Abstract
Study Design Literature review.
Objective The aim of this review is to highlight challenges in the development of a comprehensive surgical algorithm to accompany the AOSpine Thoracolumbar Spine Injury Classification System.
Methods A narrative review of the relevant spine trauma literature was undertaken with input from the multidisciplinary AOSpine International Trauma Knowledge Forum.
Results The transitional areas of the spine, in particular the cervicothoracic junction, pose unique challenges. The upper thoracic vertebrae have a transitional anatomy with elements similar to the subaxial cervical spine. When treating these fractures, the surgeon must be aware of the instability due to the junctional location of these fractures. Additionally, although the narrow spinal canal makes neurologic injuries common, the small pedicles and the inability to perform an anterior exposure make decompression surgery challenging. Similarly, low lumbar fractures and fractures at the lumbosacral junction cannot always be treated in the same manner as fractures in the more cephalad thoracolumbar spine. Although the unique biomechanical environment of the low lumbar spine makes a progressive kyphotic deformity less likely because of the substantial lordosis normally present in the low lumbar spine, even a fracture leading to a neutral alignment may dramatically alter the patient's sagittal balance.
Conclusion Although the new AOSpine Thoracolumbar Spine Injury Classification System was designed to be a comprehensive thoracolumbar classification, fractures at the cervicothoracic junction and the lumbosacral junction have properties unique to these junctional locations. The specific characteristics of injuries in these regions may alter the most appropriate treatment, and so surgeons must use clinical judgment to determine the optimal treatment of these complex fractures.
Keywords: AOSpine Thoracolumbar Spine Injury Classification System, thoracolumbar trauma, cervicothoracic junction, low lumbar burst fractures, lumbosacral fractures
Introduction
An ideal spine injury classification system is able to both guide treatment and facilitate clear communication between the surgeons, researchers, and trainees. Early classifications such as the Denis classification and Magerl classification described the thoracolumbar spine and were later extended to describe cervical spine injuries.1 2 More recently, dedicated classification systems for the thoracolumbar and subaxial cervical spine have been published or presented,3 4 including the AOSpine Thoracolumbar Spine Injury Classification System and the AOSpine Subaxial Cervical Spine Injury Classification System.5 6
The AOSpine Thoracolumbar Spine Injury Classification System initially separates fractures into one of three morphologic types (Fig. 1)5: type A, the compression injuries; type B, the injuries associated with a failure of the anterior or posterior tension band without evidence of translation; and type C, the translational injuries resulting from the failure of all the stabilizing elements leading to a complete disruption of the bony and soft tissue hinge. Type A (Fig. 2) and type B (Fig. 3) fractures are further separated into five and three subtypes, respectively. Next, the patient is assigned one of five neurologic grades5: N0, the patient is neurologically intact; N1, the patient had a transient neurologic deficit; N2, the patient has persistent symptoms or signs of a nerve root injury; N3, the patient has an incomplete spinal cord injury or a cauda equina injury; N4, the patient has a complete spinal cord injury; and NX, the neurologic examine of the patient cannot be obtained. Finally, the classification allows for patient-specific modifications: M1 denotes a possible ligamentous injury to the tension band that may necessitate surgery, and M2 denotes injury-specific morbidities, such as ankylosing spondylitis, polytrauma, significant medical comorbidities, among others, that may alter the recommended treatment.5
Fig. 1.
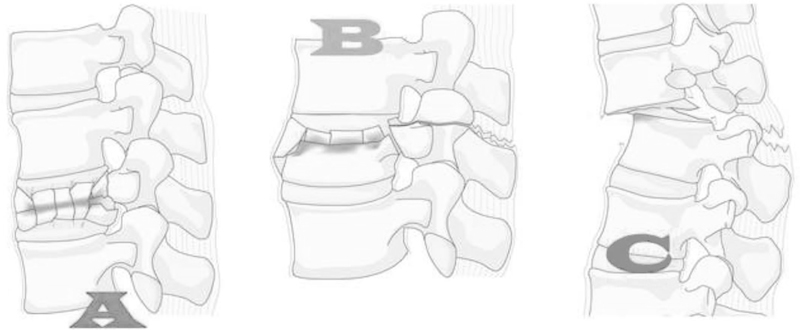
The three types of thoracolumbar fractures: type A, compression injuries; type B, injuries associated with a failure of the anterior or posterior tension band without evidence of translation; and type C, translational injuries resulting from the failure of all elements leading to complete disruption of the bony and soft tissue hinge.5
Fig. 2.
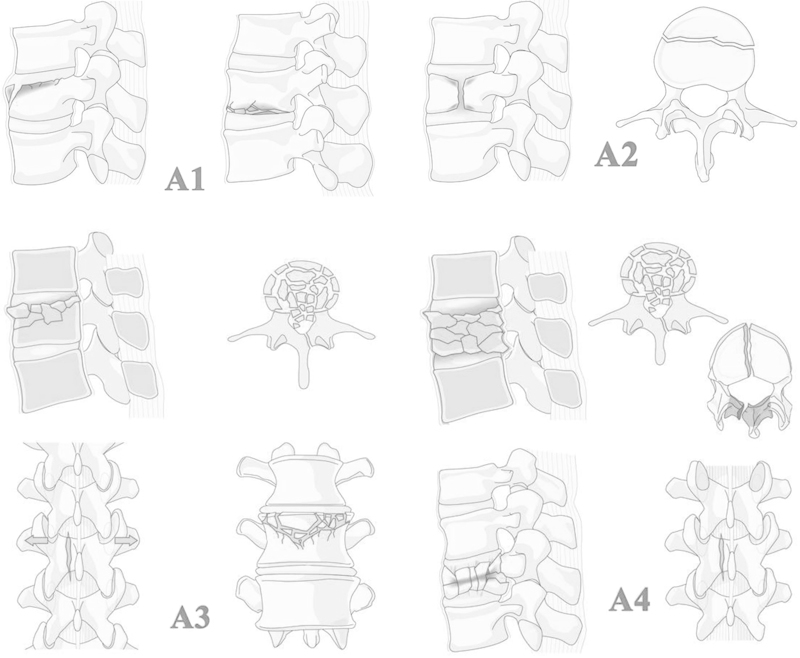
The subtypes of compression injures: A0, spinous/transverse process fracture; A1, compression/wedge fracture; A2, pincer fracture; A3, incomplete burst/burst with a single end plate involved; A4, complete burst/burst with both end plates involved.5
Fig. 3.
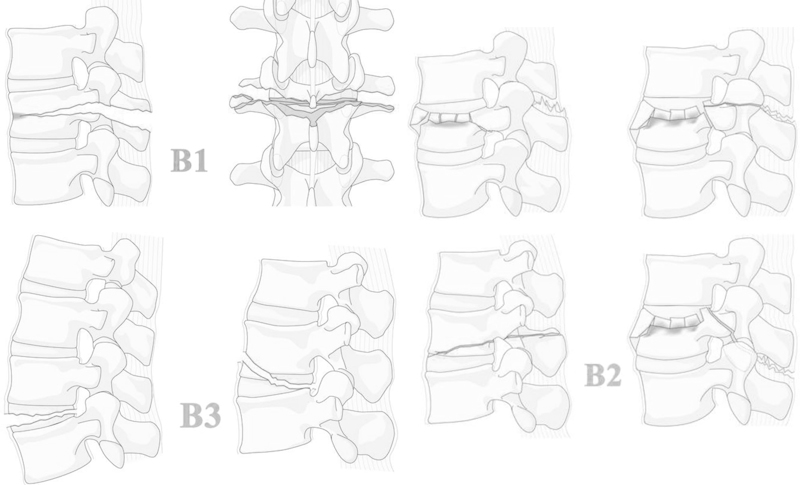
The subtypes of tension band injuries: B1, transosseous disruption; B2, posterior tension band injury; B3, anterior tension band injury.5
Initially substantial inter- and intraobserver reliability of the AOSpine Thoracolumbar Spine Injury Classification System was reported in a group of highly trained academic spine surgeons (0.72 and 0.77, respectively),5 and later moderate interobserver reliability (kappa = 0.56) of the system was reported in 100 surgeons from all regions of the world who had no prior knowledge of the system.7 Utilizing an injury severity score for each variable in the classification,8 Kepler et al proposed a Spine Injury Score (Table 1) to accompany the new classification.9 Although the surgical threshold has yet to be established, the Spine Injury Score will be used to help guide treatment.
Table 1. The Spine Injury Score that accompanies the AOSpine Thoracolumbar Injury Classification System.
| Fracture morphology | Points |
|---|---|
| A: Compression | |
| A0 | 0 |
| A1 | 1 |
| A2 | 2 |
| A3 | 3 |
| A4 | 5 |
| B: Tension band | |
| B1 | 5 |
| B2 | 6 |
| B3 | 7 |
| C: Translation | |
| C | 8 |
| Neurology | |
| N0 | 0 |
| N1 | 1 |
| N2 | 2 |
| N3 | 4 |
| N4 | 4 |
| Nx | 3 |
| Patient-specific modifiers | |
| M1 | 1 |
| M2 | 0 |
Given the regional variation in treatment of thoracolumbar trauma, significant research has been performed attempting to determine the need for a regional interpretation of the Spine Injury Score; however, little has been written about the possible need for altering the surgical threshold based on the injury location within the thoracolumbar spine. There are significant differences in both the bony morphology and the neural elements between the upper thoracic spine and the lower lumbar spine, and these differences may significantly affect the ideal treatment algorithm. This aim of this narrative review, which collates the expertise of a multidisciplinary group of experienced spine surgeons in the AOSpine International Trauma Knowledge Forum, is to highlight two possible difficulties in the development of a single surgical algorithm for the entire thoracolumbar spine.
The Cervicothoracic Junction
Although a universally accepted definition of the cervicothoracic junction has not been defined, with different authors reporting C7–T1, C6–T2, and C6–T3 as the cervicothoracic junction, this review will consider fractures between C6–T3 as the cervicothoracic junction. Fractures at this region account for 2.4 to 4.5% of spine fractures,10 and although these injuries may technically occur in the thoracic spine, they often behave similar to subaxial cervical fractures with 60 to 83% of these injuries resulting in neurologic impairment.11 12 The higher incidence of neurologic injuries at this level is likely multifactorial. First, the upper thoracic spinal canal is particularly narrow, leading to an increased risk of neurologic compression with any canal compromise. Additionally, the cervicothoracic junction down to T4 is a watershed area for the blood supply to the spinal cord. The terminal branches of the vertebral, thyrocervical, and costoclavicular branches of the subclavian artery supply the caudal cervical spinal cord, and the radicular vessels from the proximal intercostal arteries provide the blood supply to the cephalad thoracic spinal cord.11 Comparatively, significant canal compromise in the lumbar spine may or may not be associated with a major neurologic injury, as the spinal cord terminates around L2 and the cauda equina has a much higher tolerance for compressive lesions.13
The upper thoracic vertebrae also are morphologically more similar to cervical vertebrae than lumbar vertebrae. Stanescu et al reported on the bony characteristics of 128 vertebrae in 16 spines between C5 and T5, and they found a similar pedicle length and laminar height and width between the C7 vertebrae and the T1 vertebrae.14 Additionally, despite a statically significant increase in the width of the T1 pedicle compared with the C7 pedicle (7.8 versus 6.5 mm, p < 0.05), the pedicle width decreases between T2 and T5, such that it more closely resembles that of the cervical spine than the lumbar spine.14 15 16 Furthermore, the lamina pedicle angle is fairly consistent from C7 (88.3 degrees) to T2 (90.5 degrees), but then it slowly increases to 96.7 degrees at T5.14 The clinical relevance behind these morphologic similarities can be seen in the comparable prevalence of injuries such as fracture-dislocations, burst fractures, and facet subluxation/dislocations in the subaxial cervical and upper thoracic spine.10
Although the upper thoracic spine more closely resembles the subaxial cervical spine than the lumbar spine, it also has some properties more consistent with the remainder of the thoracic spine than the cervical spine. The facet orientation undergoes a significant change at the cervicothoracic junction, with the facet angle changing from 86 degrees at C7 to 69 degrees at T2 (Fig. 4A) and the disk facet angle rapidly (Fig. 4B) changing from 123 degrees at C6 to 107 degrees at T2.17 Additional morphologic similarities between the upper thoracic spine and the remainder of the thoracic spine include the prominent transverse processes and the stabilizing costovertebral joint.
Fig. 4.
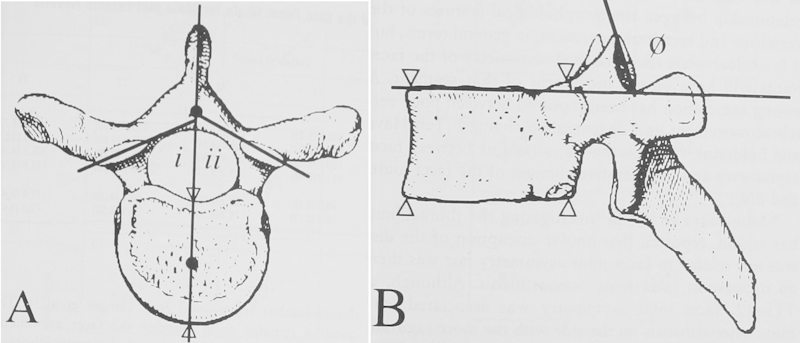
(A) The facet angle and (B) the disk facet angle.17 (i = the right facet angle; ii = the left facet angle; theta = the disk facet angle.)
Although the upper thoracic spine has characteristics of both the subaxial cervical spine and the caudal thoracic spine, there are anatomic features unique to the upper thoracic spine that present specific challenges to the treating surgeon. The change from cervical lordosis to thoracic kyphosis, along with the significant increase in the stiffness of the thoracic spine, makes fractures in this region particularly prone to developing progressive kyphosis18; the successful stabilization of these injuries is difficult as the placement of upper thoracic pedicle screws is challenging given the small pedicle size. Additionally, the presence of the heart and great vessels prohibit an anterior approach to T2–T4; however, performing a complete posterior decompression around the spinal cord is challenging. Manipulation of an already damaged spinal cord can result in permanent neurologic injuries, but the failure to expeditiously decompress the spinal cord will lead to a decreased rate of meaningful neurologic recovery.19
Low Lumbar Fractures
Low lumbar burst fractures (L3–L5) are relatively rare fractures, accounting for 1.2% of all spine fractures,20 and this is due to the unique anatomy of the lower lumbar spine. The stout iliolumbar ligaments afford significant stability to the caudal lumbar vertebrae, and the segments caudal to the pelvic brim and the apex of the lumbar lordosis are somewhat protected from trauma.21 22 23 24 25 However, recently there has been an increased interest in the treatment of these injuries after Lehman et al reported that lower lumbar burst fractures account for 60% of combat-related thoracolumbar fractures in the United States military.24 The authors postulate that this is due to the advent of a new body armor, which provides increased rigidity in the upper lumbar spine, effectively moving the transition zone between the rigid and stable segments into the low lumbar spine. Furthermore, the improvised explosive devices used by combatants in Afghanistan and Iraq result in a violent axial force.24
Historically, many authors have advocated the nonoperative treatment of low lumbar burst fractures, as the biomechanical environment of the low lumbar spine is significantly different from that of the thoracolumbar junction.20 21 25 At the thoracolumbar junction, the immediate transition from the rigid thoracic spine to the more mobile lumbar spine creates a fulcrum that may lead to an increased risk of instability affecting the upper lumbar spine more than the better-protected lower lumbar spine.21 23 24 Moreover, the center of gravity at the thoracolumbar junction is located in the anterior column of the spine, therefore predisposing fractures at this level to develop progressive kyphosis.24 In contrast, caudal to L2 the center of gravity is located posterior to the vertebral body, leading to a more evenly distributed axial force across the fractured vertebra.24 Butler et al reported on 14 neurologically intact patients with an L5 burst fracture.21 Ten were treated nonoperatively and four underwent an L4–S1 instrumented posterolateral fusion. No substantial radiographic difference was identified, with nonoperative patients having 10 degrees of kyphosis compared with 11 degrees in the operative group. However, the nonoperative group reported less pain and improved function at a mean follow-up of 71 months.21 Similarly, Seybold et al reported on 42 patients with low lumbar burst fractures; 22 patients underwent either an anterior, posterior, or combined decompression and fusion.25 Surgical patients had a nonsignificant (p < 0.40) improvement in radiographic alignment (9.8 degrees of lordosis compared with 1.9 degrees), but there was no difference in the ability of the patient to return to work or the functional outcomes between the groups.
Although historic studies have not demonstrated a short or midterm benefit to operative treatment of low lumbar burst fractures, the importance of sagittal balance is a relatively recent concept that has not been reported in any of the aforementioned studies. A fracture at the thoracolumbar junction resulting in neutral or slightly kyphotic focal alignment represents little change from the natural alignment, as the normal lordosis between T12 and L2 is 1.7 degrees.26 However, the normal alignment between L4 and S1 is 49.2 degrees of lordosis,26 so an injury leading to the neutral alignment in the L5 vertebra significantly alters the overall alignment of the spine and dramatically affects the patient's sagittal balance. Although the long-term effects of this altered alignment have not been reported in the spine trauma literature, the deformity literature is clear in demonstrating that a pelvic incidence-lumbar lordosis mismatch leads to significantly inferior health-related quality-of-life outcome measures.27 28 29
Undoubtedly, further studies evaluating the sagittal balance of patients with low lumbar burst fractures are needed; however, it is unclear if this is improved with acute surgical intervention. Both Butler et al and Seybold et al reported no significant difference in the radiographic parameters of patients treated with or without surgery.21 25 However, in a study that included 365 neurologically intact patients with a thoracolumbar compression or burst fracture, Reinhold et al reported an improved ability to restore and maintain lordosis in patients who underwent a combined anterior and posterior procedure.30 Similarly, in a study of 45 patients with thoracolumbar fractures, Schnake et al reported the ability to correct and maintain the alignment over a 5-year period if a combined anterior and posterior approach was used.31
In addition to low lumbar burst fractures, fractures of the L5–S1 facet joint present a unique set of challenges to the treating physician. Although these fractures may occur in isolation, it is also possible that they are the cephalad extension of a sacral fracture resulting in spinopelvic instability.32 The treatment algorithm for these complex fractures is significantly different than for the fractures throughout the rest of the thoracolumbar spine, and a separate AOSpine sacral classification system is being developed.
Specifically, although the need for early decompression in patients with an injury leading to a neurologic deficit in the thoracic and lumbar spine is clear,19 the role for an urgent formal decompression in fractures at the lumbosacral junction is debated in the literature. In one study, Schildhauer et al reported on 22 patients with a neurologic deficit from vertically unstable sacral fractures, and the authors did not perform a formal decompression.33 However, in a separate study published the same year, Schildhauer et al reported on 18 patients with complete bowel and bladder dysfunction from a U-type sacral fracture resulting in lumbopelvic dissociation, and all patients underwent a formal decompression.34 Although there is significant heterogeneity in the two patient populations with regard to the severity of injury and the timing of surgery, only 6/22 patients (27%) who did not undergo a formal decompression had any signs of neurologic recovery, whereas 15/18 patients (84%) who underwent a formal decompression had at least partial neurologic recovery.33 34
In addition to the neurologic differences, the surgical technique for fractures of the lumbosacral junction varies significantly from fractures of the cephalad thoracolumbar spine. Spinopelvic fixation is required for these fractures, and cadaveric studies have demonstrated an enhanced stability with a triangular osteosynthesis (a technique utilizing both spinopelvic fixation and either sacroiliac or trans-sacral screw fixation).35 36
Conclusion
The new AOSpine Thoracolumbar Spine Injury Classification System was developed to facilitate the communication and guide the treatment for thoracolumbar trauma. Although the classification and Spine Injury Score have been published, the surgical threshold is still being investigated.5 9 However, the current review details two areas that will present a challenge to the forthcoming global algorithm for the management of thoracolumbar trauma. Fractures at the cervicothoracic junction and the lumbosacral junction have some properties similar to the remaining thoracolumbar spine, but they also have properties unique to these junctional locations. The criteria to decide on the outcome of injuries in these separate areas may be different. A survey is now being conducted by the AOSpine among spinal surgeons to define which factors are deemed relevant for the short- and long-term outcome in these different areas. Because of the unique properties of fractures at the cervicothoracic junction and lumbosacral junction, injuries at these areas will require surgeons to use their clinical judgment to determine if the fracture is best classified with the new AOSpine Thoracolumbar Spine Injury Classification System, the AOSpine Subaxial Cervical Spine Injury Classification System, or the upcoming AOSpine Sacral Injury Classification System.5 6
Acknowledgments
This manuscript was the work of the AOSpine Trauma Knowledge Forum. Each author was involved in the initial planning of this manuscript, designing the concept of the manuscript, and critically revising the manuscript. This manuscript is part of a much larger project designed to determine a surgical algorithm based off of the AOSpine Thoracolumbar Injury Classification.
AOSpine is a clinical division of the AO Foundation—an independent, medically guided, not-for-profit organization. The AO has a strong financial independence thanks to the foundation's endowment. The annual operating activities are financed through three pillars: Collaboration and support agreements with DePuy Synthes and other industrial partners, return on own financial assets and other third-party income (e.g., participant fees, R&D projects, memberships).
The AOSpine Knowledge Forums are pathology-focused working groups acting on behalf of AOSpine in their domain of scientific expertise. Each forum consists of a steering committee of up to 10 international spine experts who meet biannually to discuss research, assess the best evidence for current practices, and formulate clinical trials to advance their field of spine expertise. Authors are compensated for their travel and accommodation costs. Study support is provided directly through AOSpine's Research department and AO's Clinical Investigation and Documentation unit. There are no other institutional subsidies, corporate affiliations, or funding sources supporting this work unless clearly documented and disclosed.
Footnotes
Disclosures Gregory D. Schroeder, Grant: Medtronic Chris D. Kepler, Grant: AOSpine; Consultant: HealthGrades John K. Koerner, Grant: Medtronic F. Cumhur Oner, Consultant: Medtronic, Synthes; Grant: AOSpine, Depuy Michael G. Fehlings, Grant: AOSpine Bizhan Aarabi, Grant: AOSpine Klaus J. Schnake, Grant: AOSpine; Consultant: Medtronic, Expanding Orthopaedics, OttoBock Healthcare, Depuy Shanmuganathan Rajasekaran, Grant: AOSpine Frank Kandziora, Grant: AOSpine; Board membership: Eurospine, Dwg, DGOU, AOSpine; Consultant: Depuy, Siemens; Speakers bureau: Depuy, Siemens, AOSpine; Educational development: ESJ-OOT Luiz R. Vialle, Grant: AOSpine; Board membership: AOSpine Foundation Alexander R. Vaccaro, Grant: AOSpine; Consultant: Medtronic, Stryker, Globus, Stout, Gerson Lehrman Group, Guidepoint Global, Medacorp, Innovative Surgical Design, Orthobullets, Expert testimony, Ellipse; Scientific advisory board: Innovative Surgical Design, Spinicity; Royalties: Thieme, Jaypee, Elsevier, Taylor and Francis, Aesculap, Globus, Medtronic, Stryker, DePuy; Institutional support: Cerapedics; Stocks: Spine Medica, Computational Biodynamics, Progressive Spinal Technologies, Spinology, Small Bone Innovations, Cross Current, In Vivo, Flagship Surgical, Advanced Spinal Intellectual Properties, Cytonics, Bonovo Orthopaedics, Electrocore, Gamma Spine, Location Based Intelligence, FlowPharma, R.S.I., Replication Medica, Globus, Stout Medical, Rothman Institute and Related Properties, Innovative Surgical Design, Spinicity
References
- 1.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8(8):817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Magerl F, Aebi M, Gertzbein S D, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 3.Vaccaro A R, Hulbert R J, Patel A A. et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine. 2007;32(21):2365–2374. doi: 10.1097/BRS.0b013e3181557b92. [DOI] [PubMed] [Google Scholar]
- 4.Vaccaro A R, Lehman R A Jr, Hurlbert R J. et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976) 2005;30(20):2325–2333. doi: 10.1097/01.brs.0000182986.43345.cb. [DOI] [PubMed] [Google Scholar]
- 5.Vaccaro A R, Oner C, Kepler C K. et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 2013;38(23):2028–2037. doi: 10.1097/BRS.0b013e3182a8a381. [DOI] [PubMed] [Google Scholar]
- 6.Vaccaro A R Koerner J D Radcliff K E et al. AOSpine subaxial cervical spine injury classification system Eur Spine J 2015; February 26 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 7.Kepler C K Vaccaro A R Koerner J D et al. Reliability analysis of the AOSpine thoracolumbar spine injury classification system by a worldwide group of naïve spinal surgeons Eur Spine J 2015; January 20 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 8.Schroeder G D, Vaccaro A R, Kepler C K. et al. Establishing the injury severity of thoracolumbar trauma: confirmation of the hierarchical structure of the AOSpine Thoracolumbar Spine Injury Classification System. Spine (Phila Pa 1976) 2015;40(8):E498–E503. doi: 10.1097/BRS.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 9.Kepler C K, Vaccaro A R, Schroeder G D,
- 10.Amin A, Saifuddin A. Fractures and dislocations of the cervicothoracic junction. J Spinal Disord Tech. 2005;18(6):499–505. doi: 10.1097/01.bsd.0000156831.76055.f0. [DOI] [PubMed] [Google Scholar]
- 11.An H S, Vaccaro A, Cotler J M, Lin S. Spinal disorders at the cervicothoracic junction. Spine (Phila Pa 1976) 1994;19(22):2557–2564. doi: 10.1097/00007632-199411001-00011. [DOI] [PubMed] [Google Scholar]
- 12.Nichols C G, Young D H, Schiller W R. Evaluation of cervicothoracic junction injury. Ann Emerg Med. 1987;16(6):640–642. doi: 10.1016/s0196-0644(87)80060-4. [DOI] [PubMed] [Google Scholar]
- 13.Vaccaro A R, Nachwalter R S, Klein G R, Sewards J M, Albert T J, Garfin S R. The significance of thoracolumbar spinal canal size in spinal cord injury patients. Spine (Phila Pa 1976) 2001;26(4):371–376. doi: 10.1097/00007632-200102150-00013. [DOI] [PubMed] [Google Scholar]
- 14.Stanescu S, Ebraheim N A, Yeasting R, Bailey A S, Jackson W T. Morphometric evaluation of the cervico-thoracic junction. Practical considerations for posterior fixation of the spine. Spine (Phila Pa 1976) 1994;19(18):2082–2088. doi: 10.1097/00007632-199409150-00014. [DOI] [PubMed] [Google Scholar]
- 15.Ebraheim N A, Xu R, Ahmad M, Yeasting R A. Projection of the thoracic pedicle and its morphometric analysis. Spine (Phila Pa 1976) 1997;22(3):233–238. doi: 10.1097/00007632-199702010-00001. [DOI] [PubMed] [Google Scholar]
- 16.Liu J, Napolitano J T, Ebraheim N A. Systematic review of cervical pedicle dimensions and projections. Spine (Phila Pa 1976) 2010;35(24):E1373–E1380. doi: 10.1097/BRS.0b013e3181e92272. [DOI] [PubMed] [Google Scholar]
- 17.Boyle J J, Singer K P, Milne N. Morphological survey of the cervicothoracic junctional region. Spine (Phila Pa 1976) 1996;21(5):544–548. doi: 10.1097/00007632-199603010-00003. [DOI] [PubMed] [Google Scholar]
- 18.Evans D K. Dislocations at the cervicothoracic junction. J Bone Joint Surg Br. 1983;65(2):124–127. doi: 10.1302/0301-620X.65B2.6826614. [DOI] [PubMed] [Google Scholar]
- 19.Fehlings M G, Vaccaro A, Wilson J R. et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS) PLoS ONE. 2012;7(2):e32037. doi: 10.1371/journal.pone.0032037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Finn C A, Stauffer E S. Burst fracture of the fifth lumbar vertebra. J Bone Joint Surg Am. 1992;74(3):398–403. [PubMed] [Google Scholar]
- 21.Butler J S, Fitzpatrick P, Ni Mhaolain A M, Synnott K, O'Byrne J M. The management and functional outcome of isolated burst fractures of the fifth lumbar vertebra. Spine (Phila Pa 1976) 2007;32(4):443–447. doi: 10.1097/01.brs.0000255076.45825.1e. [DOI] [PubMed] [Google Scholar]
- 22.Dai L D. Low lumbar spinal fractures: management options. Injury. 2002;33(7):579–582. doi: 10.1016/s0020-1383(02)00021-9. [DOI] [PubMed] [Google Scholar]
- 23.Dai L Y Jiang S D Wang X Y Jiang L S A review of the management of thoracolumbar burst fractures Surg Neurol 2007673221–231., discussion 231 [DOI] [PubMed] [Google Scholar]
- 24.Lehman R A Jr, Paik H, Eckel T T, Helgeson M D, Cooper P B, Bellabarba C. Low lumbar burst fractures: a unique fracture mechanism sustained in our current overseas conflicts. Spine J. 2012;12(9):784–790. doi: 10.1016/j.spinee.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Seybold E A, Sweeney C A, Fredrickson B E, Warhold L G, Bernini P M. Functional outcome of low lumbar burst fractures. A multicenter review of operative and nonoperative treatment of L3–L5. Spine (Phila Pa 1976) 1999;24(20):2154–2161. doi: 10.1097/00007632-199910150-00016. [DOI] [PubMed] [Google Scholar]
- 26.Abdel M P, Bodemer W S, Anderson P A. Supine thoracolumbar sagittal spine alignment: comparing computerized tomography and plain radiographs. Spine (Phila Pa 1976) 2012;37(4):340–345. doi: 10.1097/BRS.0b013e31821946d1. [DOI] [PubMed] [Google Scholar]
- 27.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy J P. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34(17):E599–E606. doi: 10.1097/BRS.0b013e3181aad219. [DOI] [PubMed] [Google Scholar]
- 28.Lazennec J Y, Ramaré S, Arafati N. et al. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9(1):47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schwab F, Patel A, Ungar B, Farcy J P, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35(25):2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 30.Reinhold M, Knop C, Beisse R. et al. Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, Internet-based multicenter study of the Spine Study Group of the German Association of Trauma Surgery. Eur Spine J. 2010;19(10):1657–1676. doi: 10.1007/s00586-010-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schnake K J, Stavridis S I, Kandziora F. Five-year clinical and radiological results of combined anteroposterior stabilization of thoracolumbar fractures. J Neurosurg Spine. 2014;20(5):497–504. doi: 10.3171/2014.1.SPINE13246. [DOI] [PubMed] [Google Scholar]
- 32.Isler B. Lumbosacral lesions associated with pelvic ring injuries. J Orthop Trauma. 1990;4(1):1–6. doi: 10.1097/00005131-199003000-00001. [DOI] [PubMed] [Google Scholar]
- 33.Schildhauer T A Josten Ch Muhr G Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing J Orthop Trauma 200620(1, Suppl):S44–S51. [PubMed] [Google Scholar]
- 34.Schildhauer T A, Bellabarba C, Nork S E, Barei D P, Routt M L Jr, Chapman J R. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma. 2006;20(7):447–457. doi: 10.1097/00005131-200608000-00001. [DOI] [PubMed] [Google Scholar]
- 35.Schildhauer T A, Ledoux W R, Chapman J R, Henley M B, Tencer A F, Routt M L Jr. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17(1):22–31. doi: 10.1097/00005131-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Berber O, Amis A A, Day A C. Biomechanical testing of a concept of posterior pelvic reconstruction in rotationally and vertically unstable fractures. J Bone Joint Surg Br. 2011;93(2):237–244. doi: 10.1302/0301-620X.93B2.24567. [DOI] [PubMed] [Google Scholar]


