57 (0.54) | 46.71 (0.75) | 47.65 (0.59) | 46.63 (0.83) | 47.77 (0.82) | 48.10 (1.09) |
| T-score ≥60 | 29 (17%) | 17 (19%) | 21 (13%) | 13 (16%) | 18 (15%) | 18 (27%) |
| T-score>65 | 11 (6%) | 9 (10%) | 7 (4%) | 9 (11%) | 6 (5%) | 12 (18%) |
| T-score>70 | 7 (4%) | 4 (4%) | 4 (2%) | 5 (6%) | 1 (1%) | 4 (6%) |
| Internalizing Problems: | ||||||
| Range | 31–77 | 31–80 | 31–72 | 31–79 | 36–71 | 36–77 |
| Adjusted mean (se) | 48.94 (0.59) | 47.14 (0.83) | 47.85 (0.64) | 47.16 (0.90) | 47.64 (0.94) | 48.75 (1.26) |
| T-score ≥60 | 29 (17%) | 18 (20%) | 19 (12%) | 13 (16%) | 18 (15%) | 13 (20%) |
| T-score>65 | 13 (8%) | 10 (11%) | 8 (5%) | 8 (10%) | 4 (3%) | 5 (8%) |
| T-score>70 | 6 (3%) | 5 (6%) | 3 (2%) | 4 (5%) | 1 (1%) | 4 (6%) |
| Externalizing Problems: | ||||||
| Range | 30–74 | 30–73 | 30–76 | 32–78 | 39–77 | 39–80 |
| Adjusted mean (se) | 47.89 (0.47) | 47.05 (0.66) | 48.15 (0.59) | 47.19 (0.82) | 48.23 (0.71) | 48.38 (0.95) |
| T-score ≥60 | 20 (12%) | 13 (14%) | 21 (13%) | 14 (17%) | 15 (12%) | 18 (27%) |
| T-score>65 | 7 (4%) | 9 (10%) | 7 (4%) | 6 (7%) | 4 (3%) | 9 (14%) |
| T-score>70 | 5 (3%) | 2 (2%) | 4 (2%) | 2 (2%) | 2 (2%) | 5 (8%) |
| Social Problems: | ||||||
| Range | 50–87 | 50–83 | 50–73 | 50–81 | 50–81 | 50–74 |
| Adjusted mean (se) | 54.35 (0.37) | 53.18 (0.52) | 53.02 (0.35) | 53.61 (0.49) | 52.31 (0.45) | 53.32 (0.60) |
| T-score ≥60 | 28 (16%) | 17 (19%) | 16 (10%) | 16 (19%) | 12 (10%) | 17 (26%) |
| T-score>65 | 14 (8%) | 11 (12%) | 6 (4%) | 14 (17%) | 3 (3%) | 4 (6%) |
| T-score>70 | 4 (2%) | 4 (4%) | 1 (1%) | 5 (6%) | 1 (1%) | 1 (2%) |
| Thought Problems: | ||||||
| Range | 50–76 | 50–76 | 50–76 | 50–73 | 50–70 | 50–70 |
| Adjusted mean (se) | 53.48 (0.35) | 52.70 (0.48) | 53.11 (0.35) | 52.51 (0.49) | 51.40 (0.38) | 50.96 (0.50) |
| T-score ≥60 | 17 (10%) | 14 (16%) | 16 (10%) | 11 (13%) | 4 (3%) | 6 (9%) |
| T-score>65 | 8 (5%) | 8 (9%) | 6 (4%) | 9 (11%) | 2 (2%) | 4 (6%) |
| T-score>70 | 2 (1%) | 3 (3%) | 1 (1%) | 3 (4%) | 0 (0%) | 0 (0%) |
| Attention Problems: | ||||||
| Range | 50–82 | 50–84 | 50–78 | 50–81 | 50–84 | 50–81 |
| Adjusted mean (se) | 54.96 (0.35) | 53.46 (0.48) | 53.64 (0.35) | 54.01 (0.50) | 53.61 (0.65) | 54.21 (0.87) |
| T-score ≥60 | 36 (21%) | 14 (16%) | 17 (10%) | 17 (20%) | 17 (14%) | 20 (30%) |
| T-score>65 | 20 (12%) | 6 (7%) | 10 (6%) | 6 (7%) | 6 (5%) | 13 (20%) |
| T-score>70 | 10 (6%) | 4 (4%) | 4 (2%) | 3 (4%) | 2 (2%) | 4 (6%) |
Note: se = standard error. Means for both CBCL and TRF ratings are adjusted for SES and race. Means for post-injury CBCL ratings were additionally adjusted for corresponding pre-injury CBCL ratings. Despite the unexpected trend for T-score elevations to be higher for the OI group than for the mTBI group, this same trend was evident on most of the pre-injury ratings. Frequencies of pre-injury CBCL T-scores ≥60 for the mTBI and OI groups, respectively, were 22 (13%) vs. 23 (26%) for the Total Problem scale, 24 (14%) vs. 19 (21%) for Internalizing, 23 (13%) vs. 20 (22%) for Externalizing, 25 (14%) vs. 25 (28%) for Social Problems, 28 (16%) vs. 21 (23%) for Thought Problems, and 43 (24%) vs. 18 (20%) for Attention Problems. See text for findings from analysis of covariate-adjusted group differences in raw ratings, T-scores ≥60, and effects of age at injury and time (3- versus 12-months, CBCL only).
Associations of mTBI Characteristics with Behavior Outcomes
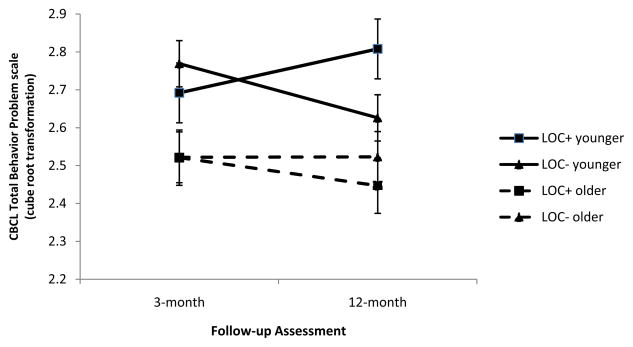
Analysis of CBCL ratings for the Total Behavior Problem scale revealed a LOC(+/−) x age at injury x time since injury interaction, F (1 ,171) = 4.94, p=.028. Follow-up analysis indicated a significant decline in scores from the 3- to 12-month follow-up for the younger LOC- subgroup, est. (se) = −0.20 (0.09), p = .035, standardized regression coefficient = .20, but not for the younger LOC+ subgroup (see Figure 2). Hospitalization was associated (as a main effect) with higher scores on the TRF Total Behavior Problem scale, F (1,116) = 16.63, est. (se) = 0.70 (0.17), p<.001, d = .70; Externalizing, F (1,116) = 14.80, est. (se) = 0.65 (0.17), p<.001, d = .65; Internalizing, F (1,116) = 12.67, est. (se) = 0.66 (0.19), p<.001, d = .66; and Social Problems, F (1,116) = 13.08, est. (se) = 0.64 (0.18), p<.001, d = .64; and motor-vehicle-related injuries with higher scores on the TRF Total Behavior Problem scale, F (1,116) = 4.69, est. (se) = 0.50 (0.23), p=.032, d = .50. MRI abnormality interacted with age at injury in analyses of TRF Thought Problems, F (1,113) = 6.95, p<.010, with a trend for MRI abnormality to be associated with higher scores only among younger children, est. (se) = 0.70 (0.35), p=.047, d = .70.
Figure 2.
Model estimates of mean ratings on the CBCL Total Behavior Problems scale (cube root transformation) at 3- and 12-month follow-up assessments for mild traumatic brain injury (mTBI) subgroup with loss of consciousness (LOC+) vs. the subgroup without loss of consciousness (LOC-) at younger and older age levels. Mean scores are estimates from mixed model analysis that control for the pre-injury rating on this measure as well as SES (see text for definition), race, sex, and age at injury. Error bars designate range of values within 1 standard error of the means. Scores declined significantly from 3 to 12 months only for the LOC- subgroup at the younger age level, with a trend (p=.072) for lower scores for the younger LOC- subgroup compared to the younger LOC+ subgroup at the 12-month follow-up.
In parallel with these findings, GEE analysis of rates of T-score ≥60 revealed a LOC+/− x time since injury interaction for the CBCL Total Behavior Problem scale, χ2 (1) = 4.01, p=.045. Follow-up of this interaction indicated a decline in rates of T-scores ≥60 over follow-up only for the LOC- subgroup, OR (CI) = 0.37 (0.15, 0.89), p=.027, with a trend for the LOC+ subgroup to have a higher rate of elevated T-scores than the LOC- subgroup at the 12-month follow-up, OR (CI) = 2.80 (0.92, 8.56), p=.071. Additionally, hospitalization was associated with higher rates of score T-scores ≥60 on the TRF Total Behavior Problem scale, OR (CI) = 3.50 (1.14, 10.76), p=.029; Internalizing, OR (CI) = 4.55 (1.49, 13.96), p=.008; and Social Problems, OR (CI) = 44.30 (5.01, 391.70), p<.001. Analysis also revealed that a lower rate of T-scores ≥60 for CBCL Social Problems for the LOC+ relative to LOC- subgroup, F (1,173) = 7.38, p=.007, a finding that is difficult to reconcile with the adverse effects of LOC on the CBCL Total Behavior Problem scale.
DISCUSSION
Younger children with mTBI, compared to those with OI, had higher parent ratings of behavior problems out to 1 year post injury. Within the mTBI group, LOC was associated with higher parent ratings of behavior problems, whereas hospitalization and motor-vehicle-related injury mechanism were associated with higher teacher ratings. Although acute abnormalities on CT scans were not associated with behavior ratings, there was also a trend for post-acute MRI abnormality to be associated with higher teacher ratings of Thought Problems in younger children. The findings are consistent with past reports of persisting behavioral sequelae of mTBI5,11,12,17,18,36 and support other evidence pointing to younger age at injury and more severe injury as risk factors for adverse behavioral, educational, and health outcomes of mTBI.5,7–9,11,12 Although younger children may be more vulnerable to brain insults,37,38 other possible explanations for this age effect include a lesser ability of younger children to adjust to mTBI-related somatic and cognitive PCS or greater parental awareness of behavioral changes in younger children.
The findings extend past evidence for persisting behavior sequelae of mTBI by demonstrating differences relative to a comparison group with other injuries. Our procedure of recruiting consecutive admissions to the two participating emergency departments and low attrition rate also contribute to our confidence in the findings. The results contrast with the failure of a similarly designed study to reveal adverse effects of mTBI relative to other injuries on the CBCL at 1 year post injury.14 However, the latter investigation did not examine age at injury as a moderator of group differences and did not include children hospitalized for mTBI. As nearly one third of our mTBI group was hospitalized, our mTBI cohort likely included children with more severe injuries. In comparing our findings to previous reports, it is important to emphasize that effects sizes for significant differences were small to medium and that differences were only significant for younger children on the CBCL or in relation to injury severity factors. As illustrated by the descriptive data presented in Table 2, adverse effects of mTBI were less evident in comparisons that failed to consider these factors.
Increased post-injury symptoms in the mTBI group relative to OI group on the CBCL at a younger age level were found on a summary rating of behavior problems as well as on ratings of externalizing and social problems. These differences suggest that younger school-age children with mTBI are at increased risk for symptoms of disruptive and oppositional behaviors and difficulties relating to others. Higher ratings of internalizing problems by teachers for the subgroup of children hospitalized for mTBI compared to those not hospitalized suggests that children admitted to an inpatient unit following mTBI are more likely to develop symptoms of anxiety, withdrawal, and depressed mood. The findings indicate risks for both dimensional increases in symptoms of behavior problems and higher rates of moderately elevated symptom ratings relative to normative standards (T-scores ≥60). However, as the rates of score elevations within the clinical range were too small to permit meaningful analysis, the findings fail to indicate an increased risk for clinical disorders. While we cannot rule out the possibility of post-injury-onset disorders in a small subset of children, behavior changes following mTBI may be primarily within the subclinical range.
Neural abnormalities have been identified in some individuals with mTBI39,40 and insults to brain circuits underlying behavior and mood self-regulation have been proposed as a potential neural basis of post-injury-onset affective disorders.17 Other factors that may have contributed to post-injury increases in behavior symptoms in the mTBI group include parent expectations regarding the effects of mTBI, children’s emotional response to their injuries, and persisting adjustment issues triggered by difficulties in the child’s ability to cope with post-acute symptoms.41,42 As part of our larger project, we administered a coping questionnaire to children and found associations of coping style with PCS.43 A further possibility is that parents were more negatively affected by transient changes in the children’s level of physical discomfort, behavior, or mentation, and may have reacted in ways that exacerbated or failed to normalize the child’s longer-term adjustment.44
Several limitations must be considered in interpreting the findings. Some parents may have minimized the adverse effects of mTBI, while others may have over-reported symptoms based on their expectations of the injury effects.15,42 Retrospective parent ratings of pre-injury status may also have been biased, although these ratings were collected soon after injury. Group differences in hospitalization (31% of mTBI vs. 0% of OI) and lower rates of pre-injury CBCL T-score elevations in the mTBI group compared to children with OI also raise questions regarding the appropriateness of these children as a comparison group. While our major purpose in recruiting children with OI was to control for behavioral predispositions to injury, mTBI and OI are associated with different types and degrees of traumatic experience. A further issue relates to the different results obtained for teacher vs. parent ratings. Some differences might be anticipated based on the modest correlations between the CBCL and TRF, as well as the fact that pre-injury status was controlled only in analysis of the CBCL. While the findings confirm the importance obtaining teacher ratings in assessing the behavioral consequences of mTBI, demographic differences between the children with and without teacher ratings suggest caution in generalizing the teacher results to a broader population of children with mTBI. Finally, children with mTBI recruited from emergency departments of children’s hospitals may not be representative of the larger population as this excludes those who are treated in other settings or do not receive acute medical care.
In conclusion, the findings suggest that children with mTBI are at risk for persistent post-injury increases in symptoms of behavior problems and that these effects are more prominent in younger school-age children and in those who sustain LOC, are hospitalized, or have motor-vehicle-related trauma or post-acute abnormalities on MRI. The findings imply a need to monitor behavioral consequences of mTBI long after injury, particularly in children in these higher risk subgroups. More research is needed to replicate the findings, determine the extent to which these symptoms are associated with clinically significant behavior problems, and examine mechanisms underlying the group differences in behavior ratings and their association with injury characteristics. We also need to identify factors that contribute to risks for persistent behavior symptoms and explore interventions to prevent or reduce these sequelae. Injury factors of interest include measures of the severity of the initial brain insult, as measured by acute abnormalities on MRI, symptom presentation, or neuropsychological impairments.39 Non-injury factors include children’s psychological adjustment to the trauma or to initial somatic, emotional, and cognitive symptoms, as well as family adaptations to the injury and to children’s initial symptoms.20 Interventions approaches could focus on managing of children’s return to school, educating children and their parents about injury consequences, or helping children, families, and schools cope with the physical and cognitive effects of injury.45,46
Acknowledgments
Source of Funding: This research was funded by project grants R01 HD39834 and K02 HD44099 from the National Institute of Child Health and Human Development to Keith Owen Yeates, Ph.D.
The authors thank Lauren Ayr, Anne Birnbaum, Amy Clemens, Taryn Fay, Amanda Lininger, Katie Pestro, Elizabeth Roth, Elizabeth Shaver, and Heidi Walker for their assistance in carrying out this project. Dr. Yeates is currently affiliated with the Department of Psychology, University of Calgary, Calgary, Alberta, Canada.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: Emergency department visits, hospitalizations, and deaths 2002–2006. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Control and Prevention; 2010. [Google Scholar]
- 2.Guerrero JL, Thurman DJ, Sniezek JE. Emergency department visits associated with traumatic brain injury: United States 1995–1996. Brain Inj. 2000;14:181–186. [PubMed] [Google Scholar]
- 3.Satz P, Alfano MS, Light R, et al. Persistent post-concussive syndrome: A proposed methodology and literature review to determine the effects, if any, of mild head and other bodily injury. J Clin Exp Neuropsychol. 1999;21:620–628. doi: 10.1076/jcen.21.5.620.870. [DOI] [PubMed] [Google Scholar]
- 4.Carroll LJ, Cassidy JD, Peloso PM, et al. Prognosis for mild traumatic brain injury: Results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med, Suppl. 2004;43:84–105. doi: 10.1080/16501960410023859. [DOI] [PubMed] [Google Scholar]
- 5.Ponsford J, Willmott C, Rothwell A, et al. Cognitive and behavioral outcomes following mild traumatic head injury in children. J Head Trauma Rehabil. 1999;14:360–372. doi: 10.1097/00001199-199908000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Barlow KM, Crawford S, Stevenson A, Sandhu SS, Belanger F, Dewey D. A prospective epidemiological study of post-concussion syndrome in pediatric mild traumatic brain injury. Pediatrics. 2010;126:e374–e381. doi: 10.1542/peds.2009-0925. [DOI] [PubMed] [Google Scholar]
- 7.Taylor HG, Dietrich A, Nuss K, Wright M, Rusin J, Bangert B, Minich N, Yeates KO. Post-concussive symptoms in children with mild traumatic brain injury. Neuropsychol. 2010;24:148–159. doi: 10.1037/a0018112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yeates KO, Taylor HG, Rusin J, et al. Longitudinal trajectories of post-concussive symptoms in children with mild traumatic brain injuries and their relationship to acute clinical status. Pediatrics. 2009;123:735–743. doi: 10.1542/peds.2008-1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeates KO, Kaizar E, Rusin J, et al. Reliable change in post-concussive symptoms and its functional consequences among children with mild traumatic brain injury. Arch Pediatr Adolesc Med. 2012;166:615–622. doi: 10.1001/archpediatrics.2011.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keightley ML, Cote P, Rumney P, et al. Psychosocial consequences of mild traumatic brain injury in children: results of a systematic review by the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil. 2014;93:5192–5200. doi: 10.1016/j.apmr.2013.12.018. [DOI] [PubMed] [Google Scholar]
- 11.Massagli TL, Fann JR, Burington BE, Jaffe KM, Katon WJ, Thompson RS. Psychiatric illness after mild traumatic brain injury in children. Arch Phys Med Rehabil. 2004;85:1428–1434. doi: 10.1016/j.apmr.2003.12.036. [DOI] [PubMed] [Google Scholar]
- 12.McKinlay A, Dalrymple-Alford JC, Horwood LJ, Fergusson DM. Long term psychosocial outcomes after mild head injury in early childhood. J Neurol Neurosurg Psychiatry. 2002;73:281–288. doi: 10.1136/jnnp.73.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bijur PE, Haslum M. Cognitive, behavioral, and motoric sequelae of mild head injury in a national birth cohort. In: Broman S, Michel ME, editors. Traumatic head injury in children. Oxford University Press; 1995. pp. 147–164. [Google Scholar]
- 14.Light R, Asarnow R, Satz P, Zucha K, McCleary C, Lewis R. Mild closed-head injury in children and adolescents: Behavior problems and academic outcomes. J Consult Clin Psychol. 1998;66:1023–1029. doi: 10.1037//0022-006x.66.6.1023. [DOI] [PubMed] [Google Scholar]
- 15.Goldstrohm SL, Arffa S. Preschool children with mild to moderate traumatic brain injury: An exploration of immediate and post-acute morbidity. Arch Clin Neuropsychol. 2005;20:675–695. doi: 10.1016/j.acn.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Yeates KO, Luria J, Bartkowski H, Rusin J, Martin L, Bigler ED. Post-concussive symptoms in children with mild closed-head injuries. J Head Trauma Rehabil. 1999;14:337–350. doi: 10.1097/00001199-199908000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Max JE, Keatley E, Wilde EA, et al. Anxiety disorders in children and adolescents in the first six months after traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2011;23:29–30. doi: 10.1176/jnp.23.1.jnp29. [DOI] [PubMed] [Google Scholar]
- 18.Max JE, Keatley E, Wilde EA, et al. Depression in children and adolescents in the first 6 months after traumatic brain injury. Int J Dev Neurosci. 2012;30:239–245. doi: 10.1016/j.ijdevneu.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Center for Injury Prevention and Control. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Atlanta, GA: Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 20.Yeates KO, Taylor HG. Neurobehavioural outcomes of mild head injury in children and adolescents. Pediatr Rehabil. 2005;8:5–16. doi: 10.1080/13638490400011199. [DOI] [PubMed] [Google Scholar]
- 21.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 22.American Association for Automotive Medicine. The abbreviated injury scale (AIS)-1990 revision. Des Plaines, IL: American Association for Automotive Medicine; 1990. [Google Scholar]
- 23.Federal Financial Institutions Examinations Council Geocoding System. [Accessed January 1, 2005—November 1, 2005]; Available at: http://www.ffiec.gov/Geocode/default.htm.
- 24.Stevens G, Cho JH. Socioeconomic indexes and the new 1980 census occupational classification scheme. Soc Sci Res. 1985;14:142–168. [Google Scholar]
- 25.Wechsler D. Wechsler Abbreviated Scale of Intelligence: Test manual. San Antonio, TX: The Psychological Corporation; 1999. [Google Scholar]
- 26.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 27.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 28.Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat. 1998;23:323–355. [Google Scholar]
- 29.Hawkins DM. The problem of overfitting. J Chem Inf Comput Sci. 2004;44:1–12. doi: 10.1021/ci0342472. [DOI] [PubMed] [Google Scholar]
- 30.Tabachnick BG, Fidell LS. Using multivariate statistics. New York: Harper & Row; 1983. [Google Scholar]
- 31.Diggle PJ, Liang K-Y, Zeger SL. Analysis of longitudinal data. New York: Oxford University Press; 1994. [Google Scholar]
- 32.Petty CR, Rosenbaum JF, Hirshfeld-Becker DR, et al. The Child Behavior Checklist broad-band scales predict subsequent psychopathology: a five-year follow-up. J Anxiety Disord. 2008;22:532–539. doi: 10.1016/j.janxdis.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwartz LS, Taylor HG, Drotar D, et al. Long-term behavior problems following pediatric traumatic brain injury: prevalence, predictors, and correlates. J Pediatr Psychol. 2003;28:251–264. doi: 10.1093/jpepsy/jsg013. [DOI] [PubMed] [Google Scholar]
- 34.Levin HS, Hanten G, Roberson G, et al. Prediction of cognitive sequelae based on abnormal computed tomography findings in children following mild traumatic brain injury. J Neurosurg Pediatrics. 2008;1:461–470. doi: 10.3171/PED/2008/1/6/461. [DOI] [PubMed] [Google Scholar]
- 35.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 36.Anderson VA, Catroppa C, Morse S, Haritou F, Rosenfeld J. Outcome from mild head injury in young children: a prospective study. J Clin Exp Neuropsychol. 2001;23:705–717. doi: 10.1076/jcen.23.6.705.1015. [DOI] [PubMed] [Google Scholar]
- 37.Anderson V, Jacobs R, Spencer-Smith M, et al. Does early age at brain insult predict worse outcome? Neuropsychological implications. J Pediatr Psychol. 2010;35:716–727. doi: 10.1093/jpepsy/jsp100. [DOI] [PubMed] [Google Scholar]
- 38.Taylor HG, Alden J. Age-related differences in outcome following childhood brain injury: An introduction and overview. J Int Neuropsychol Soc. 1997;3:555–567. [PubMed] [Google Scholar]
- 39.Bigler ED. Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. J Int Neuropsychol Soc. 2008;14:1–22. doi: 10.1017/S135561770808017X. [DOI] [PubMed] [Google Scholar]
- 40.Yallampalli R, Wilde EA, Bigler ED, et al. Acute white matter differences in the fornix following mild traumatic brain injury using diffusion tensor imaging. J Neuroimaging. 2010;XX:1–4. doi: 10.1111/j.1552-6569.2010.00537.x. [DOI] [PubMed] [Google Scholar]
- 41.Asarnow RF, Satz P, Light R, Lewis R, Neumann E. Behavior problems and adaptive functioning in children with mild and severe closed head injury. J Pediatr Psychol. 1991;16:543–555. doi: 10.1093/jpepsy/16.5.543. [DOI] [PubMed] [Google Scholar]
- 42.Gunstad J, Suhr JA. “Expectation as etiology” versus “the good old days”: Postconcussion syndrome symptom reporting in athletes, headache sufferers, and depressed individuals. J Int Neuropsychol Soc. 2001;7:323–333. doi: 10.1017/s1355617701733061. [DOI] [PubMed] [Google Scholar]
- 43.Woodrome SE, Yeates KO, Taylor HG, et al. Coping strategies as a predictor of post-concussive symptoms in children with mild traumatic brain injury. J Int Neuropsychol Soc. 2011;17:317–326. doi: 10.1017/S1355617710001700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wade SL, Taylor HG, Walz NC, et al. Parent-child interactions during the initial weeks following brain injury in young children. Rehabilitation Psychol. 2008;53:180–190. doi: 10.1037/0090-5550.53.2.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kirkwood MW, Yeates KO, Taylor HG, Randolph C, McCrea M, Anderson VA. Management of pediatric mild traumatic brain injury: A neuropsychological review from injury through recovery. Clin Neuropsychol. 2008;22:769–800. doi: 10.1080/13854040701543700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ponsford J, Willmott C, Rothwell A, et al. Impact of early intervention on outcome after mild traumatic brain injury in children. Pediatrics. 2001;108:1297–1303. doi: 10.1542/peds.108.6.1297. [DOI] [PubMed] [Google Scholar]